Abstract
Background
Seriously ill patients and their physicians often avoid discussing prognosis, which may compromise optimal end-of-life (EOL) care planning. The relation between prognosis discussion and patient and family satisfaction with EOL care is unknown.
Methods
Using a 5-domain questionnaire, we surveyed inpatients with cancer or end-stage medical disease and their families on their satisfaction with specific aspects of EOL care and their overall satisfaction with EOL care. Scores were standardized to 0–100 points. We compared the results based on whether or not a physician had discussed the patient’s prognosis with them, as well as on whether the patient and family member agreed on whether the patient was nearing the end of life. Supplementary questions were also asked (e.g., preferred location of death, willingness to discuss cardiopulmonary resuscitation).
Results
Of 569 eligible patients and 176 eligible family members, 440 (77%) patients and 160 (91%) family members participated in the study. Overall, 18% of patients and 30.1% of families recalled a prognosis discussion with a physician. Patients who recalled such a discussion were more satisfied with overall care (76.1 v. 73.1 points, difference 3.0, 95% confidence interval [CI] 0.40 to 5.67, p = 0.02) and with communication and decision-making aspects of care (77.9 v. 72.4 points, difference 5.5, 95% CI 1.43 to 9.52, p = 0.008), and were more willing to discuss cardiopulmonary resuscitation status (69.6% v. 55.3%, difference 14.3, 95% CI 2.15 to 26.45, p = 0.03), than those who did not. Patients who were in accord with their family member as to whether they were nearing the end of life also showed significant satisfaction in these 3 areas. Family members’ overall satisfaction was also higher among those who recalled a prognosis discussion (75.3 v. 70.4 points, difference 4.9, 95% CI 0.53 to 9.24, p = 0.03). Multivariate analyses confirmed the significance of the relation between the prognosis discussion and overall satisfaction with care for both patients and family members.
Conclusion
Although discussions about prognosis occur infrequently for patients who have advanced terminal disease, such discussions with patients and their families may facilitate advance care planning and improve satisfaction with EOL care. Encouraging discussion regarding EOL status between the patient and family members may also lead to greater satisfaction with EOL care for patients.
“I didn’t expect him to die so soon. I got the feeling the doctors weren’t entirely honest with us about his condition. My husband resisted talking about dying and after 40 years of marriage I feel he let me down by not opening up and I guess I let him down for not knowing how to talk about some of the things that I needed to discuss. It would have been nice closure if things had been different in the end. I can never get that time back.”
– Wife of participant in end-of-life study
Truth-telling by physicians as death approaches may help patients and families to move toward closure and to discuss treatment preferences with their physicians.1,2 Observational studies document that such discussions occur infrequently3,4 and are rarely initiated by physicians.5-7 When these conversations do occur, patients often express dissatisfaction with physician performance and the quality of the interaction.8,9 Suboptimal communication at the end of life can increase anxiety and emotional distress, decrease hope and worsen overall suffering.10
The impact of prognostic discussions on patients’ perceptions of care is unknown. We sought to enrich our understanding of the relation between satisfaction with end-of-life (EOL) care and discussions regarding the patient’s prognosis. We hypothesized that prognostic discussions would have no adverse effect and may improve patient and family satisfaction with EOL care. Furthermore, in a secondary analysis, we postulated that when there is agreement between patient and family member on whether or not the patient is near or at the end of life, both groups would be more satisfied with EOL care than when they have discordant views.
Methods
Design
We administered a cross-sectional survey to inpatients in 5 Canadian tertiary care teaching hospitals. Eligible patients and methods have been reported in detail elsewhere.1,11 In brief, we enrolled patients 55 years old and older whose significant, advanced, end-stage disease could be defined by the following criteria:
Chronic obstructive lung disease: at least 2 of baseline PaCO2 of at least 45 mm Hg, cor pulmonale, an episode of respiratory failure within the preceding year, or forced expiratory volume in 1 second of 0.75 L or less.
Congestive heart failure: New York Heart Association class IV symptoms or a left-ventricular ejection fraction of 25% or less.
Cirrhosis: imaging studies or documentation of esophageal varices and 1 of hepatic coma, Child’s class C liver disease, or Child’s class B liver disease with gastrointestinal bleeding.
Cancer diagnosed as metastatic cancer or Stage IV lymphoma.
