Abstract
Objective
Physical Activity Across the Curriculum (PAAC) was a three-year cluster randomized controlled trial to promote physical activity and diminish increases in overweight and obesity in elementary school children.
Methods
Twenty-four elementary schools were cluster randomized to the PAAC intervention or served as control. All children in grades two and three were followed to grades four and five. PAAC promoted 90 minutes/wk of moderate to vigorous intensity physically active academic lessons delivered by classroom teachers. BMI was the primary outcome, daily PA and academic achievement were secondary outcomes.
Results
The three-year change in BMI for PAAC was 2.0 ± 1.9 and control 1.9 ± 1.9, respectively (NS). However, change in BMI from baseline to three years was significantly influenced by exposure to PAAC. Schools with ≥75 minutes of PAAC/wk showed significantly less increase in BMI at three years compared to schools that had <75 minutes of PAAC (1.8 ± 1.8 vs. 2.4 ± 2.0, p=0.02). PAAC schools had significantly greater changes in daily PA and academic achievement scores.
Conclusions
The PAAC approach may promote daily PA and academic achievement in elementary school children. Additionally, 75 minutes of PAAC activities may attenuate increases in BMI.
Introduction
Sedentary behavior is associated with increases in BMI and in turn, increased risk and comorbidities in children including the dramatic increase in type 2 diabetes (T2DM) (Daniels, et al., 2005, Steinberger and Daniels, 2003). Schools are an ideal site to intervene with children. Approximately 98% of children are enrolled in school (U.S. Census Bureau, 2006) and this provides access to children and enables repeated exposure to health promotion interventions (Goran, et al., 1999, Kann, et al., 2001). School policies can be modified and teachers and other personnel can be trained to deliver health promotion interventions. Schools offer continuity, so successful interventions may be sustained after the initial intervention and may be disseminated throughout school systems.
Unfortunately, schools may be a barrier for interventions to promote physical activity (PA). Children are required to sit quietly for the majority of the day to receive academic lessons. In a typical school day, this represents approximately six hours, and may be extended by 30 minutes or longer if the child is provided motorized transportation and does not actively commute to and from school. To increase PA in elementary school children, we designed and implemented a low cost, minimal intervention model that increased PA in the classroom. The intervention provided training for classroom teachers to deliver existing academic lessons taught thorough PA. In addition, we partnered with TAKE 10!, a program of the International Life Sciences Institute Research Foundation/Center for Health Promotion that promotes PA in the classroom. The combination of existing lessons from teachers and examples from Take 10! activities was termed “Physical Activity Across the Curriculum,” or “PAAC.”
The primary aim of PAAC was to increase PA sufficiently to reduce gains in BMI for PAAC compared to control schools. Secondary aims (sub-sample) were to assess changes in metabolic fitness, aerobic capacity, skinfolds, circumferences, lifestyle PA, diet intake, and academic achievement in children who received PAAC compared to control. Results for BMI, PA and academic achievement are presented in this paper. Results for other secondary outcomes have been published elsewhere (DuBose, et al., 2007, DuBose, et al., 2008, DuBose, et al., 2006, Eisenmann, et al., 2007, Gibson, et al., 2008).
Methods
Design
PAAC was a three-year, cluster randomized, controlled trial. Twenty-four elementary schools in Northeast Kansas were randomized to receive PAAC or to serve as control. Randomization was stratified by school size and rural versus urban location. PAAC promoted 90 minutes/wk of moderate to vigorous physically active academic lessons (3.0 to 6.0 METS,∼10 min each) delivered intermittently throughout the school day. Ninety minutes was chosen as the target since children were receiving 60 minutes of physical education per week and combined with PAAC lessons and this would total 150 minutes of PA per week which was consistent with recommendations from Healthy People 2010 (U.S. Department of Health and Human Services Public Health Service, 2000). The primary outcome was the difference in change in BMI from baseline to year three between PAAC and control schools. A sub-sample of volunteer participants was recruited from each school to measure the secondary outcomes.
Participants
Participants were in grades two and three at baseline and were in grades four and five at the end of the study. All students in the respective grades in the schools randomized to PAAC participated in PAAC since it was adopted as a curriculum. All students in the control schools received regular classroom instruction without physically active lessons. Written parental consent and child assent was obtained prior to participation in the sub-sample testing.
