Abstract
Background
Previous studies have suggested that psychological interventions may be effective in reducing blood pressure. Using rigorous methodology and 24-hour monitoring of ambulatory blood pressure, we compared 2 psychological interventions with treatment using a first-line antihypertensive drug in terms of their efficacy in lowering blood pressure in patients with mild primary hypertension.
Methods
In this prospective, open-label randomized controlled trial (RCT), 65 adult patients with mild, uncomplicated hypertension were randomly assigned to receive one of the following interventions for 12 weeks: (1) pharmacotherapy with hydrochlorothiazide 12.5 titrated to 25 mg/d ; (2) individualized behavioural psychotherapy, consisting of ten 1-hour sessions of stress reduction training with a psychologist; or (3) self-help psychotherapy, consisting of a 1.5-hour session with a psychologist and then daily sessions that involved reading a self-help manual and listening to an audiotape. The primary outcome measure was mean change in ambulatory blood pressure from baseline to week 12. Resting blood pressure readings were taken in the clinic, and adverse events were recorded.
Results
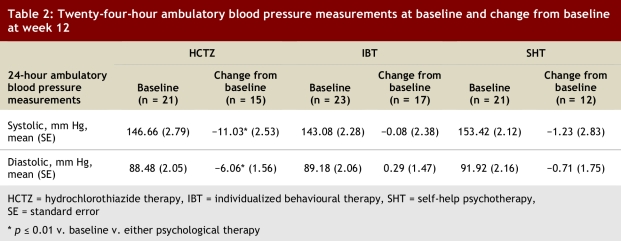
Monitoring of ambulatory blood pressure over 24 hours showed that hydrochlorothiazide therapy significantly reduced both systolic and diastolic blood pressure relative to baseline, and that this reduction was significantly greater than that achieved with either individualized behavioural psychotherapy or self-help psychotherapy (mean reduction [standard error; SE] −11.03 [2.53] / −6.06 [1.56] mm Hg v. −0.08 [2.38] / 0.29 [1.47] mm Hg v. −1.23 [2.83] / −0.71 [1.75] mm Hg, respectively; p = 0.01). Neither form of psychological therapy significantly lowered 24-hour ambulatory blood pressure relative to baseline.
Conclusion
For patients with primary elevated blood pressure, 2 psychological interventions did not lower 24-hour ambulatory blood pressure, whereas hydrochlorothiazide reduced blood pressure, as expected. The findings of this RCT represent an important addition to the evidence for health care practitioners and for patients seeking psychological interventions to reduce blood pressure.
Patients with mild primary hypertension have a number of options to help lower their blood pressure. Non-pharmacological options include the DASH (Dietary Approaches to Stop Hypertension) diet,1 a low-sodium diet,2 exercise,3 weight loss4 and relaxation therapies.5 Relaxation therapies are based on the supposition that psychological stress may contribute to the elevation of blood pressure in some patients.6,7 Others have suggested possible links between stress and hypertension are elevated sympathetic tone or vagal dysregulation.6,8 Several systematic reviews have evaluated the efficacy of diverse psychological and relaxation therapies in reducing blood pressure in patients with primary hypertension as compared to no therapy or sham therapy.5,9-13 However, these studies have yielded conflicting results.
It remains important to determine whether psychological interventions lower blood pressure and the magnitude of the effect, if any, as many patients might prefer this form of therapy over drug therapy if both were equally efficacious. We were therefore interested in evaluating the efficacy of 2 psychological interventions in lowering blood pressure: an individualized program of behavioural therapy and a self-help program of psychological therapy.
With the objective of rigorously assessing the effects of these 2 psychological interventions, we compared them with pharmacotherapy using a thiazide, a first-line drug commonly used in the treatment of mild primary hypertension. A large body of evidence from randomized controlled trials (RCTs) shows that thiazides reduce blood pressure and quantifies the magnitude of their short-term effect on systolic and diastolic blood pressure as about 9/4 mm Hg.14 There is considerable value in using a drug with a known effect as a positive control for a study such as this one. As far as we know, no previous RCTs have directly compared psychological interventions with a drug therapy control.
