Abstract
Study Design
Prospective Cohort.
Introduction
Patient satisfaction is increasingly used as a metric of health care outcomes. The relationship between patient satisfaction and functional outcomes metrics is understudied.
Purpose
To determine the minimum recovery needed in grip strength, key pinch strength, and arc of motion needed for patient satisfaction after treatment of distal radius fracture (DRF) with volar locking plating system placement.
Methods
A prospective cohort of 125 DRF patients was evaluated 3 months after surgery for grip strength, key pinch strength, wrist arc of motion, and satisfaction with hand strength and wrist arc of motion. Receiver operating characteristic (ROC) curves were constructed using patient satisfaction items as the “gold standard” and each functional measure of outcome as a predictor.
Results
We found that the optimal cut-points to distinguish satisfaction from dissatisfaction occurred when patients had recovered 65% of their grip strength, 87% of their key grip strength, and 95% of the wrist arc of motion, as measured as percents of their uninjured wrists.
Conclusions
A much greater wrist range of motion must be recovered for patients to be satisfied than what is needed to perform activities of daily living.
Level of Evidence
Diagnosis Level 2.
Keywords: Distal Radius Fracture, Grip Strength, Wrist Motion, Michigan Hand Outcomes Questionnaire, ROC Curve, Volar Locking Plate System
Introduction
Grip strength, key pinch strength, and wrist motion are standard measures of outcome after treatment for hand surgery conditions and injuries (1, 2). These outcome measures have been shown to have high reliability and validity (3–6). Additionally, they are known to be important predictors of outcome after distal radius fracture (DRF) (7). Hand surgeons and therapists strive to restore these functional outcomes measures to preinjury or premorbid state and restoration of these physical measures may reflect the optimal quality of care. However, it is uncertain whether the increased cost necessary to restore full hand strength and wrist motion is necessary to achieve sufficient patient satisfaction. The patient-centric philosophy in the outcomes movement relies on patients’ perception of outcomes such as patient satisfaction. In recent years, there is increasing recognition of the importance of using patient satisfaction as a metric of quality of patient care in deference to the traditional, physical outcomes measurements. The patient’s evaluation of outcomes is valuable because it reflects how a procedure impacts the patient’s life in ways that are meaningful to the patient (8–11). In recognition of this, payors are beginning to gather and use data on patient satisfaction as part of their evaluation of health care quality (11–13). However, the relationship between patient satisfaction and functional measures of hand outcome has never been established. It is uncertain how much hand strength and wrist motion must be regained after surgery for the majority of patients to be satisfied with their outcome. Hand therapy is costly, and if achieving a certain amount of improvement is satisfactory to the majority of patients, then precious national resources can be saved for other important areas. For a prevalent injury such as DRF, it is important to understand what level of recovery in strength and wrist motion will be considered as satisfactory to patients. The methodology employed in this study can be used in a similar manner to estimate the level of functional measures of outcome needed to achieve sufficient patient satisfaction after other types of hand surgery.
The specific aim of this paper is to use data from a prospective longitudinal outcomes study in a large cohort of DRF patients who were treated with the volar locking plating system (VLPS). Receiver Operating Characteristic (ROC) curves are constructed by comparing outcomes in the satisfaction domain of the Michigan Hand Outcomes Questionnaire (MHQ) with functional outcomes measures such as grip strength, key pinch strength, and active wrist arc of motion in order to determine the optimal thresholds of the functional outcomes measures to discriminate between satisfied and dissatisfied patients. These thresholds give surgeons and therapists estimates of the progress that must be made for patient satisfaction after DRF treatment.
Methods
Patient Sample
This prospective ongoing longitudinal cohort of study subjects was described previously (14, 15). Briefly, consecutive patients with inadequately reduced DRFs after attempt at closed reduction who subsequently underwent fixation with the VLPS were invited to participate in the study. Patients were considered to have an inadequate reduction based on the following radiographic criteria: apex volar angulation of >10°, a radial inclination angle of <15°, a radial height of <10 mm, and/or an intra-articular step-off ≥2 mm. Patients were eligible to participate if they were at least 18 years of age and literate in English. Patients were excluded if they had bilateral fractures, or if they had experienced other upper arm, head, systematic, or multiple-organ injuries. The study protocol was approved by the Institutional Review Board of the medical center. Informed consent was obtained from all participants, and the rights of participants were protected.
