Abstract
Background:
No circulating markers are routinely used for renal cancer. The objective of this pilot study was to investigate whether conditioned media (CM) from renal cancer cell lines contains potential biomarkers that, when measured in clinical fluids, have diagnostic or prognostic utility.
Methods:
Comparative 2D PAGE profiling of CM from renal cell carcinoma (RCC) and normal renal cultures identified cathepsin D that was subsequently validated in urine samples from 239 patients and healthy and benign disease subjects.
Results:
Urinary cathepsin D was found to be significantly associated with overall (OS) (hazard ratio, HR, 1.33, 95%CI [1.09–1.63], P=0.005) and cancer-specific survival (HR 1.36, 95%CI [1.07–1.74], P=0.013) in RCC patients on univariate analysis. An optimal cut point (211 ng ml−1 μmolCr−1) around which to stratify patients by OS was determined. Five-year OS equal to/above and below this value was 47.0% (95%CI 35.4%, 62.4%) and 60.9% (48.8%, 76.0%), respectively. On multivariable analysis using pre-operative variables, cathepsin D showed some evidence of independent prognostic value for OS (likelihood ratio test P-value=0.056) although requiring further validation in larger patient numbers with sufficient statistical power to determine independent significance.
Conclusion:
These data establish an important proof of principle and show the potential of proteomics-based studies. Cathepsin D may be of value as a pre-operative urinary biomarker for RCC, alone or in combination.
Keywords: renal cell carcinoma, cathepsin D, urine, prognosis, biomarker, proteomics
There are approximately 65 000 new cases of conventional renal cell carcinoma (RCC) in Europe each year, resulting in a substantial economic burden (Ferlay et al, 2007; Gupta et al, 2008). Despite recent advances in our understanding of the underlying biology, there are still no validated circulating biomarkers of RCC, which may be of value in diagnosis, prognosis or monitoring of patients.
Diagnostic markers, obviating the requirement for biopsy, are desirable, given the increased detection of smaller renal masses, of which approximately 20–25% are found to be benign (Schachter et al, 2007). Accurately determining prognosis is important in defining intensity of treatment and follow-up for individual patients. Such efforts have traditionally focused on pathological criteria, based on the surgical specimen (Leibovich et al, 2003; Sorbellini et al, 2005). However, estimates of risk are relatively wide for individual patients (Leibovich et al, 2003; Sorbellini et al, 2005) and some elements such as nuclear grade are subject to intra- and inter-observer variability (Al Aynati et al, 2003). The possibility of determining outcome pre-operatively has also recently been highlighted, with the definition of six pre-operative variables that predict risk of RCC-specific mortality with a high degree of accuracy (Raj et al, 2008; Karakiewicz et al, 2009). Such nomograms may influence patient management in terms of treatment modality, surgical strategy and neoadjuvant treatment using suninib or sorafenib for example.
Proteomic technologies hold great potential for the identification of cancer biomarkers (Koomen et al, 2008). Circulating protein markers, identified in the blood or urine, could provide more objective information and pre-operatively. However, analysis of such fluids for initial biomarker discovery is challenging because of high salt content, very wide dynamic range of protein concentrations and dominance by a small number of proteins present in high concentrations (Hanash et al, 2008). Growth media conditioned by tumour cells in culture can be used to enrich for secreted and shed membrane proteins, which may represent putative circulating markers of disease (Xue et al, 2008). Potential candidates can then be analysed in urine or blood and clinical utility assessed. The aim of this study was to carry out a pilot investigation as to whether this approach would successfully identify potential markers for renal cancer, which could then be validated in patient samples for diagnostic or prognostic use and which could form the basis for more intensive larger-scale studies subsequently.
Materials and methods
Patient samples
Mid-stream urine samples from 149 untreated patients with clear cell RCC (before nephrectomy), 30 patients with benign urological conditions and 60 healthy controls of similar age and sex were used in the study (Table 1). Immediately post voiding, samples were collected, placed on ice and pH adjusted to 7.0. One mini protease inhibitor cocktail tablet (Roche, Burgess Hill, Sussex, UK) was added per 50 ml. The urine was filtered, centrifuged at 2000 g at 4°C for 10 min, aliquotted and stored at −80°C. Samples were collected following ethical approval between May 1999 and June 2007 at St James's University Hospital as part of our prospective sample banking for biomarker studies. All RCC patients except one (biopsy only) subsequently underwent a nephrectomy. Controls were matched for similar length of sample storage and age/gender mix as the patients.
Table 1. Details of all patients included in the study.
