Introduction
Obesity continues to increase at alarming rates.1 In Hawaii, obesity has risen 57% since 1994.2 Pacific Islanders have the highest rates of obesity (46%) and shortest life expectancy (68y) of any US race/ethnic group. Body mass index (BMI, kg/m2) of Pacific Islanders and Filipinos is greater than that of Whites in our study population, while BMI of Other Asians is lower than that of Whites. 2 The obesity epidemic affects all segments of the population. National Health and Nutrition examination (NHANES) data from 2003–2004 found that the percentage overweight (BMI ≥ 25) among adults was 71% in men and 61% in women.3 The percent obese (BMI ≥ 30) was 31% in men and 33% in women.
Obesity is associated with increased risk for chronic disease.4 Increasing rates of obesity are especially associated with diabetes, gallbladder disease, cardiovascular disease, hypertension, sleep apnea, osteoarthritis, and some forms of cancer.5 Nutrition transition and migration have also been associated with both obesity and chronic disease.6 Nutrition transition refers to the turn away from consumption of traditional foods that are rich in fiber and micronutrients, and a turn toward consumption of energy-dense foods. Though a growing body of research attests to the explanatory power of migration and acculturation with respect to obesity among Mexican-Americans 7, 8 and blacks 9 these linkages have been little examined among Asians and Pacific Islanders in the US.
Associations between acculturation and the occurrence of coronary heart disease were found in the Japanese American Study. 10 Preferred language, immigrant status, and years lived in the U.S. have been previously used to determine level of acculturation in some Asian ethnic groups in a previous study of health and health-related risk factors in Northern California. 11 Participants reported their country of birth, country of birth of parents and grandparents (to obtain generational status - first or second generation), number years lived in the US for immigrants, and their age when they or their family moved to U.S. (latter used to classify participant as living < 50% of life in US, 50–75% of life in US, >75% of life in US). An index was created to indicate language preferences for reading, speaking, thinking, conversing with friends, and listening to/watching radio and TV programs. Participants were asked to report if they, or their children, have taken language courses to learn the language of their race/ethnicity’s culture (e.g., Japanese, Hawaiian, etc.)
Immigrants (those born in a country outside of the US) were 12% of the US population in 2003 12, and are a steadily increasing proportion of the population. Identification of risk factors for obesity associated with immigration will be helpful to develop appropriate interventions to prevent or curb obesity in the US. Lifestyle factors that change with migration are associated with obesity- factors such as food intake, physical activity, education level, language spoken at home. In this study, we examine migration-related influences on obesity among multi-ethnic hotel workers.
We focus on examining measures of immigration and acculturation on obesity and risk for chronic disease among Asians and Pacific Islanders - place of birth, years in US, generation of migration to US, language spoken, education, intake of selected food groups. We hypothesize that immigration and acculturation are associated with increased body mass index (as measured by BMI) in this population.
Methods and Procedures
Study population
The study design for this analysis of immigration and acculturation on BMI is cross-sectional. The sample for this study consists of 4530 hotel workers in 30 hotels (40% of hotel workforce) who were enrolled during the first year of the Work, Weight and Wellness (3W) program - a group-randomized clinical trial that aims to decrease obesity among hotel workers in Hawaii 2. Hotel workers were chosen for several reasons. First, the industry is world-wide and the work and the labor practices are very similar regardless of location, at least in major chain hotels. Second, the large number of hotels on Oahu provided more opportunities to randomize sites within a single industry, more than any other type of business. Third, the hotel industry is the pivot point of Hawaii’s major economic engine--tourism. Data were collected prior to intervention, in 2005–2006.
Measurements
Anthropometry
Weight was measured in pounds on a Tanita WB-100 Series Digital Physician Scale (Arlington Heights, Illinois), to the nearest 0.1 lb. Height was measured with a Seca 214 Road Rod (Ontario, CA) to the nearest 0.125 in. Body Mass Index (BMI), kg/m2, was calculated.