Outcomes Measurements
Patients were evaluated at 3 months after surgery using the Michigan Hand Outcomes Questionnaire (MHQ). The 3 month period was selected because the majority of the patients in this series reported overall MHQ scores over 80, which indicates excellent outcomes, and enough data on both satisfied and dissatisfied patients were collected to compare these groups. The MHQ contains specific items to evaluate satisfaction with hand strength and wrist motion; the validity of the MHQ has been established in multiple studies and over 100 publications have used the MHQ for outcomes assessment (16). The MHQ consists of 37 questions that reflect self-assessment in 6 areas: overall hand function, activities of daily living, pain, work performance, aesthetics, and satisfaction with function. Each domain of the MHQ has been found to have high content and construct validity, and high test-retest reliability (17). The satisfaction domain was found to have an intraclass correlation of 0.96, indicating high test-retest reliability (n=22) (17). The Spearman’s Correlation between satisfaction and overall hand function (0.75), ADL (0.73), and work performance (0.63) were high (n=200); this indicates that patients with better hand function tend to be more satisfied with their hand function, and proves evidence for construct validity (17). Furthermore, the satisfaction domain has been shown to be responsive to changes in health status: patients with chronic hand disorders completed the MHQ before surgical treatment and 6 to 18 months after treatment (n=187)(18). At the later time, they were also asked to rate the change in their hand(s) before and after surgery(18). The Spearman’s Correlation between the change in satisfaction score between the two times and the self-rated improvement was 0.39 (p=0.0007)(18). This indicates that the satisfaction domain is sensitive to clinical change(18). Grip strength, key pinch grip, and wrist arc of motion were used as functional measures of hand function. Measurements were made by a certified hand therapist using a Jamar dynamometer (Sammons Preston Rolyan, Bolingbrook, IL), a pinch gauge (B&L Engineering, Tustin, CA), and a goniometer (Richardson Products, Inc., Frankfort, IL), respectively.
Data Analysis
Patient satisfaction was assessed based on two questions in the Satisfaction domain of the MHQ, one of which pertains specifically to wrist motion and the other of which pertains specifically to hand strength. For each question, respondents selected one of: “Very Satisfied”, “Somewhat Satisfied”, “Neither Satisfied Nor Dissatisfied”, “Somewhat Dissatisfied”, or “Very Dissatisfied”. In order to use an ROC curve, a dichotomous “gold standard” in needed. Accordingly, the responses for the injured wrist were dichotomized, with “Very Satisfied” and “Somewhat Satisfied” indicating satisfaction with wrist motion or hand strength, and “Neither Satisfied Nor Dissatisfied”, “Somewhat Dissatisfied”, or “Very Dissatisfied” indicating dissatisfaction with wrist motion or hand strength. Ordinal data are often dichotomized in practice, although some information is lost in the process (19). We opted to dichotomize the ordinal satisfaction data at this point because we wished to focus on the transition from no satisfaction to at least some satisfaction.
Grip strength and key grip strength were each measured three times for both the injured and uninjured hand. The means for each hand were calculated and adjusted using the 10% rule for hand dominance (20). Wrist range of motion was also measured, and arc of motion was calculated as degrees of flexion plus degrees of extension. For each functional measure, the score for the injured hand was divided by the score for the uninjured hand to obtain the percent of normative function. This was used as the functional measure in all analyses.
