Abstract
AIMS
The primary aim of this paper is to provide comprehensive contemporaneous data on the demographics, patterns of presentation and management of all episodes of deliberate self-poisoning presenting to a large regional teaching hospital over a 12 month period.
METHODS
We undertook detailed, retrospective analyses using information from electronic patient records and local patient-tracking, pathology and administrative databases. Statistical analyses were performed using Chi-squared tests, anova and two-tailed t-tests (Graphpad Prism).
RESULTS
One thousand five hundred and ninety-eight episodes of deliberate self-poisoning presented over the year. Demographic data and information on the month, day and time of admission are provided. 70.7% presented to the emergency department (ED) within 4 h of ingestion. 76.3% of patients had only one episode in an extended 29 month follow-up period. A mean of 1.72 drugs were taken per episode with just over half of all episodes involving a single drug only. Paracetamol and ibuprofen were the two most commonly ingested drugs involved in 42.5% and 17.3% of all overdoses respectively. 56.3% of patients taking paracetamol reported ingesting over 8 g (one over the counter packet). Detailed mapping of the patients' pathway through the hospital allowed an estimation of the hospital cost of caring for this patient group at £1.6 million pounds per year.
CONCLUSIONS
We present comprehensive and contemporary data on presentations to hospital resulting from deliberate self-poisoning. We include demographic information, presentation patterns, drugs used, a detailed analysis of episodes involving paracetamol and an estimate of the financial burden to hospitals of overdose presentations.
Keywords: epidemiology, overdose, paracetamol, self-poisoning
WHAT IS ALREADY KNOWN ABOUT THIS SUBJECT
Deliberate self-poisoning accounts for 170 000 presentations to UK hospitals each year with a profound impact on the health of individual patients. We have basic demographic information on self-poisoning but there is a relative paucity of contemporary, detailed information on the patterns of presentation, drugs taken in overdose and the current impact on services.
WHAT THIS STUDY ADDS
This study provides detailed analyses of demographics, timing of presentation, patterns of overdose, drugs taken with special emphasis on paracetamol, the patient pathway through hospital and an estimation of the financial impact to the hospital of this patient group. This information is essential in planning the necessary service developments in emergency departments and medical admissions units that are required to optimize management of this patient group.
Introduction
In the year 2000 there were 4740 suicides in England making it the third most important cause of ‘life years lost’ after ischaemic heart disease and cancer [1, 2].
One thousand one hundred and eighty of the 4740 suicides (24.9%) were attributable to ‘deliberate self harm’ (DSH) [1]. Self-poisoning accounts for 85–94% of cases of DSH and a higher proportion of fatal events; it is therefore a major contributor to deaths from suicide [3, 4].
It is estimated that 170 000 people each year present to hospitals in the UK with self-poisoning [5]. Although mortality in this group is relatively low (0.7%), these patients had more than twice the risk of dying than matched controls in a 23 year follow-up study due to a 17-fold increased suicide risk and a variety of other causes [6]. Contact with the health services at the point of self-poisoning, therefore, not only requires early and appropriate treatment of the overdose, but also represents an opportunity to intervene and reduce the risk of subsequent morbidity and mortality. This must be one of the approaches to achieving the Department of Health (DoH) target of reducing deaths from suicide by 20% by 2010 [7].
In addition to the human cost, there is a substantial financial burden on the health services due to self-poisoning that is spread between emergency departments, acute medical units, critical care facilities, psychiatry and psychology services, social services and primary care.
In order for strategies to be put in place to try to reduce deaths and the substantial costs to health care services, it is vital that we develop our understanding of the patterns of presentation of self poisoning and organize our services appropriately [5]. Furthermore, because suicide is fortunately a relatively rare outcome of DSH, there have been suggestions that national suicide prevention strategies be based on up to date research on non-fatal self harm with high quality follow-up [8].
The primary aim of this paper was to provide comprehensive, detailed and current data on the demographics, patterns of presentation and management of all episodes of self-poisoning presenting to one of the busiest EDs in the country. In particular we aimed to examine the changes to the patterns of drugs used in overdose, and to provide detailed information on overdoses involving the most commonly ingested drug, paracetamol.
Methods
This study involved a retrospective analysis of all episodes coded as overdose presenting to the Queens Medical Centre (QMC), Nottingham between 1 April 2006 and 31 March 2007. Two thousand six hundred and sixty-five episodes were identified from a computerized admissions database known as the Emergency Department Information System (EDIS) using Crystal II database interrogation software. After removal of patients under 16 years of age, those who had been miscoded patients where the self-poisoning was accidental and duplicate entries registered both from ED and the Acute Medical Unit (AMU), 1598 episodes remained.
