Abstract
This study examined whether negative parental attributions for adolescent behaviour mediate the association between parental and adolescent depressive symptoms, and whether this relationship is moderated by adolescent gender. Mothers and fathers and 124 adolescents (76 girls and 48 boys; ages 14 to 18) participated. Adolescents were primarily Caucasian, and varied in the level of depressive symptoms (with 27% of the sample meeting diagnostic criteria for a current unipolar depressive disorder). Parents and adolescents completed measures of depressive symptoms, and participated in a videotaped problem-solving discussion. After the discussion, each parent watched the videotape and, at 20s intervals, offered attributions for their adolescent's behaviour. Adolescent gender moderated the relation between parental attributions and adolescent depressive symptoms, with stronger associations for female adolescents. For both mothers and fathers, both parental depressive symptoms and negative attributions about the adolescent's behaviour made unique contributions to the prediction of depressive symptoms in adolescent females. There also was evidence that negative attributions partially mediated the link between depressive symptoms in mothers and adolescent daughters. The results are interpreted as consistent with parenting as a partial mediator between parental and adolescent depressive symptoms, and suggest that adolescent girls may be particularly sensitive to parents' negative interpretations of their behaviour.
Keywords: depression, attributions, parent-adolescent relations
A recent review of epidemiological studies reported that the prevalence rates of depression in girls and boys between 13 and 18 years of age are 5.9% and 4.6% respectively (Costello, Erkanli, & Angold, 2006). Not only is adolescent depression relatively common, it also is associated concurrently with high rates of comorbid psychiatric disorders (Kovacs, 1996), significant psychosocial impairment (Birmaher, Ryan, Williamson, & Brent, 1996), and increased risk of suicide (Rao, Weissman, Martin, & Hammond, 1993). Adolescent depression is, moreover, predictive of a wide range of long-term psychosocial impairments including recurrent depressive disorders in early adulthood (Aalto-Setälä, Marttunen, Tuulio-Henriksson, Poikolainen, & Lönnqvist, 2002; Lewinsohn, Rohde, Klein, & Seeley, 1999). The prevalence rates of adolescent depressive disorders likely underestimate the extent of the problem posed by depressive conditions because significant numbers of adolescents experience subdiagnostic depressive symptomatology (Roberts, Andrews, Lewinsohn, & Hops, 1990) and available evidence suggests that these youth present with many of the same social, clinical, and behavioral problems as do those who meet diagnostic criteria (Gotlib, Lewinsohn, & Seeley, 1995; Pine, Cohen, Cohen, & Brook, 1999). These adolescents with subdiagnostic depressive symptomatology also are at substantially increased risk of developing depressive disorders (Gotlib et al., 1995; Pine et al., 1999). The prevalence and impairment associated with adolescent depressive symptoms clearly highlight the importance of research addressing mechanisms that place youth at risk.
One factor that has been consistently linked to depression in youth, and may play a causal role, is the level of depressive symptoms in parents. In an early review, children of depressed parents were found to be six times more likely to be diagnosed with major depressive disorder than children of non-depressed parents (Downey & Coyne, 1990). Similar findings have been obtained in community samples of adolescents. For example, using a longitudinal design, Beardslee, Keller, Seifer, Lavori, Staley, and Podorefsky (1996) found the duration of parental major depressive disorder, along with the parents' total number of nonaffective disorders and the adolescents' total number of prior diagnoses, to be the strongest predictors of the onset of affective disorders in the adolescents. When compared to depressed adolescents of non-depressed parents, depressed adolescents with depressed parents also have been shown to have higher suicidal ideation, and more recurrent depressive episodes (Essau, 2004). This association between the depressive symptoms of parents and their offspring also has been observed in nonclinical samples (Hops, 1992; Ge, Conger, Lorenz, & Simons, 1994; Ge, Conger, Lorenz, Shanahan, & Elder, 1995).
Evidence suggests that the intergenerational transmission of depressive syndromes is attributable, in part, to disruptions in interactions between parents and youth associated with depressive symptomatology (Gotlib & Goodman, 1999; Radke-Yarrow & Klimes-Dougan, 2002). This is not to minimize the genetic and contextual risks (Goodman & Gotlib, 1999) that are shared by parent and child, or to ignore evidence that children with behavioral or emotional difficulties place a burden on parents that may contribute to their distress (Gartstein & Sheeber, 2004; Patterson, Chamberlain, & Reid, 1982). Nonetheless, relative to nondepressed parents, depressed parents have been shown to exhibit a pattern of parent-child interaction that is less positive, less engaged, harsher, and more critical (Lovejoy, Graczyk, O'Hare, & Neuman, 2000; Radke-Yarrow & Klimes-Dougan, 2002). These findings are largely consistent across age of child, measurement approach, and operationalizations of depression (Hammen, Burge, & Stansbury, 1990; Gotlib & Goodman, 1999; Lovejoy et al., 2000). Of particular relevance to this paper is evidence that depressed parents are rejecting and critical, and low in warmth when interacting with their depressed adolescents (Burge & Hammen, 1991; Hammen, Shih, & Brennan, 2004; Muris, Schmidt, Lambrichs, & Meesters, 2001). Notably, a meta-analysis (Lovejoy et al., 2000) indicated that the relationship between depressive symptoms and parenting style is not moderated by diagnostic status. This suggests that adverse parenting approaches are associated with parental distress, whether or not that distress reflects clinical levels of pathology.
In this paper, we focus on aspects of the parent-child relationship as mediators between parental and adolescent depressive symptoms. Several studies have indicated that the link between parenting variables and youth depression may be stronger in girls than in boys (Sheeber, Davis, & Hops, 2002). For example, using a sample of 134 high-school students, Gamble and Roberts (2005) found that adolescent gender interacted with adolescents' self-report of critical parenting experience to predict dysfunctional attitudes and negative attributional styles in the youth, with stronger relations among girls than boys. Similarly, Hale, Van Der Valk, Engels, and Meeus (2005), using a large community sample of 1329 adolescents, found that the links between perceived parental rejection and adolescent depressive symptoms were stronger for females than for males. In sum, from these studies, negative parenting attitudes emerge as one possible pathway through which parental and adolescent depressive symptoms may be linked, particularly for female adolescents. Unfortunately, given that these studies only assessed parenting from the adolescents' perspective, it is unclear whether the observed relations, including the greater association observed between parenting variables and outcome for girls, could be due to source effects, with girls reporting more adverse parenting as well as more depressive symptoms and cognitions. Studies that include independent reports of parenting are thus needed to further clarify these findings.