Classroom teacher training for implementation of PAAC
Training was provided to classroom teachers at each PAAC school in a six hour in-service at the beginning of each school year. Teachers who joined a school after the in-service received individual instruction. Teachers from PAAC schools who transferred to control schools were instructed not to use PAAC. The goal of in-service training was to develop competency and strategies to deliver 90 minutes of moderate to vigorous intensity, physically active PAAC lessons per week. Details of teacher training have been published previously (DuBose, et al., 2008, Gibson, et al., 2008).
Training of research assistants for teacher support and outcome testing
Research assistants (RA) were trained to support the classroom teachers in the design and delivery of PAAC, in trouble shooting, and problem solving strategies. RA who conducted testing were trained to collect valid and reliable data and had to obtain intraclass correlations of 0.90 or greater to be certified to administer each test. The exception was the academic achievement tests that were completed by a separate group of RA from a nearby university. Each RA for academic achievement was individually trained and certified by one of the investigators (JR).
Primary outcome (BMI)
Height and weight were obtained at the beginning and end of all three years with a stadiometer and digital scale accurate to ± 0.1 kg. Children were measured in private during the first period of the school day in t-shirts, shorts, and socks provided by the project staff. BMI percentiles were calculated using gender and age (Kuczmarski, et al., 2002).
Secondary outcomes (sub-sample only)
Sub-sample measures were obtained at baseline and at three years. Detailed descriptions of all sub-sample evaluations have been reported previously (DuBose, et al., 2008). Tests that are relevant to this paper are briefly described below.
Daily PA
From the sub-sample, a smaller sample of children (∼12 children/school) were randomly selected to wear an accelerometer (ActiGraph, 7163, Pensacola, FL) in the spring semester of each year. Accelerometers were worn over four consecutive days, which included two weekdays and two weekend days.
Academic achievement
Academic achievement for reading, writing, mathematics, and oral language skills was measured using the Wechsler Individual Achievement Test-2nd Edition (WIAT-II) (The Psychological Corporation, 2001). The standardization sample for the WIAT-II consisted of 5586 individuals who were representative of the U.S. population in terms of age, sex, race/ethnicity, grade, and geographic region during 1999 through 2001. The WIAT-II has excellent inter-scorer reliability (i.e., 0.94 to 0.98), internal consistency (e.g., by age-range from 0.89 to 0.98), and test-retest stability (e.g., for children 6 to 9 years of age, 0.92 to 0.98 over 7 to 45 days). Validity is supported via item reviews of curriculum experts and by correlations with other achievement tests (i.e., 0.52 to 0.89), measures of intelligence (i.e., 0.30 to 0.78), teacher evaluations (i.e., 0.45 to .064), and school grades (i.e., 0.29 to 0.57). The WIAT-II was individually administered during a 30-minute period. The WIAT-II produces an age based score that can be compared to show trends across time.
Implementation and Fidelity of PAAC
Extensive process evaluation measures were collected to monitor the extent to which the teachers delivered PAAC lessons as originally planned, to track the extent to which PAAC had been implemented, and to assess the levels of student and teacher PA during PAAC lessons across the school year. A detailed description of the process measures has been published elsewhere (Gibson, et al., 2008).
Direct Observations of classroom PA
Intensity of classroom PA was measured by a validated time-moment sampling procedure “System for Observation of Fitness Instruction Time,” (SOFIT) (McKenzie, et al., 1991). SOFIT is rated on a Likert scale from one to five anchored with lying down for one and very active (i.e. running) for five.
Blinding
RA were blinded to condition for measurement of the primary and secondary outcomes, and for data entry. RA who conducted classroom visitations were not blinded.
Randomization and power
A cluster randomized controlled design was used with school as the unit of randomization. Twenty-four schools were randomly assigned to treatment or control stratified by district and size. The primary endpoint of this study was change in BMI between the two treatments. The methods of Donner, et al. were used for sample size and power considerations (Donner and Klar, 2000). PAAC was powered with the assumptions of (1) a moderate ICC of 0.1; (2) a two-unit increase in BMI for control children with a standard deviation of 1.5; and (3) a 1.5-unit increase in BMI for intervention children with a standard deviation of 1.5 across three years. The power to detect these differences was >0.80.
