Abstract
Purpose:
To determine whether racial differences exist between consistency of medical care and blood pressure (BP) control over time among elderly, hypertensive African Americans and whites.
Methods:
Participants included 1,402 African Americans and 1,058 whites from the Piedmont Health Survey of the Elderly who were hypertensive (SBP >140 mmHg, DBP >90 mmHg, or used anti-hypertensive medications) at baseline (1987). Consistency of care was assessed based on self-reported receipt of physician care at each wave and categorized as consistent (care at each wave), inconsistent (care at some, but not all waves), and no standard care (no care at any wave). BP control was defined as SBP < 140 mmHg and DBP < 90 mmHg at subsequent waves of participation (1990, 1994, 1998). Repeated measures regression was used to longitudinally assess the association between consistency of care and BP control.
Results:
African Americans had a less favorable health profile and significantly less consistency of care over time (p<0.0001). In analyses adjusted for demographic factors, participants with consistent or inconsistent care had greater odds of BP control (OR=1.34, 95% CI: 1.09, 1.64 and OR=1.41, 95% CI: 1.12, 1.78) than those with no standard care, but these associations were attenuated after additional adjustment for health care characteristics and co-morbidities.
Conclusions:
Compared to no standard care, receipt of consistent or inconsistent physician care was associated with BP control among the elderly. These associations did not differ by race, although African Americans were more likely to report inconsistent or no standard care which suggests disparities in health care access remain.
Keywords: Hypertension, Race, Epidemiology, Elderly, Continuity of Care
INTRODUCTION
Racial disparities in hypertension prevalence and its sequelae persist in the United States (1-3). African Americans are disproportionately affected by hypertension and when afflicted, have less than optimal blood pressure control, despite over three decades of evidence about the benefits of pharmacologic therapy (4). Several factors have been postulated to contribute to racial disparities in hypertension prevalence and control, including diet, physical activity, health insurance, and access to quality health care (5).
Consistency of care, a measure of access to care and the health care relationship over time between patients and physicians, is an important factor in the prevention and treatment of chronic diseases including hypertension (6). A previous study reported that consistency of care was associated with hypertension diagnosis and receipt of antihypertensive therapy among the elderly, but did not evaluate blood pressure (BP) control (7). In another prospective study of elderly adults, blood pressure control was comparable between African Americans and whites over a 9-year study period, but consistency of care was not evaluated (8). A cross-sectional study reported an association between usual provider and BP control among the general population (5), but to date, no study has examined patterns of consistency of care and blood pressure control specifically among elderly hypertensives over time. Investigation of these patterns may provide useful information on potential racial differences in long-term healthcare trends and outcomes among those who have hypertension. Thus, the purpose of this population-based, observational study was to describe and examine the relationship between consistency of care and blood pressure control among elderly African Americans and whites over a 12-year period.
METHODS
Study Design
The Piedmont Health Survey of the Elderly (PHSE) was conducted by the Duke University Center for Aging and Human Development to assess health, well-being, morbidity, and mortality in community-dwelling older populations as part of the Established Populations for the Epidemiological Study of the Elderly (EPESE). A detailed description of the EPESE study design has been published (9). The PHSE selected 5,226 participants aged 65 years and older at baseline (1987) from five counties in North Carolina (1 urban, 4 rural), with an over-sampling of African Americans. Trained personnel collected baseline measures on 4,162 elders (80% response rate) through 90-minute in-home interviews and participants had three follow-up in-person examinations (1990; 1994; 1998) and also received annual telephone contacts in the intermittent years.
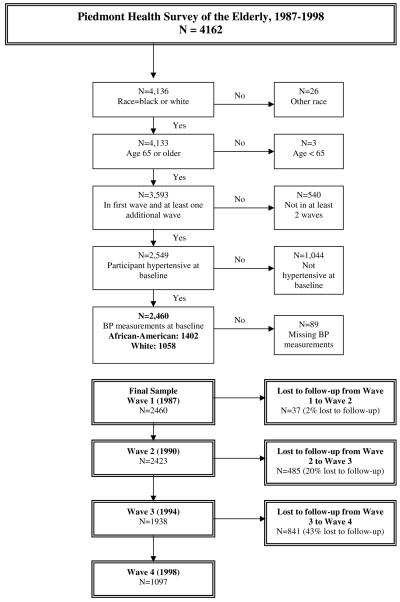
Study Sample
This study excluded participants who were not white or African-American (n=26), were less than 65 years old (n=3), did not participate in at least one follow-up wave (n=540), were not hypertensive (n=1044), or were missing blood pressure measurements (n=89). Following these exclusions, 1402 African American and 1058 white participants who were hypertensive at baseline (SBP≥140mmHg, DBP≥90mmHg, or currently taking anti-hypertensive medications) and had at least one additional wave of data were included in this study.