For each episode basic details including patients' unique identification number, gender, date of birth, date and time of arrival and onward movement from ED or AMU and destination (home or transfer location) were pulled from the database. Using the electronic clinical records from ED further information including patient reported information on the number and quantity of drugs taken, the time of the self poisoning, and whether the patient had a psychiatric history were recorded. Where details could not be found in the electronic records, case notes were requested in order to retrieve the same information. For all those patients who admitted to having self-poisoned with paracetamol, a hospital-based electronic results service (NoTIS) was searched using the unique identifiers to find the serum paracetamol concentration and the timing of the sample. Where discharge was not from ED or AMU, discharge dates were pulled from the hospital's administrative database.
All data were transferred into Excel for further analysis and calculation of additional parameters including the length of stay in the ED, time between the self poisoning episode and ED presentation, time between the self poisoning episode and paracetamol concentrations being taken and the number of drugs ingested per patient.
In order to get a more accurate representation of multiple presentations with deliberate self-poisoning, EDIS records going back to the introduction of the system (17 months prior to the start of the study period) were searched and any previous episodes involving deliberate self-poisoning by the 1598 patients who had presented in the index year were recorded. Repeated presentations within the index year and during the extended search period were analyzed separately. Statistical analyses were performed where necessary with Chi-squared tests, anova and two-tailed t-tests (Graphpad Prism). The in-patient costs of overdose presentations to the hospital were estimated using current standard tariffs.
Ethical approval
This study was classed as a detailed service evaluation and so, in keeping with national guidelines, ethics approval was not required.
Results
One thousand five hundred and ninety-eight episodes of overdose were identified during the year. Twenty-four (1.5%) of these patients were sent directly to Acute Medicine by their General Practitioner (GP); the rest presented to ED making up 1.14% of all ED episodes (Figure 1). Of this total 652 were discharged directly from ED and 946 were admitted, representing 4.7% of all of the medical admissions at QMC. This compares with chest pain/ acute coronary syndrome (13% of admissions) and gastrointestinal bleeding (2.7%).
Figure 1.
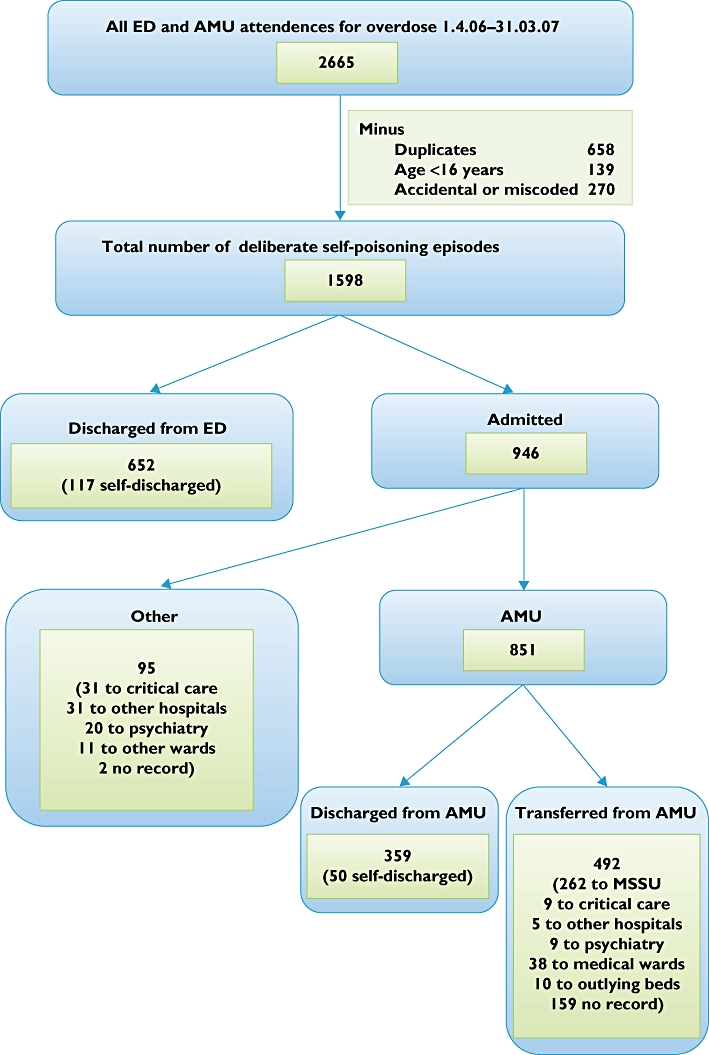
Flow diagram to illustrate how data were collected for the study. ‘Duplicates’ were episodes that had been coded both in the emergency department (ED) and the acute medical unit (AMU) on the patient tracking system. Accidental overdoses and those miscoded as overdose were filtered out by a review of the medical records. A detailed breakdown of the admissions is included. (‘MSSU’ is the medical short stay unit: this is a general medical ward intended to care for patients with an anticipated length of stay of less than 48 h.)
Figure 2 shows the gender distribution of the patients by age group (no date of birth was available for seven patients). 59.2% (n = 946) of episodes were female giving a female : male ratio of 1.45 : 1. Ages ranged from 16–90 years with a median age of 32 years. The patients were not evenly distributed between the age groups but skewed towards the younger ages. 46.8% (n = 745) of cases involved patients 30 years of age or below and 3.3% (n = 52) involved patients aged over 60 years.