Statistical Analysis
An adjusted t-test (Donner and Klar, 2000), which accounts for the intraclass correlation, was used to assess change in BMI from baseline to 3 years. Change in BMI was also analyzed longitudinally, using a linear mixed model with an autoregressive type 1 covariance structure for the longitudinal measurements over time and compound symmetric covariance structure for the intraclass correlation within schools, also adjusting for gender. SOFIT data were compared between treatment groups using a mixed linear model adjusting for grade, semester, and gender. The effects of teacher modeling on SOFIT scores were analyzed using ANOVA. Demographic data were summarized descriptively, using means and standard deviations for continuous data and frequencies and percentages for categorical data. Change from baseline to end of study was analyzed using an adjusted t-test (Donner and Klar, 2000) and a linear mixed model was used to analyze longitudinal data over time. Data in the sub-sample were analyzed in a similar fashion to the main outcome. All quantitative analyses were done using SAS version 9.1 (SAS Institute, Inc., Cary, NC, USA).
Results
Participants
Twenty-six elementary schools were initially randomly assigned to PAAC or control. Two schools (8%) discontinued participation; one due to closing of the school and one refused randomization to control. Twenty four schools completed the study; 14 PAAC and ten control. At baseline, there were 1,527 participants, 814 in PAAC schools and 713 in control schools. Boys comprised 48.8% and girls 51.7% of participants. At year three, there were 1,490 participants for attrition rate of 2.5%. Participants were 77.4% Caucasian, 6.2% African American, 10.1% Hispanic, 1.6% Native American, 1.2% Asian, and 3.6% Multi-Ethnic. Forty three percent of participants qualified for free or reduced lunch. Baseline BMI for the PAAC schools was 17.9 ± 3.1 and 18.0 ± 3.7 for control schools (NS). Age, height, weight, and BMI at baseline are shown by grade and gender in Table 1. The sub-sample (N=454) for outcomes shown in this paper was comprised of 195 (42.9%) boys and 259 (57.1%) girls, of which 15.3% were from ethnic groups.
Table 1.
Baseline Demographics by Grade, Gender, and Intervention Group (University of Kansas, 2003-2006)
| Control | PAAC | |||
|---|---|---|---|---|
| BMI (kg/m2) | Grade 2 | Female | 17.4 (3.0) | 17.7 (3.0) |
| Male | 17.5 (3.1) | 17.7 (3.0) | ||
| Grade 3 | Female | 18.7 (3.8) | 18.4 (3.4) | |
| Male | 18.6 (4.0) | 18.1 (3.4) | ||
| Age (y) | Grade 2 | Female | 7.8 (0.4) | 7.7 (0.3) |
| Male | 7.8 (0.3) | 7.7 (0.4) | ||
| Grade 3 | Female | 8.7 (0.4) | 8.7 (0.4) | |
| Male | 8.8 (0.4) | 8.7 (0.3) | ||
| Height (cm) | Grade 2 | Female | 126.6 (5.6) | 125.6 (5.6) |
| Male | 127.3 (6.4) | 127.3 (6.2) | ||
| Grade 3 | Female | 132.1 (6.5) | 131.9 (6.2) | |
| Male | 132.9 (6.2) | 132.4 (6.4) | ||
| Weight (kg) | Grade 2 | Female | 28.2 (6.5) | 28.3 (6.5) |
| Male | 28.6 (7.3) | 28.9 (6.8) | ||
| Grade 3 | Female | 33.0 (9.5) | 32.2 (7.6) | |
| Male | 33.1 (9.1) | 32.1 (8.3) |
Values are mean (SD). There were no significant differences between PAAC and Control.
Primary outcome-BMI
There were no significant differences for change in BMI or BMI percentile (baseline to year three) for PAAC vs. control and this finding was not influenced by gender. (Table 2). However, change in BMI from baseline to three years was significantly influenced by exposure to PAAC. As minutes of exposure increased, the change in BMI decreased (Figure 1). Schools (N=9) with ≥75 minutes of PAAC/wk showed significantly less increase in BMI at 3 years compared to schools (N=5) with < 75 minutes of PAAC/wk (1.8 ± 1.8 vs. 2.4 ± 2.0; p=0.02).
Table 2.
BMI change from baseline (University of Kansas, 2003-2006)
| Semester | Control | n | PAAC | n | P-value |
|---|---|---|---|---|---|
| Fall 2003 | 18.0 (3.7) | 713 | 17.9 (3.1) | 814 | |
| Spring 2006 | 20.0 (4.6) | 698 | 19.9 (4.1) | 792 | |
| Change from Baseline | 2.0 (1.9) | 2.0 (1.9) | 0.83 |
Values are means (SD).
Figure 1.
