Abstract
Numeracy, the “ability to understand and use numbers in daily life” is an important but understudied component of literacy. Numeracy-related tasks are common in healthcare and include understanding nutrition information, interpreting blood sugar readings and other clinical data, adjusting medications, and understanding probability in risk communication. While literacy and numeracy are strongly correlated, we have identified many patients with adequate reading ability but poor numeracy skills. Better tools to measure numeracy and more studies to assess the unique contribution of numeracy are needed. This research can contribute to developing interventions to improve outcomes for patients with poor numeracy.
Introduction
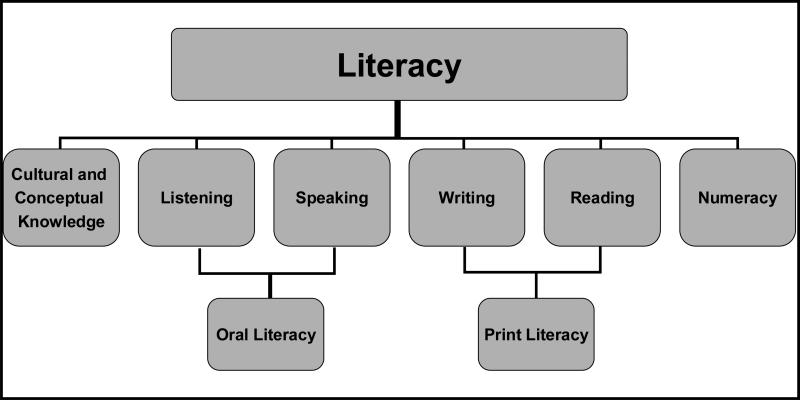
Literacy is “an individual's ability to read, write, and speak in English, and compute and solve problems at levels of proficiency necessary to function on the job and in society, to achieve one's goals, and develop one's knowledge and potential(Committee on Health Literacy, 1999).” In the recent Institute of Medicine report, Health Literacy, literacy is considered to include a variety of skills beyond reading and writing (print literacy), including: listening and speaking (oral literacy), cultural knowledge, and numeracy (Figure 1)(Institute of Medicine Committee on Health Literacy, 2004). While some research has examined the role of oral and print literacy, much less has focused on numeracy. This article will examine current measures of numeracy, review pertinent research related to the role of numeracy in health care, and explore challenges related to numeracy measurement and intervention. This article represents the perspectives and critical analysis of the authors based on current research in this field, and our own experience in numeracy and literacy research. We hope that this perspective article will promote future research in this important field of inquiry.
Figure 1. Components of Literacy.
From IOM Report(Institute of Medicine Committee on Health Literacy, 2004)
Defining Numeracy
There is currently no general agreement on the definition of health related numeracy.(Golbeck, Ahlers-Schmidt, Paschal, & Dismuke, 2005; Peters, Hibbard, Slovic, & Dieckmann, 2007; Minister of Industry, 2005) The Oxford English Dictionary defines numeracy as “the quality or state of being numerate; ability with or knowledge of numbers(OED, 2005).” Although some healthcare researchers have primarily considered numeracy in terms of understanding risks or probability(Schwartz, Woloshin, Black, & Welch, 1997; Woloshin, Schwartz, Moncur, Gabriel, & Tosteson, 2001; Schwartz, Woloshin, & Welch, 2005; Lipkus, Samsa, & Rimer, 2001; Sheridan & Pignone, 2002; Sheridan, Pignone, & Lewis, 2003; Haggstrom & Schapira, 2006; Peters et al., 2006; Schapira, Nattinger, & McAuliffe, 2006), numeracy actually involves a range of skills (Table 1) including: one's ability to perform basic math functions (calculations, fractions, algebra, geometry), understand time, money, measurement, graphs, probability, and the ability to perform multi-step math. Numeracy also includes the ability to figure out what math skills to apply to a given situation (i.e., contextual or application oriented numeracy)(Montori & Rothman, 2005; Golbeck et al., 2005). Golbeck has recently suggested that Numeracy consists of four main skills: Basic (example identifying numbers), Computational (ex. simple manipulation of numbers), Analytical (including inference, estimation, proportions), and Statistical (ex probability, risk) (Golbeck et al., 2005). Similar to the concept of “functional” literacy, we, in agreement with Golbeck, believe there is also a concept of “functional numeracy”, which involves the ability to appropriately apply math skills to perform a particular task. We have defined numeracy simply as “the ability to understand and use numbers in daily life(Rothman et al., 2006).”
