Abstract
Background
Asynchronous telehealth captures clinically important digital samples (e.g., still images, video, audio, text files) and relevant data in one location and subsequently transmits these files for interpretation at a remote site by health professionals without requiring the simultaneous presence of the patient involved and his or her health care provider. Its utility in the health care system, however, still remains poorly defined. We conducted this scoping review to determine the impact of asynchronous telehealth on health outcomes, process of care, access to health services, and health resources.
Methods
A search was performed up to December 2006 of MEDLINE, CINAHL, HealthSTAR, the Database of Abstracts of Reviews of Effectiveness, and The Cochrane Library. Studies were included if they contained original data on the use of asynchronous telehealth and were published in English in a peer-reviewed journal. Two independent reviewers screened all articles and extracted data, reaching consensus on the articles and data identified. Data were extracted on general study characteristics, clinical domain, technology, setting, category of outcome, and results. Study quality (internal validity) was assessed using the Jadad scale for randomized controlled trials and the Downs and Black index for non-randomized studies. Summary data were categorized by medical specialty and presented qualitatively.
Results
The scoping review included 52 original studies from 238 citations identified; of these 52, almost half focused on the use of telehealth in dermatology. Included studies were characterized by diverse designs, interventions, and outcomes. Only 16 studies were judged to be of high quality. Most studies showed beneficial effects in terms of diagnostic accuracy, wait times, referral management, and satisfaction with services. Evidence on the impact of asynchronous telehealth on resource use in dermatology suggests a reduction in the number of, or avoidance of, in-person visits. Reports from other clinical domains also described the avoidance of unnecessary transfer of patients.
Conclusions
A significant portion of the asynchronous telehealth literature involves its use in dermatology. Although the quality of many original studies remains poor, at least within dermatology, there is consistent evidence suggesting that asynchronous telehealth could lead to shorter wait times, fewer unnecessary referrals, high levels of patient and provider satisfaction, and equivalent (or better) diagnostic accuracy when compared with face-to-face consultations. With the exception of a few studies in pediatric asthma, the impact of this intervention on individual health outcomes remains unknown.
Note: An editable, living version of this article can be found online at http://wikisr.openmedicine.ca/
The need to deliver services to remote and underserved communities has been the main impetus behind the expansion of telehealth programs. Telehealth services that rely on real-time consultations, however, are realizing that their need to interact with dedicated, specialized facilities is limited by factors similar to those that affect traditional consultations, particularly the need to schedule face-to-face encounters between patients and health professionals. Telehealth programs may need to consider a shift toward a model that continues to rely on a physician’s real-time presence — a scarce commodity, given changing demographics and the lifestyle choices of physicians.1,2
One form of telehealth, known as asynchronous (or store-and-forward) telehealth, helps provide administrative and support services to areas that lack health professionals who can meet the needs of the population locally. Because of the widespread penetration of technologies such as the Internet, personal digital assistants (PDAs), smart phones (voice-centric handheld devices that function as phones and as PDAs), and digital photography, and in view of reductions in the cost of data storage, patients and health professionals can capture clinically important digital samples and relevant data (e.g., pictures of moles or surgical wounds, electrocardiograms, spirometry results, radiological images) in various formats (e.g., audio, video, text) from any location and send them to health professionals at distant sites for assessment at a convenient time. The independence of this digitized information from real-time interactions between patients and health professionals, together with the low cost of the required infrastructure, could allow asynchronous telehealth to reduce wait times, provide opportunities to rethink the way in which high-demand services are organized, optimize the use of limited health resources, and promote equitable access to health professionals and services.
So far, clinical applications of asynchronous telehealth have not received the same degree of attention as real-time telehealth.3 This qualitative scoping review addresses the impact of asynchronous telehealth on health outcomes, health delivery services, health care resource use, and user satisfaction.
Methods
A protocol, which is available from the corresponding author, was written a priori and followed throughout the review process. Article screening and data extraction were performed using TrialStat SRS 4.0 (Ottawa, Canada).
Literature search strategy
An information specialist (ME) prepared a detailed search strategy (online Appendix 1) combining 3 clusters of terms: the first focused on telehealth, the second on asynchronous forms of electronic communication, and the third on health services delivery. Electronic searches, performed up to mid-December 2006, included the following databases: MEDLINE (from 1966), CINAHL (from 1982), HealthSTAR (from 1975), the Database of Abstracts of Reviews of Effectiveness (DARE), and The Cochrane Library. The yield from the bibliographic databases was complemented with a scan of reference lists from eligible reports.
Selection method
An article was regarded as potentially eligible if it met all of the following criteria:
evaluated 1 or more clinical asynchronous services
involved the capture of digital clinical samples by physicians, community-based nurses, or trained members of the public
focused on the delivery of digital samples for assessment by specialists at separate locations, transferred electronically
included data on health outcomes, process of care, resource utilization, or user satisfaction
appeared in an English-language peer-reviewed journal since 1995.
Studies on clinical asynchronous telehealth were excluded if they focused only on diagnostic concordance among different methods (i.e., no other outcome data presented) or on technical issues (e.g., different modalities of telehealth or telehealth versus face-to-face consultations).
Two teams of 2 reviewers (AM and CL, and SK and HD) independently screened each title and abstract of a potentially eligible report. Two of the authors (ARJ and AD) resolved any discrepancies between the teams by independently reviewing each title and abstract or, if necessary, the full report. If disagreement persisted, a final decision was reached by consensus between ARJ and AD.
Data extraction and abstraction strategy
Both teams of reviewers extracted data independently, using unmasked copies of the reports. Where disagreements existed, the final set was reviewed independently by ARJ and AD. Any differences were resolved by consensus.
A standard data extraction form was used to collect the following information from each report:
general characteristics (e.g., name of lead author, publication title, year of publication, country of study)
study type (e.g., observational [i.e., non-experimental], experimental, or descriptive); if observational, the study was recorded as a case series, a cross-sectional effort, a cohort or a case-control study; where relevant, it was stated whether the study was identified as retrospective or prospective
technological characteristics of the telehealth platform (e.g., Integrated Services Digital Network [ISDN]- or Internet Protocol [IP]-based, resolution level)
patient population (e.g., sample size, demographic characteristics)
setting (e.g., rural or urban)
originator of the consultation (e.g., family physician, nurse, community member)
comparison group(s) (e.g., face to face)
purpose of the consultation (e.g., acute, non-acute, education, diagnosis, therapeutic support, follow-up)
outcomes measured and main findings (e.g., impact on health outcomes, process of care, resource use).
Health outcomes were defined as an effect on an individual’s health status or a clinical consequence (e.g., increased compliance with treatment or reduced burden of illness). Rates of diagnostic concordance, only if reported with other health or non-health outcomes, were considered for this category. Process of care outcomes described access to care, wait times, or time to completion for a clinical encounter. Outcomes on resource utilization included reports of cost-effectiveness data or impact on hospital admissions, visit frequency, or rate of referrals. User satisfaction was used to categorize feedback from a patient or provider on satisfaction, expectations, or acceptance of asynchronous telehealth.
Strategy for quality assessment
The methodological quality of each study was assessed using the Jadad scale for randomized controlled trials (RCTs),4 and the Downs and Black checklist for observational studies and controlled clinical trials (CCTs).5 The last question (question 27) on the Downs and Black checklist is designed to assess the study’s statistical power. Because the Downs and Black checklist was used only for qualitative studies and CCTs, we used a modified score with “0” or “1,” according to whether authors reported statistical power tests in the original article (score = 1) or not (score = 0). The modified scale allowed for a maximum possible total score of 28 for a given study.
The median study quality score was used to distinguish between low-quality and high-quality studies where no pre-specified score existed.6 RCTs were considered to be of high quality if they received a Jadad score greater than 2 points or a score greater than 14 points using the Downs and Black checklist.
Data analysis
The reports were categorized by medical specialty. A general description was provided for the set of publications that met the inclusion criteria, based on general characteristics and quality scores for the individual publications. Evidence tables were produced to summarize the information extracted from the publications.
Results were presented qualitatively. A meta-analysis was considered to be inappropriate for the present review, given the clinical heterogeneity of the included studies. There were significant disparities among studies in clinical condition, acuity of health service delivery (acute, chronic), clinical setting, and technological intervention.
