Abstract
Objective
The authors detail the public health need for depression prevention research and the decisions made in designing an experiment testing problem solving therapy as “indicated” preventive intervention for high-risk older adults with subsyndromal depression. Special attention is given to the recruitment of African Americans because of well-documented inequalities in mental health services and depression treatment outcomes between races.
Methods
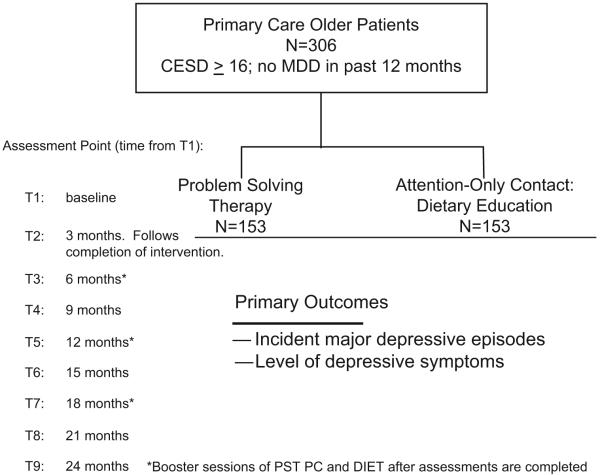
A total of 306 subjects (half white, half African American) with scores of 16 or higher on the Center for Epidemiological Studies of Depression Scale, but with no history of major depressive disorder in the past 12 months, are being recruited and randomly assigned to either problem solving therapy-primary care or to a dietary education control condition. Time to, and rate of, incident episodes of major depressive disorder are to be modeled using survival analysis. Level of depressive symptoms will be analyzed via a mixed models approach.
Results
Twenty-two subjects have been recruited into the study, and to date eight have completed the randomly assigned intervention and postintervention assessment. Four of 22 have exited after developing major depressive episodes. None have complained about study procedures or demands. Implementation in a variety of community settings is going well.
Conclusion
The data collected to date support the feasibility of translating from epidemiology to RCT design and implementation of empirical depression prevention research in later life.
Keywords: Depression prevention, indicated preventive intervention, elderly, African American, translation
Depression affects 15%-20% of adults at any one point in time and is associated with high rates of morbidity and mortality.1 Within the primary care setting, prevalence estimates of late-life major depression range between 6% and 9%.1,2 An additional 17%-37% of individuals suffer from milder yet clinically relevant symptoms.1 Because they do not qualify for “major depression” under Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria, their symptoms are often misdiagnosed, ignored, or inadequately treated, resulting in lack of appropriate surveillance or intervention.2 Elderly with depressive symptoms but not depressive disorder per se have functioning comparable to or poorer than those with chronic medical conditions, such as heart and lung disease, arthritis, and diabetes3 and are at risk for developing full-blown major depressive episodes.4 Moreover, treatment is often inadequate in relieving the burden of depressive illness in old age. Although National Institute of Mental Health cites treatment efficacy rates of at least 80% for patients with major depression (if patients are provided appropriate treatment), the National Comorbidity Survey Replication found an adequate treatment rate of only 42% among patients.5 Two large-scale studies, IMPACT and PROSPECT, using collaborative care management in primary care, found that less than half of older patients with major depression who underwent intervention experienced a 50% reduction in depressive symptoms.6,7 In the IMPACT study, only about one-quarter of patients became completely free of depressive symptoms.6 Similarly, Andrews et al.8 estimate that under optimal evidence-based depression treatment only 34% of years lived with disability could be averted. The limitations of treatment, even under optimal conditions, point to a need to develop public-health relevant approaches to prevent depression in high-risk elderly people.
Why “Indicated” Rather Than “Selective” or
“Universal” Prevention of Depression?