Table 1.
Common Numeracy Skills
| Common Numeracy Skills |
|---|
| Skills |
| Numeration/counting/hierarchy |
| Calculations (addition, subtraction, multiplication, division) |
| Understanding time/dates |
| Reading graphs/tables/figures/ measurement |
| Using fractions/ decimals/ percentages/ proportions |
| Understanding probability |
| Higher order mathematics (algebra, geometry, calculus, etc.) |
| Applied (Contextual) Skills |
| Performing multi-step math problems |
| Estimation |
| Applying logic |
| Ability to interpret/ infer mathematics from problem/situation, problem solving |
In 1992, the National Adult Literacy Survey (NALS)(Kirsch, Kader, Jensen, & Kopher, 2002)found that 26% of adults surveyed could not perform the most rudimentary of quantitative skills or had extremely limited skills, and another 32% of respondents had only basic skills. Those with basic skills could perform simple one-step arithmetic problems when the numbers were explicitly given, but could not perform multi-step arithmetic, or determine what math skills were needed when reading a problem. For example, these people could not interpret a bus schedule to figure out how much time it would take to go from one location to another(Kirsch et al., 2002).
Although there is a correlation between print literacy and numeracy (Kirsch et al., 2002), we have found that there are many patients who have adequate print literacy but are still unable to use math skills appropriately(Rothman et al., 2005; Rothman et al., 2006). Many health-related tasks, such as reading food labels, refilling prescriptions, measuring medications, interpreting blood sugars or other clinical data, and understanding health risks, rely on numeracy. These tasks often require patients to deduce which mathematical skills to use and then to use these in multi-step fashion. Patients who had difficulty learning math skills during their primary education may now be too intimidated or simply unable to call upon these skills. For patients with chronic illness that rely on self-management to safely and efficaciously self-administer treatments this is particularly relevant and may place patients who lack adequate numeracy skills at increased risk for poor health outcomes. Numeracy may be a unique explanatory factor for adverse outcomes beyond the explanations provided by overall literacy.
Measuring Numeracy
Numeracy measurement may be important for both research and clinical reasons. In research, measuring numeracy is important to document the extent of the problem, to measure the associations between numeracy and adverse health outcomes, and to test whether potential interventions to overcome numeracy-related barriers are effective in reducing disparities in these health outcomes. Measuring numeracy more rigorously in the health field could help to better determine the unique contributions of numeracy and to identify patients with adequate overall health literacy skills but inadequate numeracy skills. Measuring numeracy could also assist the development of specific numeracy-oriented interventions that might prove to be more effective than general literacy interventions for patients with low numeracy.