One aspect of parenting that has remained largely unexplored in understanding the transmission of depressive symptoms from parents to adolescents is the role of parental attributions for adolescents' behavior. Attributions are the causal explanations that parents generate for their adolescents' behaviour, and include the parents' views of aspects of the adolescent's behaviour such as the locus of control, the stability, and the controllability of behavior (Weiner, 1986). In much of the research on parental attributions, causal reasoning along these various attributional dimensions has been broadly categorized as negative or child-blaming versus positive or child-crediting (e.g., MacBrayer, Milich, & Hundley, 2003; Snyder, Cramer, Afrank & Patterson, 2005). Overall, when parents make attributions regarding their children's behaviour that are more negative (e.g., seeing misbehaviour as caused by factors internal to the child, controllable, and stable over time), they are more likely to respond with coercive parenting (Dix, Ruble, Grusec, & Nixon, 1986; Smith Slep & O'Leary, 1998), and negative affect (Hakim-Larson, Dunham, Vellet, Murdaca, & Levenbach, 1999; Smith & O'Leary, 1995), and these parenting responses are associated with poorer outcomes in the offspring (Joiner & Wagner, 1996; Miller, 1995; Mills & Rubin, 1990).
Numerous studies show associations between negative parental attributions and externalizing behavior problems in young children, both in cross sectional and longitudinal designs (e.g., Johnston, Chen, & Ohan, 2006; Hastings & Rubin, 1999; Nix et al., 1999). However, little research has explored how parental attributions may be associated with internalizing disorders or the role of parental attributions in adolescence. In this study, we focus on parents' attributions for the behaviors of adolescents, and how these attributions may be related to depressive symptoms experienced by both parents and their adolescent children. From previous studies using both community and clinic-referred samples of young children, we know that depression in parents is associated with more negative attributions for child misbehaviour (Bolton et al., 2003; Leung & Smith Slep, 2006). Specifically, Bolton et al. (2003) conducted interviews with 61 mothers of children between 4 and 11 years of age, and coded the causal explanations that mothers made for their children's problem behaviors. These authors found that mothers with higher depression scores were more likely to perceive the cause of their children's negative behaviors as internal to and controllable by their children. Similar results were obtained by Leung and Smith Slep (2006) in both mothers and fathers.
Although most previous studies have focused on child externalizing problems, a recent study of 48 mothers of 12-14 year old adolescents (Heatherington, Tolejko, McDonald & Funk, 2007) revealed that mothers' negative attributions for adolescents' behaviour were related to increased mother-adolescent conflict. In particular, mothers who perceived their adolescents' negative behaviors as resulting from more global and pervasive causes also reported having more conflicts with their adolescents. This finding, combined with results showing significant associations between negative parental attributions and negative parenting in families of children with externalizing problems, makes it reasonable to hypothesize that adolescent-blaming attributions, associated with maternal depressive symptoms, are related to depressive symptoms in the adolescent offspring. As a first step, therefore, we postulate that negative parental attributions are related to both parent and adolescent depressive symptoms, and, as one aspect of disrupted parent-youth interactions, provide one mechanism underlying the intergenerational transmission of depression.
The first goal of this study, therefore, is to examine whether negative parental attributions for adolescent behaviour are related to adolescent and parental depressive symptoms. Given the highly familial nature of depressive symptoms, we sought to determine whether negative parental attributions would be related to adolescent depressive symptoms after controlling for parental depressive symptoms, and further, whether negative parental attributions mediate the relationship between parental and adolescent depressive symptoms. Although most research in this area has focused exclusively on mothers, a previous study conducted on the larger sample from which the sample for the current study was drawn, has shown that depressed adolescents and those with subdiagnostic levels of depression experienced less supportive and more conflictual relationships with both their mothers and fathers compared to nondepressed adolescents (Sheeber, Davis, Leve, Hops, & Tildesley, 2007). Furthermore, the variance accounted for by mother and father behavior in predicting adolescent depression was unique, highlighting the need to consider the role of fathers in understanding adolescent depression. Therefore, in this report we include attributions made by both mothers and fathers to explore the potential effect of parent gender on the relations between parental and adolescent depressive symptoms.
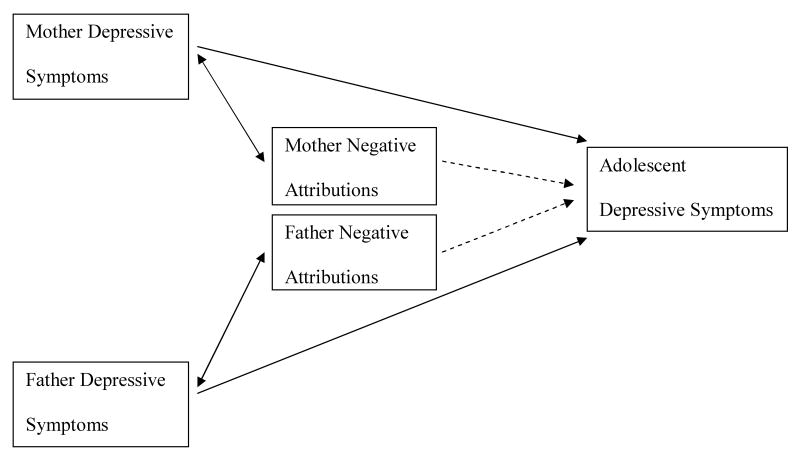
Consistent with evidence reviewed earlier that the links between parenting and adolescent depression may be particularly strong for girls, the second goal of this study was to examine whether adolescent gender moderates the links between parental attributions and adolescent depressive symptoms. The gender difference in the prevalence of adult depression is well established, and this difference appears to emerge between early and middle adolescence (Hankin & Abramson, 2001). One theory that has been proposed to account for this phenomenon suggests that girls begin to value interpersonal intimacy more than boys during adolescence as each gender becomes increasingly socialized into gender-specific roles, and as a result, adolescent girls are more vulnerable to the negative effects of stressful interpersonal events (Cyranowski, Frank, Young, & Shear, 2000). Given that parental attributions reflect aspects of the interpersonal relationships between parents and adolescents, it is likely that adolescent girls are both more attuned to the negative attributions of their parents, and more sensitive to the negative parent-youth interactions that may result from them. In sum, we hypothesized that because adolescent girls are more sensitive to interpersonal stress than adolescent boys, parental attributions that are hostile or negative toward adolescents will be more strongly associated with depressive symptoms in adolescent girls than boys. A visual representation of our hypotheses is provided in Figure 1.
Figure 1.
Hypothesized relationships between parental depressive symptoms, parental negative attributions, and adolescent depressive symptoms. Dashed lines indicate that the relationships are predicted to be moderated by adolescent gender.
Method
Participants
Description and inclusion criteria
Participants were 124 adolescents (76 girls and 48 boys) and their parents, selected from a larger sample of families participating in a study of family process associated with adolescent depression (N=243; Sheeber et al., 2007). To be included in the larger investigation, adolescents had to be between 14 and 18 years old, live with at least one parent or permanent guardian, and meet research criteria for placement in one of three groups: depressed, subdiagnostic, or healthy. In order to provide a clear description of the sample selection and recruitment process, operational definitions of these designations are included in this report. However, it should be noted that diagnostic group is not a variable in this study, in which, as described below, depressive symptoms were treated as a continuous variable.