Results
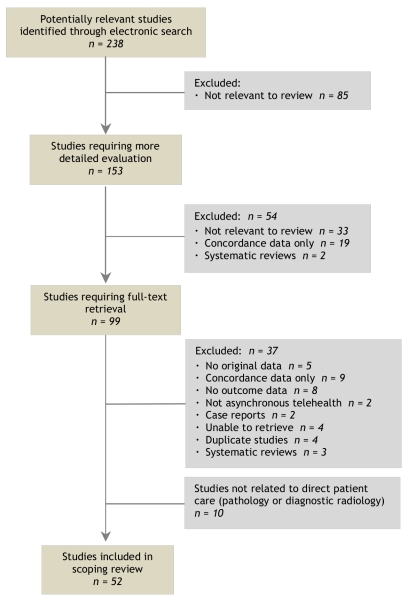
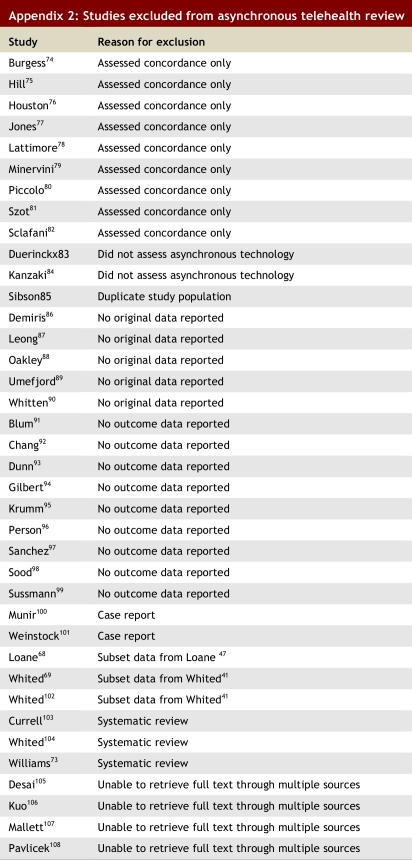
The literature search yielded 238 publications, of which 139 reports were excluded because they did not address issues related to clinical asynchronous telehealth. A total of 99 potentially eligible publications required the full-text version for further investigation. After review of the full-text version, 37 reports were excluded for various reasons (see online Appendix 2).
From the remaining 62 publications, 10 were excluded because they did not involve medical areas traditionally associated with direct patient care. Six7-12 of these involved pathology, while 413-16 addressed applications for use in radiology. Agreement between reviewers was high, although no formal statistical measure was completed.
A summary of the selection process is presented in Figure 1.
Figure 1.
Selection of studies for scoping review
Study characteristics
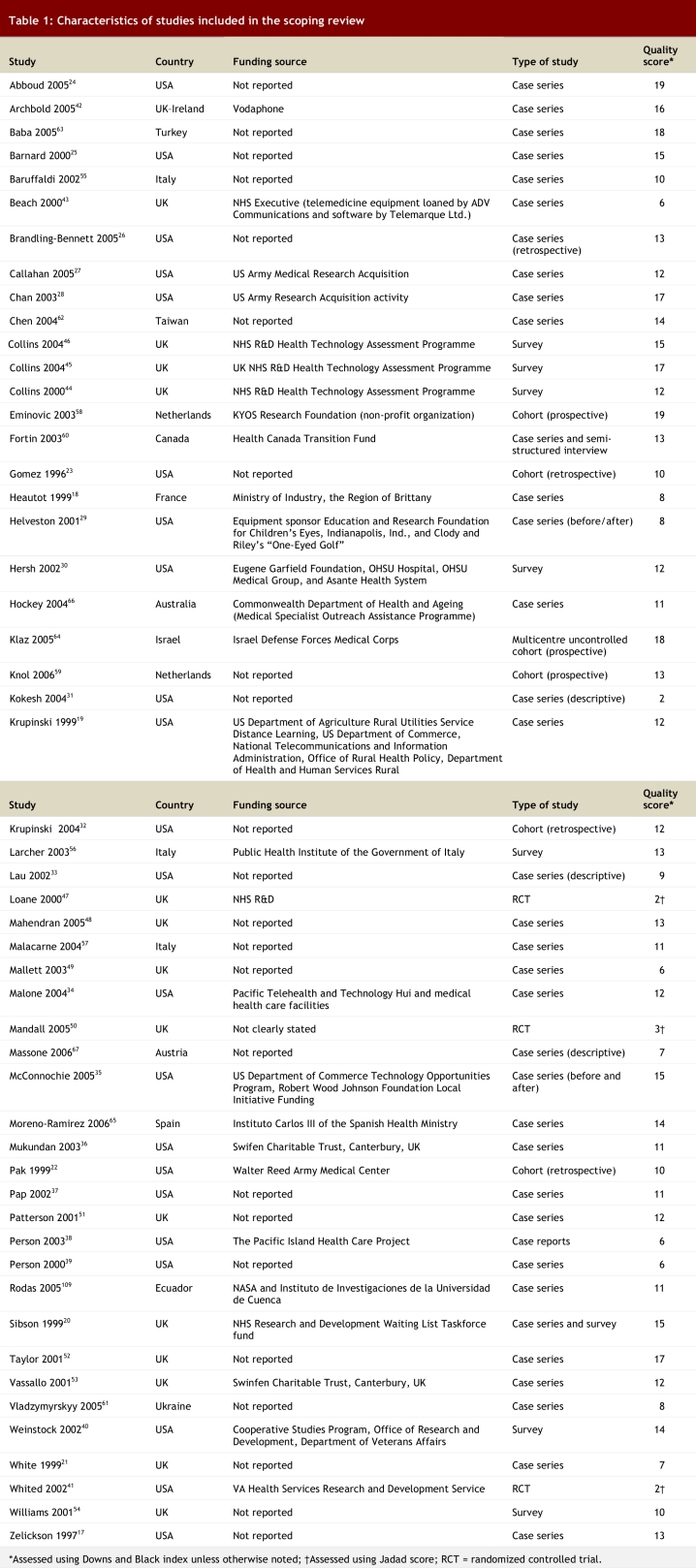
Fifty-two studies were included in this review; of these, 717-23 were published before 2000. The study characteristics are presented in Tables 1 and 2.
Table 1.
Characteristics of studies included in the scoping review
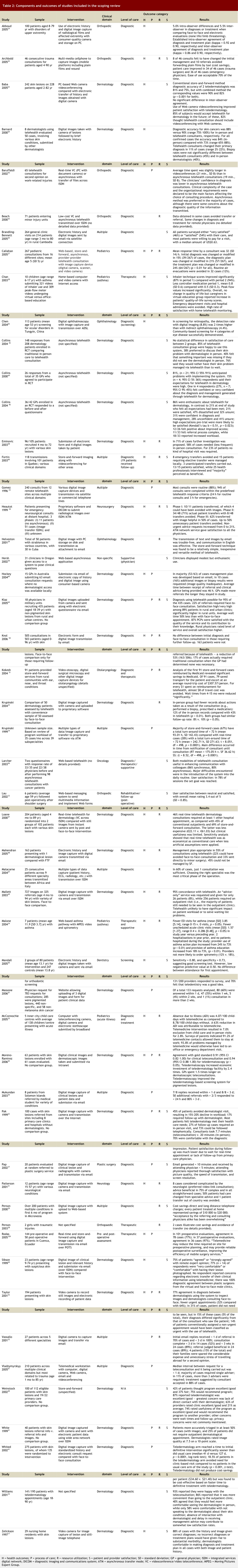
Table 2.
Components and outcomes of studies included in the scoping review
The primary author was based in the United States for 22 studies17,19,22-41 and in the United Kingdom for 15.20,21,42-46,47,48-54 Primary authors for the remaining publications were based in a number of countries, with 3 from Italy55-57 and 2 from the Netherlands.58,59 One study originated in Canada.60
Study designs included 3 RCTs41,47,50 and 7 surveys.30,40,44-46,54,56 Thirty-six publications were designed as case series studies, while 6 were characterized as cohort studies.
In 24 publications, no funding source for the study was documented.
Dermatology was the most frequently represented medical specialty (24 publications). Nine articles reported data based on results identified across various medical specialties;19,23,26,36,39,53,57,60,61 6 reported on musculoskeletal medicine,24,33,38,42,43,55 4 on pediatrics,27,28,34,35 and 2 on ophthalmology.29,62 Other clinical settings included plastic surgery and the neurological sciences.
Quality assessment
One of 3 RCTs was judged to be of high quality50 (see Table 1). Of the remaining 49 studies, 15 received high-quality ratings.20,24,25,28,35,40,42,45,46,52,58,62-65
Data analyses and synthesis
Dermatology
Many publications in this group addressed more than 1 outcome. Health outcomes (mainly diagnostic accuracy), user satisfaction and resource use were the most commonly represented categories.