Table 2 outlines current tools that are available to measure numeracy. Each tool has distinct advantages and disadvantages. The educational community uses numeracy scales designed primarily to measure mathematical skills. These tests (ex. KeyMath, K-TEA, WRAT) were created to assess school-aged children, but have often been validated in adults(Wilkinson, 1993; Kaufman & Kaufman, 1985; Connolly, Natchman W, & Pritchett, 1971; Flanagan et al., 1997). These tools’ length and heavy focus on mathematical skills as opposed to other numeracy components may be intimidating to patients with poor numeracy. Another broad measure of numeracy are the quantitative items used in the NALS in 1992(Kirsch et al., 2002) and the National Assessment of Adult Literacy (NAAL) in 2003 (US Department of Education, 2006). These scales focused on “the knowledge and skills required to apply arithmetic operations, either alone or sequentially, using numbers embedded in printed materials (Kirsch et al., 2002).” Recently, the International Adult Literacy Survey (IALS) Adult Literacy And Life Skills Survey (ALLS) was developed by a group of international experts in literacy to measure proficiency levels in a host of skills. In contrast to the NAAL, the ALLS defined numeracy very broadly as the “knowledge and skills required to effectively manage and respond to the mathematical demands of diverse situations”, and suggested that numeracy is broader than the quantitative focus of the IALS or NAAL (Minister of Industry, 2005). However, the items from the NALS, NAAL, and ALLS are not readily available for public use, and most of the items were not developed to specifically examine the role of numeracy in health.
Table 2.
Measures of Numeracy
| Test | Admin Time (min) | Age | Measurement | Advantages | Disadvantages |
|---|---|---|---|---|---|
| WRAT-3 (Wide Range Achievement Test) | 15 minutes (for Math Section) | 5-75 | Primarily calculations, basic algebra. | Validated in a large population of people. Provides absolute scores, scores standardized by age, and grade equivalents. | Primarily focuses on mathematical calculations. No health focus. |
| K-TEA (Kaufman Test of Educational Achievement) | Brief: 30 mins Comprehensive: 60 - 75 mins | Children in grades 1-12 | Measures basic arithmetic, lifelike situations, numerical reasoning, written computational skills, oral (accompanied with visual stimuli) and written problems | Can start at different grade levels. Age based and grade based norms. Brief and Comprehensive forms available. | Lengthy test. Individually administered No health focus. |
| Key Math | 35-50 minutes | Children in Grades K-9 | Covers basic concepts (numeration, geometry, etc.), operations, and applications (measurement, time, problem solving, etc.). | Can start at different grade levels. Provides comprehensive coverage. | Lengthy. Primarily focused on younger participants. No health focus. |
| Woodcock-Johnson | Test until a ceiling is reached | 2-95 | Measures calculation and applied problems in the standard battery. Quantitative concepts in the supplemental battery. | Validated in a broad age range. Can start at different levels. | Lengthy. No health focus. |
| TOFHLA (Test of Functional Health Literacy in Adults) | 10 minutes (numeracy section) | Adults | Measures numeracy and reading Comprehension | Directed toward capturing numeracy skills in the middle to low levels of literacy ability. | Numeracy questions rely heavily on verbal literacy and are highly correlated with Literacy questions. |
| Lipkus/Schwartz 3 and 7 item numeracy measures | 1-3 minutes | Adults | Measures understanding of frequency, probability, and percentages. | Brief | Focuses on one specific component of numeracy. |
| Medical Data Interpretation Test | Time not specified. Includes 18 items. | Adults | Focuses on risk perception and probability | In-depth examination of patient understanding of risks | Focuses on one component of numeracy. May not be suitable for low numerate populations |
| Newest Vital Sign | 3-5 minutes | Adults | Measures understanding of nutrition label | Correlated with full TOFHLA. Brief. | Primarily designed as a screening instrument. Not yet validated for other use. |
Several measures focus on health-related numeracy. The original TOFHLA included several reading passages and 17 questions to measure numeracy (Parker, Baker, Williams, & Nurss, 1995). In the TOFHLA, the numeracy component is scored and added to the literacy component and the total score has been compared to other literacy measures (ex. REALM, and reading section of the WRAT), but not to tests of mathematical skills(Parker et al., 1995). However, the TOFHLA primarily focuses on print literacy with limited assessment of other health literacy skills (Institute of Medicine Committee on Health Literacy, 2004). The numeracy questions primarily focus on reading prescriptions and other materials that test simple mathematical skills such as understanding dates and timing of medication dosage. More complex skills including multi-step math, probability, and problem-solving are not well assessed. In our opinion, these numeracy questions are highly dependent on reading ability, and not surprisingly, they are highly correlated to reading ability. Based on these findings, many investigators have used a shortened TOFHLA (S-TOFHLA) that does not include any numeracy questions (Baker, Williams, Parker, Gazmararian, & Nurss, 1999; Schillinger et al., 2002). We would contend that the numeracy section of the TOFHLA was not designed to accurately measure the host of numeracy skills that patients require, and focuses too much on measuring simple quantitative skills that rely more heavily on one's reading ability than on one's numeracy skills.