Participants filled out an employee questionnaire and were assisted by study staff on an as-needed basis. The questionnaire was available in three languages: English, Chinese or Korean (Filipino hotel workers spoke English). We validated the Chinese and Korean versions of the questionnaires by comparing a back-translated version produced by a separate translator with the original English version. The employee questionnaire covered the areas below. Six separate elements were taken from referenced and previously validated instruments. These include:
Race/Ethnicity Question
Race/Ethnicity was determined with the following questions,
“What race or races do you consider yourself to be? (check all that apply)” (White, Black/African American, Filipino, Samoan, Japanese, Chinese, Korean, Hispanic or Latino, American Indian, Vietnamese, Asian Indian, Vietnamese, Alaskan Native, Guamanian, Other Pacific Islander (please specify ______), Other Asian (please specify______), Native Hawaiian, Other race (please specify______), Don’t know
“If you checked more than one, with which race group do you most strongly identify?” (If they did not identify one ethnicity most identified with, an algorithm was used to classify them to one ethnicity).
Participants could select more than one choice from among 18 race/ethnic categories. We instructed participants who chose more than one category to indicate which they preferred most. When participants chose more than one race/ethnicity and did not provide a preference, a category was assigned in this priority: Samoan, Native Hawaiian, Guamanian, Other Pacific Islander, American Indian, Alaskan Native, Black/African American, Filipino, Korean, Vietnamese, Japanese, Chinese, Other Asian, Hispanic or Latino, Asian Indian, White, Other Race, Don’t Know. If they chose a category beginning with “Other” they were asked to specify their ethnicity by writing in their response. All written responses were examined by the investigators and assigned to one of the 18 categories. For example, written responses of “Hong Kong” were assigned to the Chinese category. Participants who made no choice or selected “Don’t Know” were counted as missing.
We reduced these 18 ethnic categories to the following five larger ethnic categories: Asian, Filipino, Pacific Islander, White, and Other. Participants in the Samoan, Native Hawaiian, Guamanian, or Other Pacific Islander categories were assigned to the larger Pacific Islander category. We assigned participants in the Korean, Vietnamese, Japanese, Chinese, Other Asian, to the larger Asian category. We assigned participants in the Filipino or White category to the corresponding larger category. The remaining categories had too few participants to warrant a separate group: American Indian, Alaskan Native, Black/African American, Hispanic or Latino, Other Race. We assigned participants in these groups to the larger Other category. We made Filipino a separate category from Asian for two reasons: (1) The number of Filipino participants was very large relative to the other Asian race/ethnic groups. (2) The BRFSS data show that the Filipino community in Hawaii is at higher risk for obesity and for obesity-related illnesses such as Diabetes than other Asian groups. Further, while Filipinos are from the Asian continent and are classified as Asian by the federal Office of Management and Budget guidelines and census data, we keep them as a separate group since many individuals in Hawaii were born in the Philippines and there were several waves of migration to Hawaii, which is of importance to our analysis. Thus, for this analysis, race/ethnicities were as follows: Filipino, Other Asian/Other Asian American, Pacific Islander, White (not Hispanic), Other. There were missing race/ethnicity data on 126 subjects who were excluded from all analyses. Hispanic was not treated as a separate race/ethnic category in this analysis. Eight percent of the sample selected Hispanic as one race/ethnicity. These individuals were collapsed to one of the other race/ethnic groups due to multiple race/ethnic selections. The 8% were collapsed to the following race/ethnic categories: Filipino (3%), Other Asian (1%), Pacific Islander (2%), and Other (2%)
Immigration variables
The following migration question was asked on the questionnaire:
-
How long have you lived in the United States? (check only one)
▪ All my life or
▪ I have lived in the US for (fill in the blank) ___ years
The following immigration variables were calculated for use in analysis:
Born in US- Yes/No
-
Generation when came to US
0 - born in US
1 - came to US before age 19
2 - came to US at age 19 or older
Birth place categories were created as: East Asia, Hawaii, Other Pacific Islands, Philippines and US mainland
Language Question
What language do you usually speak at home? English, Chinese (Mandarin or Cantonese), Tagalog, Korean, Ilocano, Japanese
Education Question
What is the most school that you have completed? 8th grade or less; some high school, but did not graduate; high school graduate or GED; some college or 2-year degree; technical/business school graduate; college graduate; post-graduate degree (master’s, doctorate, or equivalent).