Receiver Operating Characteristic (ROC) curves were used to characterize the unadjusted relationship between each functional measure of hand function and satisfaction. Satisfaction was considered the “gold standard”, or the true state that we wished to predict using the functional measures. Wrist arc of motion was used to predict satisfaction with wrist motion, and each of the two measures of strength was used separately to predict satisfaction with hand strength. Every possible point was used to dichotomize the functional measure; patients with higher measurement values were predicted to be satisfied, and patients with a lower measurement values were predicted to be dissatisfied. These predictions were then compared to the true satisfaction status based on the MHQ item scores to calculate sensitivity, or true-positive rate, and 1-specificity, or false- positive rate. Sensitivity and 1-specificity were plotted against each other to produce the ROC curves, and the area under the curve (AUC) was calculated for each. A diagonal line from lower left to upper right represents a perfectly useless predictor: it has the same chance of predicting satisfaction for everyone, regardless of true satisfaction status. The AUC in this case is 0.5. A perfect predictor has a ROC curve that runs up the left side and across the top of the graph: it is possible to select a cut-point that perfectly distinguishes satisfied from dissatisfied patients. This predictor has an AUC of 1. In reality, almost every predictive test falls between these two extremes. Predictive tests with an AUC of less than 0.75 are not considered clinically useful (21). In order to compare the predictive power of different tests on the same “gold standard”, the AUCs of the ROCs can be compared, with the higher being the better predictor (22). We selected the best cut-point as the point on the ROC curve furthest away from the line connecting the lower left-hand and upper right-hand corners; this is appropriate to find the predictor that best distinguishes the true state if sensitivity and specificity are equally important (23). For the best cut-off point, two additional statistics were calculated: positive predictive value (PPV), or the percentage of patients predicted to be satisfied who were satisfied; and negative predictive value (NPV), or the percentage of patients predicted to be dissatisfied that were dissatisfied. Statistical analyses were performed in SAS 9.1 (SAS Institute Inc., Cary, NC) and SPSS 16 (SPSS Inc., Chicago, IL).
Results
125 patients were eligible for these analyses. Because of missing data, the sample size for the analyses may vary. Table 1 presents a summary of the patient characteristics. The mean age was 50 years, with a range of 18 to 85. The majority of patients were female (67%), white (94%), and had college, graduate, or professional degree (57%).
Table 1.
Patient Characteristics
| Mean age, years (sd) | 50 (17) |
| Female, number (%) | 83 (67) |
| College Graduate or Higher, number (%) | 67 (57) |
| White, number (%) | 116 (94) |
| Income > $70,000 per year, number (%) | 52 (43) |
| AO Classification of Fracture, number (%)* | |
| A (%) | 41 (45) |
| B (%) | 10 (11) |
| C (%) | 40 (44) |
Among patients with available data
The outcomes measures under consideration are summarized in Table 2. At 3 months, the mean wrist arc of motion measured as a percent of the uninjured hand was 79.8% (range= 42.2–104%). The adjusted mean grip strength measured as a percent of the uninjured after adjustment with the10% rule hand was 58.2% (range = 0–115%), and the mean key grip strength measured as a percent of the uninjured hand after adjustment with the 10% rule was 81.8% (range=38.8–120%). Seventy-six participants (65% of those with available data) were satisfied with the range of motion of the injured wrist, whereas 41 (35%) were not. Eighty-six participants (58%) were satisfied with the strength in the injured hand, and 50 (42%) were not. The Pearson’ Correlation Coefficient between wrist range of motion and grip strength was 0.55 (p<0.001), and between wrist range of motion and key pinch strength was 0.35 (p<0.001). Considering satisfaction before dichotomization, we found that the estimated Spearman’s Correlation between grip strength and satisfaction with strength was 0.50 (p<0.0001), 0.47 (p<0.0001) between key pinch strength and satisfaction with strength, and 0.53 (p<0.0001) between arc of wrist motion and satisfaction with wrist motion, where positive correlation indicates that higher functional outcomes score is associated with higher satisfaction.
Table 2.