Outcome Variable
Blood pressure measurements were taken at baseline and each subsequent wave following a standardized protocol. Two sitting blood pressure measurements were taken and the mean value was used to determine blood pressure control status: controlled (SBP < 140 mmHg and DBP < 90 mmHg) and uncontrolled (SBP > 140 mmHg or DBP > 90 mmHg).
Predictor Variable
Consistency of care was defined as the level of consistent medical care received from a physician, which was derived from a PHSE survey question on use of health care services. Over each of the four waves, respondents were asked the following: “When you want help with or care for a [physical] health problem, where do you usually go?” Responses included nowhere, no usual place, a physician, a hospital or other. For those who responded a physician, they were asked the physician's name and where did they see the doctor—in a private office, or clinic, a public clinic, a VA hospital, other hospital or where. Consistency of care was classified into three categories: consistent care (receipt of physician care across all waves of participation); inconsistent care (receipt of physician care across some, but not all waves of participation); and no standard care (no receipt of physician care across any waves of participation). The participant was not required to have the same physician at each wave of participation, but was required to have a named physician at each wave of participation to be counted as having received care at that wave. If a participant was counted as having received care by a named physician, then the location of the care was then assessed as occurring at a private practice, clinic, hospital or other institution.
Covariates
The socio-demographic variables assessed were age at baseline, gender, education, annual income, marital status, and residence in a rural area. General health perception (excellent, good, fair, or poor), history of chronic diseases (heart disease, cancer, stroke, and diabetes), and limitations in activities of daily living (ADLs) were also ascertained. Several healthcare variables were assessed including Medicaid (a government health insurance program for low-income persons), Medigap (private supplemental health insurance for Medicare beneficiaries for non-covered health care costs), residence in a nursing home, residence in county where care was received, location of care (clinic/hospital, private practice, or other), and satisfaction with care. Lifestyle variables, such as diet, physical activity, alcohol consumption, and smoking were also collected; however, these variables were not collected over all four waves and/or a large proportion of responses were missing, so these variables were not included in the analyses.
Participants were asked to bring in the containers for all of the medications that they had taken in the previous two weeks or take when needed. Names of the medications were recorded and classified by indication. For antihypertensive therapy, medication included single agent therapy (diuretics; beta-blockers; calcium channel blockers; angiotensin converting enzyme (ACE) inhibitors; other antihypertensive agents) and combination therapy (diuretics plus other antihypertensive agents).
Analysis
Chi-square, analyses of variance, and t-tests were used to describe and compare, across four waves, consistency of care and blood pressure control between African Americans and whites. Repeated measures models were fit using generalized estimating equations (GEE) to simultaneously test for racial differences and trends across time for each of the socio-demographic, health status, healthcare, and consistency of care variables (10).
To test whether there was a difference in the association between consistency of care and blood pressure control across time, multivariable repeated measures models were fit using GEE. The exposure was categorized into three levels: no standard care (referent group), inconsistent care, and consistent care. Crude and adjusted analyses assessed the association between consistency of care and blood pressure control. Age, gender, and education were measured at baseline and did not change over time while annual income, work status, marital status, history of chronic diseases, limitation in activities of daily living (ADLs), health insurance coverage, residence in a nursing home, satisfaction with care, and anti-hypertensive medication use were included in the models as time varying covariates. A sensitivity analysis was also done to assess the effect of loss to follow-up at each wave. Loss to follow-up increased over the 12-year study period: 2% from wave 1 to wave 2; 20% from wave 2 to wave 3; and 43% from wave 3 to wave 4. Because of the increase in the loss to follow-up from wave 3 to wave 4, the socio-demographic characteristics of those who participated in both wave 3 and wave 4 were compared to those who participated in wave 3, but not wave 4, with differences noted for education, income, marital status, and working status. A sensitivity analysis was done to assess potential differences in effect estimates using data from all waves (1-4) and data from waves 1-3 only. The estimates were comparable, therefore all waves of data (waves 1 – 4) were used in this analysis. All analyses were done using version 9.1 of SAS®.