Schwartz and Woloshin(Schwartz et al., 1997) produced a “Numeracy Scale”, that Lipkus later modified (Lipkus et al., 2001), to assess understanding of percentages, frequency, probability, but these scales do not examine other numeracy-related skills. More recently Schwartz and Woloshin developed a more extensive scale that measures patients’ statistical skills in relation to risk perception (Schwartz et al., 2005). In our opinion, these scales focus on very high level quantitative skills, and may be of limited value in very low literacy/numeracy populations where performance on these scales would be universally poor.
Recently, Weiss and others developed the Newest Vital Sign (Weiss et al., 2005) to identify patients with low health literacy. This quick test involves interpreting information from a nutrition label. The items of the scale test literacy and numeracy skills, and the authors suggest that the numeracy aspects helped to make the scale a more valid measure of health literacy. This scale was primarily designed as a screening instrument, and its role in research has not been well validated.
Recent Studies of the Role of Numeracy in Health Care
A few studies have begun to document the importance of numeracy in health. Using the TOFHLA, Williams and colleagues (Williams et al., 1995) found that many patients could not read and understand basic medical directions containing numerical information including instructions on medication bottles and standard appointment slips and financial information. For example, approximately 1 in 4 patients could not interpret an appointment slip to determine when their next appointment was scheduled, and 19-33% of English-speaking patients could not determine the number of pills of a prescription they should take. Even patients with adequate literacy had some difficulty comprehending the more difficult numerical tasks.
Other studies have examined patients’ ability to understand sophisticated numerical concepts such as probability and risk perception (Schwartz et al., 1997; Schwartz et al., 2005; Lipkus et al., 2001; Sheridan et al., 2002; Sheridan et al., 2003; Schapira, Davids, McAuliffe, & Nattinger, 2004; Schapira et al., 2006; Haggstrom et al., 2006). Schwartz and Woloshin found only 16% of women correctly answered all three items of their Numeracy Scale. These women's numeracy skills were associated with accuracy of applying quantitative information about the benefit of mammography to their perceived risk for death(Schwartz et al., 1997). A similar study of women found that higher numeracy was associated with more consistent interpretation of breast cancer risk(Schapira et al., 2004). Sheridan and colleagues(Sheridan et al., 2003) examined whether patients could understand written information on treatment benefits when it was presented as number needed to treat (NNT), absolute risk reduction (ARR), relative risk reduction (RRR) or a combination. Participants correctly identified which of two treatments provided greater benefit 44% of the time, but only correctly calculated the exact effect of treatment on a given risk of disease 13% of the time. Higher numeracy, as measured by the 3 item Schwartz/Woloshin Numeracy Scale, was correlated with improved ability to interpret treatment benefits. Estrada (Estrada, Martin-Hryniewicz, Peek, Collins, & Byrd, 2004) found that among a group of patients on anticoagulation therapy, patients’ inability to handle basic probability and numerical concepts was associated with poorer anticoagulation control.
We recently examined the relationship between numeracy and literacy skills and patient understanding of nutrition labels among 200 patients in a primary care clinic (Rothman et al., 2006). Even though 77% of patients had ≥ 9th grade literacy skills (on the REALM), only 37% of patients had ≥ 9th grade math skills on the WRAT-3R (Table 3). Among patients with 9th grade literacy skills or greater, 36% still had < 6th grade math skills, and 18% had 7th-8th grade math skills. Patients had significant difficulties understanding and interpreting food labels. Common errors included misapplication of the serving size, confusion over extraneous information on the label (such as the Percent Daily Value information), and calculation errors. Patient comprehension of nutrition labels was highly correlated to their underlying literacy and numeracy skills.