The Institute of Medicine has addressed this need by calling for increased research on “indicated” preventive interventions,9 which target higher-risk persons who already have detectable signs of disorder but do not yet meet diagnostic criteria for the disorder.9 Schoevers et al.10 conducted a systematic analysis of risk factors to determine whether selective or indicated prevention strategies were more “efficient.” “Efficiency” comprises both the impact of the intervention and effort required to implement it. “Impact” is reflected in the epidemiological term attributable fraction (the proportion of cases that would be prevented in the population if the adverse effect of the targeted risk factor were completely blocked). “Effort” is reflected in number needed to treat (NNT, the number of patients who would need to receive a preventive intervention to avoid one new case of late-life depression). Ideally, the risk factors targeted would have a high attributable fraction, indicating a large decrease in the incidence of depression if the intervention were 100% effective and a low NNT, indicating a low effort to realize a health gain in the population.11 Schoevers et al.10 determined that the risk factor with the combination of highest attributable fraction and lowest NNT was “subsyndromal” depression; suggesting that “indicated” prevention of depression (which targets people with mild symptoms) is preferable to selective prevention (which targets asymptomatic but at-risk people).
The lack of randomized controlled trials on this subject begs the question of which intervention to use. Antidepressant medications are often prescribed at insufficient dosages and inadequate lengths of time, and a large percentage of elderly patients are nonadherent to antidepressant therapy.12 Older primary care patients also prefer counseling to medication for depression treatment, especially African Americans.13 It would most likely be even more difficult to get nondepressed patients to take antidepressant medication, thus making psychosocial strategies a more suitable preventive intervention.14 However, few effective counseling strategies are practicable within primary care due to time constraints and lack of available expertise. Moreover, because of stigma, most elderly primary-care patients prefer to be treated by nonmental health specialists in primary-care settings.15 Problem solving therapy-primary care (PST-PC) is an intervention that is brief, has shown antidepressant efficacy, and can be administered by properly trained nonmental health specialists (e.g., medical nurses) in primary care.16 Although one study examined selective preventive intervention using PST-PC in older adults with age-dependent macular degeneration,17 we are not aware of any studies that examine its use for indicated prevention.
Why Focus on Older African Americans?
Race or ethnicity issues are of high public health importance in our increasingly diverse population. The need to oversample African Americans for depression prevention research arises because inequalities in the treatment of depression continue to grow.18 Although all patients face barriers to successful depression treatment, these barriers are greater for older patients and particularly, older black patients and those with few economic resources. These patients receive mental health care predominantly from their primary care physicians (if at all) and are reluctant to accept referrals to mental health specialists because of logistic and personal factors, including stigma. Many black patients deal with unique issues of trust and stigma on the patient level, lack of cultural sensitivity and racism on the provider level, and institutional discrimination and a shortage of like-ethnic providers on the systems level. Their depression is less likely to be identified and formally diagnosed,13,19 confirming a well-documented bias in clinical judgment.20,21 Even when depression is diagnosed, treatment may differ: most but not all studies demonstrate a lower rate of treatment for depression in younger and older black persons than in white persons. Furthermore, even when recognized and treated, black patients may be less likely to remain engaged in mental health treatment.22,23 Thus, to circumvent these disparities in mental health services, it is necessary to develop preventive interventions that address these issues and that are practical, culturally appropriate, and sustainable.
We have hypothesized that PST-PC will be superior to an education-only control (dietary education: DIET) in lowering the 2-year incidence of episodes of syndromal major depression in already symptomatic elderly subjects. We plan to explore whether race predicts or moderates the strength of PST-PC’s hypothesized preventive efficacy. In this article we describe 1) our translation of the concept of indicated preventive intervention into an experimental design, 2) early pilot, feasibility, or acceptability data, and 3) protocol modifications made as a result of this experience.
EXPERIMENTAL DESIGN: METHODS AND LOGIC OF KEY CHOICES
Our recruitment strategies encompass referrals from primary care practice settings, the Healthy Black Family Project (HBFP), Institutional Review Board (IRB)-approved advertisements in print and on-air media, use of research registries, and presentations to lay groups of elderly and their families. HBFP is a program designed and staffed by the Center for Minority Health at Pittsburgh, PA’s Graduate School of Public Health. It sponsors programs in life style modification to manage hypertension and diabetes in Pittsburgh, PA’s predominantly African American neighborhoods. Activities include health-risk assessments, screening for symptoms of depression, family health history screenings, and sessions with health coaches trained in exercise, nutrition, and stress management. By partnering with HBFP, we address barriers that have hindered minority recruitment and participation in mental health research. HBFP recruitment uses the Center for Epidemiological Studies Depression (CES-D) Scale24 as part of the annual health screening of participants in to identify symptomatic individuals.