Methods
Design
Prospective, open-label, randomized controlled trial.
Setting and participants
Adult patients (aged 18 years or older) from the community, with mild hypertension defined as resting systolic blood pressureof 140 mm Hg or above and/or diastolic blood pressureof 90 mm Hg or above, were eligible. Patients were excluded if they had cardiovascular complications or any suspected medical condition that might lead to an unacceptable risk of complications resulting from uncontrolled hypertension during the study period. Patients whose hypertension was uncontrolled while they were taking medication (systolic blood pressure ≥ 170 mm Hg or diastolic blood pressure ≥ 100 mm Hg) or who had excessively high blood pressure while they were not taking any medication (≥ 180/110 mm Hg) were also excluded. Patients with suspected secondary hypertension were excluded, as were those who were pregnant or anticipated being pregnant and those with a history of allergy to, hypersensitivity to, or intolerance of thiazides. Participants were encouraged not to adopt any other changes in lifestyle, diet or exercise during the trial.
Protocol
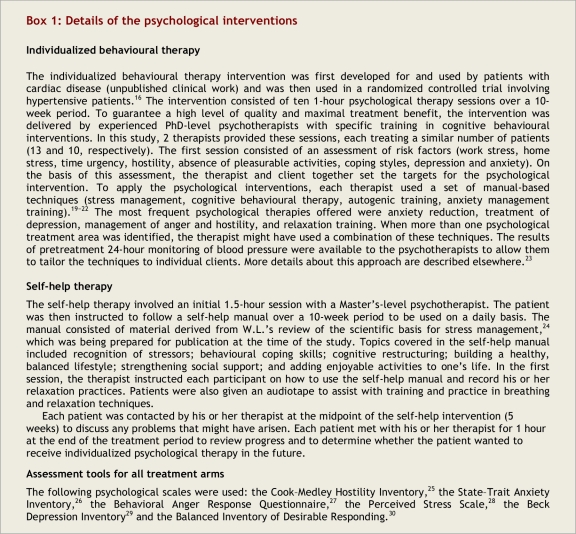
Patients who were taking medication at the time of initial screening underwent a washout period of 3–5 weeks. Patients who met the inclusion criteria and whose off-treatment baseline resting systolic blood pressure in clinic was 140 mm Hg or above or whose resting diastolic blood pressure was 90 mm Hg or above were randomly assigned to receive 1 of the following interventions for 12 weeks: (1) hydrochlorothiazide 12.5 mg/d initially and then 25 mg/d if systolic blood pressure was 140 mm Hg or above or diastolic blood pressure was 90 mm Hg or above after 4 weeks of treatment; (2) individualized behavioural psychotherapy consisting of ten 1-hour sessions with a psychologist; (3) self-help psychological therapy, consisting of an initial 1.5-hour meeting with a psychologist and then daily sessions that involved reading a self-help manual and listening to an audiotape. Both of the psychological treatments entailed learning relaxation, biofeedback and stress management. Details of these psychological forms of management are presented in Box 1. Concealment of allocation was achieved by centralized randomization conducted via telephone by the Cochrane Hypertension Review Group coordinator at the University of British Columbia. This person was blinded to patients’ identification and to characteristics other than sex and previous use of antihypertensive drugs. Information about these 2 characteristics was needed to allow block randomization. The study protocol was reviewed and approved by the institutional ethical review board at the University of British Columbia (UBC). Written informed consent was obtained from all patients.
Box 1.