Figure 2.
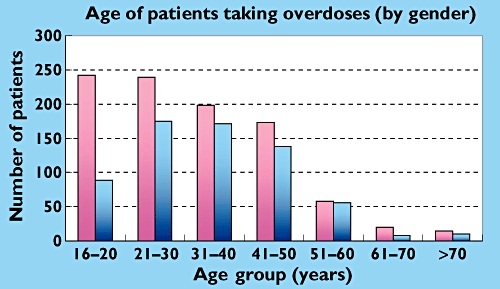
The age distribution by gender for all episodes of self-poisoning. Female ( ); Male (
); Male ( )
)
The distribution of patients between age groups differed according to gender. The female : male gender ratio was highest in the younger age groups. In the 16–20 year age group the ratio was 2.72 : 1, compared with 1.26 : 1 in the rest (P < 0.0001). In 57.6% of patients there was documentation in the ED notes of a previous psychiatric history including depression. There was no significant gender difference for risk of psychiatric history (57.4% of men vs 57.7 % of women). The likelihood of having a psychiatric history was much lower in the 16–20 year age group than in the remaining patients (40.2% vs 62.2%; P < 0.0001).
Patterns of overdose presentation were analyzed by month, by day of the week and by hours of the day. On average 4.38 overdose episodes presented to QMC each day and there were no significant monthly differences [range: 3.52 (December) – 5.14 (February)]. Equally there were no significant differences in the number of episodes per day when analyzed by day of the week [range: 4.10 (Thursday) – 4.62 (Saturday)].
By contrast there were marked differences when admissions were analyzed by hour of the day. This is shown in Figure 3 alongside a plot of the total numbers of ED attendances to show that patients who have taken overdoses tend to present later in the day than those attending for other reasons.
Figure 3.
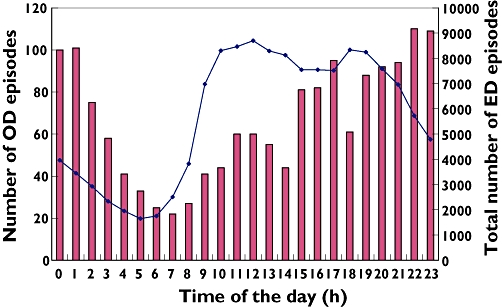
The timing of all overdose presentations during the year of the study (bars plotted against the left-hand y axis) compared with all ED presentations in the year (line plotted against the right-hand y axis) over the 24 h period. OD episodes ( ); All ED episodes (
); All ED episodes ( )
)
The time between deliberate self poisoning and ED presentation is shown in Figure 4. Data were unavailable for 18.7% of the episodes. In those patients where timing of overdose was known, 70.7% presented to ED within 4 h of taking the self-poisoning while just 9.9% presented after 12 h. There were no statistical differences between genders or age groups for these variables.
Figure 4.
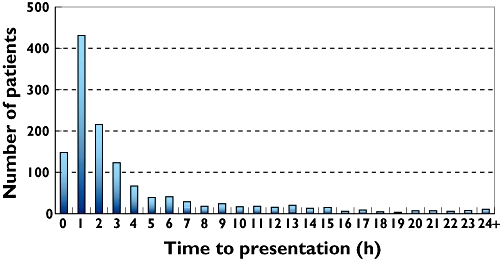
The distribution of time from reported ingestion to presentation by plotting the number of patients presenting in each hour block
76.3% of patients presenting after overdose had only one episode in a 29 month follow-up period (87.7% in the 12 month study period). Conversely 48.5% of all episodes of overdose in the 29 months were accounted for by patients who presented on more than one occasion. This skew is due to the large number of presentations by certain individuals; the most in this study was 41.
Information from the patient on the number of drugs taken in overdose was available in 1571 out of 1598 (98.3%) of episodes. A total of 2703 drugs were taken in these episodes (1.72 per episode) with just over half of all episodes involving a single drug only (Figure 5). Results did not differ significantly when analyzed by gender, age group or in patients admitted vs those discharged directly from ED.
Figure 5.
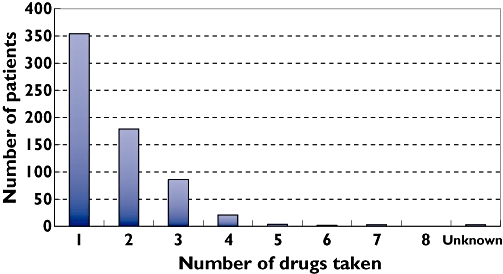
The distribution of the number of drugs taken in overdose. A total of 2703 drugs were taken by 1571 patients; data were not available in 27 episodes of self-poisoning
A detailed analysis of the drug taken in overdose when grouped by British National Formulary (BNF) classification, demonstrated that non-opioid analgesics were by far the most common accounting for 902/2703 (33.4%) of the drugs taken. They were followed by antidepressants (15.8%), non-steroidal anti-inflammatory drugs (NSAIDS) (13.3%), hypnotics and anxiolytics (8.7%), opiates (6.0%), and drugs used in psychoses and related disorders (3.7%). All other drug classes accounted for less than 2.5% of the total. The ‘top ten’ individual drugs taken in overdose are listed in Table 1.