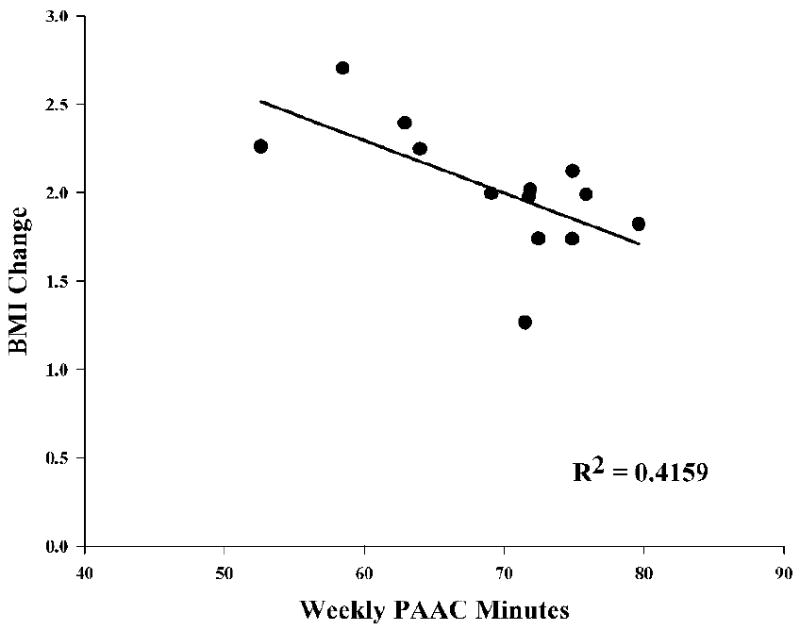
Correlation between BMI change and the average weekly PAAC minutes reported by each elementary school in northeast Kansas(2003-2006).
We examined shifts in BMI percentiles from baseline to year three. In children at risk for obesity at baseline (BMI≥85%), 21.8% moved to normal BMI (BMI<85%) in the PAAC group compared to 16.8% in the control group (NS), and 22.6% in the PAAC group compared to 31.1% in the control group moved to overweight (BMI≥95; NS). For children who were overweight at baseline, 17.1% of the PAAC group compared to 8.3% of the control group moved to at risk (p=0.08).
Secondary outcomes (sub-sample)
There were no significant differences at baseline between PAAC and control in the sub-sample for any variable.
Daily PA
A random sample (n = 77 PAAC, n = 90 control) from the PAAC sub-sample completed four consecutive days (Thursday-Sunday) of PA monitoring by accelerometer during the spring semester of each of the three intervention years. Results indicated that on average over the three year intervention, children in PAAC schools had greater PA (13% >) compared to children in control schools (Table 3). Children in PAAC schools had significantly greater levels of PA during the school day (12%>) and on weekends (17%>) and also exhibited greater levels of PA on weekdays (8%>, p = 0.05) compared to children in control schools. Children in PAAC schools also exhibited 27% greater levels of moderate to vigorous intensity PA (≥ 4 METS) compared to children in control schools.
Table 3.
Mean Accelerometer Counts/min (University of Kansas, 2003-2006)
| Accelerometer Periods | Control (n=90) | PAAC (n=77) | P* |
|---|---|---|---|
| 4-day Average | 744 (183) | 851 (233) | 0.007 |
| Weekday | 738 (192) | 800 (222) | NS |
| Weekend day | 750 (219) | 901 (279) | 0.001 |
| During School (8AM – 2:59PM) | 606 (205) | 688 (199) | 0.01 |
| After School (3PM – 5:59PM) | 946 (332) | 1,017 (365) | NS |
| Evening (6PM-11PM) | 812 (349) | 891 (361) | NS |
| Minutes of MVPA (≥4 METs) | 72 (36.5) | 98 (42.7) | 0.001 |
Values are means (SD) taken from 4 day averages. NS, Non-Significant. MVPA, Moderate-vigorous physical activity. MET, Metabolic equivalent.
Controlling for gender, race, ethnicity, cohort.
Academic achievement
Significant improvements in academic achievement from baseline to three years were observed in the PAAC compared to the control schools for the composite, reading, math, and spelling, scores (Figure 2).
Figure 2.