These criteria define a group of patients with end-stage disease at risk of dying and are associated with a 50% probability of survival at 6 months.12 These patients would not necessarily be considered “palliative” or “terminal” or be receiving palliative care. Most would be receiving active medical treatment for exacerbations or complications associated with their advanced disease.
Research coordinators screened medical wards for patients who had been in hospital for at least 72 hours and who met the eligibility criteria. Although mental status was not formally assessed, we excluded patients who were likely to have communication difficulties, such as language or cognitive barriers, on the basis of conversation with staff or with the patient in some circumstances. Patients identified a family member or person close to them (hereafter referred to as the family member) who provided some form of care at home. If no such person was available, patients were given only the patient-based questionnaire. All study participants gave informed written consent before participation; this study was approved by the research ethics boards of all participating institutions.
Questionnaire development
The overall goal of this research program was to develop and validate a novel satisfaction questionnaire to measure quality EOL care. There are no existing instruments for use in our target population in the hospital setting.13 The development of the questionnaire and its pre-testing have been explained in detail elsewhere.1,11 Briefly, to generate items for this satisfaction questionnaire, we reviewed taxonomies of quality EOL care published at the time of protocol development14-16 and held focus groups with health care professionals. We then conducted 12 semistructured interviews with seriously ill inpatients who met the inclusion criteria to determine whether any elements had been overlooked or were ambiguously phrased. The final 26 items were categorized into 5 domains: medical and nursing care, communication and decision-making, social relationships and support, meaningful existence, and community care.
Participants in this current study rated their satisfaction with each item on a 5-point Likert scale. Since the items were largely derived from the existing published literature and complemented with feedback from patients and health care providers, the questionnaire had both face and content validity. The questionnaire can be found at www.thecarenet.ca.
Variables
Scores for the items in the questionnaire were summed for each of the EOL care domains and for overall satisfaction and then standardized to a maximum score of 100 points by dividing by the maximum possible score and multiplying by 100. Patients and family members were also asked if they had had a discussion regarding their prognosis with a physician, using the question, “Have the doctors told you how long you (or the patient) can expect to live?” Response categories for both groups were yes/no. If the response was “no,” participants were then asked if they would like to be told this information. Next, to assess self-evaluation of the patient’s prognosis, all participants were asked if the patient was currently facing issues at the end of life (response options: I/the patient am/is currently facing them or have faced them; will likely face them in the next few weeks to months; will likely face them in the next 6 months; will likely face them in the next year; or not relevant).
Patients who were aware of their prognosis may have a different preference for other EOL decisions or aspects of care. Accordingly, patients were asked if they were willing to discuss their cardiopulmonary resuscitation preferences and to identify what level of care they would prefer to receive currently, using a scale of 1–10 where 1 = comfort measures only and 10 = full aggressive curative care. Finally, both patients and family members were asked to state their preference for location of death (response options: home, hospital, or doesn’t matter).
Sociodemographic data collected for the patients included availability of a family member, education, employment status, age, sex, marital status, religion, and type of community in which they lived (rural v. urban). Patient health-related variables included diagnosis and self-assessed functional status, determined using the Katz Functional Status Tool,17 a 6-item scale that measures functional ability with 0 = dependence and 1 = independence for each item; scores were summed across the items to determine the overall score. Family member sociodemographic data included education, employment status, age, sex, and relationship to patient. The family member was also asked to assess the patient’s functional ability using the Katz Functional Status Tool, and was asked whether the patient was currently facing issues at the end of life; the 5 response options were the same as those offered to the patient.
Results for the primary analysis were categorized according to whether the study participants had discussed prognosis with the physician. In the secondary analysis, we categorized results according to whether the patient and family member had selected the same response when asked whether the patient is currently facing EOL issues. Satisfaction with EOL care was compared based on these categories.
Statistical analysis
The number of patients who had a discussion about prognosis was calculated and reported. Bivariate relationships between those who did and those who did not have a prognostic discussion with the physician, from both patient and family member perspectives, were examined using t tests and χ2 tests: t tests were used for continuous variables (e.g., age, overall satisfaction) and χ2 tests were used for categorical variables (e.g., gender, marital status). No adjustments were made for multiple tests of significance. Ordinary least squares regression models were developed to identify significant factors that were associated with satisfaction with EOL care. The dependent variables included overall satisfaction with EOL care and the satisfaction scores for each domain. For all models, the independent variables were the sociodemographic and health-related covariates for patients and family members listed above. All independent covariates were entered as a block into the regression models. Before performing the multivariate analyses, we corrected for skewness the assessment of functional impairment by both patients and family members by squaring this term. An F test was used to test overall fit of the model. Finally, we repeated the bivariate analyses described above to determine the associations with patient and family member agreement and disagreement on the patient’s EOL status.