RESULTS
At the baseline examination, 31% of the participants were men, 57% were African-American, and the average age was 73 years (Table 1). The majority of participants had an annual income between $4,000 and $15,000 and was not working at baseline. Compared to whites over time, African Americans had fewer mean years of education, were less likely to be currently married, and more likely to reside in a rural area (all p<0.001). Most participants reported excellent or good health, although there was a significant trend in health status over time, with fewer African Americans reporting excellent or good health (p<0.001). For diagnosed health conditions over the four waves, a greater proportion of whites than African Americans reported having cancer (p<0.001) or a heart condition (p=0.0493). In contrast, a greater proportion of African Americans than whites reported having diabetes (p<0.001), while no racial difference over time was noted for the diagnosis of stroke. ADL limitations increased over the four waves, with African Americans reporting more limitations than whites (p=0.0139). The proportion of participants with Medicaid insurance increased over time, although no clear pattern was observed for Medigap supplemental insurance coverage. More African Americans had Medicaid coverage, while more whites had Medigap supplemental insurance coverage (both p<0.001) and more African Americans received care from a public clinic whereas more white participants received care from a private practice.
Table 1.
Demographic and healthcare characteristics by race and wave, Piedmont Health Survey of the Elderly 1987-1998
| Wave 1 (1987) N=2460 |
Wave 2 (1990) N=2423 |
Wave 3 (1994) N=1938 |
Wave 4 (1998) N=1097 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| African American |
White | African American |
White | African American |
White | African American |
White | P-Value1 | |
| N=1,402 | N=1,058 | N=1,385 | N=1,038 | N=1,123 | N=815 | N=624 | N=473 | ||
| Demographics, | |||||||||
| Male, n(%) | 427(30.5) | 345(32.6) | 421(30.4) | 338(32.6) | 317(28.2) | 267(32.8) | 168(26.9) | 150(31.7) | NA2 |
| Mean (SD) Age (yrs) | 73.3(6.5) | 73.4(6.4) | 76.3(6.5) | 76.4(6.5) | 79.2(6.2) | 79.1(6.0) | 82.2(5.3) | 81.9(5.0) | 0.5784 |
| Mean (SD) Years Of Education | 7.4(4.0) | 9.9(3.6) | 7.4(4.0) | 9.9(3.6) | 7.5(3.9) | 10.0(3.6) | 7.8(3.8) | 10.2(3.7) | <.0001 |
| Married, n(%) | 454(32.4) | 431(40.7) | 386(27.9) | 368(35.5) | 279(24.8) | 261(32.0) | 158(25.3) | 143(30.2) | <.0001 |
| Currently Working, n(%) | 171(12.2) | 119(11.2) | 113(8.2) | 76(7.3) | 76(6.8) | 47(5.8) | 34(5.4) | 25(5.3) | 0.3258 |
| Annual Household Income, n(%) | |||||||||
| $0-$3999 | 347(24.8) | 92(8.7) | 227(16.4) | 62(6.0) | 80(7.1) | 27(3.3) | 23(3.7) | 5(1.1) | NA2 |
| $4000-$6999 | 554(39.5) | 264(25.0) | 548(39.6) | 226(21.8) | 407(36.2) | 140(17.2) | 234(37.5) | 66(14.0) | |
| $7000-$14999 | 201(14.3) | 243(23.0) | 245(17.7) | 244(23.5) | 252(22.4) | 205(25.2) | 184(29.5) | 143(30.2) | |