Using strategies from our earlier PROSPECT study,7 recruitment from primary care involves sending a letter signed by primary care physicians (PCPs) to patients with an upcoming scheduled appointment. The letter indicates that their physician is participating in the study and encourages patients to participate in telephone screening. Patients accepting telephone calls from study staff are asked to provide verbal consent for answering screening questions, from the CES-D. Interested subjects who screen positive are scheduled for a diagnostic evaluation via the Structured Clinical Interview for DSM-III-R (SCID)7 and informed as to whether they meet eligibility for inclusion in the study.
The inclusion criteria require that subjects a) be age 50 years or older, b) have a CES-D24 score of 16 or greater, c) have a Folstein Minimental state25 score of 24 or higher, d) are not currently receiving antidepressant medication or participating in other mental health treatment, and e) are willing to provide informed consent. Because this study is a prevention trial, we exclude participants who have had a) an episode of major depression within the past 12 months, b) an episode of alcohol or other substance abuse within the past 12 months c) a lifetime history of bipolar disorder or other psychotic disorder, and d) a diagnosis of any neurodegenerative disorder or of dementia. We acknowledge that exclusion of persons with current alcohol abuse or dependence could constrain the external validity or generalizability of study results. We are tracking and intend to report the numbers of people excluded for this reason. We think that people with current comorbid alcohol abuse or dependence need treatment beyond the prevention purview of this study.
A CES-D score of 16 or greater was chosen as inclusion criteria because our pilot study indicated that this score provided optimal sensitivity and specificity for identifying participants in the PROSPECT7 study who were not currently depressed but would go on to develop major depression at 2-year followup. Approximately 25% of such subjects did so. We have also lowered the age of entry into the study from 60 to 50 at the request of community partners to ease the recruitment process and to capture participants in their 50s already living with risk factors for depression (subsydromal symptoms, disability, care giving burden, social isolation, chronic pain, bereavement, or insomnia). Black patients are being oversampled (153 of 306 participants) to recruit a racially balanced sample that will allow us to explore race as a predictor or moderator of PST-PC’s hypothesized prevention efficacy. White subjects are being recruited from practices that care for medically indigent patients to empanel a group comparable to black subjects in socioeconomic status.
After screening, subjects who meet study inclusion or exclusion criteria and who provide informed consent are stratified by sex, race, site and, previous history of major depression (yes or no). They are then randomly assigned to either PST-PC or to DIET.
By design, our recruitment strategy yields a heterogeneous sample: thus, some patients have already experienced major depressive episodes in the past, and for them the study tests the efficacy of PST-PC to prevent recurrence. Others have no history of depression, as best we can tell; for them, the study tests PST-PC’s efficacy to prevent initial or first episodes. Because those with prior episodes are probably at higher risk, we stratify the randomization by presence or absence of previous episodes of major depression.
INTERVENTIONS: RATIONALE AND CONTENT
PST-PC is a behavioral treatment for depression in primary care that teaches problem-solving orientation and skills. As shown in IMPACT, it is a manual-driven intervention that is effective for late-life depression.6 PST-PC involves the patient and therapist working through a prescribed process for problem-solving: selecting and defining a problem as presented by the patient, setting a realistic goal, evaluating the advantages and disadvantages of each solution, brainstorming solutions to reach that goal, choosing a preferred solution, and developing a concrete plan for implementing and evaluating outcomes.16 Through PST-PC, patients learn to solve problems as well as develop a positive problem-solving orientation, which comprises the beliefs and expectations one has regarding life’s problems.26 Specifically, a positive problem orientation consists of acceptance of problems as a normal part of life; belief in one’s ability to solve problems (“self-efficacy”); labeling of anxiety, sadness, and physiological symptoms as cues to initiate problem-solving; and use of the “stop and think” technique in problem situations.16 In PST-PC, the development of a positive orientation and enhanced self-efficacy comes about through experience and success using the problem solving model as well as encouragement from the therapist when reviewing patient progress.16 The final component of PST-PC is activity scheduling in which the therapist helps the patient plan daily pleasurable events to combat the vicious cycle of worsening mood and decreased activity.16
DIET was chosen as a control condition over usual care because it is a plausible health-related intervention in its own right, of relevance to older black and white people who are overweight or have hypertension; and to control for nonspecific effects, such as time spent with therapist and attention given to client. DIET focuses on healthy eating practices. Using a manualized educational intervention, clinicians review general nutrition guidelines, including the United States Department of Agriculture Food Pyramid, help subjects prepare weekly menus and grocery lists, cut out food coupons, and review food intake since the last visit. Topics discussed include access to healthy food, cost of food, meal preparation, and culturally specific foods. Backup from a university-based dietician is provided, as needed.