Acculturation Scale
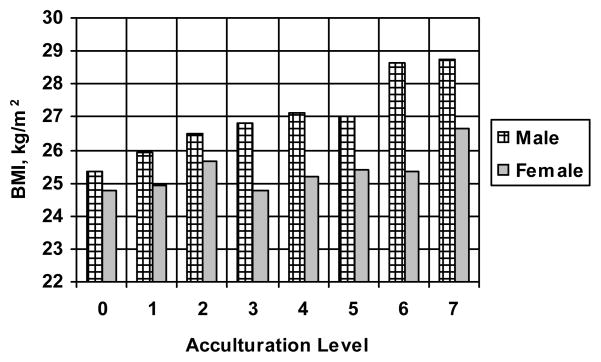
Building on prior work on the association between acculturation and BMI among Mexican immigrants 22, we developed the following scale of acculturation. The scale provides an increased score for later age at migration to the US, migration from an English speaking country, English spoken at home, and a higher educational level (Figure 2).
Figure 2.
BMI by Sex and Acculturation Level
Legend:
0 = came to US age 19 or older + came from non-European or non-English-speaking country, English not spoken at home, education < high school (HS)
1 = came to US at age 19 or older, came from non-European or non-English-speaking country, English not spoken at home, education >= HS
2 = came to US at age 19 or older, came from non-European or non-English-speaking country, English spoken at home, education < HS
3 = came to US at age 19 or older, came from non-European or non-English-speaking country, English spoken at home, education >= HS
4 = came to US before age 19 or English spoken at home, came from non-European or non-English speaking country, education <= HS
5 = came to US before age 19 or English spoken at home, came from non-European or non-English-speaking country, education >= HS
6 = born in US, came from European or English-speaking country
7 = born in US + English spoken at home
Dietary Questions
Dietary questions were queried in number of servings/day, with examples and descriptions of portion size (eg. How many servings of sweetened drinks or soda do you drink in a day? A serving is a 12 oz. can, a small size drink, or one regular glass. Examples of sweetened drinks include regular soda, sweetened fruit juices and teas, punch, Hawaiian Sun, and coffee drinks.) Questions were derived from published references. 23–26
Analyses
We modeled BMI as a function of immigration status, generation, ethnicity, age, acculturation, gender, and food intake in a series of regression models. We estimated the models’ parameters using maximum likelihood within the general linear model framework as implemented in the PROC GLM routines of the SAS v9.1 software package (Carey, North Carolina, 2007). In keeping with the model building nature of our work, our primary interest was in the size of the parameter estimates rather than the significance of the (unadjusted) p values for each parameter. We retained variables in the model if they were significant at p < 0.1 or if we judged that there was a clear scientific justification for the expectation that they would impact the results.
Human Subjects
The study was conducted by the Kaiser Permanente Center for Health Research Hawaii. The Kaiser Permanente Institutional Review Board approved the study. Informed consent was obtained from each participant.
Results
The study sample was composed of 1941 males (43%) and 2514 females (57%), with a mean age of 44.4 (± 11.3) years. The population was 42% Filipino, 32% Other Asian, 13% Pacific Islander, 9% White, 1% Black/African American and 3% Other. The mean BMI was 26.5 (±5.0 kg/m2). Forty percent of the sample had less than or equal to a high school education, while 60% had more than a high school education. Fifty five percent of hotel workers were born outside of the US: 38% in the Philippines, 3% in Japan, 3% in Southeast Asia, 1% in other Pacific Islands and 10% in other locations (eg. China, Korea, Hong Kong…). Of the 45% that were born in the US, 35% were born in Hawaii and 10% were born on the US mainland.