| >$15000 | 80(5.7) | 265(25.0) | 91(6.6) | 276(26.6) | 88(7.8) | 215(26.4) | 65(10.4) | 153(32.3) | |
| Respondent Lives In A Rural Area, n(%) | 851(60.7) | 512(48.4) | 845(61.0) | 503(48.5) | 689(61.4) | 399(49.0) | 392(62.8) | 241(51.0) | <.0001 |
| General Health Perception: | |||||||||
| Excellent Or Good | 623(44.4) | 598(56.5) | 588(42.5) | 519(50.0) | 431(38.4) | 401(49.2) | 269(43.1) | 238(50.3) | <.0001 |
| Fair | 528(37.7) | 303(28.6) | 434(31.3) | 255(24.6) | 322(28.7) | 168(20.6) | 187(30.0) | 134(28.3) | |
| Poor | 195(13.9) | 139(13.1) | 144(10.4) | 100(9.6) | 100(8.9) | 60(7.4) | 63(10.1) | 46(9.7) | |
| Diagnosed Health Conditions, n(%) | |||||||||
| Heart Condition | 177(12.6) | 171(16.2) | 223(16.1) | 194(18.7) | 188(16.7) | 161(19.8) | 127(20.4) | 93(19.7) | 0.0493 |
| Cancer | 96(6.8) | 172(16.3) | 110(7.9) | 198(19.1) | 102(9.1) | 179(22.0) | 96(15.4) | 130(27.5) | <.0001 |
| Stroke | 123(8.8) | 88(8.3) | 153(11.0) | 120(11.6) | 144(12.8) | 101(12.4) | 102(16.3) | 75(15.9) | 0.7824 |
| Diabetes | 349(24.9) | 182(17.2) | 383(27.7) | 199(19.2) | 313(27.9) | 174(21.3) | 201(32.2) | 105(22.2) | <.0001 |
| One or more ADL limitation, n(%) | 158(11.3) | 94(8.9) | 287(20.7) | 191(18.4) | 254(22.6) | 149(18.3) | 246(39.4) | 159(33.6) | 0.0139 |
| Healthcare Characteristics | |||||||||
| Medicaid Insurance, n(%) | 157(11.2) | 36(3.4) | 248(17.9) | 60(5.8) | 285(25.4) | 73(9.0) | 230(36.9) | 66(14.0) | <.0001 |
| Medigap Supplemental Insurance, n(%) | 453(32.3) | 790(74.7) | 423(30.5) | 692(66.7) | 294(26.2) | 480(58.9) | 172(27.6) | 323(68.3) | <.0001 |
| Ever Resided In A Nursing Home, n(%) | 11(0.8) | 24(2.3) | 78(5.6) | 87(8.4) | 114(10.2) | 127(15.6) | 86(13.8) | 82(17.3) | <.0001 |
| Resided In County Where Care Provided, n(%) | 834(59.5) | 819(77.4) | 700(50.5) | 665(64.1) | 637(56.7) | 508(62.3) | 359(57.5) | 302(63.8) | NA2 |
| Location of Care, n(%) | |||||||||
| No Usual Place | 56(4.0) | 34(3.2) | 32(2.3) | 27(2.6) | 34(3.0) | 14(1.7) | 14(2.2) | 7(1.5) | <.0001 |
| Private Practice | 870(62.1) | 915(86.5) | 774(55.9) | 802(77.3) | 610(54.3) | 620(76.1) | 463(74.2) | 435(92.0) | |
| Public Clinic | 472(33.7) | 101(9.5) | 454(32.8) | 92(8.9) | 324(28.9) | 56(6.9) | 145(23.2) | 24(5.1) | |
| Other3 | 0(0.0) | 4(0.4) | 8(0.6) | 21(2.0) | 3(0.3) | 2(0.2) | 0(0.0) | 7(1.5) | |
| Respondent Satisfaction with Care, n(%) | |||||||||
| Satisfied | 1,231(87.8) | 931(88.0) | 1,079(77.9) | 807(77.7) | 799(71.1) | 591(72.5) | 491(78.7) | 382(80.8) | 0.0378 |
| Dissatisfied | 95(6.8) | 94(8.9) | 63(4.5) | 50(4.8) | 46(4.1) | 38(4.7) | 24(3.8) | 30(6.3) | |
P-value indicates differences in respondent characteristics between African Americans and Whites and is obtained from Generalized Estimating Equations.
P-value indicates there is a differential effect over time (significant interaction of race by time) in which differences in characteristics vary across time. Therefore, no main effects model can be presented (male p=0.0204; income p<0.0001; and lives in same county where care provided p=0.0016).