The same group of therapists who administer PST-PC also deliver DIET, to minimize therapist effects. To manage allegiance effects, group supervision and one-on-one feedback using blind evaluations of audiotapes of PST-PC and DIET sessions take place weekly.
Therapists are masters-level social workers and mental health nurses; six have been trained in PST-PC under the supervision of Patricia Arean, Ph.D. Training consisted of reviewing the PST-PC treatment manual, watching training videotapes, treating practice patients, and participating in weekly group supervisory sessions conducted by two coauthors (MM and JM).
PST-PC and DIET are delivered in 6 - 8 sessions over a 6-12 week period. The initial session lasts 1 hour with subsequent sessions lasting 30 minutes. The total time spent by therapist and participant is 5-7 hours. Thirty-minute booster sessions are also scheduled in both treatment conditions at 6, 12, and 18 months from baseline assessment (T1), after the scheduled follow-up assessments are completed. The decision to include booster sessions is based upon Rovner’s findings that PST-PC demonstrates efficacy over usual care in preventing depression at 2 months following completion of therapy; however, this effect disappears at 6 months.17 Booster PST-PC sessions may increase the likelihood of a sustained effect of the intervention.
ASSESSMENT: PRIMARY OUTCOME MEASURE
Measures are collected by research staff blind to randomized assignment who participate in regular interrater reliability checks. All measures have been successfully used with African American samples and have similar psychometric properties among black and white older persons. The primary outcome measure is incident major depressive episode, per the SCID/DSM-IV section for mood disorders.27 The SCID/DSM-IV mood disorders module is administered at screening (T1), at the end of treatment (T2), and every 3 months subsequently until the end of 24 months by a research assessor blind to randomized intervention assignment (Fig. 1). This frequency of administration allows for a reasonable degree of temporal precision in determining onset of episode. Independent confirmation of the occurrence of a major depressive episode is carried out by a geriatric psychiatrist or geropsychologist. Levels of depressive symptoms via the beck depression inventory (BDI-24; range: 0 [better]-72 [worse])28 and the Hamilton rating for depression (HRSD-17; range:0 [better]-52 [worse]),29 as well as health-related quality of life (Medical Outcomes study 36-item short form30), are assessed at the same time points. The BDI is also being administered at every treatment session as a check on symptomatic status, including suicidal ideation.
FIGURE 1.
Experimental Design of “Preventing Depression in Later Life”
Other domains assessed include cognitive performance (Mini-Mental Status Exam; range: 0 [worse]-30 [better])25; coexisting medical illnesses (Cumulative Illness Rating Scale for Geriatrics, range: 0 [better]-52 [worse]) and count of endorsed items,31 problem solving skills (Social Problem Solving Inventory, range: 55 and below [extremely below average]-145 and above [extremely above average]),32 self-efficacy (Pearlin Mastery Scale, range: 7 [low]-28 [high]),33 self-esteem (Rosenberg Self-Esteem Scale, range: 10 [low]-40 [high]),34 anxiety (brief symptom inventory, range: 0 [better]-4 [worse])35; and Barratt dietary knowledge, attitudes, and actions scale.36
RESPONDENT BURDEN AND COMPENSATION
The pretreatment (T1) assessment lasts approximately 3 hours. Each follow-up assessment (T2-T9) lasts approximately 1.5 hours. Thus, over a 2-year period, assessment time totals approximately 15 hours. Participants are paid an honorarium of $50 for each of these nine completed assessments, for a total of $450.