Table 3.
The relationship between numeracy, literacy, and education status
| Variable (n=200) | Numeracy Ability (Measured by WRAT) |
||||
|---|---|---|---|---|---|
| |
1-6th grade |
7th-8th grade |
9th-12th grade |
> 12th grade |
P value** |
| Education Level | <0.0001 | ||||
| < High School | 15 (88%) | 2 (12%) | 0 (0%) | 0 (0%) | |
| High School | 35 (73%) | 5 (10%) | 8 (17%) | 0 (0%) | |
| Some College | 31 (46%) | 12 (18%) | 18 (26%) | 7 (10%) | |
| ≥ College |
11 (16%) |
15 (22%) |
24 (36%) |
17 (25%) |
|
| Literacy Level* | < 0.0001 | ||||
| 0-6th Grade | 16 (100%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| 7th-8th | 20 (67%) | 6 (20%) | 3 (10%) | 1 (3%) | |
| ≥ 9th Grade | 56 (36%) | 28 (18%) | 47 (31%) | 23 (15%) | |
Measured by Rapid Estimate of Adult Literacy in Medicine (REALM)
Chi squared analyses
We have also found significant numeracy deficits related to diabetes. In one study, we developed and administered a scale, the Diabetes Numeracy Evaluation (DIANE) to 250 diabetes patients recruited from two sites (Montori et al., 2004). In this well-educated sample of patients (83% ≥ 9th grade literacy skills on the REALM) with decent glycemic control (mean A1c 7.7%), 88% identified whether a glucose value was within the target range, and 82% identified a trend in a series of 5 self-monitored glucose values. While 87% of patients seen in the diabetes specialty clinic chose the correct dose of insulin for the carbohydrates ingested, only 52% of patients seen in the community clinic were able to do so. In another study, we recently developed a more comprehensive measure of diabetes related numeracy skills (the Diabetes Numeracy Test) and administered it to 398 patients (Rothman et al., 2005). Patients had difficulties performing many numeracy related tasking including: calculating carbohydrate intake, understanding glucose meter readings, interpreting sliding scale regimens, titrating oral medications or insulin, and adjusting insulin for carbohydrate content. Higher performance on the Diabetes Numeracy Test was significantly correlated with higher diabetes knowledge and higher perceived self efficacy. A modest correlation with glycemic control (A1C) as also observed. Manuscripts further detailing findings related to theses diabetes related numeracy scales are currently under review. We are also currently in the process of using the information learned from these studies to perform a randomized trial of an educational intervention that uses numeracy-related accommodations for patients with diabetes.
Methodological Challenges of Measuring Numeracy
The measurement tradition recognizes three domains to consider whether a measurement has value: judgment or content validity, reliability (such as test-retest reliability), and empirical validity (Streiner & Norman, 2003). Content validity results from expert judgment about the extent to which a tool appears to measure what is desired to measure. Numeracy is a multidimensional skill that involves assessing when to use numerical skills, deciding which skills to use, using the skills effectively to solve the problem, and then interpreting the results appropriately. For a generic numeracy tool to have content validity, it should capture each of these dimensions. As we discussed above, in our opinion, the numeracy items of the TOFHLA or the numeracy scales of Schwartz-Woloshin/Lipkus do not appear to have sufficient content validity for a generic multidimensional numeracy tool. To our knowledge, there are no generic health numeracy tools with adequate content validity available.