Other location: Employee health facility and other
The distribution of consistency of care across the four waves is presented in Table 2. The majority of the study sample had consistent care with significantly more whites having consistent care, and more African Americans having inconsistent or no standard care (all p<0.001). Across all four waves, and for both race groups, the mean systolic blood pressure was greater than 140 mmHg, while the mean diastolic blood pressure was less than 90 mmHg (Table 3). No racial differences were noted for systolic blood pressure, but African Americans had a higher diastolic blood pressure (p<0.001) compared to whites. There was an increase over time from wave 1 to wave 4 in the proportion of African Americans and whites with controlled blood pressure. Over all four waves, a greater proportion of whites had Stage 1 hypertension than African Americans although there was no significant difference in Stage 2 hypertension.
Table 2.
Distribution of consistency of care by race and wave, Piedmont Health Survey of the Elderly 1987-1998
| Wave 1 (1987) N=2460 |
Wave 2 (1990) N=2423 |
Wave 3 (1994) N=1938 |
Wave 4 (1998) N=1097 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| African American |
White | African American |
White | African American |
White | African American |
White | P-Value1 | |
| N | 1,402 | 1,058 | 1,385 | 1,038 | 1,123 | 815 | 624 | 473 | |
| Consistent Care, n(%) | 1,120(79.9) | 956(90.4) | 838(60.5) | 773(74.5) | 603(53.7) | 551(67.6) | 381(61.1) | 362(76.5) | <.0001 |
| Inconsistent Care, n(%)* | - | - | 381(27.5) | 214(20.6) | 454(40.4) | 250(30.7) | 224(35.9) | 106(22.4) | <.0001 |
| No Standard Care, n(%) | 282(20.1) | 102(9.6) | 166(12.0) | 51(4.9) | 66(5.9) | 14(1.7) | 19(3.0) | 5(1.1) | <.0001 |
Inconsistent Care is not assessed at Wave 1 since the definition requires data from two or more time periods.
Two-sided test of racial difference in consistency of care characteristics over time using Generalized Estimating Equations.
Table 3.
Blood pressure characteristics and antihypertensive therapy use by race and wave, Piedmont Health Survey of the Elderly 1987-1998
| Wave 1 (1987) N=2460 |
Wave 2 (1990) N=2423 |
Wave 3 (1994) N=1938 |
Wave 4 (1998) N=1097 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| African American |
White | African American |
White | African American |
White | African American |
White | P-Value1 | |
| N=1,402 | N=1,058 | N=1,385 | N=1,038 | N=1,123 | N=815 | N=624 | N=473 | ||
| Mean (SD) SBP | 149.2(19.6) | 150.3(19.2) | 145.4(22.0) | 145.1(20.2) | 146.9(23.3) | 147.1(22.2) | 144.7(22.5) | 145.2(21.3) | 0.3792 |
| Mean (SD) DBP | 82.9(12.1) | 80.1(12.0) | 79.3(12.7) | 77.1(11.4) | 76.4(13.9) | 73.7(12.6) | 74.2(12.4) | 71.1(13.7) | <.0001 |
| BP Control Status, n(%) | |||||||||
| Controlled | 359(25.6) | 238(22.5) | 517(37.3) | 391(37.7) | 388(34.6) | 259(31.8) | 271(43.4) | 177(37.4) | 0.1478 |
| Stage 1 HTN | 635(45.3) | 515(48.7) | 399(28.8) | 314(30.3) | 283(25.2) | 235(28.8) | 184(29.5) | 163(34.5) | 0.0018 |
| Stage 2 HTN | 408(29.1) | 305(28.8) | 309(22.3) | 196(18.9) | 275(24.5) | 180(22.1) | 144(23.1) | 102(21.6) | 0.2408 |
| Missing | 0(0.0) | 0(0.0) | 160(11.6) | 137(13.2) | 177(15.8) | 141(17.3) | 25(4.0) | 31(6.6) | 0.0997 |
| Antihypertensive Single Medication Therapy, n(%) |
|||||||||
| Ace Inhibitors | 3(0.2) | 7(0.7) | 27(1.9) | 15(1.4) | 23(2.0) | 30(3.7) | 23(3.7) | 20(4.2) | 0.2247 |
| Diuretics | 459(32.7) | 280(26.5) | 324(23.4) | 194(18.7) | 227(20.2) | 117(14.4) | 125(20.0) | 63(13.3) | <.0001 |
| Beta-Blockers | 47(3.4) | 79(7.5) | 32(2.3) | 68(6.6) | 16(1.4) | 39(4.8) | 21(3.4) | 23(4.9) | <.0001 |
| Calcium Channel Blockers | 10(0.7) | 31(2.9) | 37(2.7) | 45(4.3) | 69(6.1) | 65(8.0) | 71(11.4) | 41(8.7) | NA2 |
| Other Antihypertensive Medications, n(%) |
220(15.7) | 101(9.5) | 155(11.2) | 76(7.3) | 89(7.9) | 38(4.7) | 48(7.7) | 20(4.2) | <.0001 |
| Diuretics + Other Antihypertensive Agents, n(%) |
145(10.3) | 68(6.4) | 121(8.7) | 61(5.9) | 70(6.2) | 25(3.1) | 30(4.8) | 21(4.4) | NA2 |
P-value indicates differences in respondent characteristics between African Americans and Whites and is obtained from Generalized Estimating Equations.