Health outcomes
Eleven publications evaluated the role of health outcomes. Ten of these reported on diagnostic concordance or diagnostic accuracy. Several publications reported high levels of diagnostic accuracy with the use of telehealth in dermatology. One study reported that diagnostic accuracy for teleconsultants as a group was obtained in 73% of all cases of skin lesions and in 90% of evaluations of skin cancer lesions.25 Other reports documented rates of diagnostic accuracy varying from 75% to 88%.17,52,63 Combining images from asynchronous telehealth with standard patient histories increased diagnostic accuracy to 90% and 82% (p < 0.001) for 2 teledermatologists.63 The level of agreement with the gold standard (face-to-face consultation) was 0.91 (95% confidence interval [CI] 0.82-1.00) for clinical consultations using telehealth and 0.94 (95% CI 0.88-1.00) for dermatoscopy using telehealth (p > 0.05).65 Discrepancies were reported in the ability of asynchronous telehealth to contribute to the development of a management plan. In 1 study,66 an appropriate management plan was developed in 84% of the cases, but another study48 suggested that the use of asynchronous telehealth was successful in 55% of cases, while 45% could not be properly assessed. Mallett reported that “advice only” was possible in 8% of cases.49
Process of care
Of the 9 publications that assessed process-of-care outcomes, most studies reported a reduction in time to consultation. The average time between referral and clinical advice was reported to be 46 hours (range 17-119, standard deviation [SD] 24) in 1 publication.66 Massone reported that, of 133 requests analyzed, 80 (60%) were answered within a day.67 The use of telehealth in dermatology resulted in a time to initial definitive intervention that was significantly shorter than that of usual care (median 41 days v. 127 days, p < 0.0001); 25 patients (18.5%) in the telehealth arm avoided the need to visit a dermatology clinic.41 Klaz noted that the average wait times for asynchronous telehealth consultations (n = 435) were 50% less than those for face-to-face consultation.64 The time to perform a consultation was also affected by the use of asynchronous telehealth: the time to complete a telehealth consultation was one-third shorter on average than an in-person assessment.22 Three studies reported the ability to properly prioritize patients to address medical urgency.21,52,59 White21 reported that asynchronous telehealth, including the use of images, resulted in more accurate triage in 20 of the 40 (50%) cases. Telehealth use in dermatology also resulted in 14% of non-urgent referrals being upgraded to urgent, while another 24 of 136 (17%) were deemed to need assessment when none was planned.52,59
The use of asynchronous telehealth in dermatology decreased the frequency of in-person visits or avoided them altogether. Eminovic58 reported that 56 of 96 (58%) cases required less frequent in-person visits. The avoidance of an in-person visit ranged from 8% to 53%.21,22,48,49,52,58,59,64 One publication reported that the use of telehealth in dermatology resulted in the avoidance of 45% of in-person visits, producing a 15%-20% decline in workload.22
Resource utilization
Eleven publications on the use of telehealth in dermatology reported outcomes pertaining to resource use. Two studies41,47 quantified costs and reported their outcomes in 268,69 separate publications. Asynchronous telehealth was found to be less expensive than real-time telehealth consultations, but its clinical usefulness was limited.68 Whited69 noted that the use of telehealth in dermatology was not associated with cost-savings but seemed to be cost-effective when the faster time to definitive treatment was taken into account.
User satisfaction
Patient or provider satisfaction in general was determined to be high in 11 publications assessing telehealth in dermatology. Ninety-three percent of patients reported that they were happy with telehealth consultations.54 Klaz64 noted an 89% patient satisfaction rate with higher results in rural areas than in urban areas. Two studies45,63 reported that 85% of patients said they would accept the use of telehealth in dermatology in the future, 18% feeling that the conventional asynchronous method was sufficient. In contrast, 38% to 40% agreed with the statement that they would prefer to discuss their skin problem with the dermatologist in person and preferred direct contact.45,54 In addition, 40% said that they would feel that something important was missing if they did not see the dermatologist in person. When placed in the context of longer wait times, 76% preferred to be assessed by telehealth rather than wait for an in-person consultation.45
Most dermatologists felt comfortable making a diagnosis and devising a treatment plan in those cases for which they had access to the image and the patient’s history.17 One early study noted that 81% of general practitioners anticipated problems with implementation, while 15% said that expectations were high.44 A more recent report documented that 84% of providers had high expectations at the start of the study and 21% had similar expectations at the end.46 Furthermore, 21% were satisfied with the use of telehealth in dermatology, while 47% were dissatisfied and 32% were unsure. The most common reasons cited for negative responses were complex process and increased workload.
Studies involving multiple medical specialties
Health outcomes
Among the 9 articles in this group, none presented data on individual patient health outcomes for any of the medical specialties.
Process of care
Articles generally reported that less time was needed to process referrals. Most asynchronous telehealth cases (67%) had a total turn-around time of less than 72 hours, and the average turn-around time for store-and-forward cases was almost 40% faster than for real-time telehealth.19 Replies within 1 day of referral were provided in 70%-87.5% of cases and within 3 days of referral in 100% of cases.36,53 Actual telehealth consultations were completed within 3 days in 14 cases (52%) and within 3 weeks in 24 cases (89%). Vladymyrszki61 reported that the median interval between a request for consultation using telehealth services and it being conducted was less than 1 day, with an acceptance of treatment results in 88% of cases.
In mixed (i.e., multiple) medical specialities, 2 studies reported an approximate 15%-23% reduction in patient transfers.53,60 One Canadian study60 reported that of the 101 patients evaluated, 8 emergency transfers were avoided, and 15 patients who would have required elective transfer were managed locally via telehealth. No study in this group provided actual cost data. One study stated, “Cost savings have been substantial, not only direct costs but long distance telephone charges have been markedly reduced.”39
Resource utilization
Among the 9 articles in this group, none were identified that presented data on the impact of asynchronous telehealth on the use of resources.
User satisfaction
Three studies26,39,60 involving multiple medical specialties commented on patient and provider satisfaction. One study documented that patients were satisfied or very satisfied with the care received.26 Two others commented on positive acceptance and a general perception of asynchronous telehealth as being beneficial.39,60
Orthopedics
Five publications in the area of musculoskeletal medicine assessed trauma or injury.24, 38, 42, 43, 55 One study focused on postoperative recovery after shoulder surgery.33
Health outcomes
One study assessed the validity of asynchronous telehealth, noting minimal diagnostic disagreement (5% intra-observer and 5.5% inter-observer differences) with face-to-face and similar treatment plans to deliver care.24 None of the differences identified were regarded as serious (e.g., limb- or life-threatening). Archbold42 reported that 17% of asynchronous consults changed the initial management plan. The authors reported that results of all imaging of the injury revealed that initial descriptions submitted by the referring physician were inaccurate with respect to the nature of the injury.
Process of care
The 1 study that assessed process of care documented that the average time spent by orthopedic specialists was longer in videoconferencing (21 minutes, SD 8) than in asynchronous telehealth consultations (19 minutes, SD 8). However, a clinician’s confidence in the diagnosis was generally lower with asynchronous consultations.55
Resource utilization
Studies in orthopedics reported that the transport of plain films by taxi was avoided in 10 referrals,42 while in other settings patients avoided transfer or referral.38,43
Pediatrics
All studies in this group reported health outcomes, while 327,34,35 evaluated resource use.
Health outcomes
The use of asynchronous telehealth for pediatric care was associated with positive health outcomes. Two studies, with a combined sample of 17 patients, assessed the effect of asynchronous telehealth in pediatric asthma.28,34 Inhaler technique scores and quality-of-life survey scores improved in the intervention group.28 The use of asynchronous telehealth was also thought to be helpful in modifying the diagnosis in up to 15% of cases.27 One study on acute illnesses noted a 63% reduction in absence from school due to sickness with the use of telehealth.35
Process of care
Three pediatric studies reported a decrease in health care use. Malone34 noted a drop in emergency department visits (mean [SD] 3.85 [5.14], versus 0 visits, p < 0.05) and admissions (mean [SD] 1.57, [1.27], versus 0.286 [0.48], p < 0.05) compared with the year before. McConnochie35 also reported fewer visits to the emergency department, while Callahan27 reported avoidance of air evacuation in 12% of the population.
Other conditions
Health outcomes
Two studies focused on ocular conditions. Diagnostic agreement was reported in 12 of 15 cases that presented with strabismus.29 Another study, in which a digital ophthalmoscope was used to screen for retinopathy, showed a detection rate twice as high with digital imaging (8.8%) compared with indirect ophthalmoscopy (4.4%).62
Process of care
One study, which assessed the provision of nonsurgical oncology consultations to underserved communities, reported that the use of synchronous and asynchronous telehealth resulted in enhanced communication with colleagues (86% and 80% respectively).56 Kokesh31 documented that the use of asynchronous telehealth for ear, nose, and throat disorders reduced wait times of 4 to 15 months “significantly,” although specific data were not provided.
Similar findings were noted in neurological conditions, where the treatment plan was changed in 50% of the cases as a result of the specialist’s advice and 1 transfer of a patient out of the country was avoided.51 The use of asynchronous telehealth to transmit imaging in the context of neurosurgical evaluation reduced the need to transfer a patient by 50%.18
Resource utilization
One study was identified in this group as providing utilization data. In otolaryngology, 79 of 91 patients saved transport costs, producing a savings of US$307.57 per person.31 This study concluded that for every $1 spent on reimbursement for telehealth, $8 in travel costs could be avoided.
Discussion
Similar to telehealth literature reviewed elsewhere,70-72 the original literature in this review was of low methodological quality. Most publications did not appear to follow sound methodological principles, or described results based on small sample sizes that would be consistent with feasibility studies or pilot projects. However, despite the poor quality of evidence, certain trends were consistent across many studies.