Objective outcomes and satisfaction 3 months after fixation with the volar locking plating system
| Mean Wrist Arc of Motion, % (sd)* | 0.80 (0.13) |
| Mean Grip Strength, % (sd)* | 0.58 (0.25) |
| Mean Key Grip Strength, % (sd)* | 0.82 (0.16) |
| Wrist Arc of Motion** | |
| Satisfied (%) | 76 (65) |
| Dissatisfied (%) | 41 (35) |
| Strength** | |
| Satisfied (%) | 68 (58) |
| Dissatisfied (%) | 50 (42) |
Measured as percent of the uninjured side
Among patients with available data
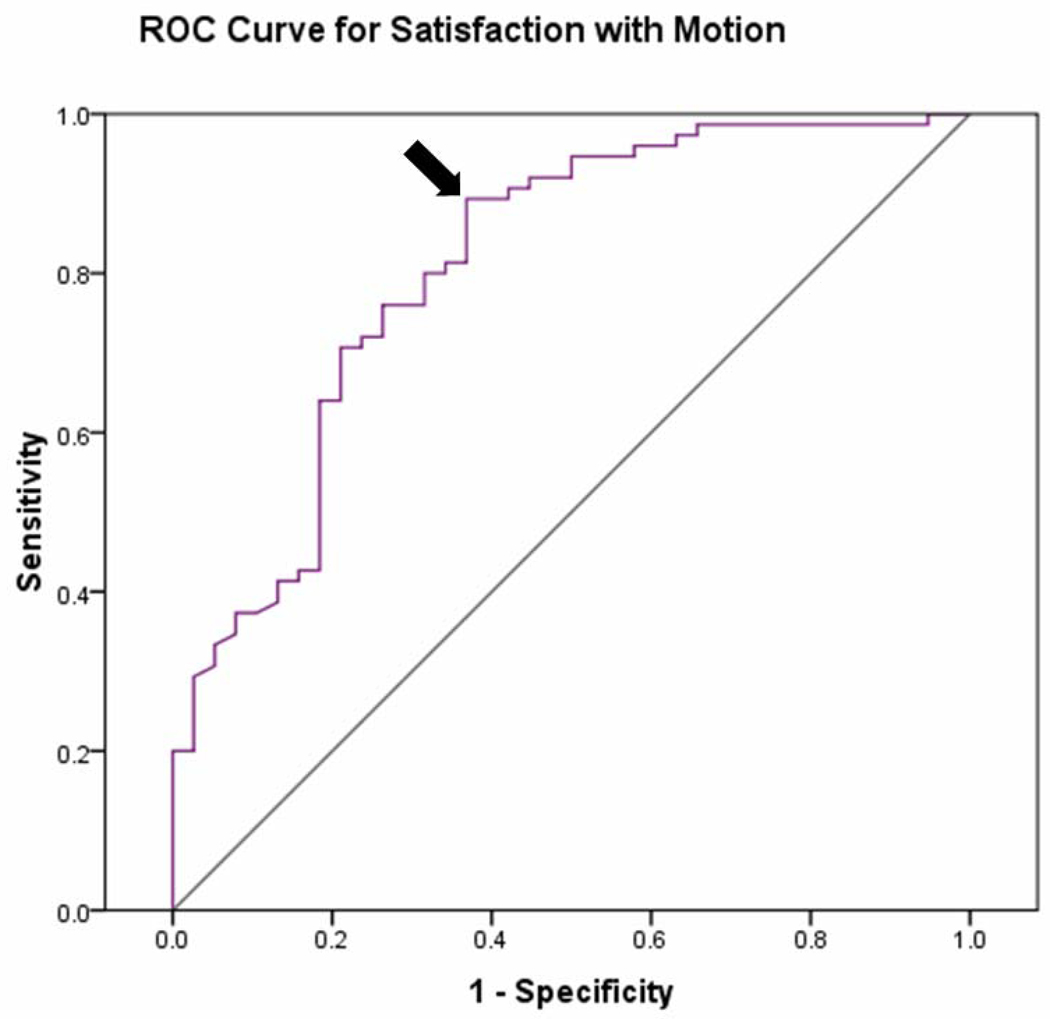
The AUC of the ROC curve between wrist arc of motion and satisfaction with wrist motion (Figure 1) was calculated to be 0.81 (95% CI: 0.72, 0.90). A cut-off point of 95% of the normative hand was selected. This cut-off point has sensitivity of 0.89, specificity of 0.63, PPV of 0.83, and NPV of 0.75.
Figure 1.
ROC curve using satisfaction with wrist motion as the “gold standard”, and arc of motion as the continuous predictor. The arrow indicates the cut-point that best discriminates between satisfied and dissatisfied.