P-value indicates there is a differential effect over time (significant interaction of race by time) in which differences in characteristics vary across time. Therefore, no main effects model can be presented (calcium channel blocker p<.0001; diuretic combination therapy p=0.0059).
The distribution of consistent care and BP control by wave is presented in Table 4 and the odds ratios and 95% CI for the association between consistent care and blood pressure control are presented in Table 5. In crude analyses, participants with consistent care or inconsistent care had greater odds of BP control (OR=1.51, 95% CI: 1.24, 1.84 and OR=2.08, 95% CI: 1.67, 2.59) compared to those with no standard care. Additional adjustment for socio-demographic factors slightly attenuated the association for consistent (OR=1.26, 95% CI: 0.99, 1.59) and inconsistent care (OR=1.35, 95% CI: 1.03, 1.77). Inclusion of insurance, medical care satisfaction, and health history variables further attenuated these associations. Effect modification by race was not significant nor were there differences in BP control after adjustment for socio-demographic and health care variables (OR=1.06, 95% CI: 0.90, 1.24).
Table 4.
Blood pressure control status by consistency or care and wave, Piedmont Health Survey of the Elderly 1987-1998
| Wave 1 (1987) | Wave 2 (1990) | Wave 3 (1994) | Wave 4 (1998) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Consistent Care |
Inconsistent Care* |
No Care | Consistent Care |
Inconsistent Care |
No Care | Consistent Care |
Inconsistent Care |
No Care | Consistent Care |
Inconsistent Care |
No Care | |
| N=2,076 | N=0 | N=384 | N=1,611 | N=595 | N=217 | N=1,154 | N=704 | N=80 | N=743 | N=330 | N=24 | |
| BP Status, n(%) | ||||||||||||
| BP Controlled | 526(25.3) | -- | 71(18.5) | 671(41.7) | 167(28.1) | 70(32.3) | 441(38.2) | 184(26.1) | 22(27.5) | 307(41.3) | 131(39.7) | 10(41.7) |
| Stage 1 HTN | 974(46.9) | -- | 176(45.8) | 520(32.3) | 147(24.7) | 46(21.2) | 367(31.8) | 133(18.9) | 18(22.5) | 232(31.2) | 106(32.1) | 9(37.5) |
| Stage 2 HTN | 576(27.7) | -- | 137(35.7) | 361(22.4) | 92(15.5) | 52(24.0) | 317(27.5) | 120(17.0) | 18(22.5) | 171(23.0) | 70(21.2) | 5(20.8) |
| Missing | 0(0.0) | -- | 0(0.0) | 59(3.7) | 189(31.8) | 49(22.6) | 29(2.5) | 267(37.9) | 22(27.5) | 33(4.4) | 23(7.0) | 0(0.0) |
Inconsistent Care is not assessed at Wave 1 since the definition requires data from two or more time periods.
Table 5.