Table 1.
The top ten drugs used in overdose giving absolute number of overdoses in which the drug was used, the percentage of overdoses involving the drug and the percentage of all of the drugs used in overdose. Differences between the last two values reflect the fact that single overdoses can involve multiple drugs and the more commonly used agents are more likely to be used as part of a multi-drug overdose
| Position | Drug | Number of times used in overdose | % of overdoses involving drug | % of all drugs used in overdoses |
|---|---|---|---|---|
| 1 | Paracetamol | 679 | 42.5 | 25.1 |
| 2 | Ibuprofen | 277 | 17.3 | 10.2 |
| 3 | Citalopram | 107 | 6.7 | 4.0 |
| 4 | Zopiclone | 92 | 5.8 | 3.4 |
| 5 | Fluoxetine | 84 | 5.3 | 3.1 |
| 6 | Co-codamol* | 81 | 5.1 | 3.0 |
| 7 | Aspirin | 79 | 4.9 | 2.9 |
| 8 | Diazepam | 78 | 4.9 | 2.9 |
| 9 | Codeine | 61 | 3.8 | 2.3 |
| 10 | Diclofenac | 60 | 3.8 | 2.2 |
Co-codamol is a compound analgesic agent containing paracetamol (500 mg per tablet) and codeine phosphate (8, 15 or 30 mg per tablet).
Analysis of differences in the number of self-poisoning episodes involving the more common drugs/categories by gender showed that NSAIDS and selective serotonin re-uptake inhibitors (SSRIs) were more commonly taken by women (Odds Ratios (OR) 1.38 (P= 0.019) and 1.36 (P= 0.025) respectively. No significant differences were found for paracetamol (OR 1.03), TCAs (OR 1.14), zopiclone (OR 0.97) and aspirin (OR 1.49).
Seven hundred and two of the 770 (91.2%) episodes of self-poisoning involving paracetamol or paracetamol-containing compound analgesics gave a history detailing the number of tablets ingested and had this information documented in ED. From those episodes where this information was available 43.7% took less than one ‘over the counter’ packet (16 × 500 mg tablets) and 77.2% took less than one pharmacy packet (32 × 500 mg tablets). Figure 6 demonstrates the distribution of the number of grams of paracetamol taken by patients who were admitted after ingestion of paracetamol compared with those discharged directly from ED. The median and mean in the admitted group were 12.5 g and 16.19 g; in the discharged group equivalent figures were significantly lower at 8 g and 9.52 g respectively (P < 0.05). Comparison of number of grams ingested and paracetamol concentrations showed a number of patients above the treatment line despite reported ingestion of less than 8 g paracetamol.
Figure 6.
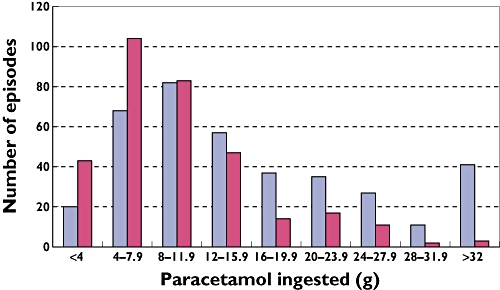
The amount of paracetamol ingested by patients who took paracetamol either alone or in combinations available over the counter. Data were available for 702/795 patients. Admitted patients ( ); Discharged from Ed (
); Discharged from Ed ( )
)
Figure 7a shows a scatterplot of serum paracetamol concentration against time from ingestion for patients discharged directly from ED. The plots are superimposed on the BNF treatment lines for normal and high risk patients which are used in the United Kingdom (UK) as a guide as to which patients require treatment with intravenous acetylcysteine to minimize the risk of liver damage. Figure 7b is the equivalent plot for admitted patients. The points have been grouped into ranges of number of grams of paracetamol ingested. Table 2 summarizes the results.
Figure 7.