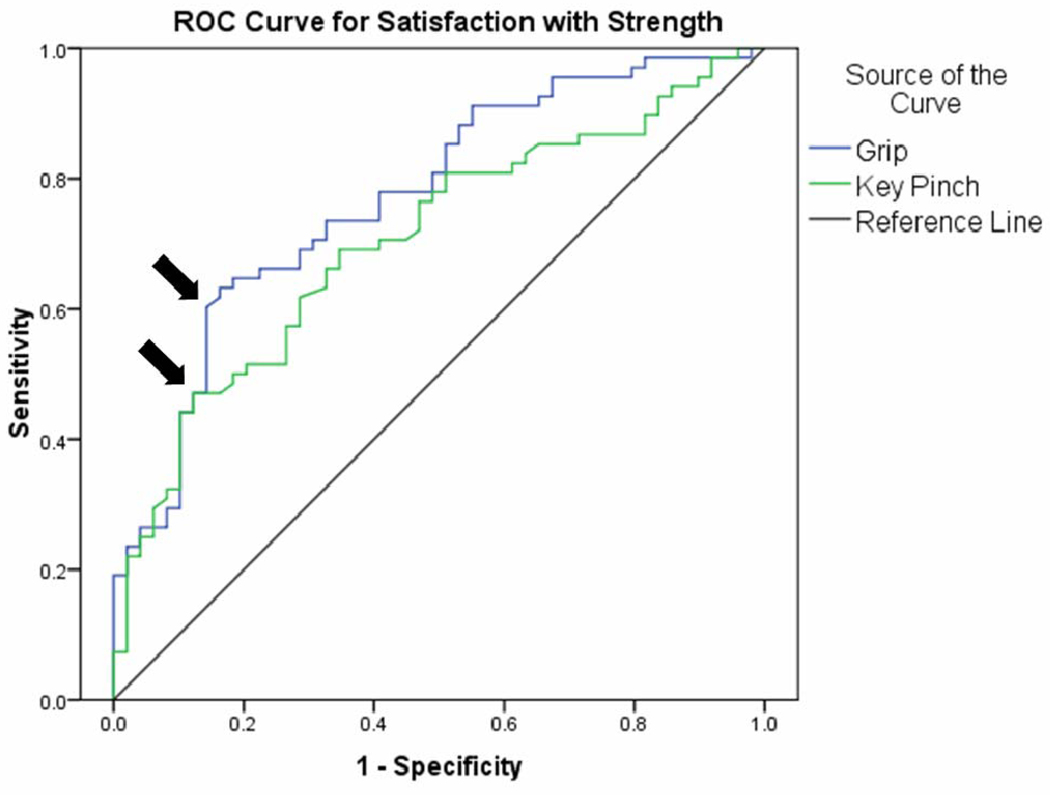
The AUC of the ROC curve between grip strength and satisfaction with hand strength (Figure 2) was 0.77 (95% CI: 0.68, 0.86). The best cut-off point was determined to be 65% of the normative hand. This cut-off point had a sensitivity of 0.60 and a specificity of 0.86. The PPV is 0.85 and the NPV is 0.61.
Figure 2.
ROC curve with satisfaction with hand strength as the “gold standard”, and grip strength and key pinch strength as the continuous predictors. The arrows indicate the cut-points that best discriminate between satisfied and dissatisfied.
The AUC for the ROC curve between key pinch strength and satisfaction with hand strength (Figure 2) was 0.71 (95% CI: 0.61, 0.80). The best cut-point was 87% of the normative hand, with sensitivity of 0.47 and specificity of 0.88. The PPV is 0.84 and the NPV is 0.54.
Discussion
ROC curves are often used to find a suitable cut-off value for a laboratory test to predict presence or absence of disease; however, this technique can be used more generally to find the value of any continuous variable that best discriminates between the states of a dichotomous variable. For example, this technique has recently been used to find the minimal clinically important improvement in self-rated pain, function, ADL, and ability to work needed for patient satisfaction (24) . In this study, we used the ROC curves to evaluate the strength of association between the functional measures of grip strength, key pinch strength, and wrist arc of motion with patient satisfaction, and to define the level of recovery of the_functional measures that best predicts patient satisfaction. Grip strength, with an AUC of 0.77, was found to be a better predictor of satisfaction with hand strength than key grip (AUC=0.71). All of the functional measures we considered had a moderately high AUC with patient satisfaction, indicating that satisfaction and these functional measures are positively related. However, the functional measures are far from perfectly predictive of patient satisfaction, as is clear from the sensitivity, specificity, PPV, and NPV; none of the functional measures of outcome perfectly distinguish dissatisfied from satisfied patients. This finding agrees with previous studies that have found that functional measures of outcome are positively associated with patient evaluation after wrist and hand surgery, but do not fully explain patient evaluations of their outcomes. For example, Karnezis and Fragkiadakis (25) found that in distal radius fracture patients, grip strength, but not wrist extension and flexion, was predictive of better self-reported outcome using the patient-rated wrist evaluation (PRWE) score using multiple linear regression. Their final model for predicting PRWE included grip strength and adjusted for patient demographic and presence of an intra-articular fracture of the radiocarpal or distal radio-ulnar joints, and had an R2 value of 0.43, indicating that the model explained only 43% of the variability of PRWE.
