Abstract
Objective
Currently, there is no standardized approach to the calculation of growth velocity (GV; g/kg/day) in hospitalized very low birth weight (VLBW) infants. Thus, differing methods are used to estimate GV, resulting in different medical centers and studies reporting growth results that are difficult to compare. The objective of this study was to compare actual GV calculated from infant daily weights during hospitalization in a Neonatal Intensive Care Unit (NICU) with estimated GV using two mathematical models that have previously been shown to provide good estimated GVs in extremely low birth weight infants: an exponential model (EM) and a 2-Point model (2-PM).
Study Design
Daily weights from 81 infants with birth weights of 1000–1499g were used to calculate actual GV in daily increments from two starting points: (1) birth and (2) day of life of regaining birth weight. These daily GV values were then averaged over the NICU stay to yield overall NICU GV from the two starting points. We compared these actual GV with estimated GV calculated using the EM and 2-PM methods.
Results
The mean absolute difference between actual and EM estimates of GV demonstrated <1% error for 100% of infants from both starting points. The mean absolute difference between actual and 2-PM estimates demonstrated <1% error for only 38% and 44% of infants from birth and regaining birth weight, respectively. The EM was unaffected by decreasing BW and increasing length of NICU stay, while the accuracy of the 2-PM was diminished significantly (p<.001) by both factors.
Conclusions
In contrast to the 2-PM, the EM provides an extremely accurate estimate of growth velocity in larger VLBW infants, and its accuracy is unaffected by common infant factors. The EM has now been validated for use in all VLBW infants to assess growth and provides a simple-to-use and consistent approach.
Keywords: anthropometry, birth weight, premature infant, growth assessment, neonates
INTRODUCTION
Postnatal growth in premature infants is a strong predictor of outcome, both as a reflection of concurrent morbidities as well as long-term neurodevelopment 1–8. Several investigators have demonstrated that postnatal growth in very low birth weight infants (VLBW; birth weight <1500g) is influenced by the severity of coexisting morbidities that affect infant nutritional and metabolic status 1–6, 9, 10, and that infants without major morbidities grow at a faster rate than less healthy infants 1, 2, 9, 10. Additionally, poor growth during the neonatal intensive care unit (NICU) stay has long-term implications 7, 8, 11. In extremely low birth weight infants (ELBW; BW <1000g), poor growth during NICU stay exerts a significant, and possibly independent effect on neurodevelopment at 18–22 months corrected age 7. Thus the accurate measurement of postnatal growth is essential to clinical care and research for VLBW infants because growth provides an indirect measure of overall health and nutritional adequacy, and the consequences of poor growth in the NICU may impact these infants for years to come.
Weight growth velocity (GV, g/kg/d) is a commonly used measure in growth and nutrition research in VLBW infants because it summarizes infant weight gain over a specific time interval, smoothing the variability that is inherent in daily weight measures. However, calculation of GV from daily weight measures and averaging these values over the desired time interval is extremely labor-intensive and several methods for estimating the actual average GV have been employed by different researchers 1, 2, 12–17, as previously described for ELBW infants 18. The results of our previous analysis for ELBW infants showed that the most accurate methods are those that use a weight for the denominator that accounts for ongoing infant growth as opposed to simply using birth weight (BW). The exponential model (EM) 18 accurately estimates postnatal GV in ELBW infants throughout the NICU stay, and is unaffected by length of stay, BW, or the presence of chronic lung disease. The 2-point average weight model (2-PM) 13 provides a less accurate, but reasonably close estimate of actual GV, but its accuracy is markedly diminished by the above factors. However, our previous study did not include larger VLBW infants (BW = 1000–1499g), for whom accurate estimates of GV are also important for research and practice. Thus, the purpose of this study was to compare the accuracy of GV estimates obtained with these two mathematical methods to the actual GV calculated from daily weight measures in larger VLBW infants
METHODS
Subjects
One hundred forty infants with BW between 1000–1499g were admitted to Rush University Medical Center NICU between January 1, 1997 and December 31, 1998. Daily weight measures from admission to discharge or transfer were retrospectively accessed from an existing dataset of these larger VLBW infants who survived to discharge19. Exclusion criteria for infants were (1) mother with positive drug screen, (2) to be placed for adoption, (3) admitted after day of life (DOL) 3, and (4) GV for the first month could not be calculated. Daily weight measures for the remaining 81 infants were used to calculate the accurate standard GVs for this study. This study was approved by the Rush University Institutional Review Board.