Details of the psychological interventions
Recruitment, clinical evaluation and follow-up
Participants were recruited by means of newspaper advertising and/or referral by health care practitioners or friends. This recruitment was coordinated by UBC's Behavioural Cardiology Laboratory (BCL). Patients who had not previously been receiving antihypertensive drugs but who exhibited elevated blood pressure at the BCL were sent to the hypertension medical clinic for confirmation of eligibility. Patients who were already taking antihypertensive drugs were seen at the laboratory and were then sent to the clinic, where blood pressure was measured before and after washout, with the possibility of a third post-washout check in the event of borderline blood pressure readings. All of these potential participants provided a medical history and underwent a physical examination. A specific laboratory assessment was ordered if considered necessary. After enrolment, the patients attended the clinic every 4 weeks. At each visit, resting blood pressure was measured. All resting blood pressure measurements were reported as the average of 5 readings, separated by 1-minute intervals, with the first reading after 5 minutes of rest. The patient was in a seated position and the examiner was out of the room during the readings, which were obtained with an automatic device that concealed the measurements from the patient (oscillometric VSM-100 automated blood pressure machine-VSM MedTech Ltd., Vancouver, BC, Canada15). This rigorous methodology was intended to prevent any bias in the blood pressure measurements. True blinding of the patients and investigators was not feasible in view of the type of interventions in this study. At week 7, serum levels of potassium were checked for all of the patients who had been randomly assigned to receive hydrochlorothiazide, to detect hypokalemia, if present, and to allow the prescription of a potassium-sparing diuretic if required. Patients were instructed to report to the clinic immediately if they experienced any unusual symptoms during the study.
Before treatment of any kind, each patient underwent 24-hour monitoring of ambulatory blood pressure, by means of the Spacelabs Medical ambulatory blood pressure monitor (model 90207, Spacelabs Inc, Redmond, Washington, USA). For this monitoring, blood pressure was recorded at 20-minute intervals between 8:00 a.m. and 8:00 p.m. (for daytime measurements) and at 1-hour intervals between 8:00 p.m. and 8:00 a.m. (for nighttime measurements). The monitoring was repeated 12 weeks later (i.e., at the end of the study).
Outcome measures
The primary outcome measure was the mean change in ambulatory blood pressure from baseline to week 12. The secondary outcome measure was the mean change in resting clinic blood pressure, over 12 weeks of treatment. All adverse events, regardless of their nature, were documented, reviewed and reported to the ethics committee.
Statistical analysis
The calculation of the sample size was based on a previous study,16 in which there was a 7 mm Hg (standard deviation 11 mm Hg) difference in systolic pressure between individualized behavioural psychotherapy and no treatment. We calculated that a sample size of 40 patients per treatment arm would provide 80% power at the α = 0.05 level for detection of the above-mentioned difference in blood pressure. However, because of the potential for dropouts, the desired sample size was increased to 50 patients per treatment arm. The efficacy end-points were analyzed according to the intention-to-treat principle. All statistical analyses were performed using the statistical package NCSS 2007 (LLC, Kaysville, Utah, USA). Paired Student’s t test was used to compare variables with continuous data before and after treatment within each group. Treatment groups were compared by analysis of variance using the general linear model approach for repeated measurements and Tukey’s test for multiple comparisons. Using baseline values as covariates, analysis of covariance (ANCOVA) was also performed. A p value less than 0.05 was considered statistically significant.
Results
Study population
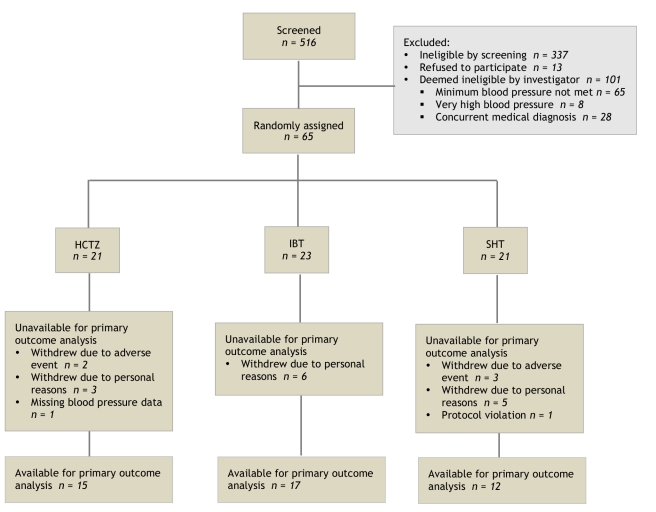
Recruitment for this single-centre study began in March 2002 and ended in May 2006. Unfortunately, because of recruitment difficulties, the desired sample size of 50 per group was not achieved. Of the 516 patients with suspected hypertension who were screened, 337 were not eligible because they did not meet the study’s inclusion criteria at the initial screening. The reasons for not qualifying varied: past medical history, desire to choose a particular treatment, required commitment of time too great, inability to come to our centre (e.g., living far away), lack of interest in stress management or in the drug. The remaining 179 patients were sent to the medical hypertension clinic for evaluation. Of these, 13 patients decided not to participate after undergoing the evaluation. An additional 101 patients were ineligible for the following reasons: 65 patients did not meet the minimum blood pressure inclusion criteria after the washout process, 8 patients had excessively high blood pressure (≥180/110 mm Hg), and 28 had a medical history that precluded their participation (such as coronary artery disease) (Fig. 1).