| N | % | |
|---|---|---|
| Characteristic | Normal | |
| Total | 60 | 100 |
| Sex | ||
| Male | 38 | 63.3 |
| Female | 22 | 36.7 |
| Age (years) | ||
| Median (range) | 63 (27, 82) | |
|
Benign
|
||
| Total | 30 | 100 |
| Sex | ||
| Male | 19 | 63.3 |
| Female | 11 | 36.7 |
| Age (years) | ||
| Median (range) | 58 (34, 84) | |
| Condition | ||
| Urinary tract infection | 4 | 13 |
| Benign prostatic hypertrophy | 3 | 10 |
| Renal stone | 12 | 40 |
| Cystic disease | 4 | 13 |
| Benign renal tumoura | 6 | 20 |
| Renal atrophy | 1 | 4 |
|
RCC
|
||
| Total | 149 | 100 |
| Sex | ||
| Male | 94 | 63.1 |
| Female | 55 | 36.9 |
| Age (years) | ||
| Median (range) | 61 (37, 85) | |
| pTumour diameter (cm) | ||
| Median (range) | 6 (2.0, 15.5) | |
| CT Tumour diameter (cm) | ||
| Median (range) | 6 (2.0, 21) | |
| Grade | ||
| 1 | 3 | 2.0 |
| 2 | 33 | 22.2 |
| 3 | 73 | 49.0 |
| 4 | 40 | 26.8 |
| Sarcomatoid change | ||
| No | 137 | 91.9 |
| Yes | 12 | 8.1 |
| pT stage | ||
| 1a | 31 | 20.8 |
| 1b | 32 | 21.5 |
| 2 | 14 | 9.4 |
| 3a | 27 | 18.1 |
| 3b | 42 | 28.2 |
| 4 | 3 | 2.0 |
| CT T stage | ||
| 1a | 35 | 27.3 |
| 1b | 38 | 29.7 |
| 2 | 31 | 24.2 |
| 3a | 19 | 14.8 |
| 4 | 5 | 3.9 |
| N stage | ||
| 0 | 132 | 88.6 |
| 1 | 17 | 11.4 |
| M stage | ||
| 0 | 111 | 74.5 |
| 1 | 38 | 25.5 |
| TNM stage | ||
| I | 58 | 38.9 |
| II | 10 | 6.7 |
| III | 42 | 28.2 |
| IV | 39 | 26.2 |
| Symptoms | ||
| Local | 63 | 43.2 |
| Asymptomatic | 49 | 33.6 |
| Systemic | 34 | 23.3 |
| Relapse | ||
| No | 76 | 65.5 |
| Yes | 40 | 34.5 |
| Cancer death | ||
| No | 112 | 75.2 |
| Yes | 37 | 24.8 |
| Death from any cause | ||
| No | 94 | 63.1 |
| Yes | 55 | 36.9 |
Abbreviation: CC=renal cell carcinoma.
3 × oncocytoma, 1 × metanephric adenoma, 1 × cystic nephroma, 1 × inflammatory pseudotumour.
Cell lines and conditioned medium preparation
The human RCC cell lines HTB46, HTB47, HTB49 (ATCC) and TK10 (NCI Frederick Repository, Washington, USA) were grown in RPMI 1640 medium (HTB49-MEM alpha)/10% v/v FCS/2 mM L-glutamine and maintained at 37°C in an humidified incubator with 5% CO2. Ten primary renal cultures (four normal and three matched normal/tumour pairs) from patients with clear cell RCC (grades 2–4; stage III/IV) were generated from nephrectomy samples (normal pole of nephrectomy specimen and areas of tumour, respectively) and characterised by immunocytochemistry to confirm epithelial origin as described earlier (Craven et al, 2006b). For this proof of principle study, the strategy involved comparison by 2D PAGE of conditioned media (CM) from HTB49 with HTB49 cell lysate to characterise proteins enriched in CM, which may represent secreted or shed membrane proteins. HTB49 CM was then compared with a CM pool prepared from four normal primary cultures to further highlight potential tumour/normal differences with prioritisation given to those enriched in CM compared with lysate. It was not possible to use the ideal choice of primary matched pair cell lines for the discovery experiments because of limited culture potential and the volumes of CM needed and this also dictated the use of pooled CM as the comparator.
For collection of CM, cells were grown to 70–80% confluency, washed 3 × with HBSS and media replaced with serum-free culture medium supplemented with insulin–transferrin–sodium selenite (Sigma-Aldrich, Poole, Dorset, UK). After 24 h incubation, which had been shown earlier not to affect cell viability, CM was collected, placed on ice and filtered through a 0.2 μm filter to remove cell debris. After addition of protease inhibitor (Complete, Roche; one tablet per 50 ml), supernatants (200 ml) were concentrated using a Gyrosep 300 stirred cell (Intersep, Wokingham, Berks, UK) pressurised at 4 bar with a 10 kDa MWCO ultrafiltration membrane (Millipore, Watford, Herts, UK) with further concentration to 1 ml using a 10 kDa MWCO Amicon Ultra centrifugal filter device (Millipore). The CM was then buffer exchanged into 2D PAGE lysis buffer [12] and stored at −80°C.
2D PAGE analysis
Samples (30 μg of protein; triplicate) were subjected to isoelectric focusing on 18 cm pH 3–10 NL IPG strips before separation by SDS–PAGE (10% polyacrylamide), silver staining and analysis, all as described earlier (Craven et al, 2006b). Spots upregulated >2-fold within each cell line-normal culture comparison (P<0.05, Student's t-test) were selected for further analysis. For preparative grade gels, 1 mg protein was used and gels were fixed and stained with PlusOne silver stain using a modified protocol compatible with MS (Yan et al, 2000).
Mass spectrometric sequencing
Excised protein spots were digested with trypsin (Craven et al, 2006b). Positive-ion MALDI mass spectra were obtained using an Applied Biosystems 4700 Proteomics Analyser (Applied Biosystems, Manchester, UK) in reflectron mode. Final mass spectra were internally calibrated using tryptic autoproteolysis products or using an internal spike (angiotensin, 1296.6853). Three to ten of the strongest peaks (S : N >50) in each MS spectrum were selected for CID-MS/MS. The default calibration was used for MS/MS spectra, which were baseline subtracted and smoothed with peak detection using a minimum S : N of 3 or 5, local noise window of 50 m/z and minimum peak width of 2.9 bins or as described earlier (Craven et al, 2006a). Batch-acquired MS and MS/MS spectral data were submitted to a combined peptide mass fingerprint and MS/MS ion search through the Applied Biosystems GPS Explorer software interface (version 3.5) to Mascot (Matrix Science Ltd, version 2.2.03, London, UK) with criteria as described earlier (Vasudev et al, 2008).