Beyond diagnostic accuracy and concordance, most publications did not report meaningful data on health outcomes such as individual health status or other clinical parameters. The best evidence for improved health outcomes was found in the management of pediatric asthma. These studies reported positive effects on treatment compliance and a reduction in the need for acute intervention. This is consistent with previously reported evidence supporting the use of telehealth in the management of chronic conditions.70
Several publications, most on the use of telehealth in dermatology and some that assessed multiple medical specialties, reported a positive impact on process-of-care outcomes, including a reduction in time to consultation, shorter wait times, and less time to perform a consultation. In some cases, the reduction in wait times was significant relative to face-to-face care, decreasing by almost 50%.64 Improved triage facilitated the prioritization of patients on the basis of urgency, thus enhancing workflow logistics. It remains unclear whether triage led to overall faster care or improved health outcomes. It is also unknown whether the expectation of faster and more effective care could be met if asynchronous technology were expanded beyond small pilot projects and feasibility studies.
The results of this scoping review are consistent with previous findings that the methods to assess the cost-effectiveness of telehealth are poor.71 Most evidence for cost savings is implied through indirect reductions in resource utilization. Cost savings in these situations are achieved through the avoidance of patient-generated costs, such as those associated with travel, lost time from work, or caregiver reimbursement. These costs, although not insignificant, are variable and are correlated with travel distance; thus, it could be difficult to demonstrate cost-effectiveness in more urban areas. Other studies reported a decreased frequency or avoidance of patient transfers. This was most notable in the triage of surgical cases in orthopedics and neurosurgery. In these situations, it could be possible to avoid the mobilization of health professionals (e.g., ambulance attendant, nurse, physician).
The quality of literature on patient satisfaction, as in other aspects of telehealth, was considered to be poor.73 Consistent with previous publications, however, satisfaction levels were found to be generally above 80% for the use of telehealth in dermatology, although some studies reported a preference for in-person consultation.45,54 The satisfaction ratings seemed to be influenced by wait times for obtaining traditional in-person care. Provider acceptance was mixed: compared with primary care providers, consultants were more amenable to the use of telehealth in dermatology. The latter group perceived the complexity of the referral process and the increased workload as negative factors. In most of the other clinical domains, however, clinicians reported a positive acceptance of the use of asynchronous telehealth.
Limitations
This scoping review has several limitations. The search of databases was performed in December 2006. Asynchronous telehealth, with its low-cost technology and potential to decrease reliance on scarce resources for real-time consultation, is still rapidly evolving. Systematic reviews must be updated regularly to ensure that our knowledge of asynchronous telehealth is up to date with new evidence.110
The literature search was restricted to English publications. Although there could be reports published in other languages, previous studies have suggested that restricting literature searches to English does not bias systematic reviews of conventional medical interventions.111
The scope of asynchronous telehealth was limited in this review. Specifically, the search strategy focused on the clinical applications of asynchronous telehealth but may not have identified all evaluations of remote home-based monitoring. Better evidence for improved health outcomes appears to originate from this latter body of literature. A review focusing on this area may generate more robust results to support the use of asynchronous telehealth. Additionally, the 10 publications that assessed the use of asynchronous telehealth in pathology and diagnostic radiology were not included in this report. These clinical domains may add information with respect to the benefits of asynchronous telehealth. These publications were eliminated to maintain consistency with other literature on asynchronous telehealth, which generally exclude those medical specialties that traditionally do not involve direct patient care.
Despite repeated calls for improved study designs, methodological quality and standardized outcome assessments, the overall quality of the telehealth literature remains poor. However, although the evidence is weak, there are trends, especially within dermatology, that support the use of asynchronous telehealth as a supplement, rather than as a replacement, for other health services. Specifically, there is consistent evidence suggesting that asynchronous telehealth could lead to shorter wait times, fewer unnecessary referrals, high levels of patient and provider satisfaction, and equivalent (or even better) diagnostic accuracy in comparison with face-to-face consultations.
Acknowledgments
We applied the “first-last” author emphasis approach for the sequence of authors. We are grateful to Marina Englesakis, information specialist, for providing valuable feedback in developing the search strategy and completing searches of the databases; Hammad Durrani (HD) and Cynthia Lokker (CL) for their help in data extraction; Dijana Vasic and Vladan Jovic for their aid in retrieving the articles for this review; and Melissa Ohotski and Jessie Venegas-Garcia for their assistance in preparing citation lists. Martha Garcia, from Foresight Links Corporation, provided management and administrative oversight throughout all phases of the project.
Biographies
Amol Deshpande, MD, MBA, is a consultant with Foresight Links Corporation, Toronto, Ontario, Canada.
Shariq Khoja, MD, PhD, is an assistant professor in the Department of Community Health Sciences and Medical Director’s Office, Aga Khan University, Karachi, Pakistan.
Julio Lorca, MD, is general director of the Institute for Innovation on Human Well-being in Malaga, Andalusia, Spain.
Ann McKibbon, BSc, MLS, PhD, is associate professor (part-time) at the Health Information Research Unit, Faculty of Health Sciences, McMaster University, Hamilton, Ontario.
Carlos Rizo, MD, is a PhD candidate in the Department of Health Policy, Management and Evaluation at the University of Toronto, Toronto, Ontario.
Donald Husereau, BScPharm, MSc, is director of project development at the Canadian Agency for Drugs and Technologies in Health, Ottawa, Ontario.
Alejandro R Jadad, MD, DPhil, FRCPC, is professor, chief innovator and founder of the Centre for Global eHealth Innovation, University Health Network and University of Toronto, Toronto, Ontario.
Appendices
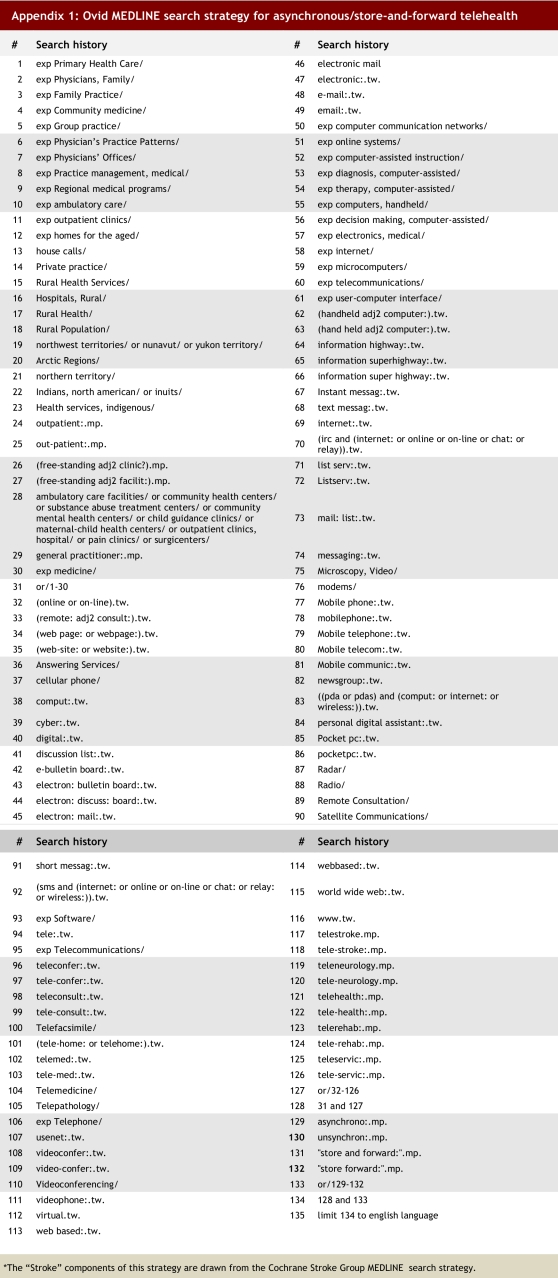
Appendix 1.
Ovid MEDLINE search strategy for asynchronous/store-and-forward telehealth
Appendix 2.
Studies excluded from asynchronous telehealth review
Footnotes
Competing interests: None declared.
Contributors: Amol Deshpande (AD) led the research and coordinated the project, including the design of data extraction tables, supervision of data extraction, confirmation of final selected trials, preparation of initial draft of the review and participation in subsequent report revisions. Alejandro R. Jadad (ARJ) conceived the project, developed the initial protocol, assisted in data extraction and participated in all phases of the writing of the report. Carlos Rizo (CR) extracted and tabulated data for the environmental scan and assisted in report writing. Ann McKibbon (AM) and Shariq Khoja (SK) selected trials and studies, extracted and tabulated data and reviewed the final report. Julio Lorca prepared the initial draft of the asynchronous telehealth environmental scan. Donald Husereau reviewed and provided comments on the research protocol and subsequent drafts. All of the authors contributed to the revisions of the report.
This study was sponsored by the Canadian Agency for Drugs and Technologies in Health, Ottawa, Ont.