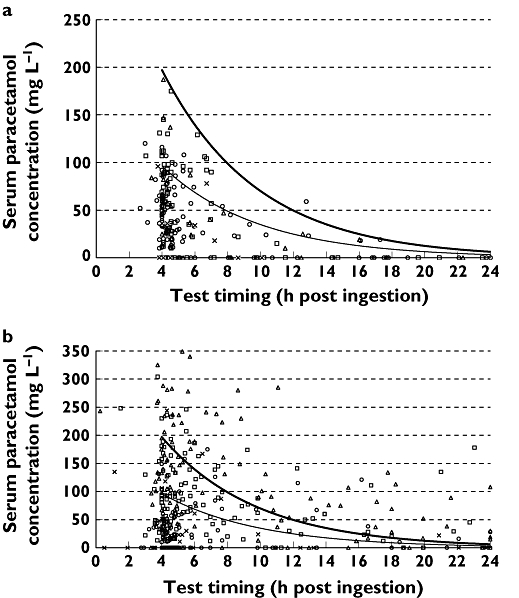
Plots of serum paracetamol concentrations against timing of the test superimposed onto the standard and high risk treatment nomograms as found in the British National Formulary. 7a represents patients discharged from the Emergency Department, and 7b those requiring medical admission. Where information on amount ingested was reported, this has been incorporated by the use of different point markers for those who ingested <8 g, 8–16 g and over 16 g paracetamol. Episodes where the ingested amount was not reported by the patient have been marked with a cross. Those patients for whom the timing of the overdose was unclear have not been included. Reported ingestion up to 8 g Paracetamol (○); Reported ingestion 8–16 g Paracetamol (□); Reported ingestion >16 g Paracetamol (▵); Unknown quantity of paracetamol taken (×)
Table 2.
A summary of the results in Figure 7a,b
| Patients discharged from ED (n= 244) (%) | Admitted patients (n= 365) (%) | |
|---|---|---|
| Below high risk treatment line | 204 (84.0) | 184 (50.4) |
| Between normal and high risk treatment lines | 39 (16.0) | 80 (21.9) |
| Above normal treatment line | 1 (0.004) | 101 (27.7) |
Serum paracetamol concentrations taken earlier than 4 h post-ingestion can be misleading and so blood samples ought to be taken after this time. Using a 30 min leeway for inaccuracy of documentation, 20 patients had their paracetamol concentrations measured before this time.
The movement of patients attending ED/AMU after an episode of self-poisoning is demonstrated in Figure 1. Nine hundred and forty-six (59.2%) of all episodes led to admission with the vast majority (n = 851, 90%) going through the AMU. Of the 652/1598 (40.8%) sent home directly from ED, 82.1% of these had a planned discharge and 17.9% self-discharged or refused treatment.
For those patients discharged directly from ED the mean length of stay was 3 h and 17 min, the median 3 h and 34 min. 93.8% were discharged within 4 h. Length of stay data were available for 89.5% of admitted patients but, due to limitations of the hospital's database could only be measured in days. 77.7% of those episodes where length of stay information was available required admission for less than 1 day.
We estimated the in-patient costs associated with overdoses. Assuming the tariff cost for presentation to the ED of £73 per episode this would equate to £114 902 for the study population of 1574 who presented to the ED. The 24 patients admitted to the medical assessment bay directly by their GPs cost £220 per assessment, £5280 in total. For those patients admitted for treatment or observation the average tariff-based charge to the primary care trusts was £1800 making a total of £1 468 800 for the 816 who did not go to critical care. The 40 patients admitted to critical care cost in excess of £50 000. Ninety-nine patients had no length of stay data and for the purposes of this estimation were assumed only to have cost the ED tariff; this almost certainly underestimates the charges for their admissions. The overall estimated cost of the care of patients presenting with deliberate self-poisoning to the QMC is therefore over £1.6 million per year.
Discussion
This study provides a contemporary, comprehensive and detailed analysis of presentations to hospital after self-poisoning. Its strengths lie in the robust electronic search facilities allowing capture of all presentations and the ability to search electronic patient records containing essential clinical information and clinical chemistry data. Coding options for deliberate self-poisoning were limited and the diagnosis at presentation was usually clear so the search criteria captured the vast majority of overdoses. By reading electronic clinical notes we could accurately exclude patients miscoded as deliberate self-poisoning. This ensured completeness of the data presented and allowed a large study involving over 1500 presentations to be performed quickly so that the information presented remains relevant to current practice. This is essential in a field where changes in prescribing habits and trends alter the pattern of overdose presentation over time [4, 9–11]. Length of stay data were available directly from EDIS for all ED discharges and those patients whose stay was confined to the Acute Medical areas which used EDIS. For patients admitted to other wards there were some patients for whom an accurate length of stay could not be found due to the limitations of cross-referencing with parts of the Trust's administrative database. The major weakness in the study is the inherent potential for inaccuracy in patient reporting of timing, dose and type of drug used in overdose.
Previous literature relating to the epidemiology of self poisoning is both sparse given its profound impact on life years lost and health service resources, and difficult to interpret for a variety of reasons including confusion over the terminology (self-harm and self-poisoning), coding variations, incomplete patient information and presentation of data by episode or person given the relatively high level of re-attendance [12, 13]. With these provisos we have examined our data in the context of the existing literature.