Results
Participants
A total of 569 eligible patients were identified and approached for consent at 5 Canadian hospitals between November 2001 and June 2003. Of these, 447 provided consent, for an overall response rate of 78.6%. One patient died the day before the interview and 6 patients withdrew from the study shortly after the start of the interview, leaving 440 (77%) completed patient interviews. Most families were not available for interviews during the day; only 176 family members were approached for consent and, of these, 160 (90.9%) agreed to participate.
Patient characteristics and health- and care-related variables based on discussion of prognosis
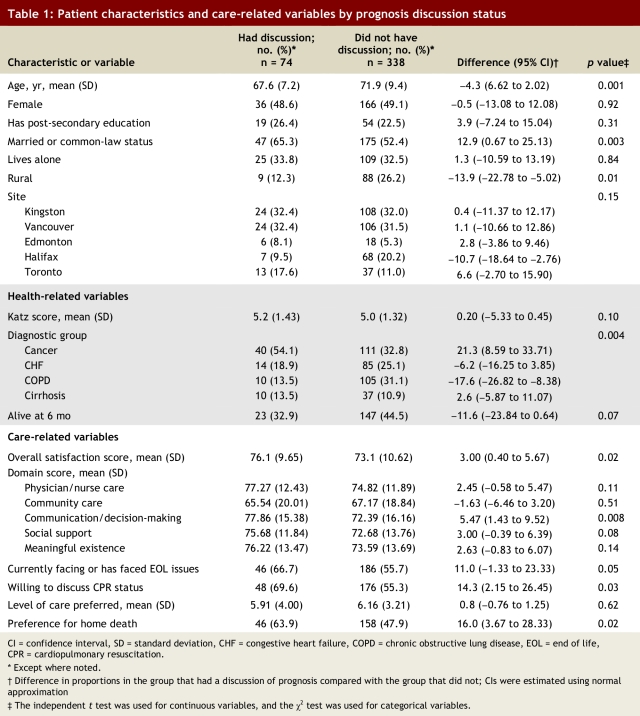
Of the 440 patients, 412 responded to the prognosis discussion question; 74 (18.0%) stated that they had discussed their prognosis with a physician. Demographic characteristics and health- and care-related variables according to prognosis discussion status are presented in Table 1. Patients with cancer were much more likely to have a discussion about prognosis that patients with medical diseases (40/151 [26%] v. 34/261 [13%], difference 13.5%, 95% confidence interval [CI] 5.33% to 21.60%, p = 0.0006).
Table 1.
Patient characteristics and care-related variables by prognosis discussion status
Overall satisfaction with EOL care was higher among patients who had discussed prognosis with a physician than among those who had not (76.1 v. 73.1 points, difference 3.0, 95% CI 0.40 to 5.67, p = 0.02). When significance tests were run separately for each of the 5 satisfaction domains (see Table 1), the results suggest that patients who had a discussion about their prognosis were more satisfied with communication and decision-making items than those who did not (77.9 v. 72.4, difference 5.5, 95% CI 1.43 to 9.52, p = 0.008).
These patients were also more willing to discuss preferences regarding cardiopulmonary resuscitation (69.6% v. 55.3%, difference 14.3, 95% CI 2.15 to 26.45, p = 0.03) and were more likely to prefer a home death (63.9% v. 47.9%, difference 16.0, 95% CI 3.67 to 28.33, p = 0.02); there was a trend toward these patients being more likely to state that they were currently facing EOL issues (66.7 v. 55.7%, difference 11.0, 95% CI –1.33 to 23.33, p = 0.054). Of the 338 patients who had not had a discussion about prognosis with their attending physician, 143 (43.6%) said they would be interested in having such a conversation and 185 (56.4%) said they would not.