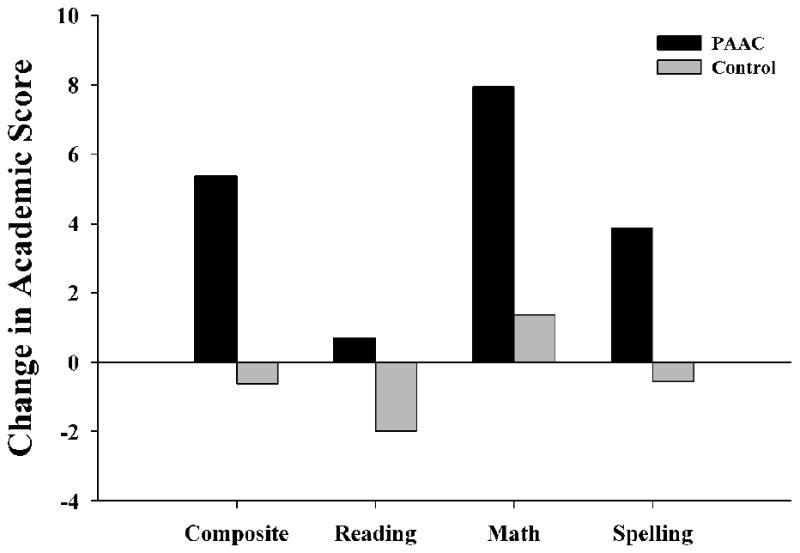
Change in academic score baseline to 3 years in elementary schools in northeast Kansas (2003-2006). All between group differences were significant (p<0.01). PAAC (n=l17). Control (n=86).
Process Measures
Delivery of PAAC Lessons
The majority of teachers indicated that they incorporated PA primarily into language arts and mathematics. Teacher reports of the number of minutes of PA performed each week were averaged each month and ranged from 45 minutes to ≥75 minutes per week. Nine of 14 PAAC schools averaged ≥75 minutes per week. The average number of minutes of PA were lowest at the beginning of each semester and increased significantly within each year, and across years from baseline to the end of year three (p<0.0001).
Intensity of PAAC Lessons
The average scores across the intervention showed a value of 3.4 ± 0.46 for PAAC schools compared to 2.1 ± 0.19 in control schools (p=0.0001). SOFIT scores were consistent within and across school years showing little fluctuation. Average SOFIT scores were statistically different across grade level with grades four and five lower than grades two and three (p=0.0001), although the small differences may not have practical importance.
Teacher participation in classroom activity (modeling)
Teacher participation in classroom PA was directly related to PA levels measured by SOFIT. Teachers who themselves were more physically active had students who were also more physically active (p<0.001).
Discussion
We found no significant difference for change in BMI over 3 years for children in PAAC compared with control schools. Our findings are in agreement with a number of other school based trials that evaluated the impact of PA on BMI. For example, there were no significant differences found for change in BMI between PAAC and control schools in either the CATCH (Luepker, et al., 1996) or SPARK trials (Sallis, et al., 1993). Others have used shifts in BMI categories as the choice of analysis to determine the effect of interventions on overweight and obesity (Spiegel and Foulk, 2006). Interestingly, when we compared shifts in BMI categories we found each change in a positive direction for PAAC compared to controls and the change for overweight to at-risk approached significance (p=0.08).
Results for change in BMI were shown to be influenced by exposure to PAAC. Schools that delivered ≥75 minutes of PAAC lessons/wk had significantly smaller increases in BMI compared to schools that received <75 minutes. In addition to increasing the minutes of PAAC, total energy expenditure might be increased by increasing the intensity of PAAC activities.
Gutin has recently demonstrated decreases in weight and fat mass in response to higher rather than lower intensity PA in adolescents (Gutin, 2008). This strategy would not require an increase in the time devoted to PAAC activities, yet it would increase energy expenditure. Most PAAC activities were on the order of 1.4 - 5.2 kcal/min (avg. = 3.4 ± 0.5 METS) as measured by indirect calorimetry (Honas, et al., 2008). However ∼ 61% of PAAC activities are greater than 3.0 METs. The average energy expenditure of activities greater than 3.0 METs was 3.73 kcal/min (∼4.0 METS). The preferential use of the activities with greater energy expenditure may increase the total energy expenditure delivered in the PAAC lessons. In turn, this may increase the effectiveness of PAAC activities to attenuate increases in BMI over time.
Teachers who modeled PA by active participation in the PAAC lesson had greater SOFIT scores shown by their students compared to students with teachers at lower levels of modeling. Modeling desired behaviors by a person significant to the targeted individual is frequently associated with greater achievement of that behavior (Bandura, 1986, Smith, et al., 1988). Modeling by teachers may be an important mediator of PA in children and strategies to remove classroom barriers and increased teacher modeling should be emphasized in future studies.