Growth Velocity
The procedures used to perform the daily weights and their extraction from the existing dataset have been previously described 18. Briefly, all weights were performed by NICU nurses using standard procedures, except for days that infants were deemed too unstable for weighing. The treatment of these missing data is described below. The daily weights from the infant’s medical record were collected and entered into the original database by research assistants 19, and then extracted without editing or deletion for the research reported here. From these weights, the DOL to regain BW was identified for each infant, defined as the first of three successive days that the weight was ≥ BW 18. Actual or accurate standard GV (g/kg/d) was calculated as in daily increments until discharge, where Wn= weight in grams on day “n” and Wn+1= weight in grams on the following day. If the weight had not been recorded for a period of 1–3 days, accurate standard GV was estimated using the weights from the day before and the day after the missing day(s) and averaging over the appropriate time interval. For the majority of cases, weights were missing for a single day at a time; however, weights were not available for 2, 3 and 4 consecutive days in 5, 1 and 1 infant(s), respectively. Weights were estimated as above for only 63 days (1.8%) of a total combined hospital stay of 3 514 days.
The actual and estimated GV methods were applied over two time intervals to determine whether accuracy of the measures varied based on the chosen interval. For each infant, the daily accurate standard GVs were averaged over two time intervals: from day of birth to NICU discharge, and from day of regaining BW to NICU discharge. These actual GV data served as the accurate standard for our comparisons of estimated GV from the two mathematical models. The 2-PM and EM were also applied to each infant over identical time intervals:
Data Analysis
The accurate standard GVs and the estimated GVs from the two models (2-PM and EM) are reported as mean ± SD for the 81 infants. The GVs estimated by the two models were compared to the accurate standard GVs by computing the magnitude of error as reflected by the percentage of absolute difference , and are reported as the mean percentage of absolute difference ± SD. Spearman correlation coefficients (rs) and Mann-Whitney U tests were used to examine the relationship between the absolute magnitude of error in the estimated GVs and factors that may potentially influence the accuracy of GV, such as BW and length of stay. Results were considered significant at p <0.05. Data were analyzed using the SPSS-PC version 15.0 (SPSS, Chicago, IL, USA).
RESULTS
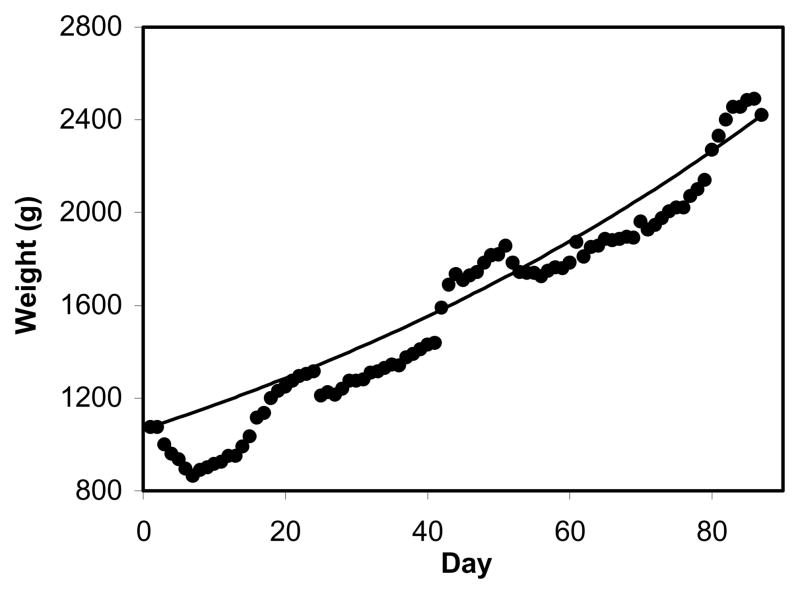
The characteristics of the sample are summarized in Table 1. The mean accurate standard GVs and mean estimated GVs using the two models are summarized in Table 2. For the birth starting point, the mean accurate standard GV was 9.8 g/kg/d (range: 3.1–18.4), and for the regaining BW starting point was 16.1 g/kg/d (range: 9.3–35.3). The mean differences between the accurate standard and estimated GVs are summarized in Table 2. The EM approximated accurate standard GVs extremely closely regardless of starting point used, whereas there were small differences with the 2-PM. Specifically, the mean absolute difference between actual and EM estimates of GV demonstrated <1% error for all 81 infants from both starting points. In contrast, the mean absolute difference between actual and 2-PM estimates of GV demonstrated <1% error for 38% and 44% of infants from birth and regain BW starting points, respectively. Figure 1 shows daily weights from one infant with superimposed EM curve. While the EM does not duplicate the daily variations in weight, it provides a very close approximation of the mean GV over a period of time.