Figure 1.
Flow diagram for patients in the study
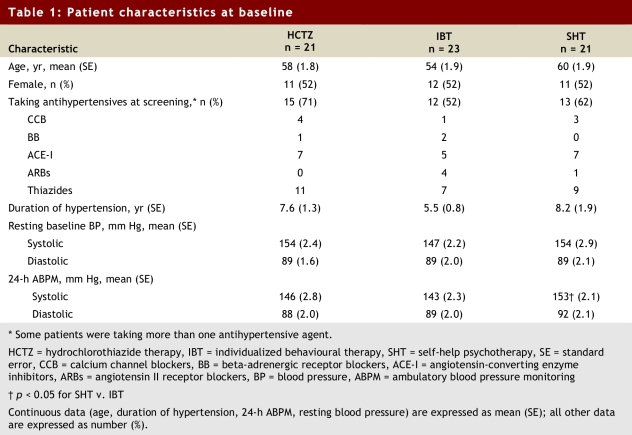
A total of 65 patients (with baseline characteristics as listed in Table 1) were randomly assigned to 1 of the 3 groups: 21 to receive hydrochlorothiazide, 23 to undergo individualized behavioural psychotherapy, and 21 to perform self-help psychotherapy. Two patients in each group acknowledged that they had sought psychological or psychiatric help in the past. One of these patients (assigned to the hydrochlorothiazide group) had received self-help psychological therapy (in the form of a booklet). There was no statistically significant difference in the number of patients who had previously received hydrochlorothiazide or any other antihypertensive drug. Except for systolic blood pressure as recorded during 24-hour ambulatory monitoring, which was higher for those in the self-help psychotherapy group, the groups were similar with respect to all variables (Table 1). Six patients in the hydrochlorothiazide group, 6 in the individualized behavioural psychotherapy group, and 9 in the self-help psychotherapy group withdrew from the study or did not undergo the second 24-hour monitoring of ambulatory blood pressure (at 12 weeks) (Fig. 1).
Table 1.
Patient characteristics at baseline
Primary outcome: change in ambulatory blood pressure (24-hour monitoring)
Hydrochlorothiazide produced a statistically significant reduction in both systolic and diastolic blood pressure during 24-hour monitoring of ambulatory blood pressure, and this change was greater than the changes observed with either individualized behavioural or self-help psychological therapy (systolic mean reduction ± standard error: −11.03 ± 2.53 v. −0.08 ± 2.38 v. −1.23 ± 2.83 mm Hg, respectively, p = 0.006; diastolic: −6.06 ± 1.56 v. 0.29 ± 1.47 v. −0.71 ± 1.75 mm Hg, respectively, p = 0.01; Table 2). Neither form of psychological therapy reduced ambulatory blood pressure, as measured by 24-hour monitoring, relative to baseline.
Table 2.