Fifty-seven percent of the sample was overweight or obese (BMI ≥ 25 kg/m2) while less than 1% were underweight (BMI ≤ 18.5). The BMI of those born in the US was 2.2 kg/m2 higher than that of those born in another country.
In a model testing the influence of immigration on BMI showed that, after adjusting for sex and ethnicity, those born in the US were 1.3 kg/m2 heavier than those not born in the US (Table 1, Model 1). Females were 2.1 kg/m2 lighter than males. Other Asians were 1.1 kg/m2 smaller than Whites, while Filipinos were 1.3 kg/m2 heavier, and Pacific Islanders were 3.2 kg/m2 heavier than Whites. Educational level did not significantly contribute to the model (not shown). On the other hand, a model testing the interaction of immigrant with sex was significant (the effect of immigration was dependent on sex, with male immigrants having higher BMI than female immigrants, not shown), as was a model testing the interaction of immigrant status with race/ethnicity (the effect of immigration being dependent on ethnicity, with Filipino and Pacific Islanders having higher BMI than Whites, and Other Asians and having lower BMI than Whites, not shown). In order to test the role of food groups on BMI we tested a model adjusting for diet (not shown) resulted in servings of sweet drinks and meat showing positive association with BMI, and serving of fruit showing negative association with BMI, when the immigrant variable was taken out and Filipino race/ethnicity was added to the model (R2= 17.9%).
Table 1.
Models of Migration and Related Influences on BMI
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Parameter Est. | SE | P< | Parameter Est. | SE | P< | Parameter Est. | SE | P< | Parameter Est. | SE | P< |
| Intercept | 28.24 | 0.027 | 0.0001 | 24.11 | 0.047 | 0.0001 | 24.42 | 0.58 | 0.0001 | 23.14 | 0.69 | 0.0001 |
| Immigrant | −1.33 | 0.61 | 0.03 | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| Female | −2.12 | 0.21 | 0.0001 | −1.96 | 0.47 | 0.0001 | −1.69 | 0.22 | 0.0001 | −0.67 | 0.69 | 0.0001 |
| Other Asian ethnicity* | −1.14 | 0.30 | 0.0002 | --- | --- | --- | --- | --- | --- | −1.66 | 0.35 | 0.0001 |
| Filipino ethnicity* | 1.31 | 0.38 | 0.0006 | --- | --- | --- | --- | --- | --- | 0.83 | 0.42 | 0.05 |
| Other ethnicity* | 0.34 | 0.54 | 0.53 | --- | --- | --- | --- | --- | --- | 0.02 | 0.48 | 0.98 |
| Pacific Islander ethnicity* | 3.22 | 0.33 | 0.0001 | --- | --- | --- | --- | --- | --- | 2.81 | 0.38 | 0.0001 |
| Ethnicity other than White | --- | --- | --- | --- | --- | --- | 0.86 | 0.31 | 0.0001 | --- | --- | --- |
| Born in East Asia# | --- | --- | --- | −3.17 | 0.45 | 0.0001 | --- | --- | --- | −0.81 | 0.49 | 0.10 |
| Born in Hawaii# | --- | --- | --- | 0.67 | 0.35 | 0.05 | --- | --- | --- | 0.48 | 0.33 | 0.15 |
| Born in the Pacific | --- | --- | --- | 4.35 | 1.03 | 0.60 | --- | --- | --- | 2.46 | 0.69 | 0.0004 |
| Islands# | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- |
| Born in the Philippines# | --- | --- | --- | −1.61 | 0.36 | 0.0001 | --- | --- | --- | −1.44 | 0.51 | 0.005 |