References
- 1.Kondro Wayne. Trends in physician supply. CMAJ. 2006;175(11):1362. doi: 10.1503/cmaj.061434. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=17116899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Labour and Business Centre. Physician workforce in Canada: literature review and gap analysis. Final Report. Canadian Labour and Business Centre; 2003. http://www.effectifsmedicaux.ca/reports/literatureReviewGapAnalysis-e.pdf. [Google Scholar]
- 3.Jaatinen Pekka T, Forsström Jari, Loula Pekka. Teleconsultations: who uses them and how. J Telemed Telecare. 2002;8(6):319–324. doi: 10.1258/135763302320939194. [DOI] [PubMed] [Google Scholar]
- 4.Jadad A R, Moore R A, Carroll D, Jenkinson C, Reynolds D J, Gavaghan D J, McQuay H J. Assessing the quality of reports of randomized clinical trials: is blinding necessary. Control Clin Trials. 1996;17(1):1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 5.Downs S H, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52(6):377–384. doi: 10.1136/jech.52.6.377. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=9764259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brouwers Melissa C, Johnston Mary E, Charette Manya L, Hanna Steve E, Jadad Alejandro R, Browman George P. Evaluating the role of quality assessment of primary studies in systematic reviews of cancer practice guidelines. BMC Med Res Methodol. 2005 Feb 16;5(1):8. doi: 10.1186/1471-2288-5-8. http://www.biomedcentral.com/1471-2288/5/8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Desai Sangeeta, Patil Rajasa, Kothari Ashok, Shet Tanuja, Kane Shubhada, Borges Anita, Chinoy Roshni. Static telepathology consultation service between Tata Memorial Centre, Mumbai and Nargis Dutt Memorial Charitable Hospital, Barshi, Solapur, Maharashtra: an analysis of the first 100 cases. Indian J Pathol Microbiol. 2004;47(4):480–485. [PubMed] [Google Scholar]
- 8.Dunn B E, Choi H, Almagro U A, Recla D L, Krupinski E A, Weinstein R S. Routine surgical telepathology in the Department of Veterans Affairs: experience-related improvements in pathologist performance in 2200 cases. Telemed J. 1999;5(4):323–337. doi: 10.1089/107830299311899. [DOI] [PubMed] [Google Scholar]
- 9.Dunn B E, Almagro U A, Choi H, Recla D L, Weinstein R S. Use of telepathology for routine surgical pathology review in a test bed in the Department of Veterans Affairs. Telemed J. 1997;3(1):1–10. doi: 10.1089/tmj.1.1997.3.1. [DOI] [PubMed] [Google Scholar]
- 10.Lanschuetzer C M, Pohla-Gubo G, Schafleitner B, Hametner R, Hashimoto T, Salmhofer W, Bauer J W, Hintner H. Telepathology using immunofluorescence/immunoperoxidase microscopy. J Telemed Telecare. 2004;10(1):39–43. doi: 10.1258/135763304322764185. [DOI] [PubMed] [Google Scholar]
- 11.Marcelo A, Fontelo P, Farolan M, Cualing H. Effect of image compression on telepathology. A randomized clinical trial. Arch Pathol Lab Med. 2000;124(11):1653–1656. doi: 10.5858/2000-124-1653-EOICOT. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=11079019&Code=tu&JrId=758. [DOI] [PubMed] [Google Scholar]
- 12.Settakorn J, Kuakpaetoon T, Leong F J W-M, Thamprasert K, Ichijima K. Store-and-forward diagnostic telepathology of small biopsies by e-mail attachment: a feasibility pilot study with a view for future application in Thailand diagnostic pathology services. Telemed J E Health. 2002;8(3):333–341. doi: 10.1089/15305620260353225. [DOI] [PubMed] [Google Scholar]
- 13.Gómez E J, Caballero P J, Malpica N, del Pozo F. Optimisation and evaluation of an asynchronous transfer mode teleradiology co-operative system: the experience of the EMERALD and the BONAPARTE projects. Comput Methods Programs Biomed. 2001;64(3):201–214. doi: 10.1016/s0169-2607(00)00140-1. [DOI] [PubMed] [Google Scholar]
- 14.Hussain P, Melville D, Mannings R, Curry D, Kay D, Ford P. Evaluation of a training and diagnostic ultrasound service for general practitioners using narrowband ISDN. J Telemed Telecare. 1999;5 Suppl 1:S95–S99. doi: 10.1258/1357633991932757. [DOI] [PubMed] [Google Scholar]
- 15.Johnson M A, Davis P, McEwan A J, Jhangri G S, Warshawski R, Gargum A, Ethier J, Anderson W W. Preliminary findings from a teleultrasound study in Alberta. Telemed J. 1998;4(3):267–276. doi: 10.1089/tmj.1.1998.4.267. [DOI] [PubMed] [Google Scholar]
- 16.Lewis Chris. A tele-ultrasound needs analysis in Queensland. J Telemed Telecare. 2005;11 Suppl 2:S61–S64. doi: 10.1258/135763305775124696. [DOI] [PubMed] [Google Scholar]
- 17.Zelickson B D, Homan L. Teledermatology in the nursing home. Arch Dermatol. 1997;133(2):171–174. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=9041829&Code=tu&JrId=725. [PubMed] [Google Scholar]
- 18.Heautot J F, Gibaud B, Catroux B, Thoreux P H, Cordonnier E, Scarabin J M, Carsin M, Gandon Y. Influence of the teleradiology technology (N-ISDN and ATM) on the inter-hospital management of neurosurgical patients. Med Inform Internet Med. 1999;24(2):121–134. doi: 10.1080/146392399298465. [DOI] [PubMed] [Google Scholar]
- 19.Krupinski E, Webster P, Dolliver M, Weinstein R S, Lopez A M. Efficiency analysis of a multi-specialty telemedicine service. Telemed J. 1999;5(3):265–271. doi: 10.1089/107830299312014. [DOI] [PubMed] [Google Scholar]
- 20.Sibson L, Dunn R, Evans J, Jones R, Hayward M, Wallace S. The virtual mole clinic: preliminary results from the Plymouth skin cancer screening study using telemedicine. Med Inform Internet Med. 1999;24(3):189–199. doi: 10.1080/146392399298393. [DOI] [PubMed] [Google Scholar]
- 21.White H, Gould D, Mills W, Brendish L. The Cornwall dermatology electronic referral and image-transfer project. J Telemed Telecare. 1999;5 Suppl 1:S85–S86. doi: 10.1258/1357633991932694. [DOI] [PubMed] [Google Scholar]
- 22.Pak H S, Welch M, Poropatich R. Web-based teledermatology consult system: preliminary results from the first 100 cases. Stud Health Technol Inform. 1999;64:179–184. [PubMed] [Google Scholar]
- 23.Gomez E, Poropatich R, Karinch M A, Zajtchuk J. Tertiary telemedicine support during global military humanitarian missions. Telemed J. 1996;2(3):201–210. doi: 10.1089/tmj.1.1996.2.201. [DOI] [PubMed] [Google Scholar]
- 24.Abboud Joseph A, Bozentka David J, Beredjiklian Pedro K. Telemedicine consultation for patients with upper extremity disorders is reliable. Clin Orthop Relat Res. 2005;2005(435):250–257. doi: 10.1097/01.blo.0000155009.77961.5c. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=15930947&Code=tu&JrId=3046. [DOI] [PubMed] [Google Scholar]
- 25.Barnard C M, Goldyne M E. Evaluation of an asynchronous teleconsultation system for diagnosis of skin cancer and other skin diseases. Telemed J E Health. 2000;6(4):379–384. doi: 10.1089/15305620050503843. [DOI] [PubMed] [Google Scholar]
- 26.Brandling-Bennett Heather A, Kedar Iris, Pallin Daniel J, Jacques Gary, Gumley Graham J, Kvedar Joseph C. Delivering health care in rural Cambodia via store-and-forward telemedicine: a pilot study. Telemed J E Health. 2005;11(1):56–62. doi: 10.1089/tmj.2005.11.56. [DOI] [PubMed] [Google Scholar]
- 27.Callahan Charles W, Malone Francis, Estroff David, Person Donald A. Effectiveness of an Internet-based store-and-forward telemedicine system for pediatric subspecialty consultation. Arch Pediatr Adolesc Med. 2005;159(4):389–393. doi: 10.1001/archpedi.159.4.389. http://archpedi.ama-assn.org/cgi/pmidlookup?view=long&pmid=15809396. [DOI] [PubMed] [Google Scholar]
- 28.Chan Debora S, Callahan Charles W, Sheets Scott J, Moreno Carol N, Malone Francis J. An Internet-based store-and-forward video home telehealth system for improving asthma outcomes in children. Am J Health Syst Pharm. 2003;60(19):1976–1981. doi: 10.1093/ajhp/60.19.1976. [DOI] [PubMed] [Google Scholar]