The depressed group included adolescents who both scored above an adolescent appropriate cut-off score on the CES-D (≥ 26 for males and ≥ 30 for females) during an initial school-based screening and met the DSM-IV (American Psychiatric Association, 1994) diagnostic criteria for a current unipolar depressive disorder in a subsequent assessment. The subdiagnostic group included adolescents who scored above the cut-off on the CES-D scale at screening, but who did not meet diagnostic criteria for current or lifetime affective disorders, or current nonaffective disorders. The healthy group included adolescents who scored below the cut-off scores on the CES-D scale at screening, did not meet criteria for current or lifetime diagnoses, and had no history of mental health treatment.
Due to resource limitations, attributional coding was only completed on a subset of the larger sample. Because we were interested in examining the relations between attributions and depressive symptoms in both mothers and fathers, only two-parent families in which both parents participated were included. This approach enabled us to ensure that mothers and fathers were making attributions about the same child's behavior. Additionally, of families meeting these inclusion criteria, 21 were excluded because audiotaped attribution data were unavailable due to problems in taping. Twenty-seven percent of the adolescents included in our subsample were from the original depressed group, 36% were from the subdiagnostic group, and 37% were from the healthy group.
Recruitment procedures
For the larger study from which our subsample was drawn, families were recruited and selected using a two-gate procedure consisting of an in-school screening and an in-home diagnostic interview. Students from area high schools participated in the school screening which was conducted during class time. To facilitate recruitment of a representative sample of students, we used a combined passive parental consent and active student consent procedure to inform families about the project and request their participation in the school screening (Biglan & Ary, 1990; Severson & Ary, 1983). Approximately 75% of eligible students (N = 4495) participated. Participating students completed the screening CES-D, a demographic information form, and a contact form.
Research staff telephoned families of those adolescents selected based on CES-D scores obtained from the school screening and invited them to participate in an informational meeting in the families' homes. At these meetings, staff described the project and obtained active informed consent from the adolescents and their parents. Following the consent procedure, interviewers (bachelor to doctoral level research staff) conducted the diagnostic interviews with the adolescents (Schedule of Affective Disorders and Schizophrenia-Children's Versions [K-SADS]; Orvaschel & Puig-Antich, 1994). Of families invited to participate in the diagnostic interview, approximately 80% (N=537) consented. Of those subsequently eligible to participate in the full family assessment, approximately 94% (246) agreed to do so. Rates of decline did not vary as a function of CES-D score, group status, age, race, or gender. Greater detail on recruitment procedures is available in Sheeber et al. (2007).
Measures
Parent and Adolescent Depressive Symptoms
The CES-D is a widely-used, self-report measure that has respectable psychometric properties for use in both adolescent and adult populations (Radloff, 1991; Radloff & Teri, 1986; Roberts, Andrews, Lewinsohn, & Hops, 1990). It has been shown to discriminate between psychiatric inpatient and healthy control groups, and to correlate moderately with clinician ratings of severity of depression (Radloff, 1977). It also has been demonstrated to have adequate sensitivity and specificity for detecting current episodes of depression and dysthymia in an adolescent sample (Roberts, Lewinsohn, & Seeley, 1999).
The CES-D was administered on two occasions. As noted above, adolescents first completed the CES-D during the school screening which served as the first-gate of the selection procedure. Adolescents and their parents subsequently completed the CES-D during the lab-based family assessment in order to provide a continuous measure of depressive symptoms. Data from this second assessment was used as the outcome variable in this report. The CES-D scores were continuously distributed and demonstrated adequate internal consistency for mothers (α = .93), fathers (α = .92), and adolescents (α = .94).
Video-Mediated Recall Procedure
Each family engaged in two 10-minute family problem-solving interactions (PSIs) in which they discussed and tried to resolve two identified areas of conflict (e.g., fighting with siblings; helping out around the house). The topic of greater conflict (as indicated by parent and adolescent report of frequency and intensity) was discussed second. Immediately subsequent to the PSIs, mothers and fathers participated separately in a video-mediated recall procedure (VMR). For this procedure, each parent simultaneously watched and responded to a videotaped replay of the second problem-solving interaction in private. We conducted the VMR immediately subsequent to the second interaction so that participants would have the clearest possible recall of the interaction. The video replay was paused automatically every 20s and parents responded to two questions regarding their adolescent's behavior during the observed section of the interaction: 1) What is your child doing? and 2) Why was he/she doing that? Parents' responses were audiotaped and coded for parental attributions. The video-mediated recall procedure has been employed in previous research to assess parental cognitions (e.g., Dadds, Mullins, McAllister, & Atkinson, 2003; Johnston & Freeman, 1997; Sanders, Dadds, Johnston, & Cash, 1992), and has consistently shown sensitivity to group differences in parental attributions. Although the method is somewhat less standardized than the traditional approach of eliciting parental attributions from vignettes depicting child behaviors, it has the advantage of being more ecologically valid as it is based on actual behaviour displayed by the parents' own child.
Attribution Coding System
Mothers' and fathers' responses to the questions “what is your child doing” and “why is he/she doing that” were transcribed verbatim. As parents often included attributions in their response to the question of “what is your child doing” (e.g., she was just not trying), the decision was made to code all instances of causal attributions in the responses to both questions. Causal attributions were defined as explanations that parents generated for their adolescents' behavior. In addition to reading the transcribed responses, coders listened to the audiotape of the parents' response during coding in order that tone of voice and affect could be considered in coding the attributions.
The coding system used in this study was based on the systems previously used by MacBrayer et al. (2003) and Snyder et al. (2005). In this study, positive attributions were defined as attributions that gave the adolescent credit for positive behaviors, or excused or removed blame from the adolescent for negative behaviors. These included: 1) attributions that minimized a negative adolescent behavior (e.g., she just got confused); 2) attributions that implied positive intentions or characteristics in the adolescent (e.g., he's trying to understand our point of view); and 3) attributions that invoked external circumstances, the parent's own behaviors, or the adolescent's lack of knowledge to explain negative adolescent behaviors (e.g., she is still young; he stopped listening because I wasn't clear). Negative attributions were defined as attributions that blamed the adolescent for negative behaviors or did not give the adolescent credit for positive behaviors. These included 1) attributions that implicated negative personality traits (e.g., she is lazy); 2) attributions that suggested the adolescent acted with hostility, indifference, defiance, or a significant lack of concern (e.g., she's not willing to pay attention; he knows he can make his brother mad by saying that); and 3) attributions that invoked external circumstances or the parent's own behaviors to explain positive adolescent behaviors (e.g., he's only listening because that's what he's been told to do). Attributions that could not be unambiguously classified as either positive or negative were coded as neutral. For each interval, coders indicated the presence or absence of each type of attribution (positive, neutral, and negative), or coded the interval as “no attribution” if the parent did not offer any causal attributions in their response.