| Born in any other Place | --- | --- | --- | --- | --- | --- | --- | --- | --- | −0.44 | 0.55 | 0.42 |
| Age, y | --- | --- | --- | 0.04 | 0.006 | 0.0001 | 0.06 | 0.007 | 0.0001 | 0.06 | 0.007 | 0.0001 |
| Sweetened Drinks, servings/day | --- | --- | --- | 0.32 | 0.07 | 0.0001 | 0.36 | 0.08 | 0.0001 | 0.23 | 0.07 | 0.002 |
| Fruit, servings/day | --- | --- | --- | −0.24 | 0.086 | 0.04 | −0.21 | 0.09 | 0.02 | −0.28 | 0.08 | 0.0006 |
| Meat, servings/day | --- | --- | --- | 0.59 | 0.09 | 0.0001 | 0.72 | 0.09 | 0.0001 | 0.60 | 0.09 | 0.0001 |
| Generation (later arrival in US) | --- | --- | --- | --- | --- | --- | −1.49 | 0.28 | 0.0001 | --- | --- | --- |
| Sex × Generation | --- | --- | --- | --- | --- | --- | 0.39 | 0.17 | 0.02 | --- | --- | --- |
| Acculturation Scale, 0–7 | --- | --- | --- | --- | --- | --- | --- | --- | --- | 0.24 | 0.08 | 0.002 |
| Acculturation × Female | --- | --- | --- | --- | --- | --- | --- | --- | --- | −0.19 | 0.06 | 0.0016 |
R2: Model 1= 17.1%, Model 2=14.0%, Model 3=13.2%, Model 4= 19.6%; Models of body mass index used three different measures of migration. Model 1. Immigration status, Model 2. Place of Birth, Model 3. Generation, Model 4. A calculated acculturation scale (see figure legend explaining the acculturation scale).
Reference Ethnicity= White
Reference Birth Place= Born US Mainland (continental US)
Testing a model describing migration using the variable, place of birth (rather than immigrant status), showed that those born in the Philippines had a BMI 1.6 kg/m2 lower than those born on the US mainland, and those born in Southeast Asia had a BMI 3.2 kg/m2 lower (Table 1, Model 2). Those born in the Pacific Islands had a BMI that was 4.4 kg/m2 higher than those born on the US mainland. There was no significant interaction of sex and birth place.
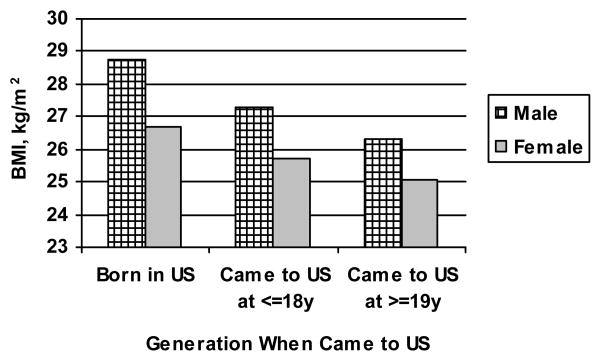
Testing the role of age at arrival in the US (“generation”) on BMI, we found a negative linear relationship (Figure 1), with males larger than females. A regression model (Model 3, Table 1) shows this relationship, and that the interaction of generation and sex is significant; the effect of generation is dependent on sex, where living in the US had a stronger negative influence on BMI (greater BMI) in males than in females.
Figure 1.
BMI by Sex and Generation When Came to US
Examining migration using the variable “acculturation” yielded a similar relationship (Figure 2), where greater acculturation is associated with greater BMI, especially among males. A regression model explains 20% of the variability in BMI with sex, age, race/ethnicity, place of birth, food intake and acculturation measures (Table 1, Model 4). Another model (not shown) demonstrated significant interaction of acculturation and sex, demonstrating that acculturation depended on sex, where more acculturated females have a lower BMI than more acculturated males. Though we found higher BMI among the more acculturated participants of both sexes, the increase of BMI with acculturation was markedly greater among males.