- 29.Helveston E M, Orge F H, Naranjo R, Hernandez L. Telemedicine: strabismus e-consultation. J AAPOS. 2001;5(5):291–296. doi: 10.1067/mpa.2001.118214. [DOI] [PubMed] [Google Scholar]
- 30.Hersh William, Miller Robin, Olson Daniel, Sacherek Lynetta, Cross Ping. Professional’s Information Link (PiL): a web-based asynchronous consultation service. Proc AMIA Symp. 2002:325–329. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=12463840. [PMC free article] [PubMed] [Google Scholar]
- 31.Kokesh John, Ferguson A Stewart, Patricoski Chris. Telehealth in Alaska: delivery of health care services from a specialist’s perspective. Int J Circumpolar Health. 2004;63(4):387–400. doi: 10.3402/ijch.v63i4.17756. [DOI] [PubMed] [Google Scholar]
- 32.Krupinski Elizabeth A, Engstrom Mike, Barker Gail, Levine Norman, Weinstein Ronald S. The challenges of following patients and assessing outcomes in teledermatology. J Telemed Telecare. 2004;10(1):21–24. doi: 10.1258/135763304322764149. [DOI] [PubMed] [Google Scholar]
- 33.Lau Christopher, Churchill R Sean, Kim Janice, Matsen Frederick A, Kim Yongmin. Asynchronous web-based patient-centered home telemedicine system. IEEE Trans Biomed Eng. 2002;49(12):1452–1462. doi: 10.1109/TBME.2002.805456. [DOI] [PubMed] [Google Scholar]
- 34.Malone Francis, Callahan Charles W, Chan Debora S, Sheets Scott, Person Donald A. Caring for children with asthma through teleconsultation: “ECHO-Pac, The Electronic Children’s Hospital of the Pacific”. Telemed J E Health. 2004;10(2):138–146. doi: 10.1089/tmj.2004.10.138. [DOI] [PubMed] [Google Scholar]
- 35.McConnochie Kenneth M, Wood Nancy E, Kitzman Harriet J, Herendeen Neil E, Roy Jason, Roghmann Klaus J. Telemedicine reduces absence resulting from illness in urban child care: evaluation of an innovation. Pediatrics. 2005;115(5):1273–1282. doi: 10.1542/peds.2004-0335. http://pediatrics.aappublications.org/cgi/pmidlookup?view=long&pmid=15867035. [DOI] [PubMed] [Google Scholar]
- 36.Mukundan Srinivasan, Vydareny Kay, Vassallo David J, Irving Simon, Ogaoga Divi. Trial telemedicine system for supporting medical students on elective in the developing world. Acad Radiol. 2003;10(7):794–797. doi: 10.1016/s1076-6332(03)80125-3. [DOI] [PubMed] [Google Scholar]
- 37.Pap Stephen A, Lach Elliot, Upton Joseph. Telemedicine in plastic surgery: E-consult the attending surgeon. Plast Reconstr Surg. 2002;110(2):452–456. doi: 10.1097/00006534-200208000-00012. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=12142659&Code=tu&JrId=6482. [DOI] [PubMed] [Google Scholar]
- 38.Person Donald A, Hedson Johnny S, Gunawardane Kamal J. Telemedicine success in the United States Associated Pacific Islands (USAPI): two illustrative cases. Telemed J E Health. 2003;9(1):95–101. doi: 10.1089/153056203763317701. [DOI] [PubMed] [Google Scholar]
- 39.Person D A. Pacific Island Health Care Project: early experiences with a Web-based consultation and referral network. Pac Health Dialog. 2000;7(2):29–35. [PubMed] [Google Scholar]
- 40.Weinstock Martin A, Nguyen Farrah Q, Risica Patricia M. Patient and referring provider satisfaction with teledermatology. J Am Acad Dermatol. 2002;47(1):68–72. doi: 10.1067/mjd.2002.119666. [DOI] [PubMed] [Google Scholar]
- 41.Whited John D, Hall Russell P, Foy Marjorie E, Marbrey Laurie E, Grambow Steven C, Dudley Tara K, Datta Santanu, Simel David L, Oddone Eugene Z. Teledermatology’s impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health. 2002;8(3):313–321. doi: 10.1089/15305620260353207. [DOI] [PubMed] [Google Scholar]
- 42.Archbold H A P, Guha A R, Shyamsundar S, McBride S J, Charlwood P, Wray R. The use of multi-media messaging in the referral of musculoskeletal limb injuries to a tertiary trauma unit using: a 1-month evaluation. Injury. 2005;36(4):560–566. doi: 10.1016/j.injury.2004.08.027. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=15755440&Code=tu&JrId=4255. [DOI] [PubMed] [Google Scholar]
- 43.Beach M, Goodall I, Miller P. Evaluating telemedicine for minor injuries units. J Telemed Telecare. 2000;6 Suppl 1:S90–S92. doi: 10.1258/1357633001934276. [DOI] [PubMed] [Google Scholar]
- 44.Collins K, Nicolson P, Bowns I, Walters S. General practitioners’ perceptions of store-and-forward teledermatology. J Telemed Telecare. 2000;6(1):50–53. doi: 10.1258/1357633001933844. [DOI] [PubMed] [Google Scholar]
- 45.Collins Karen, Walters Stephen, Bowns Ian. Patient satisfaction with teledermatology: quantitative and qualitative results from a randomized controlled trial. J Telemed Telecare. 2004;10(1):29–33. doi: 10.1258/135763304322764167. [DOI] [PubMed] [Google Scholar]
- 46.Collins Karen, Bowns Ian, Walters Stephen. General practitioners’ perceptions of asynchronous telemedicine in a randomized controlled trial of teledermatology. J Telemed Telecare. 2004;10(2):94–8. doi: 10.1258/135763304773391530. [DOI] [PubMed] [Google Scholar]
- 47.Loane M A, Bloomer S E, Corbett R, Eedy D J, Hicks N, Lotery H E, Mathews C, Paisley J, Steele K, Wootton R. A randomized controlled trial to assess the clinical effectiveness of both realtime and store-and-forward teledermatology compared with conventional care. J Telemed Telecare. 2000;6 Suppl 1:S1–3. doi: 10.1258/1357633001933952. [DOI] [PubMed] [Google Scholar]
- 48.Mahendran R, Goodfield M J D, Sheehan-Dare R A. An evaluation of the role of a store-and-forward teledermatology system in skin cancer diagnosis and management. Clin Exp Dermatol. 2005;30(3):209–214. doi: 10.1111/j.1365-2230.2005.01735.x. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=15807671&Code=tu&JrId=3011. [DOI] [PubMed] [Google Scholar]
- 49.Mallett R B. Teledermatology in practice. Clin Exp Dermatol. 2003;28(4):356–359. doi: 10.1046/j.1365-2230.2003.01313.x. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=12823290&Code=tu&JrId=3011. [DOI] [PubMed] [Google Scholar]
- 50.Mandall N A, O’Brien K D, Brady J, Worthington H V, Harvey L. Teledentistry for screening new patient orthodontic referrals. Part 1: A randomised controlled trial. Br Dent J. 2005;199(10):659–662. doi: 10.1038/sj.bdj.4812930. discussion 653 http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=16311569&Code=tu&JrId=1712. [DOI] [PubMed] [Google Scholar]
- 51.Patterson V, Hoque F, Vassallo D, Farquharson Roberts M, Swinfen P, Swinfen R. Store-and-forward teleneurology in developing countries. J Telemed Telecare. 2001;7 Suppl 1:52–53. doi: 10.1177/1357633X010070S121. [DOI] [PubMed] [Google Scholar]
- 52.Taylor P, Goldsmith P, Murray K, Harris D, Barkley A. Evaluating a telemedicine system to assist in the management of dermatology referrals. Br J Dermatol. 2001;144(2):328–333. doi: 10.1046/j.1365-2133.2001.04023.x. [DOI] [PubMed] [Google Scholar]
- 53.Vassallo D J, Hoque F, Roberts M F, Patterson V, Swinfen P, Swinfen R. An evaluation of the first year’s experience with a low-cost telemedicine link in Bangladesh. J Telemed Telecare. 2001;7(3):125–138. doi: 10.1258/1357633011936273. [DOI] [PubMed] [Google Scholar]
- 54.Williams T, May C, Esmail A, Ellis N, Griffiths C, Stewart E, Fitzgerald D, Morgan M, Mould M, Pickup L, Kelly S. Patient satisfaction with store-and-forward teledermatology. J Telemed Telecare. 2001;7 Suppl 1:45–46. doi: 10.1177/1357633X010070S118. [DOI] [PubMed] [Google Scholar]
- 55.Baruffaldi F, Gualdrini G, Toni A. Comparison of asynchronous and realtime teleconsulting for orthopaedic second opinions. J Telemed Telecare. 2002;8(5):297–301. doi: 10.1258/135763302760314270. [DOI] [PubMed] [Google Scholar]
- 56.Larcher B, Arisi E, Berloffa F, Demichelis F, Eccher C, Galligioni E, Galvagni M, Martini G, Sboner A, Tomio L, Zumiani G, Graiff A, Forti S. Analysis of user-satisfaction with the use of a teleconsultation system in oncology. Med Inform Internet Med. 2003;28(2):73–84. doi: 10.1080/14639230310000600470. [DOI] [PubMed] [Google Scholar]