The team of coders consisted of the first and second authors, and three senior undergraduate students in psychology. Coders were trained in the use of the manual until they agreed on 80% of the intervals in practice transcripts. Once coding commenced, weekly meetings were held to review the coding manual and to discuss disagreements between coders. All coders were blind to the level of depressive symptoms in adolescents and parents. Forty-four percent of the transcripts were coded independently by two coders to evaluate reliability. To calculate the intraclass correlations, the attributions in each category were summed across intervals to yield four total scores. Intraclass correlation coefficients were computed between coders and were .90, .93, .96, and .99 for the positive, neutral, negative, and no attribution categories respectively. To control for differences in the absolute number of attributions that parents provided, percentage scores were computed by dividing the category total (e.g., total of positive attributions summed across intervals) by the grand total of attributions (i.e., total of all attributions summed across intervals). These percentage scores were used in all subsequent analyses. In this sample, the mean percentages of positive, negative, and neutral attributions made by mothers and fathers were .18, .16, .66, and .19, .16, and .65 respectively. Given that our hypotheses concerned only the relationship between parental levels of depressive symptoms, parents' negative attributions, and adolescent outcome, only the percentage of parents' negative attributions was included in the analyses.
Results
Preliminary Analyses
The means and standard deviations for demographic variables, adolescent depression scores, and mothers' and fathers' attributions are presented in Table 1. The adolescent CES-D score was missing for one subject. Inspection of distributions revealed that the CES-D scores for the current sample of mothers, fathers, and adolescents were all continuous. The adolescents' CES-D scores had a skewness statistic less than 1.0. There was, however, a positive skew for mothers' and fathers' negative attributions, as well as mothers' and fathers' depression scores, with the skewness statistic exceeding 1.0. Squareroot transformations were therefore applied to these four variables. The transformations successfully decreased the skewness statistic for mothers' negative attributions (from 1.10 to -.16), fathers' negative attributions (from 1.19 to 0.03), mothers' depression scores (from 1.82 to 0.27), and fathers' depression scores (from 1.74 to 0.34). These transformed scores were used in subsequent analyses.
Table 1.
Means (SD) of Demographic Variables, Depression Scores, and Parental Attributions, and Test Statistics for Gender Differences in these Variables.
| Boys (n = 48) | Girls (n = 76) | Test Statistic | Sig. | |
|---|---|---|---|---|
| Demographics | ||||
| Adolescent age | 16.52 (1.11) | 16.13 (1.15) | t =1.85 (122) | .07 |
| Adolescent Ethnicity | X2 = 2.51 (5) | .78 | ||
| European-American | 91.7% | 84.2% | ||
| African-American | 0% | 1.3% | ||
| Latin-American | 2.1% | 3.9% | ||
| Asian-American | 2.1% | 6.6% | ||
| Native-American | 2.1% | 2.6% | ||
| Other | 2.1% | 1.3% | ||
| Mother Education | X2 = 5.12 (3) | .16 | ||
| High School Graduate | 22.7% | 35.8% | ||
| Some College | 38.6% | 25.4% | ||
| College Graduate | 20.5% | 11.9% | ||
| Graduate School | 18.2% | 26.9% | ||
| Father Education | X2 = 2.08 (3) | .56 | ||
| High School Graduate | 17.1% | 27.9% | ||
| Some College | 31.7% | 26.5% | ||
| College Graduate | 22% | 23.5% | ||
| Graduate School | 29.3% | 22.1% | ||
| Depression Scores (CES-D) | ||||
| Adolescent | 13.13 (10.77) | 16.79 (13.30) | -1.68 (114.36) | .10 |
| Mother | 7.85 (8.07) | 10.21 (10.14) | -1.36 (122) | .18 |
| Father | 7.65 (8.34) | 8.74 (8.47) | -.70 (122) | .48 |
| Mother's Attributions | ||||
| % Negative | 15.65 (14.44) | 16.56 (14.19) | -.35 (122) | .73 |
| Father's Attributions | ||||
| % Negative | 15.88 (13.67) | 16.09 (15.88) | -.08 (122) | .94 |
Preliminary analyses were conducted to investigate possible gender differences in demographics, adolescent depression scores, and mothers' and fathers' attributions. Boys and girls did not differ in their mean ages, parental level of education, or depression scores (all ps > .05). Similarly, there were no significant differences in the proportions of negative attributions that parents made for boys' vs. girls' behaviour (mothers t (122) = -.49, ns; fathers, t (122) = .39, ns.) Mothers and fathers also did not differ significantly in their levels of depressive symptoms, t (123) = .84, ns. In addition, adolescent age was not significantly correlated with adolescent level of depressive symptoms, r (123) = -.11, p = .21.
Correlations between Parental Attributions and Adolescent Depressive Symptoms: Adolescent Gender as Moderator
Multiple regressions were computed to examine our hypothesis that the relationship between negative parental attributions and adolescent depressive symptoms would be moderated by adolescent gender. Regressions for mothers and fathers were computed separately. In these regressions, parental negative attributions were first centered to reduce multicollinearity with the interaction term. At Step 1 of the regressions, the centered parents' negative attributions and adolescent gender were entered as predictors of adolescent depressive symptoms. The interaction term was entered at Step 2. At each step, we tested whether the model was significant and, at Step 2, whether the incremental change in R2 was significant. Results of the two regression models are presented in Tables 3 and 4. For both mothers and fathers, there was a significant main effect of parental negative attributions and a significant interaction between parental negative attributions and adolescent gender. Specifically, for mothers, the full model was significant, R2 = .13, F (3, 119) = 5.70, p < .01. At Step 1, mothers' negative attributions accounted for significant variance in adolescent depressive symptoms, R2 = .09, F (2, 120) = 5.87, p < .01. At Step 2, the interaction term between mothers' negative attributions and adolescent gender accounted for significant incremental variance, R2 Change = .04, F Change (1, 119) = 4.96, p < .05. For fathers, the full model was significant, R2 = .17, F (3, 119) = 7.96, p < .001. At Step 1, fathers' negative attributions accounted for significant variance in adolescent depressive symptoms, R2 = .11, F (2, 120) = 7.58, p < .01. At Step 2, the interaction term between fathers' negative attributions and adolescent gender accounted for significant incremental variance, R2 Change = .06, F Change (1, 119) = 7.85, p < .01. Similar results were obtained from simple slopes analyses, with the slopes for mothers' and fathers' negative attributions being significant for depressive symptoms in adolescent girls (t = 3.77, β = .42 and t = 4.57, β = .47 respectively, p < .001) but not boys (t = .24, β = .03 and t = -.25, β = -.04 respectively, ns). These results confirmed our predictions and indicated that the relation between parental negative attributions and adolescent depressive symptoms was indeed stronger for female adolescents. We therefore conducted all subsequent analyses for boys and girls separately.
Table 3.
Bivariate Correlations between Parental Depression, Adolescent Boys' Depression, and Parents' Negative Attributions
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Mother Depression | --- | .43** | .33* | .04 | .09 |
| 2. Fathers Depression | --- | .25 | .21 | .22 | |
| 3. Adolescent Depression | --- | .04 | -.04 | ||
| 4. Mothers' Negative Attributions | --- | .52** | |||
| 5. Fathers' Negative Attributions | --- |
Note. n = 48;
p < .01;
p < .05
Table 4.