Discussion
Many factors may explain racial/ethnic differences in BMI in Hawaii. There may be genetic differences between racial/ethnic groups, which are beyond the scope of this study to elaborate. There are many possible environmental factors that may influence BMI, including prenatal, childhood and adult exposures that may differ in the US as compared to other countries of birth. These differential exposures have been found to have an especially strong influence in the fetal period, and to be associated with mother’s nutritional state. There may be early life programming to level of nutritional status, which is maladapted to later relative excess.27 “Environmental” exposures of importance to BMI include nutrition and physical activity exposures during postnatal life.6, 28 These exposures are likely partially captured by our measurements of place of birth, generation of migration to the US and by our acculturation scale, though direct measure of diet added explanatory power to our models.
There were historical waves of immigration of the different race/ethnic groups to Hawaii at different times, which may have some relationship to that group’s adaptation to the environment. Native Hawaiians arrived first to Hawaii from Polynesia; and, indeed, the Native Hawaiian ethnic group has the highest BMI29, Chinese, Japanese and Filipinos migrated to Hawaii later than the Polynesians, and they have lower average BMI. 30] We found the difference in BMI to be more pronounced by country of birth than by race/ethnicity, reflecting the importance of these “environmental” differences, even though both race/ethnicity variables and place of birth explained variability in BMI in our models. Other investigators have found that dietary changes are stronger predictors of BMI than race/ethnicity.31 In our study, BMI was 1.3–1.5 kg/m2 larger if born in US.
Similar findings, and magnitude of effect, have been found among Mexican immigrants to the US. 32 On the other hand, different race/ethnic groups may have different BMI levels that indicate health risk. Different race/ethnic groups have different genetic traits, skeletal dimensions, body composition, dietary intake and activity patterns that may influence the sensitivity and specificity of specific BMI cut points as risk indicators of disease 33. This area of study deserves further attention.
Being male, Pacific Islander, living a longer time in US, eating less fruit, eating more sweetened drinks and meat, and being more acculturated were associated with higher BMI in our study. On the other hand, highly acculturated women had a lower BMI, as did Other Asians. These data suggest that diet may be partially responsible for the higher BMI of those living longer in US.
Strengths of our study are the large numbers, race/ethnicity detail and measured (vs. self-reported) data on obesity. Limitations are the cross-sectional design, for understanding causality, limited demonstration of reliability and validity of measurements, lack of measures of dietary energy intake and not controlling for physical activity. Future studies should further develop tools to measure immigration and acculturation and examine mechanisms of association of immigration and acculturation with obesity. Measurement tools that identify race/ethnic subgroups and elaborate demographic conditions and behaviors, such as dietary and physical activity patterns, will be essential to better conceptualize, model and intervene on migration-related influences on BMI. Also, specific examination of energy intake and expenditure will help pinpoint proximal indicators of BMI. Longitudinal study designs that include different migration patterns, including movement from rural to urban areas, would be especially valuable. Testing of behavior change models specific to immigration patterns and/or ethnic populations, and incorporation of measurements of family structure, family cohesion and other measures of social support, will further advance understanding and interventions in this field.