SAMPLE SIZE AND STATISTICAL ANALYSIS
We have based the sample size calculation on data showing a 2-year incidence of major depressive episodes of 24% in people with baseline CES-D scores of 16 and greater and with prior histories of major depression (PROSPECT study). In a trial reported by Munoz et al.,37 the subgroup of participants scoring over 16 on the CESD showed an incidence rate of major depression of 17% over 1 year. In Rovner et al.’s study of selective depression prevention, the decrease in relative incidence of depression episodes was 50% in PST-PC (11%) versus treatment as usual (23%).17 Based on these data, we aim to recruit an intent-to-treat study group of 306 participants (153 in each group) to give 80% power (α = 0.05, two-tailed) to detect a 50% difference in the rates of developing depression from an assumed rate of 24% in the control (DIET) condition. This sample size takes into account a projected 20% dropout rate over 2 years. (In this context, “intent-to-treat” means all participants who have been randomly assigned to the experimental or control condition.)
Stratification variables (such as race or history of major depression) will be included in the analysis as covariates and will be explored as potential moderators of response to PST-PC.
To compare the effects of PST-PC with DIET on incidence of major depression over 2 years, we plan to conduct a survival analysis of time to and rate of major depressive episodes in PST-PC and DIET. We will also estimate clinical effect size by calculating the number needed to treat (NNT, with 95% confidence intervals) with PST-PC to prevent one major depressive episode, as compared with DIET.
To compare depression levels (BDI and HRSD scores) and improvement in health-related quality of life (Medical Outcomes study 36-item short form) over time, we will conduct mixed effect modeling with ANCOVA using repeated measures for main effects of group, time, and time-by-treatment interaction. We will also estimate effect size for time by treatment interaction (Cohen’s d statistic).
All longitudinal data will be analyzed using an intent-to-treat approach for all randomized participants regardless of treatment exposure. This could serve to protect the analysis from biases, such as early attrition related to race. Reasons for missing data are being documented. We plan to handle missing date using mixed-model analyses and not by last observation carried forward.
To explore for possible mediators of hypothesized preventive effects, we plan to compare change in problem solving skills and self-efficacy (Pearlin Mastery Scale) in the PST-PC and DIET groups over time via mixed effect models and estimates of effect sizes. We will regress final depression outcome measures on hypothesized mediators assessed before the final measurement and treatment status variable. We will also use participant characteristics such as race, history of major depression, cognition (Folstein), and level of chronic medical burden (Cumulative Illness Rating Scale for Geriatrics) as covariates to explore moderators of preventive intervention effects.
Data quality control is carried out at weekly data review meetings chaired by the principal investigator. If data are missing, every attempt is made to retrieve them or to specify a reason for missingness. If particular values do not make sense, they are double-checked. We also employ double-entry verification on a subset of data, range checks, and automated logic checks.
FEASIBILITY OF INITIAL IMPLEMENTATION EFFORTS
As of this writing (December 2007), 22 subjects have been recruited into the study. Six are self-referred, six through PCPs, six through comprehensive geriatric clinics, and two each through either another academic medical unit or other research program referral. The mean age of participants is 69.2 years (SD: 8.9). Seventeen subjects are women, 19 are white, and 3 are black. Half of the subjects (11 of 22) have a history of past major depression. Other SCID diagnoses include current depressive disorder not otherwise specified (“minor depression;” 6 of 22), adjustment disorder with depressed mood (4 of 22), history of panic (2 of 22) or generalized anxiety disorder (3 of 22), current panic disorder (1 of 22), and two current anxiety disorders not otherwise specified (2 of 22). Other risk factors present in the sample include current depressive symptoms (17 of 22), emotional distress (20 of 22), bereavement (5 of 22), chronic insomnia (10 of 22), and living alone (9 of 22). Preintervention BDI score is 12.3 (SD: 5.2) and HRSD-17 score is 11.4 (SD: 3.7), indicating mild symptoms of depression. Social problem solving inventory score is 104.4 (SD: 13.3), consistent with normal problem-solving skills. Pearlin Mastery scale score is 20.0 (SD: 2.6) and Rosenberg Self-Esteem Scale score is 32.0 (SD: 4.5), both within normal limits. Body mass index (BMI) is 33.7 (SD: 7.2), with 13 of the 22 subjects having a BMI of 30 or greater.
To date, eight subjects have completed the intervention and postintervention assessment at T2. Three subjects so far have had at least one booster session and have undergone assessment at T3 (6 months). Four subjects have exited the study due to onset of episodes major depressive disorder. Such subjects are offered treatment in another NIH-sponsored protocol (“Geriatric Depression: Getting Better, Getting Well;” MH37869; C.F. Reynolds, Principal Investigator). No subjects have complained about study procedures or demands. Interventions have been delivered at an outpatient mental health facility, a community hospital, primary care physician offices, and over the telephone.