Twenty-four-hour ambulatory blood pressure measurements at baseline and change from baseline at week 12
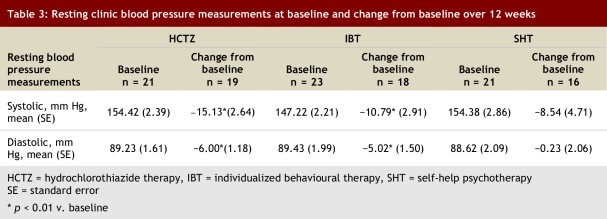
Secondary outcome: change in resting clinic blood pressure
For this outcome, we included data from all patients with at least one blood pressure measurement after treatment and used the weighted average from all post-treatment blood pressure measurements for the analysis. As such, data were available for more participants: 19 in the hydrochlorothiazide group, 18 in the individualized behavioural therapy group, and 16 in the self-help therapy group. In this analysis, both hydrochlorothiazide therapy and individualized behavioural psychotherapy were associated with a statistically significant reduction (relative to baseline) in systolic and diastolic blood pressure (Table 3). The extent of reduction in blood pressure was numerically greater in the group receiving hydrochlorothiazide than in the other 2 groups, but the mean change in resting clinic systolic or diastolic blood pressure over 12 weeks showed no statistically significant difference among the 3 groups.
Table 3.
Resting clinic blood pressure measurements at baseline and change from baseline over 12 weeks
Adverse events
A total of 5 patients withdrew because of adverse events. Three participants experienced intractable headache (1 patient in the hydrochlorothiazide group and 2 in the self-help therapy group). In all 3 cases, the headache subsided after withdrawal from the study. One patient who was receiving hydrochlorothiazide withdrew because of a suspected allergic reaction to the study medication (the patient stopped taking the drug at day 21 because of soreness in the tongue and lips). One patient in the self-help therapy group withdrew because of palpitations. In addition to these 5 withdrawals, 1 patient who was receiving 25mg of hydrochlorothiazide experienced hypokalemia, which was corrected by the addition of spironolactone. There were no serious adverse events during the trial.
Discussion
It has been hypothesized that psychological stress may contribute to the elevation of blood pressure in patients with primary hypertension, and, conversely, that psychological therapy may lower blood pressure. However, these hypotheses have been called into question by the results of a recent Cochrane systematic review, in particular the results obtained when the analysis was limited to studies that used blinded outcome assessment.5 In that review of relaxation therapies, 25 RCTs (n = 1198 patients) were evaluated. The authors concluded that the effect of these therapies in lowering blood pressure was questionable because of the poor quality of the studies. In fact, when only trials using blinded outcome assessment were included (9 RCTs, n = 498 patients), there was no significant reduction in either systolic or diastolic blood pressure.5
The current study is the first RCT to directly compare psychological therapy with a standard pharmacological antihypertensive treatment. The use of hydrochlorothiazide as a control worked well in this study. The drug lowered ambulatory blood pressure, as measured by 24-hour monitoring, by about 11/6 mm Hg, which is similar to the reduction reported in a meta-analysis of other studies of standard-dose thiazide given for a similar duration of therapy, 9/4 mm Hg.14 This result demonstrates that the patients in this trial were representative of patients in other trials studying mild to moderate hypertension.
This study has shown that in a clinical setting where thiazide therapy lowered blood pressure by a magnitude similar to that expected, 2 psychological therapies did not have this effect. This difference in outcome was particularly evident from the blood pressure data obtained with 24-hour monitoring. In particular, the individualized behavioural therapy and self-help psychotherapy had no effect on 24-hour ambulatory systolic or diastolic blood pressure.
Hydrochlorothiazide also significantly lowered resting clinic blood pressure relative to baseline. In addition, individualized behavioural psychotherapy but not self-help psychotherapy produced a statistically significant change in resting clinic blood pressure from baseline. For this outcome, however, there was no statistically significant difference among the groups. This lack of difference may have been due in part to the “placebo effect” commonly observed in studies that used in-clinic measurements of blood pressure. The causes of this phenomenon are unknown, but participating in a study may offer the patient some reassurance (e.g., by having the doctor’s full attention, by meeting a psychological need), which could be enough to reduce anxiety and stress or to provoke changes in attitudes, which in turn might improve blood pressure readings in the clinic setting. It is also possible that the individualized behavioural psychotherapy helped patients to learn to relax in the clinic setting, which would have offset the “white-coat effect.” If so, this would be unlikely to have any clinical value, as there was no reduction in ambulatory blood pressure as measured by 24-hour monitoring. This study was a good demonstration of the value of such 24-hour monitoring. A previous study provided evidence for the lack of a placebo effect in patients with mild to moderate hypertension when blood pressure was measured by 24-hour monitoring.17 The combination of a lack of the placebo effect and the large number of blood pressure measurements obtained increases the power of 24-hour monitoring to identify a treatment effect, as occurred in this trial.