Table 1.
Characteristics of the study sample
| Characteristic | Mean ± SD (range) or N (%) |
|---|---|
| Gestational age (weeks) | 29.7 ± 1.9 (27–36) |
| Birth weight (g) | 1241 ± 135 (1010–1485) |
| Discharge weight (g) | 1916 ± 328 (1320–2745) |
| Age at regain BW (day) | 16 ± 5 (1–28) |
| Length of hospital stay (day) | 44 ± 16 (15–87) |
| Gender | |
| Male | 52 (64.2%) |
| Female | 29 (35.8%) |
| Race | |
| White | 35 (43.2%) |
| African American | 29 (35.8%) |
| Hispanic | 15 (18.5%) |
| Asian | 2 (2.5%) |
N = 81. Data are reported as mean ± SD (range) or Frequency (% of infants)
Table 2.
Accurate standard and estimated mean growth velocities with percentage of absolute difference
|
Growth Velocity to NICU Discharge (g/kg/d) |
|||||
|---|---|---|---|---|---|
| Starting Point | Accurate Standard GV (mean ± SD) | EM GV (mean ± SD) | EM Percentage of Absolute Difference | 2-PM GV (mean ± SD) | 2-PM Percentage of Absolute Difference |
| From Birth: | 9.841 ± 2.419 | 9.842 ± 2.420 | 0.01% ± 0.02% | 9.653 ± 2.333 | 1.76% ± 1.43% |
| From Regain Birth Weight: | 16.061 ± 3.747 | 16.063 ± 3.747 | 0.01% ± 0.01% | 15.809 ± 3.786 | 1.66% ± 1.40% |
Abbreviations: GV, growth velocity; EM, exponential model; 2-PM, 2 point model. Values reported are mean ± SD, percentage of absolute differences between accurate standard and estimated GVs.
Figure 1. Variability in growth for one infant with superimposed Exponential model curve.
• = Actual daily weight; Line represents Exponential model curve for this infant.
Factors Affecting the Accuracy of GV Estimates
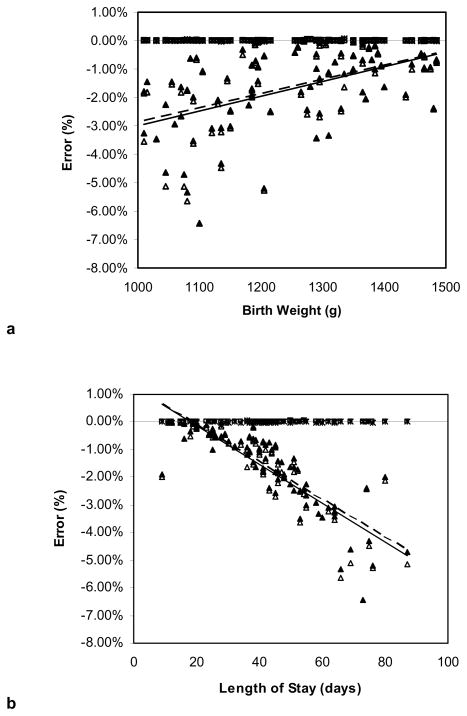
Figure 2 depicts the relationships between BW and length of stay with the magnitude of error, expressed as the percentage of difference between accurate standard and estimated GVs, for each of the models and with both starting points. Lower BW was associated with a greater magnitude of error for the 2-PM from both starting points of birth and regaining BW (rs= −0.49, p<.001; rs= −0.48, p<.001, respectively); whereas the EM was not affected by BW (rs= −0.02, p= 0.86; rs= −0.08, p= 0.50, respectively). Increasing length of stay was highly correlated with an increasing absolute magnitude of error for the 2-PM from both starting points of birth and regaining BW (rs= 0.91, p<.001; rs= 0.91, p<.001, respectively). In contrast, the absolute magnitude of error in the EM from both starting points was unaffected by increasing length of stay (rs= −0.10, p =0.38; rs= 0.05; p=0.68, respectively).
Figure 2. Relationship between percentages of difference for each model studied and birth weight and length of stay.
(a): Percent Error vs. BW. (b): Percent Error vs. Length of stay. Δ = 2-PM Birth, ▲ = 2-PM Regain BW, * = EM Birth, □ = EM Regain BW, — = 2-PM Birth linear trend line, ---- = 2-PM Regain BW linear trend line.