- 57.Malacarne Mara, Lesma Alessandro, Madera Angelo, Malfatti Eugenio, Castelli Alberto, Lucini Daniela, Pizzinelli Paolo, Pagani Massimo. Preliminary experience of shared clinical management between Milan and Pointe Noire using the INteractive TeleConsultation Network for Worldwide HealthcAre Services (INCAS): telemedicine between Milan and Africa. Telemed J E Health. 2004;10(4):437–443. doi: 10.1089/tmj.2004.10.437. [DOI] [PubMed] [Google Scholar]
- 58.Eminović N, Witkamp L, Ravelli A C J, Bos J D, van den Akker TW, Bousema M T, Henquet C J M, Koopman R J J, Zeegelaar J E, Wyatt J C. Potential effect of patient-assisted teledermatology on outpatient referral rates. J Telemed Telecare. 2003;9(6):321–327. doi: 10.1258/135763303771005216. [DOI] [PubMed] [Google Scholar]
- 59.Knol A, van den Akker TW, Damstra R J, de Haan J. Teledermatology reduces the number of patient referrals to a dermatologist. J Telemed Telecare. 2006;12(2):75–78. doi: 10.1258/135763306776084365. [DOI] [PubMed] [Google Scholar]
- 60.Fortin Jean-Paul, Gagnon Marie-Pierre, Cloutier Alain, Labbé Françoise. Evaluation of a telemedicine demonstration project in the Magdalene Islands. J Telemed Telecare. 2003;9(2):89–94. doi: 10.1258/135763303321327948. [DOI] [PubMed] [Google Scholar]
- 61.Vladzymyrskyy Anton V. Four years’ experience of teleconsultations in daily clinical practice. J Telemed Telecare. 2005;11(6):294–297. doi: 10.1258/1357633054893337. [DOI] [PubMed] [Google Scholar]
- 62.Chen Li-Sheng, Tsai Ching-Yao, Liu Tzeng-Ying, Tung Tao-Hsin, Chiu Yueh-Hsia, Chan Chang-Chuan, Liou Der-Ming, Chen Tony Hsiu-Hsi. Feasibility of tele-ophthalmology for screening for eye disease in remote communities. J Telemed Telecare. 2004;10(6):337–341. doi: 10.1258/1357633042602035. [DOI] [PubMed] [Google Scholar]
- 63.Baba Mete, Seçkin Deniz, Kapdağli Serhan. A comparison of teledermatology using store-and-forward methodology alone, and in combination with Web camera videoconferencing. J Telemed Telecare. 2005;11(7):354–360. doi: 10.1258/135763305774472097. [DOI] [PubMed] [Google Scholar]
- 64.Klaz Itay, Wohl Yonit, Nathansohn Nir, Yerushalmi Nir, Sharvit Sharon, Kochba Ilan, Brenner Sarah. Teledermatology: quality assessment by user satisfaction and clinical efficiency. Isr Med Assoc J. 2005;7(8):487–490. http://www.ima.org.il/imaj/dynamic/web/ArtFromPubmed.asp?year=2005&month=08&page=487. [PubMed] [Google Scholar]
- 65.Moreno-Ramirez D, Ferrandiz L, Galdeano R, Camacho F M. Teledermatoscopy as a triage system for pigmented lesions: a pilot study. Clin Exp Dermatol. 2006;31(1):13–18. doi: 10.1111/j.1365-2230.2005.02000.x. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=16309470&Code=tu&JrId=3011. [DOI] [PubMed] [Google Scholar]
- 66.Hockey A D, Wootton R, Casey T. Trial of low-cost teledermatology in primary care. J Telemed Telecare. 2004;10 Suppl 1:44–47. doi: 10.1258/1357633042614221. [DOI] [PubMed] [Google Scholar]
- 67.Massone C, Soyer H P, Hofmann-Wellenhof R, Di Stefani A, Lozzi G P, Gabler G, Dong H, Argenziano G, Ozdemir F, Fink-Puches R, Salmhofer W, Zalaudek I, Nunzi E, Kerl H. Two years’ experience with Web-based teleconsulting in dermatology. J Telemed Telecare. 2006;12(2):83–87. doi: 10.1258/135763306776084419. [DOI] [PubMed] [Google Scholar]
- 68.Loane M A, Bloomer S E, Corbett R, Eedy D J, Hicks N, Lotery H E, Mathews C, Paisley J, Steele K, Wootton R. A comparison of real-time and store-and-forward teledermatology: a cost-benefit study. Br J Dermatol. 2000;143(6):1241–1247. doi: 10.1046/j.1365-2133.2000.03895.x. [DOI] [PubMed] [Google Scholar]
- 69.Whited John D, Datta Santanu, Hall Russell P, Foy Marjorie E, Marbrey Laurie E, Grambow Steven C, Dudley Tara K, Simel David L, Oddone Eugene Z. An economic analysis of a store and forward teledermatology consult system. Telemed J E Health. 2003;9(4):351–360. doi: 10.1089/153056203772744671. [DOI] [PubMed] [Google Scholar]
- 70.Hersh William R, Hickam David H, Severance Susan M, Dana Tracy L, Krages Kathryn Pyle, Helfand Mark. Telemedicine for the Medicare Population: Update. Rockville (MD): Agency for Healthcare Research and Quality; 2006. Publication No. 06-E007. [PMC free article] [PubMed] [Google Scholar]
- 71.Whitten Pamela S, Mair Frances S, Haycox Alan, May Carl R, Williams Tracy L, Hellmich Seth. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ. 2002;324(7351):1434–1437. doi: 10.1136/bmj.324.7351.1434. http://bmj.com/cgi/pmidlookup?view=long&pmid=12065269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roine R, Ohinmaa A, Hailey D. Assessing telemedicine: a systematic review of the literature. CMAJ. 2001;165(6):765–771. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=11584564. [PMC free article] [PubMed] [Google Scholar]
- 73.Williams T L, May C R, Esmail A. Limitations of patient satisfaction studies in telehealthcare: a systematic review of the literature. Telemed J E Health. 2001;7(4):293–316. doi: 10.1089/15305620152814700. [DOI] [PubMed] [Google Scholar]
- 74.Burgess L P, Holtel M R, Syms M J, Birkmire-Peters D P, Peters L J, Mashima P A. Overview of telemedicine applications for otolaryngology. Laryngoscope. 1999;109(9):1433–1437. doi: 10.1097/00005537-199909000-00014. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=10499050&Code=tu&JrId=5476. [DOI] [PubMed] [Google Scholar]
- 75.Hill Anne J, Theodoros Deborah G, Russell Trevor G, Cahill Louise M, Ward Elizabeth C, Clark Kathy M. An Internet-based telerehabilitation system for the assessment of motor speech disorders: a pilot study. Am J Speech Lang Pathol. 2006;15(1):45–56. doi: 10.1044/1058-0360(2006/006. [DOI] [PubMed] [Google Scholar]
- 76.Houston M S, Myers J D, Levens S P, McEvoy M T, Smith S A, Khandheria B K, Shen W K, Torchia M E, Berry D J. Clinical consultations using store-and-forward telemedicine technology. Mayo Clin Proc. 1999;74(8):764–769. doi: 10.4065/74.8.764. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=10473351&Code=tu&JrId=5565. [DOI] [PubMed] [Google Scholar]
- 77.Jones SM, Milroy C, Pickford MA. Telemedicine in acute plastic surgical trauma and burns. Ann R Coll Surg Engl. 2004;86(4):239–242. doi: 10.1308/147870804344. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15239862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lattimore M R. A store-forward ophthalmic telemedicine case report from deployed U. S. Army forces in Kuwait. Telemed J. 1999;5(3):309–313. doi: 10.1089/107830299312069. [DOI] [PubMed] [Google Scholar]
- 79.Minervini M I, Yagi Y, Marino I R, Lawson A, Nalesnik M, Randhawa P, Wu T, Fung J J, Demetris A. Development and experience with an integrated system for transplantation telepathology. Hum Pathol. 2001;32(12):1334–1343. doi: 10.1053/hupa.2001.29655. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=11774166&Code=tu&JrId=4136. [DOI] [PubMed] [Google Scholar]
- 80.Piccolo D, Soyer H Peter, Burgdorf W, Talamini R, Peris K, Bugatti L, Canzonieri V, Cerroni L, Chimenti S, De Rosa G, Filosa G, Hoffmann R, Julis I, Kutzner H, Manente L, Misciali C, Schaeppi H, Tanaka M, Tyler W, Zelger B, Kerl H. Concordance between telepathologic diagnosis and conventional histopathologic diagnosis: a multiobserver store-and-forward study on 20 skin specimens. Arch Dermatol. 2002;138(1):53–58. doi: 10.1001/archderm.138.1.53. http://archderm.ama-assn.org/cgi/pmidlookup?view=long&pmid=11790167. [DOI] [PubMed] [Google Scholar]