Validation of results by western blotting
Samples of CM (5 μg) were analysed by western blotting using 10% acrylamide gels (Craven et al, 2006a). A monoclonal antibody to cathepsin D (clone 49, BD Biosciences (Oxford, UK); 12.5 ng ml−1) was used and detection performed using mouse EnVision HRP-conjugated antibody (Dako, Ely, Cambridgeshire, UK; 1 : 200). In the absence of a reliable loading control for CM, parallel Coomassie brilliant blue stained gels were used to check for equal loading.
Immunoassay for cathepsin D
Urine was thawed, vortexed and microfuged briefly. An in-house sandwich ELISA for cathepsin D was developed and validated. All wash and dilution steps used solution WB (2.5 mM NaH2PO4, 7.5 mM Na2HPO4, 500 mM NaCl/0.1% (v/v) Tween 20, pH7.2) unless otherwise indicated. Wells (96-well Nunc Maxisorp plates, VWR, Lutterworth, Leicestershire, UK) were coated with 100 μl of monoclonal anti-cathepsin D antibody (5 μg ml−1; Clone 49) in sodium phosphate buffer (2.5 mM NaH2PO4, 7.5 mM Na2HPO4, 0.145 M NaCl, pH 7.2) overnight at 4°C and washed 3 × . For the standard curve, human cathepsin D (Sigma-Aldrich) was prepared in doubling dilutions from 8000 ng ml−1 to 500 ng ml−1. Diluted samples (20 × ) and standards (100 μl) were added to duplicate wells and incubated at RT for 2 h. After washing 5 × , 100 μl of rabbit anti-cathepsin D antibody (10.4 μg ml−1; Abcam, Cambridge, UK) in WB/10% (w/v) milk was added to each well and incubated at RT for 2 h. After washing, 100 μl of biotinylated goat anti-rabbit antibody (0.19 μg ml−1; Dako) in WB/1% (v/v) mouse serum was added, plates incubated for 1 h, washed and 100 μl of HRP-conjugated streptavidin (0.3 μg ml−1; Dako) added to each well. After 30 min and a wash step, 100 μl of TMB substrate (Sigma-Aldrich) was added and colour development stopped after 20 min by addition of 100 μl of 0.5 M sulphuric acid per well and absorbance read at 450 nm.
Samples were analysed blind, randomised throughout and two QC samples were included on all plates. Mean intra-assay CVs for duplicate samples was 12.1% (s.d. 12.4) and mean inter-assay CVs for the QC samples over five consecutive days was 12.8%. Linearity was shown on serial dilutions of four samples. Mean recovery on four urines was 109.3% (s.d. 22.8) for 1500 ng ml−1 spikes and 112.1% (s.d. 13.4) for 3000 ng ml−1 spikes.
Statistical analysis
Study design and analysis conformed to ReMARK and STARD guidelines (Bossuyt et al, 2003; McShane et al, 2005). Sample size was determined for the test of diagnostic potential being powered to detect a fair diagnostic ability of the marker (power 1-β=0.90, significance level of α=0.05), defined as an AUC of 0.7, such that a minimum of 33 patients in each group were required (Obuchowski 2000). Receiver operating characteristic (ROC) curve analysis was performed to test the diagnostic ability of each marker (Obuchowski 2000). Prognostic value was evaluated as a secondary investigation where DFS (defined as date of recurrence or death from any cause), OS and CSS were examined relative to nephrectomy date. Patients who were still alive or who were lost to follow-up were censored, as were patients who died from causes other than RCC in the CSS analysis. To assess the association of cathepsin D with known prognostic factors, non-parametric methods of testing for association (Kruskal–Wallis and Wilcoxon–Mann–Whitney tests), trend (Cuzick's Wicoxon-like test) and correlation (Spearman's rho) were used where appropriate. Similarly, to assess prognostic ability and the characteristics of the study population with respect to known prognostic factors, the Kaplan–Meier estimate of the survival function, the log rank test and Cox proportional hazards regression were used. These methods were undertaken using Stata 9.2 (StataCorp, College Station, TX, USA). To identify the optimum cut point of cathepsin D for prognosis, an ROC(t) curve analysis was undertaken (Heagerty et al, 2000).
Results
Comparative analysis of CM
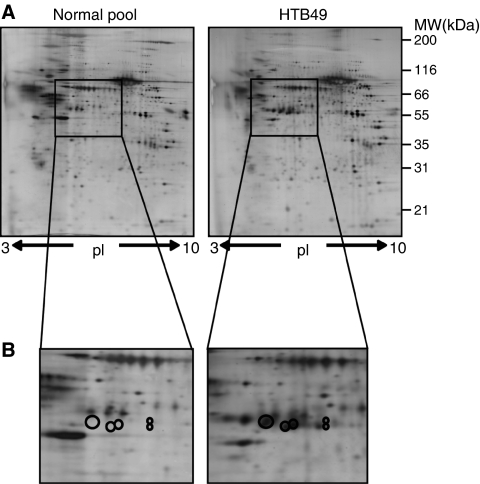
One hundred and thirty-three (13%) protein spots were enriched in HTB49 CM in comparison to whole cell lysate, with 27 subsequently identified and accounting for 10 different proteins (Table 2), all of which were predicted to undergo secretion through either classical or non-classical routes (SecretomeP and SignalP) (Bendtsen et al, 2004a, 2004b). Gel images and detailed mass spectrometry data of these and a further 40 proteins included for reference purposes are provided as Supplementary data (Supplementary Table 1; Supplementary Figure 1). Comparison of HTB49-derived CM with that from primary normal renal cultures showed 61 (6%) protein spots upregulated in the HTB49 sample. After prioritisation on the basis of enrichment in CM compared with lysate (Table 2), biological relevance, antibody availability and novelty, cathepsin D (Figure 1) was taken forward.