Daily PA was significantly increased in PAAC children compared to controls. As expected, PA was increased during the school day, due to exposure to PAAC. The week day daily average as well as the weekend day average were significantly greater for PAAC compared to control children. Minutes of moderate to vigorous intensity PA were greater for PAAC compared to control and may be important since this level of PA is known to increase fitness and decrease risk factors for chronic disease in children (Gutin, et al., 2002, Gutin, et al., 2005, Owens, et al., 1999). The greater weekend PA for PAAC participants compared to control is particularly interesting. This could be explained by a change in children's attitudes and beliefs fostered by the PAAC intervention that they can be physically active anywhere and during almost any situation rather than relying on the need for a formal PA opportunity, although this is speculative and should be tested further.
Academic achievement was significantly improved with exposure to PAAC. Foremost, this finding affirms that PAAC did not interfere with learning. Carlson et al. recently reported findings from a fove year cohort investigation that followed kindergarten students through fifth grade and compared the amount of physical education received to academic achievement (Carlson, et al., 2008). The major conclusion was that physical education did not have adverse effects on academic achievement and limiting physical education to avoid adverse effects on learning does not appear to be legitimate. This conclusion was corroborated in a systematic review of PA and academic performance by Trudeau and Shephard (Trudeau and Shephard, 2008). Suggested mechanisms for the association between PA and academic performance included concentration, memory, cognitive processing, and classroom behavior. For example, Davis et al. (Davis, et al., 2007), recently reported increases in executive function that resulted from 15 weeks of aerobic exercise training in overweight children (85th%). Children who received aerobic exercise of 40 min/day showed higher scores for executive function compared to controls. Potential mechanisms for the association of PA and improvements in academic performance need further exploration in studies designed and powered for this purpose.
Most investigations of PA and academic achievement have used cross-sectional, correlational data between academic achievement and fitness tests (California Dept of Ed, 2001, Castelli, et al., 2007, Coe, et al., 2006). Our results are from a longitudinal, randomized, controlled trial and compared PA (not fitness) to academic achievement. These important findings require confirmation as they may have a profound impact on school administrators and teachers and their perception of PA in the classroom. The positive influence of PAAC on academic achievement may influence whether such a program will be received favorably and supported school-wide given the current climate centered on academic performance generated by the No Child Left Behind Act of 2001.
Few research studies have the resources to ensure that their interventions can be sustained (Bull, et al., 2003, Oldenburg, et al., 1999). We designed PAAC to be a low burden, minimal cost intervention that would not decrease academic instruction time, would not increase teacher preparation time, and would be enjoyable for students, teachers, and staff. PAAC was well received by children, teachers, and administration according to the results from process analysis and focus groups. Importantly, the acceptance and enthusiasm for PAAC was corroborated by findings from a post intervention survey administered to PAAC teachers in an effort to determine if PAAC was continued in the absence of the investigators. Teachers were surveyed ∼nine months after completion of PAAC and without any contact from our staff over the nine month period. Approximately 95% of teachers indicated they were using PAAC lessons one day/wk or more. Approximately 55% of teachers indicated they were using PAAC two to four days/wk, ∼35% were using PAAC on most days or every day, and only 5% were not using PAAC lessons. Although teachers indicated continued use of PAAC, these results are limited by self-report and should be objectively verified in any future studies. Additionally, twenty percent of school days were not centered on academic instruction due to assembly, field trips, etc. and this diminished the exposure to PAAC. Strategies are needed to plan for these disruptions in academic instruction to better assure the intended level of PAAC activities are delivered.
In summary, we found that greater levels of exposure to PAAC lessons were associated with smaller increases in BMI and favorable shifts in BMI percentile. Children who received PAAC were more physically active across 24 hours and on weekends compared to children who did not receive PAAC. There was a positive association between teacher modeling of PAAC lessons and the level of PA achieved by the children. There was a very intriguing, positive, and important outcome for academic achievement for those children who received PAAC compared to controls. Sixty four percent of PAAC schools were able to average ≥75 minutes PAAC activities across the intervention period. This, combined with the observation that PAAC has been sustained by teachers without any further contact by the investigators, speaks to the overall favorable perception and acceptance for the PAAC approach by both teachers and school administrators. Continued research is needed to develop and evaluate strategies to provide greater exposure to PAAC lessons since exposure was associated with attenuated increases in BMI. Furthermore the important secondary outcomes for increased daily PA and academic achievement deserve pursuit in adequately powered and designed studies.