Rates of self-poisoning are known to vary with age. In keeping with data from this study the average age of presentation with DSH and/or self-poisoning is around 31–34 years [4, 5, 12, 14, 15]. Although elderly patients into their nineties [14] have been reported taking overdoses, the proportion of elderly as a percentage of the total is small. Hawton et al. quote 3.9% of patients with DSH being aged >60 years compared with 3.3% in this study [6]. The increased incidence of self-poisoning in women in younger age groups (between 15 and 24 years old) demonstrated in Figure 2 is reflected in other studies [10, 16]. The overall female : male ratio of 1.45 : 1 we report is somewhat higher than the 1.2 : 1 ratio described in other recent studies [4, 14, 15]. Our results confirm that patients in the youngest age group (16–19 year olds) who presented after self-poisoning were significantly less likely to have a recorded psychiatric history. Full assessment of the psychiatric evaluations of this patient group might provide useful insight into potential preventative strategies.
There appears to be little variation in the day of the week or month of the year that self-poisoning patients present to hospital. However, there is a clear pattern to the time of presentation [3, 15]. In this study 70.8% of self-poisoning episodes presented outside working hours of 09.00 h to 17.00 h compared with 73–80% in published literature [3, 15]. This has clear implications for designing safe and efficient care pathways for these patients.
There are few data published on the delay from overdose to presentation. Inevitably patient reporting may be inaccurate but there is usually no other way of collecting this information. We present reported data from 81.3% of episodes of self-poisoning and demonstrate that over 70% of them present within 4 h implying either that the deliberate self-poisoning was a ‘cry for help’ with no true suicidal intent, or that the patients quickly regretted their decision to self-poison.
Re-admissions with episodes of DSH are frequent. They are important not only because of their resource implications but also because they are a marker of increased risk of suicide. In their review article, Owens et al. quoted a median repetition rate of 16% in 1 year, with studies lasting longer than 4 years showing a median 23% [8]. Rafnsson et al. studied all admissions and re-admissions to the Royal Infirmary of Edinburgh between 1981 and 2001 finding that 73% of all admissions were isolated episodes, 24% were for 2–5 admissions and 3% were people admitted six or more times [9]. Our data are comparable with these results with 76.3% of patients presenting with self-poisoning over a 29 month follow-up period having an isolated episode and the remaining 23.7% of patients accounting for 48.5% of all episodes.
A mean of 1.7 drugs were taken in each episode, higher than the 1.2 per episode suggested by Townsend et al.[17]. 46% of episodes involved more than one drug compared with 39–63% quoted by other studies [9, 17]. These data were based on the history taken from patients at the time of admission and therefore subject to inevitable potential inaccuracies of reporting.
Paracetamol, taken as a single compound was the most commonly ingested drug as found in other studies. Self-poisoning episodes involving paracetamol are often highly impulsive due to its ready availability [18]. Its harmful effects are due mostly to the damage it inflicts on the liver. This has been shown to be more likely to occur in individuals who take >25 tablets [19]. Legislation was introduced in 1998 to reduce the availability of paracetamol by restricting sales to 32 tablets (500 mg) from a pharmacy and 16 tablets from other retailers, to increase knowledge of its dangers in self-poisoning by compulsory health warnings in packets, and to decrease the speed with which multiple tablets may be ingested by mandatory use of blister packs [20, 21]. Before the introduction of the legislation its use had risen from an involvement in 31.3% of self-poisoning episodes in 1985 to 49.6% in 1995 [22].
The efficacy of the 1998 legislation is not yet clear as the majority of studies looking at its effects are based on short-term follow up in specific areas of the UK [23]. There is agreement that the severity of paracetamol self-poisoning has reduced but the initial reduction in its frequency may not have been maintained [20, 24–28]. In this study paracetamol was taken in 42.5% of episodes of deliberate self-poisoning (48.2% if paracetamol-containing compounds are included) comprising 25.1% (29.4% including compounds) of all drugs taken. This approaches published pre-legislation levels. In addition, based on the patient-reported information available, in 702 out of 795 episodes including paracetamol or paracetamol-containing products available over the counter, 56.3% took more than one non-pharmacy pack (8 g) and 22.8% more than one pharmacy pack (16 g). The validity of the information on the number of tablets ingested and the timing of ingestion as reported by patients or witnesses is questionable in some cases: 39 out of 388 patients (10.1%) who claimed to have taken 8 g of paracetamol or more and had blood samples taken between 6 and 18 h after ingestion had concentrations of less than 10 mg l−1. There is, however, no better way of gathering such information so it should be used but interpreted with caution.
Data from the scatter plots (Figure 7a,b) raise two areas of concern. Firstly a small but potentially significant minority whose serum paracetamol concentrations were measured too early to provide meaningful results [29] and secondly the large cohort who fall between normal and high risk nomograms where documentation of risk is not always clear. It is reassuring that, barring one patient who self-discharged, all patients above the normal risk treatment line were admitted. Of note 56% of admitted patients did not require treatment according to their concentrations, the majority were admitted pending paracetamol concentrations or awaiting psychological assessment to avoid breaching the UK's target of no ED waits to exceed 4 h. Further studies with details of whether these assessments were delayed by inadequate staffing or because intoxication or emotional upset precluded adequate early assessment of risk, and with focus on the financial implications of admission are needed.