Table 2. HTB49 CM spot identities.
| Name | Accession no. | No of spots | No. of matched peaks | No. of unmatched peaks | % Coverage | MASCOT Score | MSMS | Status |
|---|---|---|---|---|---|---|---|---|
| IGFBP-rP1 | Q16270 | 1 | 14 | 66 | 45.0 | 120 | SiP | |
| Reticulocalbin 1 precursor | Q15293 | 1 | 9 | 42 | 42.0 | 80 | SiP† | |
| SPARC | P09486 | 1 | 9 | 42 | 32.0 | 70 | SiP† | |
| Vimentin | P08670 | 1 | 35 | 67 | 71.0 | 291 | SeP | |
| PAI-1 | P05121 | 4 | 18 | 30 | 49.9 | 157 | 2 | SiP |
| Transferrin | P02787 | 8 | 13 | 27 | 30.0 | 105 | ||
| Cathepsin D | P07339 | 5 | 9 | 28 | 32.1 | 83 | SiP† | |
| Nucleobindin 1 | Q02818 | 1 | 22 | 56 | 54.0 | 172 | SiP | |
| BIGH3 | Q15582 | 5 | 20 | 33 | 41.5 | 166 | 2 | SiP |
| Complement C3 | P01024 | 1 | 20 | 32 | 23.8 | 138 | SiP |
From HTB49 CM, 27 spots (10 proteins) upregulated vs whole cell lysate were identified. Where a protein was found in more than one spot, a representative example of scores is shown. Confirmation of peptide mass finger printing (PMF) by MS/MS was undertaken for some spots and this is indicated by the number of significant peptides found. Proteins predicted to contain a signal sequence using SignalP 3.0 are denoted SiP and those predicted to undergo non-classical secretion using SecretomeP are denoted SeP. In the Status column, proteins marked † indicate those proteins upregulated in comparison to normal conditioned media (CM) (further proteins identified are listed in Supplementary Table 1).
Figure 1.
Conditioned media analysed by 2D PAGE. (A) A measure of 30 μg of HTB49 and pooled normal renal culture CM were separated on 18 cm pI 3–10 IPG strips in the first dimension. Each sample was run and analysed in triplicate and representative gels are shown. (B) The location of cathepsin D as a cluster of spots is shown, which was enriched in CM compared with lysate and increased in RCC CM compared with normal renal primary CM.
Western blot validation
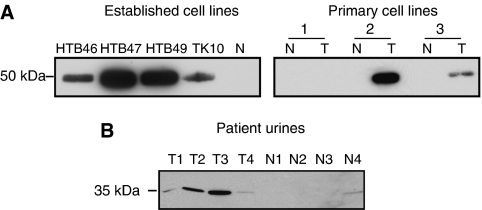
Western blotting confirmed the presence of pro-cathepsin D (50 kDa) in CM from 4/4 established RCC lines, but not the normal CM. In CM from the three matched primary line pairs, cathepsin D was detected in only the tumour samples of two pairs and was absent completely in a third pair (Figure 2A; Supplementary Figure 2). Before immunoassay development, presence of mature cathepsin D (34 kDa) in urine was confirmed in 4/4 samples from RCC patients and only 1/4 healthy control samples (Figure 2B).
Figure 2.
Western blot validation of cathepsin D. (A) Samples of CM (5 μg load in each case) were probed for cathepsin D. Expression was seen in all established cell lines examined but absent in one normal sample included for comparison purposes. Increased expression by tumour cultures in two out of three primary tumour (T)/normal (N) matched pairs was also apparent. Parallel Coomassie staining was performed for loading control purposes. (B) Urine from four healthy controls and four patients with RCC were probed for cathepsin D. 15 μl of urine was loaded in each case. Uncropped blots are presented in Supplementary Figure 2.
Immunoassay of urinary cathepsin D
All results were normalised by urinary creatinine. Sample storage time varied from 2 to 99 months but comparison of a set of 30 ‘old’ and 30 ‘new’ (average 63.4 months vs 7.1 months, respectively) urines from healthy controls found no significant differences. Similar comparisons with patient samples were not feasible because of the confounding background effects of varying disease severity in such a heterogeneous group and will require future longitudinal stability studies.
Diagnostic utility
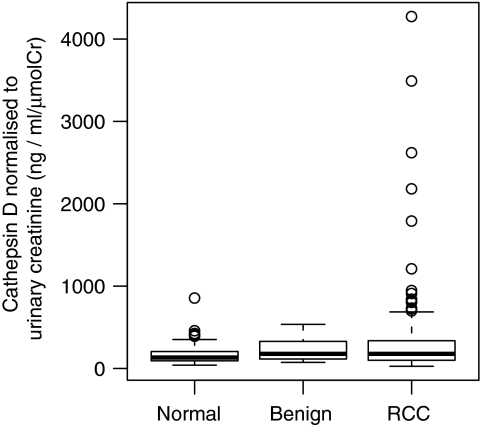
A wider range of cathepsin D concentrations were seen in the RCC group but showed only weak evidence of a significant difference between groups (P=0.052 using the Kruskal–Wallis test; Figure 3; Table 3). ROC analysis showed no diagnostic utility with area under the curve being 0.5612, 90% confidence interval (CI) (0.505–0.615) when comparing RCC patients vs controls (benign and normal).
Figure 3.
Box-plot of urinary cathepsin D normalised to creatinine. The box extends to the interquartile range (IQR), the line transecting this box representing the median. The bars extend to 1.5 × the IQR and the dots represent outliers that are beyond these limits.