Several previous studies have quantified the range of active wrist motion needed to perform activities of daily living (ADL). Ryu et al. found that in 40 healthy subjects, most activities simulating ADL could be performed with 40 degrees each of wrist flexion and extension, with some complementary rotation of the forearm (26). Palmer et al. determined that 30 degrees of wrist extension and 5 degrees of wrist flexion are needed to perform 52 ADL tasks (27). If we take the normal wrist arc of extension-flexion motion to be about 140 degrees (26, 28), these studies estimate that 25–57% of normal arc of motion is needed to carry out ADL. Despite these previous studies indicting that a relatively restricted wrist arc of motion is sufficient to perform ADL, we found that DRF patients need to regain 95% of the arc of motion, almost returning to their pre-injury arc of motion, to be satisfied, based on ROC curves relating arc of motion with patient satisfaction. Although it may not be possible to return to the pre-injury arc of wrist motion after DRF (28), surgeons and therapists should be aware that their patients may only be satisfied with regaining close to their normal wrist arc of motion. The difference between the minimum arc of motion needed for ADLs and that needed for satisfaction may be related to patient expectations. After injury, an otherwise healthy patient may expect to regain full function of his or her wrist, and may not be satisfied with the minimum arc of motion needed to perform ADL. However, it is possible in that in chronic conditions in which both hands are affected, such as rheumatoid arthritis, patient expectation may be much lower, and a much lower arc of motion may be needed for patients to feel satisfied with their wrist motion. This is a hypothesis that is worth exploring in the future.
In their evaluation of outcomes measures in Colles’ fracture patients, Sarmiento et al. considered patients with less than 60% of normative grip strength to have significantly impaired function (29). Our study confirms Sarmiento et al.’s estimation of a cut-point for the grip strength that patients seek. We estimate that patients need to recover about 65% of the grip strength and 87% of the key-pinch strength of their normative hand to be satisfied.
Conclusions
In this paper, we establish cut-off points for functional measures of outcome that best distinguish between patient satisfaction and dissatisfaction with their outcomes after DRFs. Development and use of statistical and outcomes tools to allow patients to evaluate their health are likely to continue to expand. It is of practical interest to consider what these tools are measuring, including how they are related to traditional, functional outcomes measures.
Acknowledgments
Supported in part by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120), and an Exploratory/Developmental Research Grant Award (R21 AR056988) (To Dr. Kevin C. Chung). We appreciate the assistance of the hand therapists at the University of Michigan for collecting the hand functional data.
The authors would like to thank the hand therapists at the medical center for collecting the data used in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chung KC, Squitiere L, Kim HM. A comparative outcomes study of using the volar locking plating system for distal radius fractures in both young and elderly adults. J Hand Surg. 2008;33A:809–819. doi: 10.1016/j.jhsa.2008.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Handoll HH, Huntley JS, Madhok R. Different methods of external fixation for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2008:CD006522. doi: 10.1002/14651858.CD006522.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boone DC, Azen SP, Lin CM, Spence C, Baron C, Lee L. Reliability of goniometric measurements. Phys Ther. 1978;58:1355–1390. doi: 10.1093/ptj/58.11.1355. [DOI] [PubMed] [Google Scholar]
- 4.Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg [Am] 1984;9:222–226. doi: 10.1016/s0363-5023(84)80146-x. [DOI] [PubMed] [Google Scholar]
- 5.Low JL. The reliability of joint measurement. Physiotherapy. 1976;62:227–229. [PubMed] [Google Scholar]