Bivariate Correlations between Parental Depression, Adolescent Girls' Depression, and Parents' Negative Attributions
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Mother Depression | --- | .31** | .46** | .38** | .21 |
| 2. Fathers Depression | --- | .27* | .13 | .05 | |
| 3. Adolescent Depression | --- | .39** | .46** | ||
| 4. Mothers' Negative Attributions | --- | .51** | |||
| 5. Fathers' Negative Attributions | --- |
Note. n = 76;
p < .01;
p < .05
Correlations among Parental Depressive Symptoms, Parental Negative Attributions and Adolescent Depressive Symptoms
Table 3 shows the bivariate correlations between parental depressive symptoms, adolescent depressive symptoms, and parental negative attributions. For girls, at the bivariate level, mothers' depression scores correlated significantly with adolescent depression scores as well as with mothers' negative attributions. Fathers' depression scores correlated significantly with adolescent girls' depression scores, but not with fathers' negative attributions. For boys, the only significant correlation was between mothers' and adolescents' depression scores.
Predicting Adolescent Depressive Symptoms based on Parental Depressive Symptoms and Negative Attributions
Given the lack of significant correlations between parental attributions and adolescent boys' depressive symptoms, subsequent analyses were performed on data from families of adolescent girls only. Hierarchical regressions were used to examine whether parents' depressive symptoms and negative attributions each contributed independently to the prediction of adolescent girls' depressive symptoms. Hierarchical regressions were performed separately for mothers and fathers, with adolescent girls' depressive symptoms as the outcome variable. At Step 1 of the regressions, parent's level of depressive symptoms was entered. At Step 2, parental negative attribution was entered. At each step, we tested whether the model was significant and, at Step 2, whether the incremental change in R2 was significant. The beta weights for each variable at Step 2 reflect the independent contribution of that variable, controlling for the other. The statistics for the two models are presented in Table 5. For mothers, the full model was significant, R2 = .27, F (2, 74) = 13.23, p < .001. At Step 1, mothers' depressive symptoms accounted for significant variance in adolescent girls' depressive symptoms. At Step 2, mothers' negative attributions accounted for significant incremental variance, R2 Change = .06, F Change (1, 72) = 5.42, p < .05. Hence, both mothers' depressive symptoms and mothers' negative attributions contributed uniquely to the prediction of adolescent girls' depressive symptoms. For fathers, the full model was significant, R2 = .27, F (2, 74) = 12.95, p < .001. At Step 1, fathers' depressive symptoms accounted for significant variance in adolescent girls' depressive symptoms. At Step 2, fathers' negative attributions accounted for significant incremental variance, R2 Change = .19, F Change (1, 72) = 18.72, p < .001. Hence, both fathers' depressive symptoms and fathers' negative attributions contributed uniquely to the prediction of adolescent girls' depressive symptoms.
Table 5.
Regression Analyses Predicting Adolescent Girls' Depression
| Predictors | B | SE B | Beta | Partial r | t | p | |
|---|---|---|---|---|---|---|---|
| Mothers | |||||||
| Step 1 | Depression | 3.84 | .86 | .46 | .46 | 4.45 | .00 |
| Step 2 | Depression | 3.07 | .90 | .37 | .34 | 3.41 | .00 |
| Negative Attribution | 16.83 | 7.23 | .25 | .24 | 2.33 | .02 | |
| Fathers | |||||||
| Step 1 | Depression | 2.44 | 1.02 | .27 | .27 | 2.41 | .02 |
| Step 2 | Depression | 2.09 | .91 | .23 | .26 | 2.29 | .03 |
| Negative Attribution | 27.22 | 6.29 | .44 | .45 | 4.33 | .00 | |
Is the Association Between Parental and Adolescent Depressive Symptoms Mediated by Parental Negative Attributions?
Finally, the bootstrap procedure (Shrout & Bolger, 2002) was used to test whether mothers' attributions mediated the association between maternal and adolescent girls' depressive symptoms. The bootstrap method uses a resampling approach to generate an empirical distribution for further significance testing. Thus, the bootstrap makes fewer assumptions regarding the distribution of the indirect or mediated effect and has been shown to produce more accurate confidence intervals (MacKinnon, 2007; MacKinnon, Lockwood, & Williams, 2004; Shrout & Bolger, 2002).
With 1000 bootstrap resamples, the 95th percentile bias-corrected confidence interval for the mediational effect ranged between .007 and .107. Given that this confidence interval did not include zero, the mediation effect was interpreted as statistically significant at the p < .05 level (Shrout & Bolger, 2002). Of note, the direct effect of maternal depressive symptoms on adolescent depressive symptoms while reduced, remained strong (β = .25, t = 4.62, p < .01), indicating partial mediation of this effect. Similar results were obtained from repeated bootstrap analyses using 2000, 3000, and 4000 resamples. Mediation analysis was not conducted for fathers given the lack of significant correlation between paternal depressive symptoms and paternal negative attributions.
Discussion
Extending the literature on family processes and adolescent depressive symptoms, this study takes a first step in examining the relationship between parents' negative attributions for youth behaviour and adolescents' internalizing problems. Specifically, we investigated whether parents' negative attributions were related to adolescent depressive symptoms, whether this relationship was moderated by adolescent gender, and whether attributions mediated the link between parental and adolescent depressive symptoms. Our results indicated that, although parents' negative attributions were related to adolescents' symptoms of depression as predicted, this association was only significant for girls. This study also revealed differences in the pattern of results for mothers and fathers of adolescent girls. Specifically, whereas mothers' negative attributions partially mediated the relationship between mothers' and adolescent girls' depressive symptoms, fathers' negative attributions, although related to adolescent girls' depressive symptoms, were not significantly associated with fathers' level of depressive symptoms.
Turning first to the effects of adolescent gender, our results are consistent with previous findings showing that adolescent girls may be more vulnerable to the effects of interpersonal stress relative to adolescent boys. Previous studies have found not only that girls experience more interpersonal stress than boys during adolescence, but also that they become more emotionally distressed than boys in the face of interpersonal disharmony (Goodyer & Altham, 1991; Rudolph, 2002; Shih, Eberhart, Hammen, & Brennan, 2006). Indeed, having a more positive self-perception in the domain of interpersonal relationships has been shown to serve as a protective factor against depression for adolescent girls (Eberhart, Shih, Hammen, & Brennan, 2006). Given that parents of boys and girls did not differ significantly in the percentage of observer-rated negative attributions for adolescent behaviour that they generated, the fact that parents' negative attributions were significantly associated with depressive symptoms only in adolescent girls' suggests that the same negative parental cues are differentially related to child outcome in adolescent boys and girls. Although the smaller sample size of adolescent boys compared to girls in this study could have contributed to lower statistical power for detecting significant associations, the small magnitude of the correlations found for boys suggests that this is an unlikely cause for the lack of significant findings. It is important to note that, given the cross-sectional design of this study, the directionality of the associations cannot be discerned from these data. Thus, although these results are consistent with the hypothesis that the higher levels of depressive symptoms in adolescent girls resulted from their greater sensitivity to their parents' negative attributions, one cannot rule out other causal possibilities.