Table 3. Association of patient and tumour characteristics with urinary cathepsin D by univariate analysis.
| Cathepsin D concentration | |||
|---|---|---|---|
| Status | Median (range) (ng ml−1 μmolCr−1) | P -value (association) | P -value (trend) |
| Normal | 133.2 (40.2, 856.5) | 0.052a | |
| Benign | 177.6 (73.9, 536.0) | ||
| RCC | 178.0 (27.0, 4274.0) | ||
| Control | 144.3 (40.2, 856.5) | 0.113b | |
| Sex | 0.188 | ||
| Male | 145.5 (27.0, 4274.0) | ||
| Female | 200.0 (40.2, 1209.0) | ||
| Agec | 0.103c | 0.212 | |
| Grade | 0.854 | 0.577 | |
| 1or2 | 195.0 (27.0, 4274.0) | ||
| 3 | 178.0 (54.0, 3492.0) | ||
| 4 | 172.0 (41.0, 2180.0) | ||
| Sarcomatoid change | 0.032 | ||
| No | 171.0 (27.0,1789.0) | ||
| Yes | 380.0 (73.0,2180.0) | ||
| pT stage | 0.254 | 0.080 | |
| 1 | 172.0 (27.0, 4274.0) | ||
| 2 | 175.0 (70.0, 471.0) | ||
| 3 | 204.5 (48.0, 3492.0) | ||
| 4 | 836.0 (86.0, 1789.0) | ||
| CT T stage | 0.159 | 0.086 | |
| 1 | 161.0 (27.0, 4274.0) | ||
| 2 | 182.0 (27.0, 2180.0) | ||
| 3 | 325.0 (48.0, 912.0) | ||
| 4 | 139.0 (86.0, 802.0) | ||
| N stage | 0.001 | ||
| 0 | 165.0 (27.0, 4274.0) | ||
| 1/2 | 362.0 (60.0, 2180.0) | ||
| M stage | 0.034 | ||
| 0 | 169.0 (27.0, 4274.0) | ||
| 1 | 251.0 (60.0, 1789.0) | ||
| Overall stage | 0.216 | 0.043 | |
| I | 165.0 (27.0,4274.0) | ||
| II | 175.0 (70.0,376.0) | ||
| III | 164.5 (48.0,3492.0) | ||
| IV | 224.0 (60.0,1789.0) | ||
| Symptoms | 0.368 | 0.190 | |
| Local | 169.0 (27.0,4274.0) | ||
| Asymptomatic | 172.0 (33.0,3492.0) | ||
| Systemic | 226.5 (63.0,912.0) | ||
| Tumour size c | |||
| CT | 0.143c | 0.109 | |
| pathology | 0.115c | 0.173 | |
Refers to test comparing normal, benign and renal cell carcinoma (RCC) group.
Refers to test comparing control (normal and benign) with RCC group.
Spearman's rank correlation coefficient.
Age, sex and tumour-related factors relate to RCC group only. P-value (association) is result of test comparing distributions in groups under null hypothesis of them being identical and P-value (trend) is the result of a test under the null hypothesis of no trend in naturally ordinal groups.
Association with prognosis
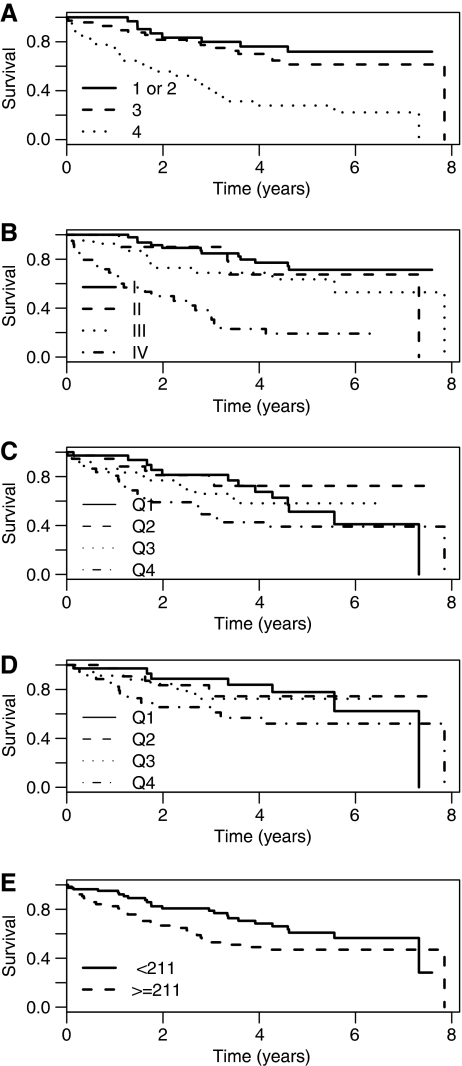
Patients with nodal/metastatic disease or sarcomatoid change had significantly higher median urinary cathepsin D levels (Table 3). The median length of follow-up from nephrectomy of those patients still alive was 34 months (range 0–94 months). The representative nature of the population was first confirmed by association of survival with grade and stage (P=0.001 for both; Figure 4A and B). On univariate analysis there was evidence of an association between overall survival and cathepsin D (hazard ratio (HR) 1.33, 95%CI [1.09–1.63], P=0.005) that is for every rise of 1 unit on the log 2 scale (doubling in concentration of cathepsin D), the hazard of dying increased by 1.3-fold (Figure 4C). There was no evidence of the proportional hazards assumption being violated using the test of Grambsch and Therneau (P=0.208). There was also evidence of an association between CSS and cathepsin D (HR 1.36, 95%CI [1.07–1.74], P=0.013) (Figure 4D), but not with DFS (HR 1.19, 95%CI [0.93–1.52], P=0.168) – although the estimated HR is similar.