Odds ratios (OR) and 95% CI for the association between medical care receipt and blood pressure control among the elderly, Piedmont Health Survey of the Elderly 1987-1998
| Model* | Variable | OR | 95% CI |
|---|---|---|---|
| 1 | No Standard Care | 1.00 | |
| Inconsistent Care | 2.08 | (1.67, 2.59)**** | |
| Consistent Care | 1.51 | (1.24, 1.84)**** | |
| 2 | No Standard Care | 1.00 | |
| Inconsistent Care | 2.09 | (1.68, 2.60)**** | |
| Consistent Care | 1.54 | (1.26, 1.88)**** | |
| African American Race | 1.10 | (0.98, 1.23) | |
| 3 | No Standard Care | 1.00 | |
| Inconsistent Care | 1.41 | (1.12, 1.78)** | |
| Consistent Care | 1.34 | (1.09, 1.64)** | |
| African American Race | 1.10 | (0.98, 1.24)~ | |
| 4 | No Standard Care | 1.00 | |
| Inconsistent Care | 1.35 | (1.03, 1.77)* | |
| Consistent Care | 1.26 | (0.99, 1.59)~ | |
| African American Race | 1.04 | (0.90, 1.19) | |
| 5 | No Standard Care | 1.00 | |
| Inconsistent Care | 1.14 | (0.85, 1.52) | |
| Consistent Care | 1.00 | (0.78, 1.28) | |
| African American Race | 1.06 | (0.90, 1.24) | |
Model 1: Unadjusted
Model 2: Adjusted for race
Model 3: Adjusted for race, age at baseline, gender, and study year
Model 4: Adjusted for race, age at baseline, gender, and study year, marital status, work status, education, and income
Model 5: Adjusted for race, age at baseline, gender, and study year, marital status, work status, education, income, residence in a rural area, nursing home residence, Medicaid insurance, Medigap supplemental insurance, satisfaction with medical care, physical limitation, use of antihypertensive medication, and history of stroke, diabetes, heart disease, and cancer.
p<0.10
p<0.05
p<0.01
p<0.001
p<0.0001
DISCUSSION
In this population-based, observational study of hypertensive, elderly African Americans and whites, participants with consistent care or inconsistent care had greater odds of BP control compared to participants with no standard care over a 12 year period; however, these associations were attenuated after adjustment for socio-demographic and health care characteristics.
A previous study reported that consistent care was associated with recognition of hypertension and receipt of antihypertensive therapy among the elderly (7), while another study reported no association between consistent care and recognition of hypertension after adjustment for potential confounders (11). These findings for hypertension awareness could have implications for BP treatment and control, particularly among the elderly given that hypertension prevalence increases with age. In this prospective study of the elderly, an association between consistency of care and BP control was found, but this association was explained by health care characteristics and co-morbidities. This study's results are similar to findings from a cross-sectional study that reported that using the same health care facility or the same health care provider was associated with blood pressure control in the general population, although that study's association persisted even after adjustment for covariates (5).
Inconsistent care and no standard care were more common among African Americans than white participants in this study. No racial differences in BP control were found in this study, but the differences in receipt of physician care are notable given that African Americans had poorer demographic and health care characteristics. These adverse characteristics observed over time among African Americans compared to whites may affect health care outcomes, including blood pressure control, which requires long-term management. In this study, African Americans were significantly less likely than whites to have private supplemental health insurance, which helps to defray out-of-pocket costs, and lack of financial resources may be a barrier to hypertension management (12). Furthermore, African Americans' lack of satisfaction with prior care received may contribute to a lack of trust in the health care system and also deter healthcare-seeking behaviors (13-15).
This study has several limitations. The PHSE Study collected information about study participants during four visits over 12 years. Consistent care and blood pressure control were only assessed at these visits, so it is possible that participants had breaks in care or fluctuated between controlled and uncontrolled blood pressure which could not be evaluated in this study. Also, the definition of consistent care was limited in this study because participants were asked where they usually seek care and to name their physician. The definition of consistency of care used in this study is just one measure of the physician-patient care relationship. Other measures have been reported in the literature, such as continuity of care, usual source of care, and usual provider of care, and may be more specific than the definition used in this study because of the use of various indices, such as the usual provider of care index, which measures the number of visits to a usual provider divided by the total number of primary care visits (16). Consistent care is difficult to define because it is typically used to assess the various aspects of the interpersonal relationship between the physician and the patient (17, 18) in addition to encompassing other attributes such as extent of visit, knowledge, and environment (19). The definition of consistency of care for this study did not assess these different aspects of the physician-patient care relationship so some attributes of the relationship may not be captured in the definition used in this study. Also, this study did not have information about medication adherence by participants which is associated with BP control and may be affected by consistency of care. Another potential limitation to this study is the high attrition rate due to the advanced age of the participants. Attrition and missing data could bias results if they are not random, but there was no difference observed in a supplemental analysis. Also, the participants were mostly from rural areas of North Carolina, so these results may not be generalizable to other populations.