Family member characteristics and care-related variables based on discussion of prognosis
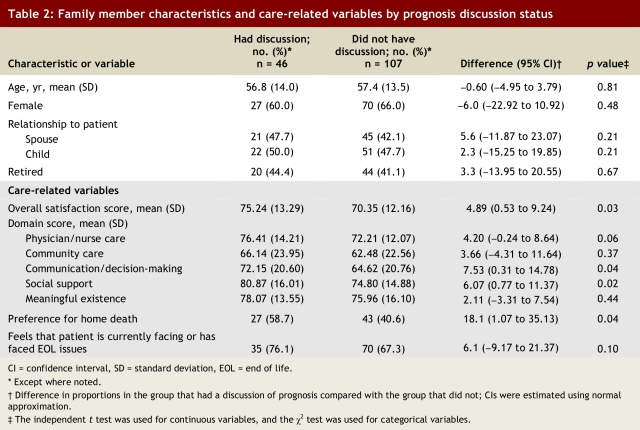
Of 160 family members, 153 responded to the question about prognosis; 46 (30.1%) stated that they had discussed the patient’s prognosis with the patient’s physician. Of these 46, 25 corresponding patients also reported having had a discussion with the physician. Therefore, a total of 95 patients or family members (95 of 412 respondents or 23.2%) reported having a discussion about prognosis with the doctor. The demographic characteristics and care-related variables for family members according to the prognosis discussion status are shown in Table 2.
Table 2.
Family member characteristics and care-related variables by prognosis discussion status
Family members’ overall satisfaction was higher in the group that had discussed prognosis compared with those who had not (75.3 v. 70.4 points, difference 4.9, 95% CI 0.53 to 9.24, p = 0.03). They were also more satisfied with communication and decision-making (72.2 v. 64.6 points, difference 7.6, 95% CI 0.31 to 14.78, p = 0.04) and the social support (80.9 v. 74.8 points, difference 6.1, 95% CI 0.77 to 11.37, p = 0.02). There was a non-significant trend toward increased satisfaction with physician/nurse care in the group that had discussed prognosis (76.4 v. 72.2 points, difference 4.2, 95% CI –0.24 to 8.64, p = 0.06). Of the 107 family members who had not had a discussion about prognosis with the attending physician, 97 (89.8%) said they would like such a discussion and 11 (10.2%) said they would not.
Multivariable model
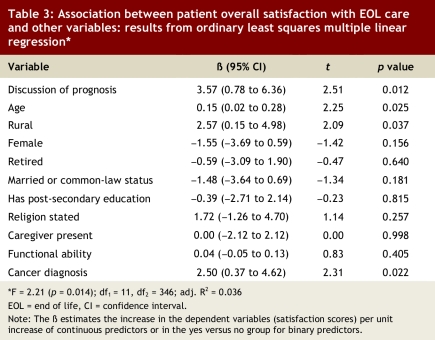
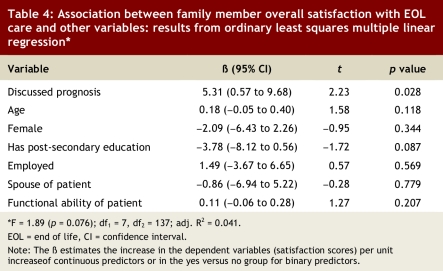
For both patients and family members, the multivariate analyses confirmed the significant relation between having a prognosis discussion and overall satisfaction with EOL care, after controlling for demographic characteristics and health-related variables (95% CI 0.78 to 6.36, p = 0.012 for patients; 95% CI 0.57 to 9.68, p = 0.028 for family members; see Tables 3 and 4).
Table 3.
Association between patient overall satisfaction with EOL care and other variables: results from ordinary least squares multiple linear regression
Table 4.