Figure 4.
Grade, stage, urinary cathepsin D and survival. Overall survival curves based on (A) tumour grade and (B) stage validate our patient population. (C) Overall and (D) cancer-specific survival, respectively, by urinary cathepsin D concentration (normalised for creatinine) considered as quartiles. (E) Overall survival based on the optimal cut point of 211 ng ml−1 μmolCr−1 cathepsin D, determined by time-dependent ROC analysis.
Using time-dependent ROC curves, the largest AUC(t) was observed for a cut at 18 months (AUC=0.712), when comparing patients who had had an event at 18 months with those who had not. Examining the points of ROC curve gave a best cut-off in terms of sensitivity and specificity for cathepsin D of 211 ng ml−1 μmolCr−1. The 1-year OS estimates (95%CI) for < and ⩾to this cut-off were 95.2% (90.6%, 99.9%) and 80.9% (71.7%, 91.2%), respectively, with corresponding 5-year estimates of 60.9% (48.8%, 76.0%) and 47.0% (35.4%, 62.4%) (Figure 4E). Only 4 patients received adjuvant therapy; 37 patients received IFN and/or IL-2-based treatment in the metastatic setting; 2 patients received sunitinib. However, no difference was observed in the treatment patients received when considered by the cut point for cathepsin D.
To examine further the utility of urinary cathepsin D as a pre-operative marker, the association of cathepsin D with the variables used in the pre-operative nomogram developed by Karakiewicz et al (n=2474) (Karakiewicz et al, 2009), that is CT tumour size, CT T stage and symptoms at presentation was also examined (Table 3). Some evidence of a significant association between increasing cathepsin D concentration and CT T stage (P=0.086) was observed when using the non-parametric trend test (confirmed by examining medians in Table 3).
On multivariable analysis, using these pre-operative variables and considering OS, cathepsin D showed some evidence of independent prognostic value (likelihood ratio test (LRT) P-value=0.056; Table 4). No evidence was observed for association of cathepsin D with CSS (LRT P=0.291) or DFS (LRT P=0.103). Metastatic disease, sex, and CT T stage showed independently prognostic value (P<0.050), and for other variables HRs were within the 95% CIs reported earlier in a much larger dataset (Karakiewicz et al, 2009). The power to show independent prognostic value in this pilot study is low as there are a large number of variables included in the model (nine when considering all levels in categorical variables) and simulation experiments based on this model show that 200 patients would be required at observed event rates to attain a power of approximately 50% and 500 patients to attain a power of approximately 90% with similar HRs to those observed at standard significance levels (Cairns et al, in preparation). Hence, a larger study would be required to show strong evidence of an independent prognostic association with cathepsin D.
Table 4. Univariate and multivariable pre-operative prognostic modelling results for all RCC patients with cathepsin D concentration for OS.
|
Univariate analysis
|
Multivariable analysis
|
|||||
|---|---|---|---|---|---|---|
| Characteristic | HR | 95% CI | P- value | HR | 95% CI | P- value |
| Cath-D (ng ml−1 μmolCr−1) | 1.360 | (1.069, 1.738) | 0.005 | 1.302 | (1.000, 1.696) | 0.050 |
| Age (yr) | 1.007 | (0.984, 1.034) | 0.607 | 1.004 | (0.969, 1.041) | 0.828 |
| Sex | ||||||
| M vs F | 1.655 | (0.922, 2.971) | 0.091 | 2.656 | (1.057, 6.675) | 0.038 |
| CT T stage | ||||||
| T2 vs T1 | 1.098 | (0.495, 2.436) | 0.819 | 0.525 | (0.104, 2.645) | 0.435 |
| T3/T4 vs T1 | 6.315 | (2.139, 18.642) | 0.001 | 5.450 | (1.004, 29.575) | 0.049 |
| CT max. tumour diameter (cm) | 1.155 | (1.056, 1.263) | 0.002 | 1.041 | (0.821, 1.320) | 0.739 |
| M stage | ||||||
| M1 vs M0 | 4.623 | (2.657, 8.047) | 0.001 | 3.154 | (1.178, 8.449) | 0.022 |
| Symptoms | ||||||
| Local vs asymptomatic | 2.212 | (1.086, 4.505) | 0.029 | 1.230 | (0.470, 3.220) | 0.674 |
| Systemic vs asymptomatic | 4.127 | (2.008, 8.486) | 0.001 | 1.527 | (0.498, 4.683) | 0.459 |
Abbreviations: CI=confidence interval; HR=hazard ratio.
Discussion
In this pilot study, we have shown that proteomic analysis of CM from renal cancer cell lines, as described in other diseases (Xue et al, 2008), may result in the identification of potential biomarkers such as cathepsin D. Furthermore, although samples from 149 patients with RCC were included, this represents a relatively small validation study with only moderate statistical power for a potential marker with this magnitude of HR, and yet we were able to show the novel finding of an association between urinary cathepsin D in RCC and survival, which has potential clinical application.