One of the strengths of this study was the proper randomization as well as the foolproof method of concealing treatment allocation from the patients and the investigators. Two additional strengths were the use of an automated device for recording both ambulatory and clinic blood pressure, and the absence of the investigators at the time of measurement. The objective of this was to reduce subjective bias when measuring blood pressure. A further strength of this study was that all of the available results were used in the analysis, which prevented any reporting bias.
One limitation of this study was the small sample size, which was caused by difficulties in recruiting patients with newly diagnosed hypertension and by excluding a large number of previously treated patients who did not meet the blood pressure criteria after the washout period (65 [58%] of the 112 patients who underwent washout). A second, related limitation was the high rate of patients unavailable for the primary outcome analysis (6/21 [29%] from the hydrochlorothiazide group, 6/23 [26%] from the individualized behavioural psychotherapy group and 9/21 [43%] from the self-help therapy group). Because we did not achieve the desired sample size and because many patients withdrew after randomization, the study’s power was lower than planned, and the probability of accepting the null hypothesis (i.e., type II or beta error) was increased. Our inability to find differences when we compared the 3 groups of clinic blood pressure measurements is an example of this type II error. This loss of power, however, did not prevent detection of a difference between hydrochlorothiazide and either psychological intervention by 24-hour ambulatory measurements. A third limitation was the chance finding that baseline blood pressure in the self-help psychotherapy group was higher than that in the individualized behavioural psychotherapy group. This might have reduced the opportunity for the individualized behavioural psychotherapy intervention to lower blood pressure in that group. However, when we performed the post-hoc ANCOVA analysis using baseline values as a covariate, the p values changed minimally for both ambulatory and resting clinic blood pressure outcomes; we therefore believe that the initial difference in blood pressure between these 2 groups probably had little effect. Nonetheless, caution is warranted in interpreting these results, as the trial had limited power to prove a lack of effect of the psychological interventions on the 24-hour blood pressure measurements. When we planned our study, no information was available on the effect of psychological therapy in lowering blood pressure relative to a pharmacological treatment. We chose hydrochlorothiazide because, in addition to the well-known ability of this drug to lower blood pressure, the thiazides in general have the most evidence for reductions in mortality and morbidity when used as first-line drugs.18 The key important finding of this study is that compared with hydrochlorothiazide, psychological therapies appeared to have no clinically important effect in lowering blood pressure over a 12-week period, as assessed by 24-hour ambulatory monitoring. These results apply to patients with mild uncomplicated hypertension (systolic ≥ 140 and/or diastolic ≥ 90 mm Hg).
This new information needs to be put into context with other available RCT data. The best available evidence of the effect of relaxation therapies on blood pressure was provided by a recent Cochrane systematic review. In that review, Dickinson and colleagues5 found that when only RCTs with blinded blood pressure measurement were included, the psychological or relaxation techniques had no statistically significant effect in reducing blood pressure. This led the authors to conclude, “In view of the poor quality of included trials and unexplained variation between trials, the evidence in favor of causal association between relaxation therapy and blood pressure reduction is weak. Some of the apparent benefit of relaxation was probably due to aspects of treatment unrelated to relaxation.”5 The results of the RCT presented here are in agreement with that conclusion. If future trials of psychological interventions and other relaxation therapies are conducted, they must have rigorous designs to minimize bias.
Trial registration
Clinicaltrials.gov identifier: NCT00247910
Biographies
Marco I Perez is an assistant researcher in the Department of Anesthesiology, Pharmacology and Therapeutics, Faculty of Medicine, at the University of British Columbia, Vancouver, British Columbia, Canada.