DISCUSSION
This study compares the actual and estimated GVs for larger VLBW infants using two mathematical models that have previously been shown to yield good GV estimates in ELBW infants 18. These findings are consistent with those from our previous study with ELBW infants, in that different mathematical models yield varying estimates of mean GV when compared to actual mean GVs in the same infants. While both models yielded fairly accurate mean estimates, accuracy of the 2-PM was affected by factors commonly seen in VLBW infants such as lower BW and longer hospital stays. In contrast, GV estimates with the EM were unaffected by these factors. The EM accurately estimated a heterogeneous sample of actual GVs from both time intervals (3.1–35.3g/kg/d) and was accurate in individual infants during periods of weight loss. We speculate that the superior performance of the EM is a function of its non-linearity, which provides a better fit for the growth of infants during the neonatal period.
A desirable characteristic of any model used to estimate average GV is ease of application. A non-linear model by Riddle et al 20 was demonstrated to be extremely accurate in predicting growth in NICU infants. This model very closely fit growth patterns from NICU infants with BW 500–2700g using a piecewise function consisting of a parabola from birth until regaining BW and an exponential function after regaining BW. However, this model is more cumbersome for routine use in that it requires estimates of GV and time to regain BW, and uses different complex formulas for each phase of weight change. While it is very useful for creating growth curves, it would be more difficult to use for analyzing growth data in a large sample of infants undergoing different interventions or participating in clinical trials.
From a practical perspective, both the EM and 2-PM are very simple to use, requiring only weight and DOL at two time points. While the 2-PM uses simpler mathematics, the EM provides more accurate estimates of actual GV. We have effectively incorporated the EM into clinical practice in our NICU by automating the EM GV calculation in our electronic medical record. Thus, daily updated GVs for the hospital stay and for the past 7 days is available for each infant. This provides an objective measure of the infant’s growth which we can compare to a desirable growth rate, such as 18g/kg/day 7. Additionally, as nutritional regimens are adjusted, the EM GV provides a measure of efficacy of our interventions. The EM can also be easily applied to research in VLBW infant growth and nutrition by collecting weights at two time points of interest, based on the research question or intervention. However, the findings of this study are limited to NICU stay; the EM has not been tested in later infancy when weight GV slows and may no longer be best fit by an exponential model.
A potential limitation of all two point models is that the model’s accuracy is dependent on the accuracy of the two weight measures used. Therefore, careful review of the weights used in these models is recommended to ensure that the weights accurately reflect the infant’s growth pattern during the time period being studied.
Our previous review of the many methods used to estimate GV revealed the importance of establishing uniform measures of GV for ELBW and larger VLBW infants so that different interventions and outcomes could be compared across studies and clinical settings. These findings and those from our previous analysis 18 suggest the superiority of the EM for estimating GV normalized for weight for all VLBW infants during the NICU stay. The EM is an easy and powerful model that is extremely accurate and unaffected by clinical factors found commonly in VLBW infants, thus allowing its broad application for the clinical management and study of neonatal growth.
Acknowledgments
This study was partially funded by NIH Grant R01-NR010009 and Medela, Inc., McHenry, IL.
FINANCIAL DISCLOSURE: Partially funded by NIH Grant R01-NR010009 and Medela, Inc., McHenry, IL.
Footnotes
CONFLICT OF INTEREST: The exponential formula described in this publication is copyrighted c 2005 by Rush University Medical Center; all rights are reserved. Methods of using the formula are patent pending. Permission is granted to use the exponential formula for research purposes. No commercial use is permitted without a license from Rush University Medical Center.