Empirical validity can often be achieved by having individuals receive the test of interest and another test that is suppose to measure the same property (sometimes called concurrent, convergent, or criterion validity). Currently, there is no “criterion (gold) standard” health numeracy test to compare and validate any new test of health numeracy. Furthermore, there is no consensus on what numeracy domains should be included in a gold standard test. We have outlined many of the domains that should be considered for a possible health numeracy scale in Table 1. Future work needs to be performed to determine which constructs are the most useful, particularly in a health care context. In our own work, we have compared our numeracy scales to the mathematical skills measured by the math section of the WRAT, assuming the WRAT validly assesses general numeracy skills.
When criterion validity is not available, one can also look at construct validity. The assessment of construct validity requires one to set up several experiments to test the hypotheses that link what is measured with the direction and magnitude of change that one would expect on the measurement if it were valid. In our work with diabetes-related numeracy, for example, we examined the relationship between diabetes related numeracy skills and one's diabetes knowledge, diabetes self-management behaviors, and perceived self-efficacy.
Another important dimension of measurement is responsiveness. This dimension may be relevant when testing interventions to improve numeracy. A responsive numeracy tool would be expected to increase in magnitude in response to the impact of a successful intervention. However, a poorly responsive tool may not change despite real improvements. This property may be irrelevant, however, if researchers design interventions to work around numeracy limitations rather than to improve numeracy per se.
There are contextual elements of importance in healthcare that can affect the reliability or validity of numeracy tools. Patients with literacy limitations may score low on numeracy tools because they may not be able to read or understand the questions. Patients may also have difficulties when numbers are written as words, for example reading “four times a day” rather than “4 times a day”. Also, patients tested in the healthcare setting (following an emotionally intense appointment, during a hospitalization for an acute illness) may not perform as well as when they face numeracy challenges in their own environment under usual conditions. In addition, elderly patients, many of whom have chronic diseases which require numerical skills for self-management, may also have global cognitive impairments from strokes, dementia, or depression. Finally, anxiety about math or test-taking in general has been independently associated with poorer reduced working memory capacity, increased test-taking time and increased error rates(Hodge, 1999; Ashcraft & Kirk, 2001) (Eccles & Jacobs, 1986). Math anxiety appears to start early in education and is not always associated with one's math ability (Eccles et al., 1986). These contextual elements and comorbidities may cloud the assessment of numeracy. Alternatively, we may be interested in patients’ actual or current numeracy capacity, as affected as it may be by illiteracy, emotional or physical stress, or global cognitive impairment.
In the evaluation of literacy, many researchers are aware of the need to be highly sensitive to the risk that exposing patients’ inability to read or to comprehend information may embarrass them and cause adverse psychological and behavioral consequences. We are not sure about the extent to which exposing patients’ inability to solve numerical problems will lead to embarrassment and other adverse consequences. Some experts think shame is less of a problem when uncovering limited numeracy (Paulos, 2001). This may result from cultural cues that place a low value on numeracy. An example can be found in gender bias research. Researchers have described situations in which women receiving cultural cues from early age informing them that it is acceptable for women to be innumerate(Gigerenzer, 2002) later have poor performance on numerical tests (Steele, 1997; Quinn & Spencer, 2001).
In our research, we have observed patients faced with our numeracy questions resort to a number of “workarounds”. These have included discretely asking the spouse for help or using a calculator. Depending on the measurement objective, one could perceive the use of these aids as effective strategies to compensate for deficiencies or as interventions that will distort the measurement of numeracy. Again, testing numeracy in patients using aids may be pertinent if the patient always has access to these aids when solving numerical problems. We think that the use of calculators requires further investigation. Given that some numerical problems can be solved mostly without mathematical calculations, the extent to which people with limited numeracy can overcome this problem effectively with the calculator (an aid that will have limited to no impact on thinking through the solution to the problem) remains unclear. Indeed, we have often observed patients using a calculator only to obtain an answer without solving the problem.