COMMENT
The data collected to this point support the feasibility of the study in moving from concept to design and implementation. Although still early, no unexpected problems have arisen in the retention of subjects. The study and its procedures also appear to be acceptable to participants. Occurrence of major depressive episodes (4 of 22 subjects) is expected and is the main outcome measures.
Results of SCID assessment by our clinicians are consistent with subjects’ mildly elevated BDI and HRSD scores; many have met SCID criteria for depression not otherwise specified (minor depression) or adjustment disorder with depressed mood. The high BMI scores in this sample make DIET a credible and relevant control condition for this population.
Problem solving skill, self-esteem, and mastery scores are within normal limits. Although lower scores on these measures would provide a stronger theoretical target for PST-PC to act upon, it is also possible that further enhancing problem solving-skills and self-efficacy will prove helpful in preventing depression. Furthermore, PST-PC addresses multiple risk factors. Resolutions of certain problems or development of a more positive problem solving (coping) orientation may avert depression. PST-PC also encourages subjects to be more active and engaged, also a possible mediator of the intervention’s hypothesized effectiveness.
This study is the first to our knowledge to evaluate indicated depression prevention in the elderly. If PST-PC proves effective in preventing depression, the suffering of many older adults could be averted through a brief intervention that is practicable in general medical and other social service agency settings. The recruitment of African Americans to comprise half of our sample is important within the context of unequal access to mental health services. We think that PST-PC will be effective in preventing disparities of engagement and in delaying or preventing new episodes of major depression in older black adults.
Acknowledgments
The authors thank Julie Lindenberg and Joshua Rosen for their helpful comments.
This work was supported by P30 MH071944, P60 MD000-207, T32 MH19986, the University of Pittsburgh Medical Center endowment in geriatric psychiatry, and the John A. Hartford Center of Excellence in Geriatric Psychiatry.
References
- 1.Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992;14:237–247. doi: 10.1016/0163-8343(92)90094-q. [DOI] [PubMed] [Google Scholar]
- 2.Charney DS, Reynolds CF, Lewis L, et al. Depression and bipolar support alliance consensus statement on the unmet needs in diagnosis and treatment of mood disorders in late life. Arch Gen Psychiatry. 2003;60:664–672. doi: 10.1001/archpsyc.60.7.664. [DOI] [PubMed] [Google Scholar]
- 3.Cole MG, Dendukuri N. The feasibility and effectiveness of brief interventions to prevent depression in older subjects: a systematic review. Int J Geriatr Psychiatry. 2004;19:1019–1025. doi: 10.1002/gps.1200. [DOI] [PubMed] [Google Scholar]
- 4.Lyness JM, Moonseong H, Datto CJ, et al. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Ann Intern Med. 2006;144:496–504. doi: 10.7326/0003-4819-144-7-200604040-00008. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 6.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 7.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 8.Andrews G, Issakidis C, Sanderson K, et al. Utilising survey data to inform public policy: comparison of the cost-effectiveness of treatment of ten mental disorders. Br J Psychiatry. 2004;184:526–533. doi: 10.1192/bjp.184.6.526. [DOI] [PubMed] [Google Scholar]
- 9.Mrazek P, Haggerty R. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. National Academy Press; Washington, D.C.: 1994. [PubMed] [Google Scholar]
- 10.Schoevers RA, Smit F, Deeg DJH, et al. Prevention of late-life depression in primary care: do we know where to begin? Am J Psychiatry. 2006;163:1611–1621. doi: 10.1176/ajp.2006.163.9.1611. [DOI] [PubMed] [Google Scholar]
- 11.Smit F, Ederveen A, Cuijpers P, et al. Opportunities for cost-effective prevention of late-life depression: an epidemiological approach. Arch Gen Psychiatry. 2006;63:290–296. doi: 10.1001/archpsyc.63.3.290. [DOI] [PubMed] [Google Scholar]