Consistent with our hypotheses, mothers' negative attributions partially mediated the link between maternal and adolescent girls' levels of depressive symptoms. The fact that mothers' levels of depressive symptoms were related to their negative attributions for adolescent girls' behaviors is consistent with the results of previous studies conducted with younger children (Bolton et al., 2003; Leung & Smith Slep, 2006), and contributes to the literature by highlighting maternal negative attributions as an important aspect of parenting that may serve to link parental and adolescent depressive symptoms. The results of our regression model show that, controlling for mothers' depressive symptoms, mothers' negative attributions accounted for 6% of the variance in their adolescent daughters' depressive symptoms. Although this effect may appear modest, it is important to keep in mind that the significant correlation between maternal depressive symptoms and negative attributions renders this a conservative test of the potential influence of negative attributions. Furthermore, our results suggest that not only are mothers' negative attributions related to their adolescent daughters' depressive symptoms, these negative interpretations of the adolescent girls' behaviors may constitute one of the pathways through which the transmission of depressive symptoms from mothers to daughters occurs.
With respect to fathers, our results indicate that, controlling for fathers' depressive symptoms, fathers' negative attributions accounted for 19% of the variance in their adolescent daughters' depressive symptoms. That fathers' attributions appear to be more strongly associated with adolescent depressive symptoms than were mothers', likely reflects the unanticipated finding that fathers' depressive symptoms were unrelated to their negative attributions, and hence, made a unique contribution. The absence of a correlation between fathers' attributions and their depressive symptoms is in contrast to the results of Leung and Smith Slep (2006). One major difference between the two studies is that the parents in Leung and Smith's study were making attributions for a much younger group of children (i.e., 3 to 7 years of age). Our impression, based on coding of the attributions, is that fathers' attributions for the adolescents' behaviour were related to general attitudes towards youth (e.g., the appropriateness of various adolescent behaviours) and were more closely linked to negative affective states of anger than to depressive symptoms (e.g., “he is arguing just to be arguing”; “so he can hopefully get us to shut up”; “she is trying to avoid what she needs to do by bringing it back to her sister's issues”). Thus, although fathers' negative attributions were found to be related to the levels of depressive symptoms in their adolescent daughters, fathers' negative attributions were unrelated to their own levels of depressive symptoms, and may instead be related to a different set of parental characteristics than were mothers.
There are a number of shortcomings in this study. As noted above, the cross-sectional design does not allow us to draw conclusions regarding the directionality of the associations. Future longitudinal studies are needed to elucidate the directionality of these associations. In addition, the majority of the families included in this study were European-American, and of middle class, which limits the generalizability of the findings. Finally, we used a dimensional approach to assess both adolescent and parental depressive symptoms in this study, and further research would be needed to examine the extent to which these findings hold in groups based on adolescent and/or parental diagnostic status.
Nonetheless, this study makes an important contribution to the extant literature by investigating the link between parents' attributions and internalizing problems in adolescents – an area of functioning and an age group that are both relatively unexplored in the literature on parental attributions. Furthermore, the use of an observational rather than self-report measure of parents' attributions enhances the interpretability of the results as it reduces the potential confounding effects of method variance. Finally, given the dearth of studies on fathers and child psychopathology (Phares, Fields, Kamboukos, & Lopez, 2005), the inclusion of both mothers and fathers in this study is a considerable strength. In hopes of guiding future research in this area, we highlight the need for studies to examine which paternal characteristics may better predict fathers' negative attributions and which parental cognitions or behaviors may be more closely linked to depressive symptoms in adolescent boys. The findings of this study also point to the need to further examine the mechanisms that may underlie the link between parental negative attributions and adolescent girls' depressive symptoms. For example, there is a need to explore the extent to which the influence of parental negative attributions is mediated by harsh and critical parenting behaviour and/or by adolescents' perceptions of their parents' attitudes and behaviours. Previous studies have shown, for example, that children who perceive their parents as more rejecting have more maladaptive beliefs about their own ability to produce desired outcomes (Rudolph, Kurlakowsky, & Conley, 2001). In addition, there is a need to explore other potential mechanisms that may underlie the findings of gender differences, such as whether adolescent girls may be more vulnerable to depression because they, more so than boys, internalize negative parental attributions or because they are more likely to adopt a negative cognitive style through modelling of parents' negative cognitions. Bruce et al. (2006) have speculated, for example, that internalization may be one of mechanism by which children develop negative self-concepts from negative parental feedback. Such internalizations of negative attributions or cognitive styles may thus serve as more proximal risk factors for the development of depression in adolescent females.
Clinically, these results highlight the importance for clinicians working with depressed adolescent girls to attend to the levels of depression in their parents, as well as to assess how the adolescents' depression may be affecting or affected by their parents' perceptions of their behaviors. Given that both mothers' and fathers' negative attributions were related to their adolescent daughters' levels of depressive symptoms, it is important to assess both parents' attributions whenever feasible. Clinicians should explore parents' understanding of their adolescents' behavior, and be mindful of the degree to which parents are making child-blaming interpretations. The fact that parent-adolescent relationships have significant implications for adolescent depression is acknowledged by a number of current treatment approaches which incorporate intervention modules that address this issue. These include cognitive-behavioral (e.g., Wells & Albano, 2005) and interpersonal (e.g., Mufson & Dorta, 2000) interventions as well as treatments that are primarily family focused (e.g., Diamond, Siqueland, & Diamond, 2003). Attending to parental attributions for adolescent behavior would thus be relevant in the context of these intervention sessions. Finally, as more information on the mechanism underlying the link between parents' negative attributions and depression in adolescent girls emerges, it may provide the foundation for interventions designed to alter parental attributions in hopes of reducing adolescents' depression and decoupling the transmission of depression from mothers to adolescent girls.
Table 2.
Regression Analyses Examining the Moderating Effect of Adolescent Gender
| Predictors | B | SE B | Beta | t | p | |
|---|---|---|---|---|---|---|
| Mothers | ||||||
| Step 1 | Adolescent Gender | -1.75 | 1.09 | -.14 | -1.61 | .11 |
| Negative Attribution | 13.94 | 5.37 | .23 | 2.60 | .01 | |
| Step 2 | Adolescent Gender × Negative Attribution | -11.96 | 5.37 | -.19 | -2.23 | .03 |
| Fathers | ||||||
| Step 1 | Adolescent Gender | -1.97 | 1.07 | -.16 | -1.85 | .07 |
| Negative Attribution | 13.13 | 5.48 | .21 | 2.40 | .02 | |
| Step 2 | Adolescent Gender × Negative Attribution | -15.36 | 5.48 | -.25 | -2.80 | .01 |
Acknowledgments
We thank the families who participated in this study, and Wade Cook, Erin Hutton, and Krista Newbigging for their assistance with the coding of parental attributions. We would also like to thank Dr. Mathew Sanders for his help in designing the VMR protocol. This research was supported by the University of British Columbia Hampton Research Fund PG# 12R78316, and the National Institute of Mental Health Grant #57166.
Contributor Information
Mandy Chen, University of British Columbia.