Acknowledgments
This work was supported by grant NIH NIDDK R01 061489 from the National Institute of Diabetes and Digestive and Kidney Disease, Bethesda, MD. The authors would like to thank the International Life Sciences Institute for Health Promotion for educational materials. The authors are grateful to all students and teachers who participated in our project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall; Englewood Cliffs, New Jersey: 1986. [Google Scholar]
- Bull SS, Gillette C, Glasgow RE, Estabrooks P. Work site health promotion research: to what extent can we generalize the results and what is needed to translate research to practice? Health Educ Behav. 2003;30:537–49. doi: 10.1177/1090198103254340. [DOI] [PubMed] [Google Scholar]
- California Dept of Ed. California physical fitness test: Report to the governor and legislature. California Department of Education Standards and Assessment Division; Sacramento, CA: 2001. [Google Scholar]
- Carlson SA, Fulton JE, Lee SM, Maynard LM, Brown DR, Kohl HW, 3rd, Dietz WH. Physical education and academic achievement in elementary school: data from the early childhood longitudinal study. Am J Public Health. 2008;98:721–7. doi: 10.2105/AJPH.2007.117176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castelli DM, Hillman CH, Buck SM, Erwin HE. Physical fitness and academic achievement in third- and fifth-grade students. J Sport Exerc Psychol. 2007;29:239–52. doi: 10.1123/jsep.29.2.239. [DOI] [PubMed] [Google Scholar]
- Coe DP, Pivarnik JM, Womack CJ, Reeves MJ, Malina RM. Effect of physical education and activity levels on academic achievement in children. Med Sci Sports Exerc. 2006;38:1515–9. doi: 10.1249/01.mss.0000227537.13175.1b. [DOI] [PubMed] [Google Scholar]
- Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, Robinson TN, Scott BJ, St Jeor S, Williams CL. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- Davis CL, Tomporowski PD, Boyle CA, Waller JL, Miller PH, Naglieri JA, Gregoski M. Effects of aerobic exercise on overweight children's cognitive functioning: a randomized controlled trial. Res Q Exerc Sport. 2007;78:510–9. doi: 10.1080/02701367.2007.10599450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donner A, Klar N. Design and analysis of cluster randomized trials in health research. Arnold Publishers; London: 2000. [Google Scholar]
- DuBose KD, Eisenmann JC, Donnelly JE. Aerobic fitness attenuates the metabolic syndrome score in normal-weight, at-risk-for-overweight, and overweight children. Pediatrics. 2007;120:e1262–8. doi: 10.1542/peds.2007-0443. [DOI] [PubMed] [Google Scholar]
- DuBose KD, Mayo MS, Gibson CA, Green JL, Hill JO, Jacobsen DJ, Smith BK, Sullivan DK, Washburn RA, Donnelly JE. Physical activity across the curriculum (PAAC): rationale and design. Contemp Clin Trials. 2008;29:83–93. doi: 10.1016/j.cct.2007.05.004. [DOI] [PubMed] [Google Scholar]
- DuBose KD, Stewart EE, Charbonneau SR, Mayo MS, Donnelly JE. Prevalence of the metabolic syndrome in elementary school children. Acta Paediatr. 2006;95:1005–11. doi: 10.1080/08035250600570553. [DOI] [PubMed] [Google Scholar]
- Eisenmann JC, DuBose KD, Donnelly JE. Fatness, fitness, and insulin sensitivity among 7- to 9-year-old children. Obesity. 2007;15:2135–44. doi: 10.1038/oby.2007.254. [DOI] [PubMed] [Google Scholar]
- Gibson CA, Smith BK, Dubose KD, Greene JL, Bailey BW, Williams SL, Ryan JJ, Schmelzle KH, Washburn RA, Sullivan DK, Mayo MS, Donnelly JE. Physical activity across the curriculum: year one process evaluation results. Int J Behav Nutr Phys Act. 2008;5:36. doi: 10.1186/1479-5868-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goran MI, Reynolds K, Lindroos AK. Role of physical activity in the prevention of obesity in children. Int J Obes. 1999;23:s18–s33. doi: 10.1038/sj.ijo.0800880. [DOI] [PubMed] [Google Scholar]
- Gutin B. Child obesity can be reduced with vigorous activity rather than restriction of energy intake. Obesity (Silver Spring) 2008;16:2193–6. doi: 10.1038/oby.2008.348. [DOI] [PubMed] [Google Scholar]