- 81.Szot Agnieszka, Jacobson Francine L, Munn Samson, Jazayeri Darius, Nardell Edward, Harrison David, Drosten Ralph, Ohno-Machado Lucila, Smeaton Laura M, Fraser Hamish S F. Diagnostic accuracy of chest X-rays acquired using a digital camera for low-cost teleradiology. Int J Med Inform. 2004;73(1):65–73. doi: 10.1016/j.ijmedinf.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 82.Sclafani A P, Heneghan C, Ginsburg J, Sabini P, Stern J, Dolitsky J N. Teleconsultation in otolaryngology: live versus store and forward consultations. Otolaryngol Head Neck Surg. 1999;120(1):62–72. doi: 10.1016/S0194-5998(99)70371-2. [DOI] [PubMed] [Google Scholar]
- 83.Duerinckx A J, Hayrapetian A, Melany M, Valentino D J, Rahbar D, Kiszonas M, Franco R, Narin S L, Ragavendra N, Grant E G. Real-time sonographic video transfer using asynchronous transfer mode technology. AJR Am J Roentgenol. 1997;168(5):1353–1355. doi: 10.2214/ajr.168.5.9129443. http://www.ajronline.org/cgi/pmidlookup?view=long&pmid=9129443. [DOI] [PubMed] [Google Scholar]
- 84.Kanzaki Hatsumi, Makimoto Kiyoko, Takemura Tadamasa, Ashida Nobuyuki. Development of web-based qualitative and quantitative data collection systems: study on daily symptoms and coping strategies among Japanese rheumatoid arthritis patients. Nurs Health Sci. 2004;6(3):229–236. doi: 10.1111/j.1442-2018.2004.00195.x. [DOI] [PubMed] [Google Scholar]
- 85.Sibson L. The Plymouth experience: skin cancer screening using a store and forward telemedicine system. ITIN. 2000;12(1):6–9. [Google Scholar]
- 86.Demiris George, Speedie Stuart M, Hicks Lanis L. Assessment of patients’ acceptance of and satisfaction with teledermatology. J Med Syst. 2004;28(6):575–579. doi: 10.1023/b:joms.0000044959.71456.df. [DOI] [PubMed] [Google Scholar]
- 87.Leong F J. Practical applications of Internet resources for cost-effective telepathology practice. Pathology. 2001;33(4):498–503. doi: 10.1080/00313020127147. [DOI] [PubMed] [Google Scholar]
- 88.Oakley A M. Teledermatology in New Zealand. J Cutan Med Surg. 2001 Mar 02;5(2):111–116. doi: 10.1007/s102270000011. [DOI] [PubMed] [Google Scholar]
- 89.Umefjord Göran, Malker Hans, Olofsson Niclas, Hensjö Lars-Olof, Petersson Göran. Primary care physicians’ experiences of carrying out consultations on the internet. Inform Prim Care. 2004;12(2):85–90. doi: 10.14236/jhi.v12i2.112. [DOI] [PubMed] [Google Scholar]
- 90.Whitten Pamela S. Teledermatology delivery modalities: real time versus store and forward. Curr Probl Dermatol. 2003;32:24–31. doi: 10.1159/000067353. [DOI] [PubMed] [Google Scholar]
- 91.Blum A, Hofmann-Wellenhof R, Luedtke H, Ellwanger U, Steins A, Roehm S, Garbe C, Soyer H P. Value of the clinical history for different users of dermoscopy compared with results of digital image analysis. J Eur Acad Dermatol Venereol. 2004;18(6):665–669. doi: 10.1111/j.1468-3083.2004.01044.x. [DOI] [PubMed] [Google Scholar]
- 92.Chang Su-Wen, Plotkin Daniel R, Mulligan Roseann, Polido José C, Mah James K, Meara John G. Teledentistry in rural California: a USC initiative. J Calif Dent Assoc. 2003;31(8):601–608. [PubMed] [Google Scholar]
- 93.Dunn B E, Choi H, Almagro U A, Recla D L. Combined robotic and nonrobotic telepathology as an integral service component of a geographically dispersed laboratory network. Hum Pathol. 2001;32(12):1300–1303. doi: 10.1053/hupa.2001.29644 . http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=11774160&Code=tu&JrId=4136. [DOI] [PubMed] [Google Scholar]
- 94.Gilbert B K, Mitchell M P, Bengali A R, Khandheria B K. NASA/DARPA advanced communications technology satellite project for evaluation of telemedicine outreach using next-generation communications satellite technology: Mayo Foundation participation. Mayo Clin Proc. 1999;74(8):753–7. doi: 10.4065/74.8.753. http://www.ncbi.nlm.nih.gov/projects/linkout/nsh/nsh_display.cgi?PrId=5914&PmId=10473349&Code=tu&JrId=5565. [DOI] [PubMed] [Google Scholar]
- 95.Krumm M, Ribera J, Schmiedge G. Using a telehealth medium for objective hearing testing: implications for supporting rural universal newborn hearing screeining program. Semin Hear. 2005;26(1):3–12. [Google Scholar]
- 96.Person Donald A. The Pacific Island Health Care Project: easing the cancer burden in the United States associated Pacific Islands. Pac Health Dialog. 2004;11(2):243–247. [PubMed] [Google Scholar]
- 97.Sanchez Dils E, Lefebvre C, Abeyta K. Teledentistry in the United States: a new horizon of dental care. Int J Dent Hyg. 2004;2(4):161–164. doi: 10.1111/j.1601-5037.2004.00093.x. [DOI] [PubMed] [Google Scholar]
- 98.Sood S P, Bhatia J S. Development of telemedicine technology in India: “Sanjeevani” — an integrated telemedicine application. J Postgrad Med. 2005;51(4):308–311. http://www.jpgmonline.com/article.asp?issn=0022-3859;year=2005;volume=51;issue=4;spage=308;epage=311;aulast=Sood. [PubMed] [Google Scholar]
- 99.Sussmann H, Griebel H, Allescher H D, Egger K, Sandschin W, Horsch A. The teleconsultation service ENDOTEL. Implementation and first experiences. Stud Health Technol Inform. 2000;77:1117–1121. [PubMed] [Google Scholar]
- 100.Munir Jamalah A, Soh Eugene K, Hoffmann Thomas N, Stewart Jeffery P. A novel approach to tele-echocardiography across the Pacific. Hawaii Med J. 2004;63(10):310–313. [PubMed] [Google Scholar]
- 101.Weinstock M A, Kempton S A. Case report: teledermatology and epiluminescence microscopy for the diagnosis of scabies. Cutis. 2000;66(1):61–62. [PubMed] [Google Scholar]
- 102.Whited John D, Hall Russell P, Foy Marjorie E, Marbrey Laurie E, Grambow Steven C, Dudley Tara K, Datta Santanu K, Simel David L, Oddone Eugene Z. Patient and clinician satisfaction with a store-and-forward teledermatology consult system. Telemed J E Health. 2004;10(4):422–431. doi: 10.1089/tmj.2004.10.422. [DOI] [PubMed] [Google Scholar]
- 103.Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2000;2000(2) doi: 10.1002/14651858.CD002098. [DOI] [PubMed] [Google Scholar]
- 104.Whited John D. Teledermatology research review. Int J Dermatol. 2006;45(3):220–229. doi: 10.1111/j.1365-4632.2004.02427.x. [DOI] [PubMed] [Google Scholar]
- 105.Desai Sangeeta, Patil Rajasa, Chinoy Roshni, Kothari Ashok, Ghosh T K, Chavan Manoj, Mohan Ashok, Nene B M, Dinshaw K A. Experience with telepathology at a tertiary cancer centre and a rural cancer hospital. Natl Med J India. 2004;17(1):17–19. [PubMed] [Google Scholar]
- 106.Kuo R L, Aslan P, Dinlenc C Z, Lee B R, Screnci D, Babayan R K, Kavoussi L R, Preminger G M. Secure transmission of urologic images and records over the Internet. J Endourol. 1999;13(3):141–146. doi: 10.1089/end.1999.13.141. [DOI] [PubMed] [Google Scholar]
- 107.Mallett RB. Teledermatology in practice: the Peterborough experience. Brit J Healthc Comp. 2000;17(5):14–17. [Google Scholar]
- 108.Pavlicek W, Zavalkovskiy B, Eversman W G. Performance and function of a high-speed multiple star topology image management system at Mayo Clinic Scottsdale. J Digit Imaging. 1999;12(2 Suppl 1):168–174. doi: 10.1007/BF03168791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rodas Edgar, Mora Francisco, Tamariz Francisco, Cone Stephen W, Merrell Ronald C. Low-bandwidth telemedicine for pre- and postoperative evaluation in mobile surgical services. J Telemed Telecare. 2005;11(4):191–193. doi: 10.1258/1357633054068919. [DOI] [PubMed] [Google Scholar]
- 110.Shojania Kaveh G, Sampson Margaret, Ansari Mohammed T, Ji Jun, Doucette Steve, Moher David. How quickly do systematic reviews go out of date? A survival analysis. Ann Intern Med. 2007 Jul 16;147(4):224–233. doi: 10.7326/0003-4819-147-4-200708210-00179. http://www.annals.org/cgi/pmidlookup?view=long&pmid=17638714. [DOI] [PubMed] [Google Scholar]
- 111.Moher D, Pham B, Lawson M L, Klassen T P. The inclusion of reports of randomised trials published in languages other than English in systematic reviews. Health Technol Assess. 2003;7(41):1–90. doi: 10.3310/hta7410. http://www.hta.ac.uk/execsumm/summ741.htm. [DOI] [PubMed] [Google Scholar]