Association between family member overall satisfaction with EOL care and other variables: results from ordinary least squares multiple linear regression
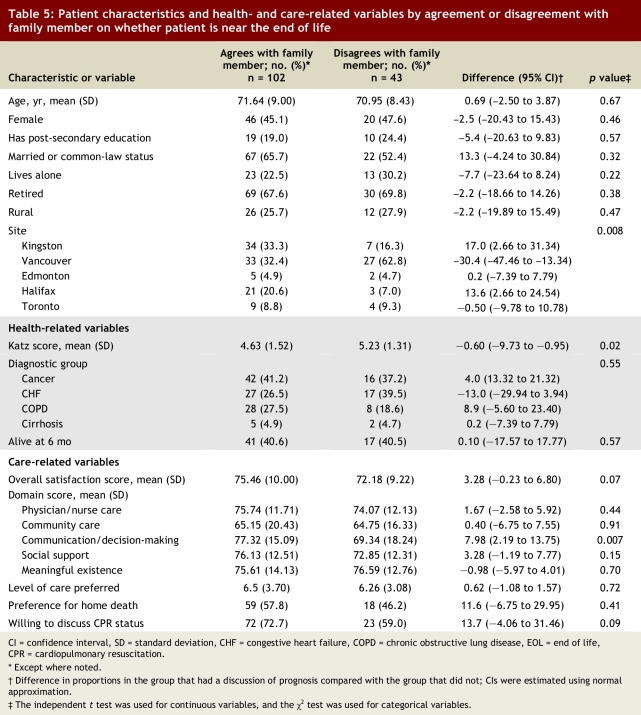
Agreement on EOL status and patient satisfaction with EOL care
Of the 145 pairs of patients and family members who responded to the question about whether the patient was currently facing EOL issues, 102 (70.3%) selected the same response. As Table 5 shows, patients who were in agreement with their family member with respect to their EOL status were more likely to be satisfied with communication and decision-making than those who were not (77.3 v. 69.3 points, difference 8.0, 95% CI 2.19 to 13.75, p = 0.007). They also tended to have a higher overall satisfaction with EOL care (75.5 v. 72.2 points, difference 3.3, 95% CI –0.23 to 6.80, p = 0.07) and were more willing to discuss preferences regarding cardiopulmonary resuscitation (72.7% v. 59.0%, difference 13.7, 95% CI –4.06 to 31.46, p = 0.09).
Table 5.
Patient characteristics and health- and care-related variables by agreement or disagreement with family member on whether patient is near the end of life
Among family members, there were no significant differences in either demographic characteristics or overall satisfaction with EOL care between those who were in agreement with the patient as to EOL status and those who were not (data not shown).
Discussion
Patients who have life-limiting, advanced chronic disease identify that receiving honest information about their condition and having time to prepare for life’s end are key aspects of quality EOL care.11 By increasing the quantity and quality of discussions about prognosis, it should be possible to increase satisfaction with EOL care. However, if knowledge of prognosis is not desired or the discussion is done poorly, the quality of EOL care may be diminished.
In this study, we surveyed 440 patients and 160 family members to examine the relation between having a conversation with the physician about prognosis and satisfaction with EOL care. We formed our study population based on established clinical criteria that define groups of patients who have a 50% probability of 6-month survival. Although more than 50% of patients died within 6 months of the interview, a minority of patients (18%) and families (30%) recalled having such a conversation with physicians. Those patients who stated they had had such a discussion were more likely to discuss their preferences for cardiopulmonary resuscitation, agree that EOL issues were relevant to them, and desire a home death. Other study results have shown that these conversations occur infrequently, that the physician and patient don’t always agree on whether such a discussion took place, that the patient and family tend to have overly optimistic expectations, and that patients and families who have unrealistic expectations of the prognosis are more likely to choose aggressive terminal care in hospital.18,19
Perhaps our most significant observation was that patients and family members who had discussed prognosis with their physicians were equally or more satisfied with EOL care than those who had not. Furthermore, when patients and families agreed on prognosis, they reported greater satisfaction with care than those who disagreed. We are not aware of other reports in the literature comparing patient satisfaction with prognostic disclosure, but our findings are consistent with those of numerous other studies of optimal EOL care that suggest that improving communication and decision-making will have the greatest impact on quality of care.11,20-22 It may be that discussions about prognosis are an integral part of quality EOL care.
Another important finding from this study was that patients who have end-stage medical diagnoses are less likely than patients who have cancer to have a discussion about prognosis. Given differing and sometimes unpredictable disease trajectories in patients who have advanced, end-stage medical diseases, this is not surprising.23 However, symptom burden and short-term outcomes for elderly patients who have end-stage medical disease is often as poor as or worse than that for patients who have cancer.24,25
Waiting until a terminal prognosis is certain before initiating a discussion about prognosis may limit opportunities for adequate information exchange and time to prepare for death. Patients and families accept prognostic uncertainty,26 and honest, timely, and complete communication are key determinants of overall satisfaction with care.11,27,28 Despite a high risk of mortality in ensuing months, most patients reported that they had not had an EOL discussion. Over half of those patients stated that they would rather not discuss prognosis with their physicians. This result is consistent with a similar survey of patients with advanced medical disease, in which 40% reported that they would prefer not to discuss life expectancy.18 Interestingly, those who preferred not to discuss these issues tended to have a much more optimistic outlook on their prognosis. They may not see the relevance of having such discussion if they do not see themselves near or at the end of life. There may be other undescribed or unrecognized barriers to these discussions; this issue warrants further investigation.