Acknowledgments
This work was supported by a research grant from the National Institutes of Health/National Heart Lung Blood Institute (5 R01 HL79505, T Vogt, PI).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Stein CJ, Colditz GA. The epidemic of obesity. J Clin Endocrinol Metab. 2004 Jun;89(6):2522–2525. doi: 10.1210/jc.2004-0288. [DOI] [PubMed] [Google Scholar]
- 2.Williams AE, Vogt TM, Stevens VJ, Albright CA, Nigg CR, Meenan RT, Finucane ML. Work, Weight, and Wellness: the 3W Program: a worksite obesity prevention and intervention trial. Obesity (Silver Spring) 2007 Nov;15 Suppl 1:16S–26S. doi: 10.1038/oby.2007.384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007 May;132(6):2087–2102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 4.Pi-Sunyer FX. The obesity epidemic: pathophysiology and consequences of obesity. Obes Res. 2002 Dec;10 Suppl 2:97S–104S. doi: 10.1038/oby.2002.202. [DOI] [PubMed] [Google Scholar]
- 5.Bray GA. Handbook of Obesity Clinical Applications. 2. New York: Marcel Dekker; 2003. p. 1. [Google Scholar]
- 6.Caballero B, Popkin BM. The Nutrition Transition: Diet and Disease in the Developing World. Academic Press; 2002. pp. 1–5. [Google Scholar]
- 7.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000 Jun;29(3):470–477. [PubMed] [Google Scholar]
- 8.Bennett GG, Wolin KY, Askew S, Fletcher R, Emmons KM. Immigration and obesity among lower income blacks. Obesity (Silver Spring) 2007 Jun;15(6):1391–1394. doi: 10.1038/oby.2007.166. [DOI] [PubMed] [Google Scholar]
- 9.Duffey KJ, Gordon-Larsen P, Ayala GX, Popkin BM. Birthplace is associated with more adverse dietary profiles for US-born than for foreign-born Latino adults. J Nutr. 2008 Dec;138(12):2428–2435. doi: 10.3945/jn.108.097105. [DOI] [PubMed] [Google Scholar]
- 10.Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese-Americans. Am J Epidemiol. 1976 Sep;104(3):225–247. doi: 10.1093/oxfordjournals.aje.a112296. [DOI] [PubMed] [Google Scholar]
- 11.Gomez SL, Kelsey JL, Glaser SL, Lee MM, Sidney S. Immigration and acculturation in relation to health and health-related risk factors among specific Asian subgroups in a health maintenance organization. Am J Public Health. 2004 Nov;94(11):1977–1984. doi: 10.2105/ajph.94.11.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bureau UC. Population Profile of the United States - Dynamic Version. 2004:1–4. [Google Scholar]
- 13.Rossi SR, Rossi JS, Rossi-DelPrete LM, Prochaska JO, Banspach SW, Carleton RA. A processes of change model for weight control for participants in community-based weight loss programs. Int J Addict. 1994 Jan;29(2):161–177. doi: 10.3109/10826089409047375. [DOI] [PubMed] [Google Scholar]
- 14.Nigg CR, Burbank PM, Padula C, Dufresne R, Rossi JS, Velicer WF, Laforge RG, Prochaska JO. Stages of change across ten health risk behaviors for older adults. Gerontologist. 1999 Aug;39(4):473–482. doi: 10.1093/geront/39.4.473. [DOI] [PubMed] [Google Scholar]
- 15.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985 Sep;10(3):141–146. [PubMed] [Google Scholar]
- 16.Nigg CR. Physical activity assessment issues in population-based interventions: A stage approach. In: Welk GJ, editor. Physical activity assessments for health-related research. Champaign, IL: Human Kinetics; 2002. pp. 227–239. [Google Scholar]
- 17.Nigg CR. There is more to stages of exercise than just exercise. Exerc Sport Sci Rev. 2005 Jan;33(1):32–35. [PubMed] [Google Scholar]
- 18.Schumann A, Nigg CR, Rossi JS, Jordan PJ, Norman GJ, Garber CE, Riebe D, Benisovich SV. Construct validity of the stages of change of exercise adoption for different intensities of physical activity in four samples of differing age groups. Am J Health Promot. 2002 May–Jun;16(5):280–287. doi: 10.4278/0890-1171-16.5.280. [DOI] [PubMed] [Google Scholar]