Charlotte Johnston, University of British Columbia.
Lisa Sheeber, Oregon Research Institute.
Craig Leve, Oregon Research Institute.
References
- Aalto-Setälä T, Marttunen M, Tuulio-Henriksson A, Poikolainen K, Löonqvist J. Depressive symptoms in adolescence as predictors of early adulthood depressive disorders and maladjustment. American Journal of Psychiatry. 2002;159:1235–1237. doi: 10.1176/appi.ajp.159.7.1235. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: Author; 1994. [Google Scholar]
- Beardslee WR, Keller MB, Seifer R, Lavori PW, Staley J, Podorefsky D. Prediction of adolescent affective disorder: Effects of prior parental affective disorders and child psychopathology. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:279–288. doi: 10.1097/00004583-199603000-00008. [DOI] [PubMed] [Google Scholar]
- Biglan A, Ary DV. Methodological issues in research on smoking prevention. In: Bell CS, Battjes R, editors. Prevention research: Deterring drug abuse among children and adolescents. Rockville, MD: U.S. Department of Health and Human Services; 1990. pp. 170–195. NIDA Research Monograph Series, No. 63. [Google Scholar]
- Birmaher B, Ryan ND, Williamson D, Brent DA. Childhood and adolescent depression: a review of the past 10 years, Part 1. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1427–1439. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- Bolton C, Calam R, Barrowclough C, Peters S, Roberts J, Wearden A, Morris J. Expressed emotion, attributions, and depression in mothers of children with problem behavior. Journal of Child Psychology and Psychiatry. 2003;44:242–254. doi: 10.1111/1469-7610.00117. [DOI] [PubMed] [Google Scholar]
- Bruce AE, Cole DA, Dallaire DH, Jacquez FM, Pineda AQ, LaGrange B. Relations of parenting and negative life events to cognitive diatheses for depression in children. Journal of Abnormal Child Psychology. 2006;34:321–333. doi: 10.1007/s10802-006-9019-x. [DOI] [PubMed] [Google Scholar]
- Burge D, Hammen C. Maternal communication: predictors of outcome at follow-up in a sample of children at high and low risk for depression. Journal of Abnormal Psychology. 1991;100:174–180. doi: 10.1037//0021-843x.100.2.174. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? Journal of Child Psychology and Psychiatry. 2006;47:1263–1271. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Young E, Shear K. Adolescent onset of the gender difference in lifetime rates of major depression. Archives of General Psychiatry. 2000;57:21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Mullins MJ, McAllister RA, Atkinson EG. Attributions, affect, and behavior in abuse-risk mothers: A laboratory study. Child Abuse & Neglect. 2003;27:21–45. doi: 10.1016/s0145-2134(02)00510-0. [DOI] [PubMed] [Google Scholar]
- Diamond G, Siqueland L, Diamond GM. Attachment-based family therapy for depressed adolescents: Programmatic treatment development. Clinical Child and Family Psychology Review. 2003;6:107–127. doi: 10.1023/a:1023782510786. [DOI] [PubMed] [Google Scholar]
- Dix T, Ruble D, Grusec J, Nixon S. Social cognition in parents: Inferential and affective reactions to children of three age levels. Child Development. 1986;57:879–894. [PubMed] [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- Eberhart NK, Shih JH, Hammen CL, Brennan P. Understanding the sex difference in vulnerability to adolescent depression: an examination of child and parent characteristics. Journal of Abnormal Child Psychology. 2006;34:495–508. doi: 10.1007/s10802-006-9020-4. [DOI] [PubMed] [Google Scholar]
- Essau CA. The association between family factors and depressive disorders in adolescents. Journal of Youth and Adolescence. 2004;33:365–372. [Google Scholar]
- Gamble S, Roberts JE. Adolescents' perceptions of primary caregivers and cognitive style: the roles of attachment security and gender. Cognitive Therapy and Research. 2005;29:123–141. [Google Scholar]
- Gartstein MA, Sheeber L. Child behavior problems and maternal symptoms of depression: a mediational model. Journal of Child and Adolescent Psychiatric Nursing. 2004;17:141–150. doi: 10.1111/j.1744-6171.2004.tb00011.x. [DOI] [PubMed] [Google Scholar]
- Ge X, Conger RD, Lorenz FO, Shanahan M, Elder GH., Jr Mutual influences in parent and adolescent psychological distress. Developmental Psychology. 1995;31:406–419. [Google Scholar]
- Ge X, Conger RD, Lorenz FO, Simons RL. Parents' stressful life events and adolescent depressed mood. Journal of Health and Social Behavior. 1994;35:28–44. [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Goodyer IM, Altham PM. Lifetime exit events and recent social and family adversities in anxious and depressed school-age children and adolescents: I. Journal of Affective Disorders. 1991;21:219–228. doi: 10.1016/0165-0327(91)90001-9. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Goodman SH. Children of parents with depression. In: Silverman WK, Ollendick TH, editors. Developmental issues in the clinical treatment of children. Needham Heights, MA: Allyn & Bacon; 1999. pp. 415–432. [Google Scholar]
- Gotlib IH, Lewinsohn PM, Seeley JR. Symptoms versus a diagnosis of depression: differences in psychosocial functioning. Journal of Consulting and Clinical Psychology. 1995;63:90–100. doi: 10.1037//0022-006x.63.1.90. [DOI] [PubMed] [Google Scholar]
- Hale WW, III, Van Der Valk I, Engels R, Meeus W. Does perceived parental rejection make adolescents sad and mad? The association of perceived parental rejection with adolescent depression and aggression. Journal of Adolescent Health. 2005;36:466–474. doi: 10.1016/j.jadohealth.2004.04.007. [DOI] [PubMed] [Google Scholar]
- Hakim-Larson J, Dunham K, Vellet S, Murdaca L, Levenbach J. Parental affect and coping. Canadian Journal of Behavioural Science. 1999;31:5–18. [Google Scholar]
- Hammen C, Burge D, Stansbury K. Relationship of mother and child variables to child outcomes in a high-risk sample: A causal modeling analysis. Developmental Psychology. 1990;26:24–30. [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: an elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hastings PD, Rubin KH. Predicting mothers' beliefs about preschool-aged children's social behaviour: evidence for maternal attitudes moderating child effects. Child Development. 1999;70:722–741. doi: 10.1111/1467-8624.00052. [DOI] [PubMed] [Google Scholar]
- Heatherington L, Tolejko N, McDonald M, Funk J. Now why'd he do that? The nature and correlates of mothers' attributions about negative teen behavior. Journal of Family Psychology. 2007;21:315–319. doi: 10.1037/0893-3200.21.2.315. [DOI] [PubMed] [Google Scholar]
- Hops H. Parental depression and child behavior problems: implications for behavioural family intervention. Behaviour Change. 1992;9:126–138. [Google Scholar]
- Joiner TE, Jr, Wagner KD. Parental, child-centered attributions and outcome: A meta-analytic review with conceptual and methodological implications. Journal of Abnormal Child Psychology. 1996;24:37–52. doi: 10.1007/BF01448372. [DOI] [PubMed] [Google Scholar]