In contrast, although most family members had not had a prognosis discussion, 90% of them indicated that they would like to have such a discussion, a finding that is congruent with other reports.29 Our finding of the association between patient and family member congruency on whether the patient was “facing EOL” and higher overall satisfaction with care suggests that efforts to align preferences for prognosis disclosure between patients and family may increase satisfaction with EOL care. Since neither the patient nor the family may understand the importance of accurate prognostic information in quality EOL care and neither may initiate the discussion, it is incumbent on health care professionals to take this lead and to foster the climate in which such discussions can be held. Guidelines for these discussions have been published and provide a good resource for assisting physicians in this challenging task.30,31
This study has several limitations. First, we relied on patient and family member recall that a prognosis discussion had or had not occurred. We did not explore whether a prognosis discussion was attempted and discontinued because of patient preference to avoid such a discussion. It is possible that physicians did have such a discussion about prognosis but that it was not recognized or remembered as such. What is important is not whether the communication actually transpired but whether the patient (or family member) recalls, from their subjective perspective, the key prognostic information necessary to adequately prepare for life’s end. Furthermore, we asked only whether patients had a discussion regarding how long they had to live. There may have been other prognostic discussions by patients and their doctors that focused on quality of life or functional status. Thus, our findings are applicable only to one aspect of prognostic discussion, quantity of life. Second, this study was conducted in academic tertiary care Canadian hospitals with principally white, Anglo-Saxon, Christian subjects; therefore, our findings may not be applicable to other settings. Third, given the cross-sectional nature of our survey, we cannot attribute increased satisfaction to a prior prognosis discussion. Fourth, we conducted multiple tests of significance, and thus some of our significant observations may be due to chance. Finally, to measure satisfaction we used a novel instrument; the clinical importance of a difference of 4–5 points on this instrument is unknown.
In summary, the results of this study suggest that when prognosis is discussed with patients and families, satisfaction with care may be greater, especially in relation to communication and decision-making. We have previously established that having time to adequately prepare for life’s end is very important to most seriously ill Canadians and their families.11 Therefore, communicating prognosis with seriously ill patients and their families, and ensuring shared perceptions of EOL status, may have a positive impact on EOL care.
Biographies
Daren K Heyland, MD, is a professor in the Department of Medicine at Kingston General Hospital/Queen’s University, Kingston, Ontario, Canada.
Diane E Allan, MA, is a research associate in the Centre on Aging at the University of Victoria, Victoria, British Columbia.
Graeme Rocker, MD, is a professor in the Department of Medicine at Dalhousie University, Halifax, Nova Scotia.
Peter Dodek, MD, is an associate professor in the Department of Medicine and Center for Health Evaluation and Outcome Sciences at St. Paul’s Hospital and University of British Columbia, Vancouver, B.C.
Deb Pichora was a research associate in the Department of Medicine at Kingston General Hospital/Queen’s University, Kingston, Ontario.
Amiram Gafni is a professor in the Department of Clinical Epidemiology and Biostatistics in the Centre for Health Economics and Policy Analysis at McMaster University, Hamilton, Ontario.
Footnotes
Competing interests: None declared.
Funding source: Provided by the National Health and Research Development Program of Canada for Dr. Daren Heyland. The sponsor played no role in the design, analysis, or interpretation of this study.
Contributors: Daren Heyland participated in the study conception and design, data collection, data analysis, and manuscript preparation. Diane Allan participated in the data analysis and manuscript preparation. Deb Pichora participated in the study conception and design, data collection, and manuscript preparation. Peter Dodek participated in the study conception and design, data collection, data interpretation, and manuscript preparation. Graeme Rocker participated in the study conception and design, data collection, data interpretation, and manuscript preparation. Amiram Gafni participated in the study conception and design, data interpretation, and manuscript preparation. All of the authors approved the final version for publication.