- 19.Campbell MK, Reynolds KD, Havas S, Curry S, Bishop D, Nicklas T, Palombo R, Buller D, Feldman R, Topor M, Johnson C, Beresford SA, Motsinger BM, Morrill C, Heimendinger J. Stages of change for increasing fruit and vegetable consumption among adults and young adults participating in the national 5-a-Day for Better Health community studies. Health Educ Behav. 1999 Aug;26(4):513–534. doi: 10.1177/109019819902600409. [DOI] [PubMed] [Google Scholar]
- 20.Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987 Nov;16(6):825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- 21.Scott SG, Bruce RA. Decision-making style: The development and assessment of a new measure educational and psychological measurement. Educational and Psychological Measurement. 1995;55(5):818–831. [Google Scholar]
- 22.Gordon-Larsen P, Harris KM, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc Sci Med. 2003 Dec;57(11):2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- 23.Martinez-Gonzalez MA, Fernandez-Jarne E, Serrano-Martinez M, Wright M, Gomez-Gracia E. Development of a short dietary intake questionnaire for the quantitative estimation of adherence to a cardioprotective Mediterranean diet. Eur J Clin Nutr. 2004 Nov;58(11):1550–1552. doi: 10.1038/sj.ejcn.1602004. [DOI] [PubMed] [Google Scholar]
- 24.Serdula M, Coates R, Byers T, Mokdad A, Jewell S, Chavez N, Mares-Perlman J, Newcomb P, Ritenbaugh C, Treiber F, et al. Evaluation of a brief telephone questionnaire to estimate fruit and vegetable consumption in diverse study populations. Epidemiology. 1993 Sep;4(5):455–463. doi: 10.1097/00001648-199309000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Block G, Gillespie C, Rosenbaum EH, Jenson C. A rapid food screener to assess fat and fruit and vegetable intake. Am J Prev Med. 2000;18(4):248–288. doi: 10.1016/s0749-3797(00)00119-7. [DOI] [PubMed] [Google Scholar]
- 26.Coates RJ, Serdula MK, Byers T, Mokdad A, Jewell S, Leonard SB, Ritenbaugh C, Newcomb P, Mares-Perlman J, Chavez N, et al. A brief, telephone-administered food frequency questionnaire can be useful for surveillance of dietary fat intakes. J Nutr. 1995 Jun;125(6):1473–1483. doi: 10.1093/jn/125.6.1473. [DOI] [PubMed] [Google Scholar]
- 27.Adair LS, Prentice AM. A critical evaluation of the fetal origins hypothesis and its implications for developing countries. J Nutr. 2004 Jan;134(1):191–193. doi: 10.1093/jn/134.1.191. [DOI] [PubMed] [Google Scholar]
- 28.Beck CT. Acculturation: implications for perinatal research. MCN Am J Matern Child Nurs. 2006 Mar–Apr;31(2):114–120. doi: 10.1097/00005721-200603000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Hawaii Department of Health. [Accessed 3/25/09];Number and percent overweight (including obese) by county, gender, age, and ethnicity - adult population of Hawaii. http://hawaii.gov/health/statistics/hhs/hhs_04/hhs04t31.pdf.
- 30.Durham BN. Hawaii Immigration Timeline. [Accessed 3/26/08];Hawaii School Reports. http://www.hawaiischoolreports.com/culture/immigration.htm.
- 31.Popkin BM, Udry JR. Adolescent obesity increases significantly in second and third generation U.S. immigrants: the National Longitudinal Study of Adolescent Health. J Nutr. 1998 Apr;128(4):701–706. doi: 10.1093/jn/128.4.701. [DOI] [PubMed] [Google Scholar]
- 32.Barcenas CH, Wilkinson AV, Strom SS, Cao Y, Saunders KC, Mahabir S, Hernandez-Valero MA, Forman MR, Spitz MR, Bondy ML. Birthplace, years of residence in the United States, and obesity among Mexican-American adults. Obesity (Silver Spring) 2007 Apr;15(4):1043–1052. doi: 10.1038/oby.2007.537. [DOI] [PubMed] [Google Scholar]
- 33.Razak F, Anand SS, Shannon H, Vuksan V, Davis B, Jacobs R, Teo KK, McQueen M, Yusuf S. Defining obesity cut points in a multiethnic population. Circulation. 2007 Apr 24;115(16):2111–2118. doi: 10.1161/CIRCULATIONAHA.106.635011. [DOI] [PubMed] [Google Scholar]