- 6.Solgaard S, Carlsen A, Kramhoft M, Petersen VS. Reproducibility of goniometry of the wrist. Scand J Rehabil Med. 1986;18:5–7. [PubMed] [Google Scholar]
- 7.Kotsis SV, Lau FH, Chung KC. Responsiveness of the Michigan Hand Outcomes Questionnaire and physical measurements in outcome studies of distal radius fracture treatment. J Hand Surg. 2007;32A:84–90. doi: 10.1016/j.jhsa.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;32:1–6. doi: 10.1007/s00264-007-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ireson CL, Schwartz RW. Measuring outcomes in surgical patients. Am J Surg. 2001;181:76–80. doi: 10.1016/s0002-9610(00)00524-9. [DOI] [PubMed] [Google Scholar]
- 10.Amadio PC. Outcomes assessment in hand surgery. What’s new? Clin Plast Surg. 1997;24:191–194. [PubMed] [Google Scholar]
- 11.Macey AC, Burke FD, Abbott K, Barton NJ, Bradbury E, Bradley A, Bradley MJ, Brady O, Burt A, Brown P. Outcomes of hand surgery. British Society for Surgery of the Hand. J Hand Surg [Br] 1995;20:841–855. doi: 10.1016/s0266-7681(95)80059-x. [DOI] [PubMed] [Google Scholar]
- 12.Davis Sears E, Burns PB, Chung KC. The outcomes of outcome studies in plastic surgery: a systematic review of 17 years of plastic surgery research. Plast Reconstr Surg. 2007;120:2059–2065. doi: 10.1097/01.prs.0000287385.91868.33. [DOI] [PubMed] [Google Scholar]
- 13.HCAHPS. Patients' Perspectives of Care Survey. Centers for Medicare & Medicaid Services; [Google Scholar]
- 14.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg. 2002;27A:205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 15.Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg. 2006;88A:2687–2694. doi: 10.2106/JBJS.E.01298. [DOI] [PubMed] [Google Scholar]
- 16.Michigan Hand Outcomes Questinnaire Website. [Google Scholar]
- 17.Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg. 1998;23A:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 18.Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999;42:619–622. doi: 10.1097/00000637-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Scott SC, Goldberg MS, Mayo NE. Statistical assessment of ordinal outcomes in comparative studies. J Clin Epidemiol. 1997;50:45–55. doi: 10.1016/s0895-4356(96)00312-5. [DOI] [PubMed] [Google Scholar]
- 20.Petersen P, Petrick M, Connor H, Conklin D. Grip strength and hand dominance: challenging the 10% rule. Am J Occup Ther. 1989;43:444–447. doi: 10.5014/ajot.43.7.444. [DOI] [PubMed] [Google Scholar]
- 21.Fan J, Upadhye S, Worster A. Understanding receiver operating characteristic (ROC) curves. CJEM. 2006;8:19–20. doi: 10.1017/s1481803500013336. [DOI] [PubMed] [Google Scholar]
- 22.Everitt BS, Palmer CR, editors. Encyclopaedic Companion to Medical Statistics. London: Hodder Arnold; 2005. Area under the Curve; pp. 12–13. [Google Scholar]
- 23.Riffenburgh RH. Statistics In Medicine. 2nd ed. San Diego, CA: Elsevier Academic Press; 2006. [Google Scholar]
- 24.Shauver M, Chung KC. Minimal Clinically Significant Difference of the Michigan Hand Outcomes Questionnaire. The Journal of Hand Surgery. doi: 10.1016/j.jhsa.2008.11.001. (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karnezis IA, Fragkiadakis EG. Association between objective clinical variables and patient-rated disability of the wrist. J Bone Joint Surg Br. 2002;84:967–970. doi: 10.1302/0301-620x.84b7.12673. [DOI] [PubMed] [Google Scholar]
- 26.Ryu JY, Cooney WP, 3rd, Askew LJ, An KN, Chao EY. Functional ranges of motion of the wrist joint. J Hand Surg [Am] 1991;16:409–419. doi: 10.1016/0363-5023(91)90006-w. [DOI] [PubMed] [Google Scholar]
- 27.Palmer AK, Werner FW, Murphy D, Glisson R. Functional wrist motion: a biomechanical study. J Hand Surg [Am] 1985;10:39–46. doi: 10.1016/s0363-5023(85)80246-x. [DOI] [PubMed] [Google Scholar]
- 28.Laseter GF. Therapist's Management of Distal Radius Fractures. In: Mackin EJ, Callahan AD, Skirven TM, Schneider EC, Osterman AL, Hunter JM, editors. Rehabilitation of the Hand and Upper Extremity. 5th ed. St. Louis: Mosby; 2002. pp. 1136–1152. [Google Scholar]
- 29.Sarmiento A, Pratt GW, Berry NC, Sinclair WF. Colles' fractures. Functional 319 bracing in supination. J Bone Joint Surg. 1975;57A:311–317. [PubMed] [Google Scholar]