In our study the class of drugs taken second most frequently were antidepressants. SSRIs comprised 67.6% of this total. The shift from tricyclic antidepressants which formed the majority of antidepressants taken in older studies [4, 22] reflects altered prescribing. NSAIDs (13.3% of all drugs taken) were the next most common group with ibuprofen being the second most common individual drug taken in overdose (10.2% of all drugs taken and involved in 17.3% of all overdose presentations). These data are at variance with previous studies which found benzodiazepines and antidepressants to be the second and third most commonly taken groups of drugs with NSAIDs being taken in only 7% of episodes [3, 9]. In our study, NSAIDs and SSRIs were significantly more commonly taken by women. The former is a novel observation, the latter in keeping with published data [3, 17].
Interestingly, while we confirm the predominance of benzodiazepines amongst hypnotics used in overdose (136/236), the most common individual drug in this class was zopiclone (n= 92; involved in 5.8% of all overdoses). This is a novel finding and almost certainly reflects recent changes in prescribing habits.
The ‘miscellaneous’ class of drugs made up 11.3% of drugs ingested. Although individual drugs within the class were used infrequently, collectively they accounted for a significant number of presentations to hospital, highlighting the importance of authoritative information and guidance from the National Poisons Information Service (NPIS) commissioned by the Health Protection Agency (HPA) in management of self-poisoning.
There is considerable variation in hospital management of self-poisoning episodes depending on the local policies and pathways with rates of admission ranging from 39 to 87% [3–5, 22]. The admission rate of 59.2% in this study reflects the fact that overdoses are not looked after on the ED observation ward and so all but those who can be safely discharged within the 4 h target are formally admitted.
The estimated cost of overdose presentations to the hospital is not a complete financial analysis. We provide an estimate of the costs of overdose presentations to the hospital: this was over £1.6 million per year. This figure markedly underestimates the true financial burden of overdoses, as we have not included out of hospital medical costs or the economic burden of lost time at work. The latest data estimates 170 000 overdose presentations to UK hospitals per year. This would equate 1.12% of all ED presentations according to the DoH hospital activity statistics for the year studied. This figure tallies closely with the 1.14% found at our hospital over the study period. Assuming similar costs apply across other hospitals, therefore, the annual hospital cost of overdose in the UK is likely to be around £170 million.
In summary this study provides comprehensive, contemporary data on the patterns of presentation of self-poisoning and the impact of these presentations on hospital services. We give a detailed analysis of paracetamol use in overdose highlighting some of the potential pitfalls in the management of this important patient group.
Competing interests
None declared.
REFERENCES
- 1.Department of Health. London: Department of Health Publications; National suicide prevention strategy for England. [Google Scholar]
- 2.Gunnell D, Frankel S. Prevention of suicide: aspirations and evidence. BMJ. 1994;308:1227–33. doi: 10.1136/bmj.308.6938.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawton K, Bergen H, Casey D, Simkin S, Palmer B, Cooper J, Kapur N, Horrocks J, House A, Lilley R, Noble R, Owens D. Self-harm in England: a tale of three cities. Multicentre study of self-harm. Soc Psychiatry Psychiatr Epidemiol. 2007;42:513–21. doi: 10.1007/s00127-007-0199-7. [DOI] [PubMed] [Google Scholar]
- 4.Wilkinson S, Taylor G, Templeton L, Mistral W, Salter E, Bennett P. Admissions to hospital for deliberate self-harm in England 1995–2000: an analysis of hospital episode statistics. J Public Health Med. 2002;24:179–83. doi: 10.1093/pubmed/24.3.179. [DOI] [PubMed] [Google Scholar]
- 5.Kapur N, House A, Creed F, Feldman E, Friedman T, Guthrie E. Management of deliberate self-poisoning in adults in four teaching hospitals: descriptive study. BMJ. 1998;316:831–2. doi: 10.1136/bmj.316.7134.831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hawton K, Harriss L, Zahl D. Deaths from all causes in a long-term follow-up study of 11,583 deliberate self-harm patients. Psychol Med. 2006;36:397–405. doi: 10.1017/S0033291705006914. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health. London: Department of Health Publications; Saving Lives: Our Healthier Nation. [Google Scholar]