Cathepsin D is a lysosomal protease, synthesised as a pre-pro-enzyme. Removal of the signal peptide yields 52 kDa pro-cathepsin D, which undergoes N-glycosylation and is then targeted to the lysosome to yield a mature two-chain enzyme consisting of a light (14 kDa) amino-terminal domain and a heavy (34 kDa) carboxyl-terminal domain. The greater amounts of pro-cathepsin D present in RCC CM do not reflect increased transcription (data not shown) but may be translation-related or occur from re-routing of the protein. Such aberrant secretion is present in many cancer types (Liaudet-Coopman et al, 2006), in a number of different glycoforms (Capony et al, 1989), which may account for the cluster of spots represented by the protein in this study. Pro-cathepsin D is known to function as a mitogen, acting entirely independently of its proteolytic activity (Vetvicka et al, 2000; Vashishta et al, 2006), although the mechanism mediating these effects is yet to be understood. On the basis of characterisation of the reactivity of the antibodies used in our ELISA, it is likely that the assay measures both precursor and mature forms.
Our current findings are thus biologically plausible. Cathepsin D levels were associated with established features of tumour aggressiveness, such as positive lymph nodes, sarcomatoid change and metastatic disease at presentation as well as CT-defined tumour and overall stage. Increased tissue expression of cathepsin D has been correlated with poorer outcome in a number of other cancers, although inconsistently (Harris et al, 2007). In RCC, high expression was associated with a significantly improved OS compared with low expressers (82 vs 53 months; P=0.03) with independent prognostic significance (Merseburger et al, 2005). Tissue cathepsin D did not correlate with tumour characteristics, unlike urinary cathepsin D in our study. These findings seem to contradict our own, but intra-cellular levels of cathepsin D may bear little correlation to the proportion/form of cathepsin D that is externalised. Indeed, unlike tissue, serum cathepsin D levels do not differ between RCC patients and healthy controls (Merseburger et al, 2007). Similarly, no diagnostic utility for urinary cathepsin D was found in this study. The source of cathepsin D in healthy control urine is uncertain, but is not thought to originate from serum because differences in glycoforms are apparent (Zuhlsdorf et al, 1983) and may reflect release from urothelial cells on turnover.
Urine is accessible but its composition is influenced by many factors such as sex, age, diet, concomitant renal disease and medications, potentially affecting the interpretation of any given test (Barratt and Topham, 2007). However, urinary cancer markers are available and approved by the FDA as exemplified by nuclear matrix protein 22 for bladder cancer. This study illustrates the principle of using CM as an initial source for biomarker discovery, with validation subsequently in biological fluids such as urine. Future work will include increasing the number of cell lines profiled to allow systematic prioritisation of candidate markers based on conserved changes, and increasing the depth of coverage to find potentially more discriminant markers. The potential utility of cathepsin D as a pre-operative marker needs to be explored further using a much larger sample bank to allow a sufficiently powered study for determination of independent prognostic ability and if positive, the inclusion in prognostic models examined. In addition, the relationship between urinary and tissue levels of cathepsin D and the various forms will be investigated with our own work with cell lines indicating a VHL-based regulation of expression (data not shown).
Acknowledgments
The funding of Cancer Research UK, the support of the Urology, Oncology and Pathology Departments at St James's University Hospital and the consent of patients to participate in our studies are gratefully acknowledged. Protein sequencing was carried out by Nick Totty and Sarah Hanrahan, Cancer Research UK, London and by Jerry Thomas of the University of York.
Footnotes
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary Material
References
- Al Aynati M, Chen V, Salama S, Shuhaibar H, Treleaven D, Vincic L (2003) Interobserver and intraobserver variability using the Fuhrman grading system for renal cell carcinoma. Arch Pathol Lab Med 127: 593–596 [DOI] [PubMed] [Google Scholar]
- Barratt J, Topham P (2007) Urine proteomics: the present and future of measuring urinary protein components in disease. CMAJ 177: 361–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendtsen JD, Jensen LJ, Blom N, von Heijne G, Brunak S (2004a) Feature-based prediction of non-classical and leaderless protein secretion. Protein Eng Des Sel 17: 349–356 [DOI] [PubMed] [Google Scholar]
- Bendtsen JD, Nielsen H, von Heijne G, Brunak S (2004b) Improved prediction of signal peptides: SignalP 3.0. J Mol Biol 340: 783–795 [DOI] [PubMed] [Google Scholar]
- Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC (2003) Toward complete and accurate reporting of studies of diagnostic accuracy. The STARD initiative. Am J Clin Pathol 119: 18–22 [DOI] [PubMed] [Google Scholar]
- Capony F, Rougeot C, Montcourrier P, Cavailles V, Salazar G, Rochefort H (1989) Increased secretion, altered processing, and glycosylation of pro-cathepsin D in human mammary cancer cells. Cancer Res 49: 3904–3909 [PubMed] [Google Scholar]
- Craven RA, Hanrahan S, Totty N, Harnden P, Stanley AJ, Maher ER, Harris AL, Trimble WS, Selby PJ, Banks RE (2006a) Proteomic identification of a role for the von Hippel Lindau tumour suppressor in changes in the expression of mitochondrial proteins and septin 2 in renal cell carcinoma. Proteomics 6: 3880–3893 [DOI] [PubMed] [Google Scholar]