- 12.Unutzer J, Katon W, Callahan CM, et al. Depression treatment in a sample of 1,801 depressed older adults in primary care. J Am Geriatr Soc. 2003;51:505–514. doi: 10.1046/j.1532-5415.2003.51159.x. [DOI] [PubMed] [Google Scholar]
- 13.Cooper-Patrick L, Gallo JJ, Powe NR, et al. Mental health service utilization by African Americans and Whites: the Baltimore epidemiologic catchment area follow-up. Med Care. 1999;37:1034–1045. doi: 10.1097/00005650-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Reynolds CF, Dew MA, Lenze EJ, et al. Preventing depression in medical illness: a new lead? Arch Gen Psychiatry. 2007;64:884–885. doi: 10.1001/archpsyc.64.8.884. Editorial commentary. [DOI] [PubMed] [Google Scholar]
- 15.Arean PA, Ayalon L. Assessment and treatment of depressed older adults in primary care. Clin Psychol Sci Pract. 2005;12:321–335. [Google Scholar]
- 16.Hegel MT, Arean PA. Problem-Solving Treatment for Primary Care (PST-PC): A Treatment Manual for Depression Project IMPACT. Dartmouth Medical School; Hanover, NH: 2003. [Google Scholar]
- 17.Rovner BW, Casten RJ, Hegel MT, et al. Preventing depression in age-related macular degeneration. Arch Gen Psychiatry. 2007;64:886–892. doi: 10.1001/archpsyc.64.8.886. [DOI] [PubMed] [Google Scholar]
- 18.Williams DR. Minority Health In America: Findings and Policy Implications From Commonwealth Fund Minority Health Survey. Johns Hopkins University Press; Baltimore: 2000. Race, Stress, and Mental Health. [Google Scholar]
- 19.Steffens DC, Artigues DL, Ornstein KA, et al. A review of racial differences in geriatric depression: implications for care and clinical research. J Natl Med Assoc. 1997;89:731–736. [PMC free article] [PubMed] [Google Scholar]
- 20.Hu TW, Snowden LR, Jerrell JM, et al. Ethnic populations in public mental health: services choice and level of use. Am J Public Health. 1991;81:1429–1434. doi: 10.2105/ajph.81.11.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neighbors HW, Jackson JS, Campbell L, et al. The influence of racial factors on psychiatric diagnosis: a review and suggestions for research. Community Ment Health J. 1989;25:301–311. doi: 10.1007/BF00755677. [DOI] [PubMed] [Google Scholar]
- 22.Arean PA, Alvidrez J, Nery R, et al. Recruitment and retention of older minorities in mental health services research. Gerontologist. 2003;43:36–44. doi: 10.1093/geront/43.1.36. [DOI] [PubMed] [Google Scholar]
- 23.Brown C, Schulberg HD, Sacco D, et al. Effectiveness of treatments for major depression in primary medical care practice: a post hoc analysis of outcomes for African American and white patients. J Affect Disord. 1999;53:185–192. doi: 10.1016/s0165-0327(98)00120-7. [DOI] [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 25.Folstein MF, Folstein SW, McHugh PR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 26.Nezu AM, Nezu CM. Problem solving therapy. J Psychother Integrat. 2001;11:187–205. [Google Scholar]
- 27.First M, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), Version 2.0. State Psychiatric Institute; New York: 1994. [Google Scholar]
- 28.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ware J, SF-36 Health Survey . Manual and Interpretation Guide 2. The Health Institute, New England Medical Center, Nimrod Press; Boston: 1997. [Google Scholar]
- 31.Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the cumulative illness rating scale. Psychiatry Res. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- 32.D’Zurilla TJ, Nezu AM. Development and preliminary evaluation of the social problem-solving inventory. Psychol Assess. 1990;2:156–163. [Google Scholar]
- 33.Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- 34.Rosenberg M. Society and the Adolescent Self-Image. Wesleyan University Press; Middletown, CN: 1989. [Google Scholar]
- 35.Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med. 1983;13:595–605. [PubMed] [Google Scholar]
- 36.Barratt J. Diet-related knowledge, beliefs and actions of health professionals compared with the general population: an investigation in a community trust. J Hum Nutr Diet. 2001;14:25–32. doi: 10.1046/j.1365-277x.2001.00267.x. [DOI] [PubMed] [Google Scholar]
- 37.Munoz RF, Ying YW, Bernal G, et al. Prevention of depression with primary care patients: a randomized controlled trial. Am J Community Psychol. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]