- 8.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. Br J Psychiatry. 2002;181:193–9. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 9.Rafnsson SB, Oliver JJ, Elton RA, Bateman DN. Poisons admissions in Edinburgh 1981–2001: agent trends and predictors of hospital readmissions. Hum Exp Toxicol. 2007;26:49–57. doi: 10.1177/0960327107071855. [DOI] [PubMed] [Google Scholar]
- 10.Bialas MC, Reid PG, Beck P, Lazarus JH, Smith PM, Scorer RC, Routledge PA. Changing patterns of self-poisoning in a UK health district. QJM. 1996;89:893–901. doi: 10.1093/qjmed/89.12.893. [DOI] [PubMed] [Google Scholar]
- 11.McEvedy CJ. Trends in self-poisoning: admissions to a central London hospital, 1991–1994. J R Soc Med. 1997;90:496–8. doi: 10.1177/014107689709000908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Camidge DR, Wood RJ, Bateman DN. The epidemiology of self-poisoning in the UK. Br J Clin Pharmacol. 2003;56:613–9. doi: 10.1046/j.1365-2125.2003.01910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawton K, Bale L, Casey D, Shepherd A, Simkin S, Harriss L. Monitoring deliberate self-harm presentations to general hospitals. Crisis. 2006;27:157–63. doi: 10.1027/0227-5910.27.4.157. [DOI] [PubMed] [Google Scholar]
- 14.Leslie S. A survey of admissions following self-poisoning. Psychiatric Bulletin. 2005;29:305–8. [Google Scholar]
- 15.Gunnell D, Bennewith O, Peters TJ, House A, Hawton K. The epidemiology and management of self-harm amongst adults in England. J Public Health (Oxf) 2005;27:67–73. doi: 10.1093/pubmed/fdh192. [DOI] [PubMed] [Google Scholar]
- 16.Bateman DN, Bain M, Gorman D, Murphy D. Changes in paracetamol, antidepressants and opioid poisoning in Scotland during the 1990s. QJM. 2003;96:125–32. doi: 10.1093/qjmed/hcg015. [DOI] [PubMed] [Google Scholar]
- 17.Townsend E, Hawton K, Harriss L, Bale E, Bond A. Substances used in deliberate self-poisoning 1985–1997: trends and associations with age, gender, repetition and suicide intent. Soc Psychiatry Psychiatr Epidemiol. 2001;36:228–34. doi: 10.1007/s001270170053. [DOI] [PubMed] [Google Scholar]
- 18.Hawton K, Ware C, Mistry H, Hewitt J, Kingsbury S, Roberts D, Weitzel H. Paracetamol self-poisoning. Characteristics, prevention and harm reduction. Br J Psychiatry. 1996;168:43–8. doi: 10.1192/bjp.168.1.43. [DOI] [PubMed] [Google Scholar]
- 19.Hawton K, Ware C, Mistry H, Hewitt J, Kingsbury S, Roberts D, Weitzel H. Why patients choose paracetamol for self-poisoning and their knowledge of its dangers. BMJ. 1995;310:164. doi: 10.1136/bmj.310.6973.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turvill JL, Burroughs AK, Moore KP. Change in occurrence of paracetamol overdose in UK after introduction of blister packs. Lancet. 2000;355:2048–9. [PubMed] [Google Scholar]
- 21.Committee on Safety of Medicines; Medicines Control Agency. Paracetamol and aspirin. Current Problems in Pharmacovigilance. 1997;23:9. [Google Scholar]
- 22.Hawton K, Fagg J, Simkin S, Bale E, Bond A. Trends in deliberate self-harm in Oxford, 1985–1995. Implications for clinical services and the prevention of suicide. Br J Psychiatry. 1997;171:556–60. doi: 10.1192/bjp.171.6.556. [DOI] [PubMed] [Google Scholar]
- 23.Hawkins LC, Edwards JN, Dargan PI. Impact of restricting paracetamol pack sizes on paracetamol poisoning in the United Kingdom: a review of the literature. Drug Saf. 2007;30:465–79. doi: 10.2165/00002018-200730060-00002. [DOI] [PubMed] [Google Scholar]
- 24.Prince MI, Thomas SH, James OF, Hudson M. Reduction in incidence of severe paracetamol poisoning. Lancet. 2000;355:2047–8. doi: 10.1016/S0140-6736(00)02354-0. [DOI] [PubMed] [Google Scholar]
- 25.Gorman DR, Bain M, Inglis JH, Murphy D, Bateman DN. How has legislation restricting paracetamol pack size affected patterns of deprivation related inequalities in self-harm in Scotland? Public Health. 2007;121:45–50. doi: 10.1016/j.puhe.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 26.Hawton K, Townsend E, Deeks J, Appleby L, Gunnell D, Bennewith O, Cooper J. Effects of legislation restricting pack sizes of paracetamol and salicylate on self-poisoning in the United Kingdom: before and after study. BMJ. 2001;322:1203–7. doi: 10.1136/bmj.322.7296.1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawton K, Simkin S, Deeks J, Cooper J, Johnston A, Waters K, Arundel M, Bernal W, Gunson B, Hudson M, Suri D, Simpson K. UK legislation on analgesic packs: before and after study of long term effect on poisonings. BMJ. 2004;329:1076. doi: 10.1136/bmj.38253.572581.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bateman DN, Gorman DR, Bain M, Inglis JH, House FR, Murphy D. Legislation restricting paracetamol sales and patterns of self-harm and death from paracetamol-containing preparations in Scotland. Br J Clin Pharmacol. 2006;62:573–81. doi: 10.1111/j.1365-2125.2006.02668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.British National Formulary. London: BMJ Publishing Group; 2008. [Google Scholar]