- Craven RA, Stanley AJ, Hanrahan S, Dods J, Unwin R, Totty N, Harnden P, Eardley I, Selby PJ, Banks RE (2006b) Proteomic analysis of primary cell lines identifies protein changes present in renal cell carcinoma. Proteomics 6: 2853–2864 [DOI] [PubMed] [Google Scholar]
- Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, Boyle P (2007) Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol 18: 581–592 [DOI] [PubMed] [Google Scholar]
- Gupta K, Miller JD, Li JZ, Russell MW, Charbonneau C (2008) Epidemiologic and socioeconomic burden of metastatic renal cell carcinoma (mRCC): a literature review. Cancer Treat Rev 34: 193–205 [DOI] [PubMed] [Google Scholar]
- Hanash SM, Pitteri SJ, Faca V (2008) Mining the plasma proteome for cancer biomarkers. Nature 452: 571–579 [DOI] [PubMed] [Google Scholar]
- Harris L, Fritsche H, Mennel R, Norton L, Ravdin P, Taube S, Somerfield MR, Hayes DF, Bast Jr RC (2007) American Society of Clinical Oncology 2007 update of recommendations for the use of tumor markers in breast cancer. J Clin Oncol 25: 5287–5312 [DOI] [PubMed] [Google Scholar]
- Heagerty PJ, Lumley T, Pepe MS (2000) Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 56: 337–344 [DOI] [PubMed] [Google Scholar]
- Karakiewicz PI, Suardi N, Capitanio U, Jeldres C, Ficarra V, Cindolo L, De La TA, Tostain J, Mulders PF, Bensalah K, Artibani W, Salomon L, Zigeuner R, Valeri A, Descotes JL, Rambeaud JJ, Mejean A, Montorsi F, Bertini R, Patard JJ (2009) A preoperative prognostic model for patients treated with nephrectomy for renal cell carcinoma. Eur Urol 55: 287–295 [DOI] [PubMed] [Google Scholar]
- Koomen JM, Haura EB, Bepler G, Sutphen R, Remily-Wood ER, Benson K, Hussein M, Hazlehurst LA, Yeatman TJ, Hildreth LT, Sellers TA, Jacobsen PB, Fenstermacher DA, Dalton WS (2008) Proteomic contributions to personalized cancer care. Mol Cell Proteomics 7: 1780–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibovich BC, Blute ML, Cheville JC, Lohse CM, Frank I, Kwon ED, Weaver AL, Parker AS, Zincke H (2003) Prediction of progression after radical nephrectomy for patients with clear cell renal cell carcinoma: a stratification tool for prospective clinical trials. Cancer 97: 1663–1671 [DOI] [PubMed] [Google Scholar]
- Liaudet-Coopman E, Beaujouin M, Derocq D, Garcia M, Glondu-Lassis M, Laurent-Matha V, Prebois C, Rochefort H, Vignon F (2006) Cathepsin D: newly discovered functions of a long-standing aspartic protease in cancer and apoptosis. Cancer Lett 237: 167–179 [DOI] [PubMed] [Google Scholar]
- McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2005) REporting recommendations for tumour MARKer prognostic studies (REMARK). Br J Cancer 93: 387–391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merseburger AS, Hennenlotter J, Simon P, Ohneseit PA, Kuehs U, Kruck S, Koch E, Vogel U, Stenzl A, Kuczyk MA (2005) Cathepsin D expression in renal cell cancer-clinical implications. Eur Urol 48: 519–526 [DOI] [PubMed] [Google Scholar]
- Merseburger AS, Hennenlotter J, Stenzl A, Beger G, Rinnab L, Kuczyk MA, Kuefer R (2007) Cathepsin D serum levels are not a valid serum marker in renal cell carcinoma. Urol Int 79: 41–43 [DOI] [PubMed] [Google Scholar]
- Obuchowski NA (2000) Sample size tables for receiver operating characteristic studies. AJR Am J Roentgenol 175: 603–608 [DOI] [PubMed] [Google Scholar]
- Raj GV, Thompson RH, Leibovich BC, Blute ML, Russo P, Kattan MW (2008) Preoperative nomogram predicting 12-year probability of metastatic renal cancer. J Urol 179: 2146–2151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schachter LR, Cookson MS, Chang SS, Smith Jr JA, Dietrich MS, Jayaram G, Herrell SD (2007) Second prize: frequency of benign renal cortical tumors and histologic subtypes based on size in a contemporary series: what to tell our patients. J Endourol 21: 819–823 [DOI] [PubMed] [Google Scholar]
- Sorbellini M, Kattan MW, Snyder ME, Reuter V, Motzer R, Goetzl M, McKiernan J, Russo P (2005) A postoperative prognostic nomogram predicting recurrence for patients with conventional clear cell renal cell carcinoma. J Urol 173: 48–51 [DOI] [PubMed] [Google Scholar]
- Vashishta A, Ohri SS, Proctor M, Fusek M, Vetvicka V (2006) Role of activation peptide of procathepsin D in proliferation and invasion of lung cancer cells. Anticancer Res 26: 4163–4170 [PubMed] [Google Scholar]
- Vasudev NS, Ferguson RE, Cairns DA, Stanley AJ, Selby PJ, Banks RE (2008) Serum biomarker discovery in renal cancer using 2D-E and pre-fractionation by immunodepletion and isoelectric focusing: increasing coverage or more of the same? Proteomics 8: 5074–5085 [DOI] [PubMed] [Google Scholar]
- Vetvicka V, Vetvickova J, Fusek M (2000) Role of procathepsin D activation peptide in prostate cancer growth. Prostate 44: 1–7 [DOI] [PubMed] [Google Scholar]
- Xue H, Lu B, Lai M (2008) The cancer secretome: a reservoir of biomarkers. J Transl Med 6: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan JX, Wait R, Berkelman T, Harry RA, Westbrook JA, Wheeler CH, Dunn MJ (2000) A modified silver staining protocol for visualization of proteins compatible with matrix-assisted laser desorption/ionization and electrospray ionization-mass spectrometry. Electrophoresis 21: 3666–3672 [DOI] [PubMed] [Google Scholar]
- Zuhlsdorf M, Imort M, Hasilik A, von Figura K (1983) Molecular forms of beta-hexosaminidase and cathepsin D in serum and urine of healthy subjects and patients with elevated activity of lysosomal enzymes. Biochem J 213: 733–740 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.