References
- 1.Heyland Daren K, Groll Dianne, Rocker Graeme, Dodek Peter, Gafni Amiram, Tranmer Joan, Pichora Deb, Lazar Neil, Kutsogiannis Jim, Shortt Sam, Lam Miu, Canadian Researchers at the End of Life Network (CARENET. End-of-life care in acute care hospitals in Canada: a quality finish? J Palliat Care. 2005;21(3):142–150. [PubMed] [Google Scholar]
- 2.Smith R. A good death. An important aim for health services and for us all. BMJ. 2000;320(7228):129–130. doi: 10.1136/bmj.320.7228.129. http://bmj.com/cgi/pmidlookup?view=long&pmid=10634711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curtis J R, Patrick D L, Caldwell E, Greenlee H, Collier A C. The quality of patient-doctor communication about end-of-life care: a study of patients with advanced AIDS and their primary care clinicians. AIDS. 1999;13(9):1123–1131. doi: 10.1097/00002030-199906180-00017. [DOI] [PubMed] [Google Scholar]
- 4.Field M, Cassel C Committee on Care at the End-of-Life Institute of Medicine. Approaching death: improving care at the end-of-life. Washington (DC): National Academy Press; 1997. [Google Scholar]
- 5.Emanuel L L, Barry M J, Stoeckle J D, Ettelson L M, Emanuel E J. Advance directives for medical care — a case for greater use. N Engl J Med. 1991;324(13):889–895. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 6.Johnston S C, Pfeifer M P, McNutt R. The discussion about advance directives. Patient and physician opinions regarding when and how it should be conducted. End of Life Study Group. Arch Intern Med. 1995;155(10):1025–1030. doi: 10.1001/archinte.155.10.1025. [DOI] [PubMed] [Google Scholar]
- 7.White Douglas B, Engelberg Ruth A, Wenrich Marjorie D, Lo Bernard, Curtis J Randall. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med. 2007;35(2):442–448. doi: 10.1097/01.CCM.0000254723.28270.14. [DOI] [PubMed] [Google Scholar]
- 8.Billings J A, Kolton E. Family satisfaction and bereavement care following death in the hospital. J Palliat Med. 1999;2(1):33–49. doi: 10.1089/jpm.1999.2.33. [DOI] [PubMed] [Google Scholar]
- 9.Curtis J R, Engelberg R A, Nielsen E L, Au D H, Patrick D L. Patient-physician communication about end-of-life care for patients with severe COPD. Eur Respir J. 2004;24(2):200–205. doi: 10.1183/09031936.04.00010104. http://erj.ersjournals.com/cgi/pmidlookup?view=long&pmid=15332385. [DOI] [PubMed] [Google Scholar]
- 10.Kuhl David. What dying people want: practical wisdom for the end of life. New York: Public Affairs; 2002. [Google Scholar]
- 11.Heyland Daren K, Dodek Peter, Rocker Graeme, Groll Dianne, Gafni Amiram, Pichora Deb, Shortt Sam, Tranmer Joan, Lazar Neil, Kutsogiannis Jim, Lam Miu, Canadian Researchers End-of-Life Network(CARENET. What matters most in end-of-life care: perceptions of seriously ill patients and their family members. CMAJ. 2006;174(5):627–633. doi: 10.1503/cmaj.050626. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=16505458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Danis M, Mutran E, Garrett J M, Stearns S C, Slifkin R T, Hanson L, Williams J F, Churchill L R. A prospective study of the impact of patient preferences on life-sustaining treatment and hospital cost. Crit Care Med. 1996;24(11):1811–1817. doi: 10.1097/00003246-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Mularski Richard A, Dy Sydney M, Shugarman Lisa R, Wilkinson Anne M, Lynn Joanne, Shekelle Paul G, Morton Sally C, Sun Virginia C, Hughes Ronda G, Hilton Lara K, Maglione Margaret, Rhodes Shannon L, Rolon Cony, Lorenz Karl A. A systematic review of measures of end-of-life care and its outcomes. Health Serv Res. 2007;42(5):1848–1870. doi: 10.1111/j.1475-6773.2007.00721.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emanuel EL, Emanuel LL. The promise of a good death. Lancet. 1998;351(Suppl 2):2–21. doi: 10.1016/s0140-6736(98)90329-4. [DOI] [PubMed] [Google Scholar]
- 15.Lynn J. Measuring quality of care at the end of life: a statement of principles. J Am Geriatr Soc. 1997;45(4):526–527. doi: 10.1111/j.1532-5415.1997.tb05184.x. [DOI] [PubMed] [Google Scholar]