Wolfgang Linden is a professor in the Department of Psychology, Faculty of Medicine, at the University of British Columbia.
Thomas Perry Jr. is a clinical assistant professor,
Lorri J Puil is a clinical fellow, and
James M Wright is a professor in the Department of Anesthesiology, Pharmacology and Therapeutics, Faculty of Medicine, at the University of British Columbia.
Footnotes
None declared.
The Canadian Institutes of Health Research (CIHR) was the funding source. The authors’ work was independent of CIHR. The funding source had no financial or other interest in the study outcome and had no role in the design of the study or the collection, analysis, interpretation or reporting of the data.
MIP participated in the design, conduct, analysis and writing of the first draft of this manuscript; WL, LP and JMW participated in the conception of the study, design, conduct and revisions of this manuscript; TPJr participated in conducting the trial.
References
- 1.Svetkey L P, Simons-Morton D, Vollmer W M, Appel L J, Conlin P R, Ryan D H, Ard J, Kennedy B M. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159(3):285–293. doi: 10.1001/archinte.159.3.285. http://archinte.ama-assn.org/cgi/pmidlookup?view=long&pmid=9989541. [DOI] [PubMed] [Google Scholar]
- 2.He FJ, MacGregor GA. Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. 2004;2004(3) doi: 10.1002/14651858.CD004937. [DOI] [PubMed] [Google Scholar]
- 3.Fagard Robert H, Cornelissen Véronique A. Effect of exercise on blood pressure control in hypertensive patients. Eur J Cardiovasc Prev Rehabil. 2007;14(1):12–17. doi: 10.1097/HJR.0b013e3280128bbb. [DOI] [PubMed] [Google Scholar]
- 4.Staessen J, Fagard R, Amery A. The relationship between body weight and blood pressure. J Hum Hypertens. 1988;2(4):207–217. [PubMed] [Google Scholar]
- 5.Dickinson Heather O, Campbell Fiona, Beyer Fiona R, Nicolson Donald J, Cook Julia V, Ford Gary A, Mason James M. Relaxation therapies for the management of primary hypertension in adults. Cochrane Database Syst Rev. 2008;(1) doi: 10.1002/14651858.CD004935.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Gerin W, Pickering T G, Glynn L, Christenfeld N, Schwartz A, Carroll D, Davidson K. An historical context for behavioral models of hypertension. J Psychosom Res. 2000;48(4-5):369–377. doi: 10.1016/s0022-3999(99)00095-1. [DOI] [PubMed] [Google Scholar]
- 7.Linden Wolfgang. Psychologic treatment for hypertension can be efficacious. Prev Cardiol. 2003;6(1):48–53. doi: 10.1111/j.1520-037x.2003.0962.x. [DOI] [PubMed] [Google Scholar]
- 8.Grossman P, Watkins L L, Wilhelm F H, Manolakis D, Lown B. Cardiac vagal control and dynamic responses to psychological stress among patients with coronary artery disease. Am J Cardiol. 1996;78(12):1424–1427. doi: 10.1016/s0002-9149(97)89295-8. [DOI] [PubMed] [Google Scholar]
- 9.Ebrahim S, Smith G D. Lowering blood pressure: a systematic review of sustained effects of non-pharmacological interventions. J Public Health Med. 1998;20(4):441–448. doi: 10.1093/oxfordjournals.pubmed.a024800. http://jpubhealth.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=9923952. [DOI] [PubMed] [Google Scholar]
- 10.Eisenberg D M, Delbanco T L, Berkey C S, Kaptchuk T J, Kupelnick B, Kuhl J, Chalmers T C. Cognitive behavioral techniques for hypertension: are they effective. Ann Intern Med. 1993;118(12):964–72. doi: 10.7326/0003-4819-118-12-199306150-00009. http://www.annals.org/cgi/pmidlookup?view=long&pmid=8489111. [DOI] [PubMed] [Google Scholar]
- 11.Linden W, Chambers L. Clinical effectiveness of non-drug treatment for hypertension: A meta- analysis. Ann Behav Med. 1994;16(1):35–45. [Google Scholar]