In summary, consistent and inconsistent care were associated with greater odds of BP control compared to no standard care in this prospective study of the elderly. African-American participants disproportionately received inconsistent or no standard care over the 12-year study period, although no racial differences were noted in BP control over time. Future studies should continue to explore the complexity of medical care relationships to identify factors that may affect blood pressure control among the elderly.
Acknowledgments
The study was funded by the Department of Health and Human Services Agency for Healthcare Research and Quality grant #R24 HS013353. Investigators were also funded, in part, by the National Institutes of Health National Center on Minority Health and Health Disparities grant #P60 MD000239.
Footnotes
We have no conflict of interest to report.
Publisher's Disclaimer: Note to NIH - Please include: The published version of this article can be accessed on the Journal of the American Board of Family Medicine website at: http://www.jabfm.org/cgi/reprint/22/3/307
REFERENCES
- 1.Cooper R, Rotimi C. Hypertension in blacks. Am J Hypertens. 1997;10(7 Pt 1):804–12. doi: 10.1016/s0895-7061(97)00211-2. [DOI] [PubMed] [Google Scholar]
- 2.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. Jama. 2003;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 3.McGruder HF, Malarcher AM, Antoine TL, et al. Racial and ethnic disparities in cardiovascular risk factors among stroke survivors: United States 1999 to 2001. Stroke. 2004;35(7):1557–61. doi: 10.1161/01.STR.0000130427.84114.50. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42(6):1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 5.He J, Muntner P, Chen J, et al. Factors associated with hypertension control in the general population of the United States. Arch Intern Med. 2002;162(9):1051–8. doi: 10.1001/archinte.162.9.1051. [DOI] [PubMed] [Google Scholar]
- 6.Saultz JW. Continuity of care. In: Saultz JW, editor. Textbook of Family Medicine. McGraw-Hill; New York, NY.: 2000. pp. 52–77. [Google Scholar]
- 7.Konrad TR, Howard DL, Edwards LJ, et al. Physician-patient racial concordance, continuity of care, and patterns of care for hypertension. Am J Public Health. 2005;95(12):2186–90. doi: 10.2105/AJPH.2004.046177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Psaty BM, Manolio TA, Smith NL, et al. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162(20):2325–32. doi: 10.1001/archinte.162.20.2325. [DOI] [PubMed] [Google Scholar]
- 9.Cornoni-Huntley J, Ostfeld AM, Taylor JO, et al. Established populations for epidemiologic studies of the elderly: study design and methodology. Aging (Milano) 1993;5(1):27–37. doi: 10.1007/BF03324123. [DOI] [PubMed] [Google Scholar]
- 10.Diggle PJ, Heagarty P, Liang KY, et al. Analysis of longitudinal data. 2nd ed. Oxford Press; New York: 2002. [Google Scholar]
- 11.Koopman RJ, Mainous AG, 3rd, Baker R, et al. Continuity of care and recognition of diabetes, hypertension, and hypercholesterolemia. Arch Intern Med. 2003;163(11):1357–61. doi: 10.1001/archinte.163.11.1357. [DOI] [PubMed] [Google Scholar]
- 12.Coleman MT, Lott JA, Sharma S. Use of continuous quality improvement to identify barriers in the management of hypertension. Am J Med Qual. 2000;15(2):72–7. doi: 10.1177/106286060001500206. [DOI] [PubMed] [Google Scholar]
- 13.Armstrong K, McMurphy S, Dean LT, et al. Differences in the Patterns of Health Care System Distrust Between Blacks and Whites. J Gen Intern Med. 2008 doi: 10.1007/s11606-008-0561-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004;53(9):721–30. [PubMed] [Google Scholar]
- 15.Blanchard J, Nayar S, Lurie N. Patient-provider and patient-staff racial concordance and perceptions of mistreatment in the health care setting. J Gen Intern Med. 2007;22(8):1184–9. doi: 10.1007/s11606-007-0210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Breslau N, Reeb KG. Continuity of care in a university-based practice. J Med Educ. 1975;50:965–969. doi: 10.1097/00001888-197510000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1(3):134–43. doi: 10.1370/afm.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159–66. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rogers J, Curtis P. The concept and measurement of continuity in primary care. Am J Public Health. 1980;70(2):122–7. doi: 10.2105/ajph.70.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]