- 16.Field MJ, Cassel CK, editors. Approaching death: improving care at the end of life. Washington (DC): National Academy Press; 1997. http://www.nap.edu/openbook.php?record_id=5801. [PubMed] [Google Scholar]
- 17.Katz S, Downs T D, Cash H R, Grotz R C. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 18.Fried Terri R, Bradley Elizabeth H, O’Leary John. Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc. 2003;51(10):1398–1403. doi: 10.1046/j.1532-5415.2003.51457.x. [DOI] [PubMed] [Google Scholar]
- 19.Weeks J C, Cook E F, O’Day S J, Peterson L M, Wenger N, Reding D, Harrell F E, Kussin P, Dawson N V, Connors A F, Lynn J, Phillips R S. Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709–1714. doi: 10.1001/jama.279.21.1709. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=9624023. [DOI] [PubMed] [Google Scholar]
- 20.Hanson L C, Danis M, Garrett J. What is wrong with end-of-life care? Opinions of bereaved family members. J Am Geriatr Soc. 1997;45(11):1339–1344. doi: 10.1111/j.1532-5415.1997.tb02933.x. [DOI] [PubMed] [Google Scholar]
- 21.Curtis J Randall, Patrick Donald L, Engelberg Ruth A, Norris Kaye, Asp Charles, Byock Ira. A measure of the quality of dying and death. Initial validation using after-death interviews with family members. J Pain Symptom Manage. 2002;24(1):17–31. doi: 10.1016/s0885-3924(02)00419-0. [DOI] [PubMed] [Google Scholar]
- 22.Malacrida R, Bettelini C M, Degrate A, Martinez M, Badia F, Piazza J, Vízzardi N, Wullschleger R, Rapin C H. Reasons for dissatisfaction: a survey of relatives of intensive care patients who died. Crit Care Med. 1998;26(7):1187–1193. doi: 10.1097/00003246-199807000-00018. [DOI] [PubMed] [Google Scholar]
- 23.Lunney June R, Lynn Joanne, Foley Daniel J, Lipson Steven, Guralnik Jack M. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–2392. doi: 10.1001/jama.289.18.2387. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=12746362. [DOI] [PubMed] [Google Scholar]
- 24.Tranmer Joan E, Heyland Daren, Dudgeon Debra, Groll Dianne, Squires-Graham Mae, Coulson Kathy. Measuring the symptom experience of seriously ill cancer and noncancer hospitalized patients near the end of life with the memorial symptom assessment scale. J Pain Symptom Manage. 2003;25(5):420–429. doi: 10.1016/s0885-3924(03)00074-5. [DOI] [PubMed] [Google Scholar]
- 25.Tanvetyanon Tawee, Leighton John C. Life-sustaining treatments in patients who died of chronic congestive heart failure compared with metastatic cancer. Crit Care Med. 2003;31(1):60–64. doi: 10.1097/01.CCM.0000038210.68440.8B. [DOI] [PubMed] [Google Scholar]
- 26.Guy Victoria. Liver failure, life support, family support, and palliation: an inside story. J Crit Care. 2006;21(3):250–252. doi: 10.1016/j.jcrc.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 27.LeClaire Michele M, Oakes J Michael, Weinert Craig R. Communication of prognostic information for critically ill patients. Chest. 2005;128(3):1728–1735. doi: 10.1378/chest.128.3.1728. http://www.chestjournal.org/cgi/pmidlookup?view=long&pmid=16162781. [DOI] [PubMed] [Google Scholar]
- 28.Heyland Daren K, Cook Deborah J, Rocker Graeme M, Dodek Peter M, Kutsogiannis Demetrios J, Peters Sharon, Tranmer Joan E, O’Callaghan Christopher J. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2002 Nov 28;29(1):75–82. doi: 10.1007/s00134-002-1569-y. [DOI] [PubMed] [Google Scholar]
- 29.Royak-Schaler Renee, Gadalla Shahinaz, Lemkau Jeanne, Ross Douglas, Alexander Carla, Scott Deborah. Family perspectives on communication with healthcare providers during end-of-life cancer care. Oncol Nurs Forum. 2006 Jul 01;33(4):753–760. doi: 10.1188/06.ONF.753-760. [DOI] [PubMed] [Google Scholar]
- 30.Back Anthony L, Arnold Robert M, Baile Walter F, Tulsky James A, Fryer-Edwards Kelly. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55(3):164–177. doi: 10.3322/canjclin.55.3.164. http://caonline.amcancersoc.org/cgi/pmidlookup?view=long&pmid=15890639. [DOI] [PubMed] [Google Scholar]
- 31.Robert Buckman. How to break bad news: a guide for health care professionals. Baltimore: Johns Hopkins University Press; 1992. [Google Scholar]