- 12.Nakao Mutsuhiro, Yano Eiji, Nomura Shinobu, Kuboki Tomifusa. Blood pressure-lowering effects of biofeedback treatment in hypertension: a meta-analysis of randomized controlled trials. Hypertens Res. 2003;26(1):37–46. doi: 10.1291/hypres.26.37. http://joi.jlc.jst.go.jp/JST.JSTAGE/hypres/26.37?from=PubMed. [DOI] [PubMed] [Google Scholar]
- 13.Stetter Friedhelm, Kupper Sirko. Autogenic training: a meta-analysis of clinical outcome studies. Appl Psychophysiol Biofeedback. 2002;27(1):45–98. doi: 10.1023/a:1014576505223. [DOI] [PubMed] [Google Scholar]
- 14.Law M R, Wald N J, Morris J K, Jordan R E. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427. doi: 10.1136/bmj.326.7404.1427. http://bmj.com/cgi/pmidlookup?view=long&pmid=12829555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mattu G S, Perry T L, Wright J M. Comparison of the oscillometric blood pressure monitor (BPM-100(Beta) ) with the auscultatory mercury sphygmomanometer. Blood Press Monit. 2001;6(3):153–159. doi: 10.1097/00126097-200106000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Linden W, Lenz J W, Con A H. Individualized stress management for primary hypertension: a randomized trial. Arch Intern Med. 2001;161(8):1071–1080. doi: 10.1001/archinte.161.8.1071. http://archinte.ama-assn.org/cgi/pmidlookup?view=long&pmid=11322841. [DOI] [PubMed] [Google Scholar]
- 17.Mancia G, Omboni S, Parati G, Ravogli A, Villani A, Zanchetti A. Lack of placebo effect on ambulatory blood pressure. Am J Hypertens. 1995;8(3):311–315. doi: 10.1016/0895-7061(94)00250-F. [DOI] [PubMed] [Google Scholar]
- 18.Wright J M, Lee C H, Chambers G K. Systematic review of antihypertensive therapies: does the evidence assist in choosing a first-line drug. CMAJ. 1999;161(1):25–32. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=10420860. [PMC free article] [PubMed] [Google Scholar]
- 19.DeRubeis R, Beck AT. Cognitive Therapy. In: Dobson KS, editor. Handbook of Cognitive Behavioral Therapy. New York: Guilford Press; 1988. pp. 273–287. [Google Scholar]
- 20.Wolfgang Linden. Autogenic training: a clinical guide. New York: Guilford Press; 1990. [Google Scholar]
- 21.Ethel Roskies. Stress management for the healthy Type A: theory and practice. New York: Guilford Press; 1987. [Google Scholar]
- 22.Richard M Suinn. Anxiety management training: a behavior therapy. New York: Plenum Press; 1990. [Google Scholar]
- 23.Linden W. Treating hypertension. In: Kuczmierczyk A, Nicevic A, editors. A case formulation approach to behavioral medicine. London: Routledge & Brunner; 2006. [Google Scholar]
- 24.Wolfgang Linden. Stress management: from basic science to better practice. Thousand Oaks (USA): Sage Publications; 2005. [Google Scholar]
- 25.Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the MMPI. J Appl Psychol. 1954;38:414–418. [Google Scholar]
- 26.Spielberger CD, Gorsuch RL, Lushene RE. Manual for the State-trait Anxiety Inventory. Palo Alto, Calif: Consulting Psychologists Press; 1970. [Google Scholar]
- 27.Linden Wolfgang, Hogan Brenda E, Rutledge Thomas, Chawla Anuradha, Lenz Joseph W, Leung Debbie. There is more to anger coping than "in" or "out". Emotion. 2003;3(1):12–29. doi: 10.1037/1528-3542.3.1.12. [DOI] [PubMed] [Google Scholar]
- 28.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 29.Beck AT. Depression inventory. Philadelphia: Center for Cognitive Therapy; 1978. [Google Scholar]
- 30.Paulhus DL. BIDR reference manual for version VI. Vancouver: University of British Columbia; 1991. [Google Scholar]