- Johnston C, Chen M, Ohan J. Mothers' attributions for behavior in nonproblem boys, boys with Attention Deficit/Hyperactivity Disorder, and boys with Attention Deficit/Hyperactivity Disorder and oppositional defiant behavior. Journal of Clinical Child and Adolescent Psychology. 2006;35:60–71. doi: 10.1207/s15374424jccp3501_6. [DOI] [PubMed] [Google Scholar]
- Johnston C, Freeman W. Attributions for child behavior in parents of children with behavior disorders and children with attention-deficit/hyperactivity disorder. Journal of Consulting Psychology. 1997;65:636–645. doi: 10.1037/0022-006X.65.4.636. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Presentation and course of major depressive disorder during childhood and later years of the lifespan. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:705–715. doi: 10.1097/00004583-199606000-00010. [DOI] [PubMed] [Google Scholar]
- Leung DW, Smith Slep AM. Predicting inept discipline: the role of parental depressive symptoms, anger, and attributions. Journal of Consulting and Clinical Psychology. 2006;74:524–534. doi: 10.1037/0022-006X.74.3.524. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Klein DN, Seeley JR. Natural course of adolescent major depressive disorder, I: continuity into young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:56–63. doi: 10.1097/00004583-199901000-00020. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- MacBrayer EK, Milich R, Hundley M. Attributional biases in aggressive children and their mothers. Journal of Abnormal Psychology. 2003;112:698–708. doi: 10.1037/0021-843X.112.4.598. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Mediation analysis. Annual Review of Psychology. 2007;58:693–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence intervals for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller SA. Parents' attributions for their children's behavior. Child Development. 1995;66:1557–1584. [PubMed] [Google Scholar]
- Mills RSL, Rubin KH. Parental beliefs about problematic social behaviors in early childhood. Child Development. 1990;61:138–151. [Google Scholar]
- Mufson L, Dorta KP. Interpersonal psychotherapy for depressed adolescents: Theory, practice, and research. In: Esman AH, Flaherty LT, Horowitz HA, editors. Adolescent psychiatry: Developmental and clinical studies. Mahwah, NJ: Analytic Press; 2000. pp. 139–167. [Google Scholar]
- Muris P, Schmidt H, Lambrichs R, Meesters C. Protective and vulnerability factors of depression in normal adolescents. Behaviour Research and Therapy. 2001;39:555–565. doi: 10.1016/s0005-7967(00)00026-7. [DOI] [PubMed] [Google Scholar]
- Nix RL, Pinderhughes EE, Dodge KA, Bates JE, Pettit GS, McFadyen-Ketchum SA. The relation between mothers' hostile attribution tendencies and children's externalizing behaviour problems: the mediating role of mothers' harsh discipline practices. Child Development. 1999;70:896–909. doi: 10.1111/1467-8624.00065. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J. Schedule for Affective Disorder and Schizophrenia for School-Age Children: Epidemiologic version. 1994 Unpublished manual. [Google Scholar]
- Patterson G, Chamberlain P, Reid JB. A comparative evaluation of a parent-training program. Behavior Therapy. 1982;13:638–650. doi: 10.1016/j.beth.2016.11.004. [DOI] [PubMed] [Google Scholar]
- Phares V, Fields S, Kamboukos D, Lopez E. Still looking for poppa. American Psychologist. 2005;60:735–736. doi: 10.1037/0003-066X.60.7.735. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen E, Cohen P, Brook J. Adolescent depressive symptoms as predictors of adult depression: Moodiness or mood disorder? American Journal of Psychiatry. 1999;156:133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- Radke-Yarrow M, Klimes-Dougan B. Parental depression and offspring disorders: a developmental perspective. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. pp. 155–173. [Google Scholar]
- Radloff LS. A CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Radloff LS, Teri L. Use of the Center for Epidemiological Studies-Depression Scale with older adults. Clinical Gerontologist. 1986;5:119–136. [Google Scholar]
- Rao U, Weissman MM, Martin JA, Hammond RW. Childhood depression and risk of suicide: a preliminary report of a longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:21–27. doi: 10.1097/00004583-199301000-00004. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Andrews JA, Lewinsohn PM, Hops H. Assessment of depression in adolescents using the Center for Epidemiologic Studies Depression Scale. Psychological Assessment. 1990;2:122–128. [Google Scholar]
- Rudolph KD. Gender differences in emotional responses to interpersonal stress during adolescence. Journal of Adolescent Health. 2002;30:3–13. doi: 10.1016/s1054-139x(01)00383-4. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Kurlakowsky KD, Conley CS. Developmental and social-contextual origins of depressive control-related beliefs and behavior. Cognitive Therapy and Research. 2001;25:447–475. [Google Scholar]
- Sanders MR, Dadds MR, Johnston BM, Cash R. Childhood depression and conduct disorder: I. Behavioral, affective, and cognitive aspects of family problem-solving interactions. Journal of Abnormal Psychology. 1992;101:495–504. [PubMed] [Google Scholar]
- Severson HH, Ary DV. Sampling bias due to consent procedures with adolescents. Addictive Behaviors. 1983;8:433–473. doi: 10.1016/0306-4603(83)90046-1. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Davis B, Hops H. Gender-specific vulnerability to depression in children of depressed mothers. In: Goodman SH, Gotlib IH, editors. Children of depressed parents: Mechanisms of risk and implications for treatment. Washington, DC: American Psychological Association; 2002. pp. 253–274. [Google Scholar]
- Sheeber LB, Davis B, Leve C, Hops H, Tildesley E. Adolescents' relationships with their mothers and fathers: associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology. 2007;116:144–154. doi: 10.1037/0021-843X.116.1.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shih JH, Eberhart NK, Hammen CL, Brennan P. Differential exposure and reactivity to interpersonal stress predict sex differences in adolescent depression. Journal of Clinical Child and Adolescent Psychology. 2006;35:103–115. doi: 10.1207/s15374424jccp3501_9. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Smith AM, O'Leary SG. Attributions and arousal as predictors of maternal discipline. Cognitive Therapy and Research. 1995;19:459–471. [Google Scholar]
- Smith Slep A, O'Leary S. The effects of maternal attributions on parenting: An experimental analysis. Journal of Family Psychology. 1998;12:234–243. [Google Scholar]
- Snyder J, Cramer A, Afrank J, Patterson GR. The contributions of ineffective discipline and parental hostile attributions of child misbehavior to the development of conduct problems at home and school. Developmental Psychology. 2005;41:30–41. doi: 10.1037/0012-1649.41.1.30. [DOI] [PubMed] [Google Scholar]
- Weiner B. An attributional theory of motivation and emotion. New York: Springer-Verlag; 1986. [Google Scholar]
- Wells KC, Albano AN. Parent involvement in CBT treatment of adolescent depression: Experiences in the Treatment of Adolescents with Depression Study (TADS) Cognitive and Behavioral Practice. 2005;12:209–220. [Google Scholar]