Future Challenges
Better measures of numeracy in the health care setting need to be developed. Research with these measures will help to demonstrate that numeracy is a unique component of literacy that is important to patient care. A better understanding of the role of numeracy in health will allow for the development of interventions to accommodate for patients with inadequate numeracy skills. Potential interventions could include: color coded measuring devices that replace measurement related numeracy, picture- or table-based materials that replace medication instructions, simplification of current labels to ease interpretation, and computerized interventions that convert mathematical problems or instructions into goal oriented text, pictures or verbal instruction. We hope this article will encourage others to consider the role of numeracy in patient care, and promote research that will help demonstrate that addressing numeracy can help to improve patient-related outcomes.
Acknowledgements
Drs. Rothman and Pignone have received funding from the National Institutes of Health (NIH), the American Diabetes Association, and the Pfizer Clear Health Communication Initiative to examine the role of literacy and numeracy in health care. Dr. Rothman is also currently funded by an NIH/NIDDK Career Development Award (K23 DK065294).
Reference List
- Ashcraft MH, Kirk EP. The relationships among working memory, math anxiety, and performance. J.Exp.Psychol.Gen. 2001;130:224–237. doi: 10.1037//0096-3445.130.2.224. [DOI] [PubMed] [Google Scholar]
- Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient.Educ.Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- Committee on Health Literacy Health literacy: report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Jama. 1999;281:552–7. [PubMed] [Google Scholar]
- Connolly A, Natchman W, Pritchett E. Key Maths,Diagnostic Arithmetic Test. American Guidance Service. 1971.
- Eccles JS, Jacobs JE. Social Forces Shape Math Attitudes and Performance. Signs. 1986 [Google Scholar]
- Estrada CA, Martin-Hryniewicz M, Peek BT, Collins C, Byrd JC. Literacy and numeracy skills and anticoagulation control. Am.J Med Sci. 2004;328:88–93. doi: 10.1097/00000441-200408000-00004. [DOI] [PubMed] [Google Scholar]
- Flanagan DP, McGrew KS, Abramowitz E, Lehner L, Untiedt S, Berger D, et al. Improvement in Academic Screening Instruments? A Concurrent Validity Investigation of the K-FAST, MBA, and WRAT-3. Journal of Psychoeducational Assessment. 1997;15:99–112. [Google Scholar]
- Gigerenzer G. Calculated risks, how to know when numbers deceive you. 1st ed. New York, NY: 2002. Innumeracy. [Google Scholar]
- Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev.Med. 2005;29:375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Haggstrom DA, Schapira MM. Black-white differences in risk perceptions of breast cancer survival and screening mammography benefit. J Gen Intern Med. 2006;21:371–377. doi: 10.1111/j.1525-1497.2006.00347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodge MB. Do anxiety, math self-efficacy, and gender affect nursing students’ drug dosage calculations? Nurse Educ. 1999;24:36, 41. doi: 10.1097/00006223-199907000-00010. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine Committee on Health Literacy . Health Literacy: A Prescription to End Confusion. The National Academies Press; Washington DC: 2004. [PubMed] [Google Scholar]
- Kaufman A, Kaufman N. Kaufman Test of Individual Acheivement (K-TEA). American Guidance Service. 1985.
- Kirsch I, Kader B, Jensen GV, Kopher W. Adult Literacy in American. National Center for Education Statistics, US Department of Education; 2002. (Rep. No. NCES 1993-275) [Google Scholar]
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis.Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- Minister of Industry , Statistics Canada, Organization for Economic Co-Operation and Development Learning a Living: First Results of the Adult Literacy and Life Skills Survey. 2005.
- Montori VM, Leung T, Thompson C, Chung J, Capes S, Smith S. Validation of a Diabetes Numeracy Evaluation Tool. Diabetes, American Diabetes Association 2004. 2004.