References
- 1.Ehrenkranz RA, Younes N, Lemons JA, Fanaroff AA, Donovan EF, Wright LL, et al. Longitudinal growth of hospitalized very low birth weight infants. Pediatrics. 1999;104(2):280–9. doi: 10.1542/peds.104.2.280. [DOI] [PubMed] [Google Scholar]
- 2.Radmacher P, Rafail S, Adamkin D. Nutrition and growth in VVLBW infants with and without bronchopulmonary dysplasia. Neonatal Intensive Care. 2004;16(1):22–6. [Google Scholar]
- 3.Steward DK, Pridham KF. Growth patterns of extremely low-birth-weight hospitalized preterm infants. J Obstet Gynecol Neonatal Nurs. 2002;31(1):57–65. doi: 10.1111/j.1552-6909.2002.tb00023.x. [DOI] [PubMed] [Google Scholar]
- 4.Berry MA, Abrahamowicz M, Usher RH. Factors associated with growth of extremely premature infants during initial hospitalization. Pediatrics. 1997;100(4):640–6. [PubMed] [Google Scholar]
- 5.Hay WW., Jr Assessing the effect of disease on nutrition of the preterm infant. Clin Biochem. 1996;29(5):399–417. doi: 10.1016/0009-9120(96)00062-8. [DOI] [PubMed] [Google Scholar]
- 6.Morris BH, Smith KE, Swank PR, Denson SE, Landry SH. Patterns of physical and neurologic development in preterm children. J Perinatol. 2002;22(1):31–6. doi: 10.1038/sj.jp.7210590. [DOI] [PubMed] [Google Scholar]
- 7.Ehrenkranz RA, Dusick AM, Vohr BR, Wright LL, Wrage LA, Poole WK. Growth in the neonatal intensive care unit influences neurodevelopmental and growth outcomes of extremely low birth weight infants. Pediatrics. 2006;117(4):1253–61. doi: 10.1542/peds.2005-1368. [DOI] [PubMed] [Google Scholar]
- 8.Lucas A, Morley R, Cole TJ. Randomised trial of early diet in preterm babies and later intelligence quotient. BMJ. 1998;317(7171):1481–7. doi: 10.1136/bmj.317.7171.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertino E, Coscia A, Mombro M, Boni L, Rossetti G, Fabris C, et al. Postnatal weight increase and growth velocity of very low birthweight infants. Arch Dis Child Fetal Neonatal Ed. 2006;91(5):F349–56. doi: 10.1136/adc.2005.090993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sullivan MC, McGrath MM, Hawes K, Lester BM. Growth trajectories of preterm infants: Birth to 12 years. J Pediatr Health Care. 2008 Mar-Apr;22(2):83–93. doi: 10.1016/j.pedhc.2007.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peterson J, Taylor HG, Minich N, Klein N, Hack M. Subnormal head circumference in very low birth weight children: Neonatal correlates and school-age consequences. Early Hum Dev. 2006;82(5):325–34. doi: 10.1016/j.earlhumdev.2005.09.014. [DOI] [PubMed] [Google Scholar]
- 12.Pauls J, Bauer K, Versmold H. Postnatal body weight curves for infants below 1000 g birth weight receiving early enteral and parenteral nutrition. Eur J Pediatr. 1998;157(5):416–21. doi: 10.1007/s004310050842. [DOI] [PubMed] [Google Scholar]
- 13.Carlson S, Ziegler E. Nutrient intakes and growth of very low birth weight infants. J Perinatol. 1998;18:252–8. [PubMed] [Google Scholar]
- 14.Fenton TR, McMillan DD, Sauve RS. Nutrition and growth analysis of very low birth weight infants. Pediatrics. 1990;86(3):378–83. [PubMed] [Google Scholar]
- 15.Innis SM, Adamkin DH, Hall RT, Kalhan SC, Lair C, Lim M, et al. Docosahexaenoic acid and arachidonic acid enhance growth with no adverse effects in preterm infants fed formula. J Pediatr. 2002;140(5):547–54. doi: 10.1067/mpd.2002.123282. [DOI] [PubMed] [Google Scholar]
- 16.Olsen IE, Richardson DK, Schmid CH, Ausman LM, Dwyer JT. Intersite differences in weight growth velocity of extremely premature infants. Pediatrics. 2002;110(6):1125–32. doi: 10.1542/peds.110.6.1125. [DOI] [PubMed] [Google Scholar]
- 17.Schanler RJ, Shulman RJ, Lau C. Feeding strategies for premature infants: Beneficial outcomes of feeding fortified human milk versus preterm formula. Pediatrics. Jun;103(6 Pt 1):1150–7. doi: 10.1542/peds.103.6.1150. [DOI] [PubMed] [Google Scholar]
- 18.Patel AL, Engstrom JL, Meier PP, Kimura RE. Accuracy of methods for calculating postnatal growth velocity for extremely low birth weight infants. Pediatrics. 2005;116(6):1466–73. doi: 10.1542/peds.2004-1699. [DOI] [PubMed] [Google Scholar]
- 19.Meier PP, Engstrom JL, Mingolelli SS, Miracle DJ, Kiesling S. The rush mothers’ milk club: Breastfeeding interventions for mothers with very-low-birth-weight infants. J Obstet Gynecol Neonatal Nurs. 2004;33(2):164–74. doi: 10.1177/0884217504263280. [DOI] [PubMed] [Google Scholar]
- 20.Riddle WR, DonLevy SC, Qi XF, Giuse DA, Rosenbloom ST. Equations to support predictive automated postnatal growth curves for premature infants. J Perinatol. 2006;26(6):354–8. doi: 10.1038/sj.jp.7211511. [DOI] [PubMed] [Google Scholar]