- Gutin B, Barbeau P, Owens S, Lemmon CR, Bauman M, Allison J, Kang HS, Litaker MS. Effects of exercise intensity on cardiovascular fitness, total body composition, and visceral adiposity of obese adolescents. Am J Clin Nutr. 2002;75:818–826. doi: 10.1093/ajcn/75.5.818. [DOI] [PubMed] [Google Scholar]
- Gutin B, Yin Z, Humphries MC, Barbeau P. Relations of moderate and vigorous physical activity to fitness and fatness in adolescents. Am J Clin Nutr. 2005;81:746–50. doi: 10.1093/ajcn/81.4.746. [DOI] [PubMed] [Google Scholar]
- Honas JJ, Washburn RA, Smith BK, Greene JL, Donnelly JE. Energy expenditure of the physical activity across the curriculum intervention. Med Sci Sports Exerc. 2008;40:1501–5. doi: 10.1249/MSS.0b013e31816d6591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kann L, Brener ND, Allensworth DD. Health education: results from the School Health Policies and Programs Study 2000. J Sch Health. 2001;71:266–78. doi: 10.1111/j.1746-1561.2001.tb03504.x. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, Wei R, Curtin LR, Roche AF, Johnson CL. 2000 CDC Growth Charts for the United States: Methods and Development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- Luepker RV, Perry CL, McKinlay SM, Nader PR, Parcel GS, Stone EJ, Webber LS, Elder JP, Feldman HA, Johnson CC, Kelder SH, Wu M. Outcomes of a field trial to improve children's dietary patterns and physical activity - The Child and Adolescent Trial for Cardiovascular Health (CATCH) JAMA. 1996;275(10):768–776. doi: 10.1001/jama.1996.03530340032026. [DOI] [PubMed] [Google Scholar]
- McKenzie TL, Sallis JF, Nader PR. SOFIT: system for observing fitness instruction time. J Teach Phys Educ. 1991;11:195–205. [Google Scholar]
- Oldenburg BF, Sallis JF, Ffrench ML, Owen N. Health promotion research and the diffusion and institutionalization of interventions. Health Educ Res. 1999;14:121–30. doi: 10.1093/her/14.1.121. [DOI] [PubMed] [Google Scholar]
- Owens S, Gutin B, Allison J, Riggs S, Ferguson M, Litaker M, Thompson W. Effect of physical training on total and visceral fat in obese children. Med Sci Sports Exerc. 1999;31:143–8. doi: 10.1097/00005768-199901000-00022. [DOI] [PubMed] [Google Scholar]
- Sallis JF, McKenzie TL, Alcaraz JE, Kolody B, Hovell MF, Nader PR. Project SPARK. Effects of physical education on adiposity in children. Ann N Y Acad Sci. 1993;699:127–36. doi: 10.1111/j.1749-6632.1993.tb18844.x. [DOI] [PubMed] [Google Scholar]
- Smith DW, Bibeau DL, Altschuld JW, Heit P. Health-related characteristics of selected school principals. J Sch Health. 1988;58:397–400. doi: 10.1111/j.1746-1561.1988.tb05812.x. [DOI] [PubMed] [Google Scholar]
- Spiegel SA, Foulk D. Reducing overweight through a multidisciplinary school-based intervention. Obesity (Silver Spring) 2006;14:88–96. doi: 10.1038/oby.2006.11. [DOI] [PubMed] [Google Scholar]
- Steinberger J, Daniels SR. Obesity, insulin resistance, diabetes, and cardiovascular risk in children - An American Heart Association scientific statement from the Atherosclerosis, Hypertension, and Obesity in the Young Committee (Council on Cardiovascular Disease in the Young) and the Diabetes Committee (Council on Nutrition, Physical Activity, and Metabolism) Circulation. 2003;107:1448–1453. doi: 10.1161/01.cir.0000060923.07573.f2. [DOI] [PubMed] [Google Scholar]
- The Psychological Corporation. WIAT-II: Wechsler individual achievement test. San Antonio: 2001. [Google Scholar]
- Trudeau F, Shephard RJ. Physical education, school physical activity, school sports and academic performance. Int J Behav Nutr Phys Act. 2008;5:10. doi: 10.1186/1479-5868-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. Current Population Survey. Housing and Household Economic Statistics Division; 2006. [Google Scholar]
- U.S. Department of Health and Human Services Public Health Service. Healthy People 2010. Vol. 2. Washington D.C.: 2000. [Google Scholar]