- Montori VM, Rothman RL. Weakness in numbers. The challenge of numeracy in health care. J.Gen.Intern.Med. 2005;20:1071–1072. doi: 10.1111/j.1525-1497.2005.051498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OED Oxford English Dictionary [On-line] 2005 Available: http://dictionary.oed.com/cgi/entry/00328393?single=1&query_type=word&queryword=numeracy&edition=3e&first=1&max_to_show=10 )
- Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- Paulos J. Innumeracy: Mathematical illiteracy and its consequences. 2nd ed. Hill and Wang; New York, NY: 2001. [Google Scholar]
- Peters E, Vastfjall D, Slovic P, Mertz CK, Mazzocco K, Dickert S. Numeracy and decision making. Psychol Sci. 2006;17:407–413. doi: 10.1111/j.1467-9280.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- Peters E, Hibbard J, Slovic P, Dieckmann N. Numeracy Skill And The Communication, Comprehension, And Use Of Risk-Benefit Information. Health Affairs. 2007;26:741–748. doi: 10.1377/hlthaff.26.3.741. [DOI] [PubMed] [Google Scholar]
- Quinn D, Spencer S. The interference of stereotype threat with women's generation of mathematical problem-solving strategies. J Soc Issues. 2001;57:55–71. [Google Scholar]
- Rothman RL, Davis D, Gregory R, Wallston KA, Sparks J, Dewalt DA, et al. Diabetes Numeracy Skills and Relationship to Glycemic Control. Diabetes, supplement, American Diabetes Association 2005. 2005.
- Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, et al. Patient Understanding of Food Labels The Role of Literacy and Numeracy. Am J Prev.Med. 2006;31:391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- Schapira MM, Davids SL, McAuliffe TL, Nattinger AB. Agreement between scales in the measurement of breast cancer risk perceptions. Risk Analysis. 2004;24:665–673. doi: 10.1111/j.0272-4332.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Schapira MM, Nattinger AB, McAuliffe TL. The influence of graphic format on breast cancer risk communication. J Health Commun. 2006;11:569–582. doi: 10.1080/10810730600829916. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. Jama. 2002;288:475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann.Intern Med. 1997;127:966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- Schwartz LM, Woloshin S, Welch HG. Can patients interpret health information? An assessment of the medical data interpretation test. Med Decis.Making. 2005;25:290–300. doi: 10.1177/0272989X05276860. [DOI] [PubMed] [Google Scholar]
- Sheridan SL, Pignone M. Numeracy and the medical student's ability to interpret data. Eff.Clin.Pract. 2002;5:35–40. [PubMed] [Google Scholar]
- Sheridan SL, Pignone MP, Lewis CL. A randomized comparison of patients’ understanding of number needed to treat and other common risk reduction formats. J Gen Intern Med. 2003;18:884–892. doi: 10.1046/j.1525-1497.2003.21102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele C. A threat in the air. How stereotypes shape intellectual identity and performance. Am Psychol. 1997;52:613–629. doi: 10.1037//0003-066x.52.6.613. [DOI] [PubMed] [Google Scholar]
- Streiner D, Norman G. Health Measurement Scales, a practical guide to their development and use. 3rd ed. Oxford University Press; New York, NY: 2003. [Google Scholar]
- US Department of Education National Assessment of Adult Literacy (NAAL): A First Look. 2006. (Rep. No. NCES 2006-470)
- Weiss BD, Mays MZ, Martz W, Castro KM, Dewalt DA, Pignone MP, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann.Fam.Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson GS. WRAT3: Wide Range Acheivement Test Administration Manual. Wide Range Inc.; 1993. [Google Scholar]
- Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, et al. Inadequate functional health literacy among patients at two public hospitals. Jama. 1995;274:1677–82. [PubMed] [Google Scholar]
- Woloshin S, Schwartz LM, Moncur M, Gabriel S, Tosteson AN. Assessing values for health: numeracy matters. Med Decis.Making. 2001;21:382–390. doi: 10.1177/0272989X0102100505. [DOI] [PubMed] [Google Scholar]