Abstract
OBJECTIVE
To examine the association between single nucleotide polymorphisms (SNPs) in the engulfment and cell motility 1 (ELMO1) gene, a locus previously shown to be associated with diabetic nephropathy in two ethnically distinct type 2 diabetic populations, and the risk of nephropathy in type 1 diabetes.
RESEARCH DESIGN AND METHODS
Genotypic data from a genome-wide association scan (GWAS) of the Genetics of Kidneys in Diabetes (GoKinD) study collection were analyzed for associations across the ELMO1 locus. In total, genetic associations were assessed using 118 SNPs and 1,705 individuals of European ancestry with type 1 diabetes (885 normoalbuminuric control subjects and 820 advanced diabetic nephropathy case subjects).
RESULTS
The strongest associations in ELMO1 occurred at rs11769038 (odds ratio [OR] 1.24; P = 1.7 × 10−3) and rs1882080 (OR 1.23; P = 3.2 × 10−3) located in intron 16. Two additional SNPs, located in introns 18 and 20, respectively, were also associated with diabetic nephropathy. No evidence of association for variants previously reported in type 2 diabetes was observed in our collection.
CONCLUSIONS
Using GWAS data from the GoKinD collection, we comprehensively examined evidence of association across the ELMO1 locus. Our investigation marks the third report of associations in ELMO1 with diabetic nephropathy, further establishing its role in the susceptibility of this disease. There is evidence of allelic heterogeneity, contributed by the diverse genetic backgrounds of the different ethnic groups examined. Further investigation of SNPs at this locus is necessary to fully understand the commonality of these associations and the mechanism(s) underlying their role in diabetic nephropathy.
Diabetic nephropathy is a major late complication of diabetes that affects ∼30–40% of all patients with either type 1 or type 2 diabetes and continues to be the leading contributor to end-stage renal disease (ESRD) in the U.S. (1–3). In both type 1 and type 2 diabetes, diabetic nephropathy has been shown to cluster in families (4–8). Despite its known familial aggregation and intense effort to determine the genetic components that underlie its risk, including both candidate gene investigations and genome-wide linkage scans, no major gene that contributes to its susceptibility has yet been identified (9).
Variants in the engulfment and cell motility 1 (ELMO1) gene, located on chromosome 7p, have previously been shown to be associated with diabetic nephropathy in Japanese patients with type 2 diabetes (10). Subsequent functional studies demonstrated increased expression of ELMO1 in the presence of high glucose. In support of a potential role in the pathogenesis of diabetic nephropathy, overexpression of ELMO1 inhibited cell adhesion while promoting excess transcription growth factor-β, collagen type 1, fibronectin, and integrin-linked kinase expression (10,11). Linkage of ESRD in type 2 diabetes has been shown with the 7p region in African Americans (12). Strong support for linkage with variation in glomerular filtration rate has also been reported at this same region in Caucasians (13). Leak et al. (14) recently examined genetic variants across ELMO1 in two large African American cohorts with type 2 diabetes and ESRD, and, in support of its potential role in the susceptibility of diabetic nephropathy, variants in intron 13 were found to be associated with disease.
We recently performed a genome-wide association scan (GWAS) for diabetic nephropathy susceptibility genes in type 1 diabetes and reported the identification of several novel susceptibility loci from the initial analysis of these data (15). In addition to uncovering associations at novel loci across the genome, these data also allow for the comprehensive examination of specific candidate disease loci. In this report, we investigated the role of 118 variations in ELMO1 on the risk of diabetic nephropathy in 1,705 Caucasian patients with type 1 diabetes using genotypic data from this GWAS.
RESEARCH DESIGN AND METHODS
A detailed description of the Genetics of Kidneys in Diabetes (GoKinD) study collection has been published previously (16). Briefly, subjects for the GoKinD collection were recruited through two centers: the George Washington University (GWU) Biostatistics Center and the Section of Genetics and Epidemiology at the Joslin Diabetes Center (JDC). Subjects enrolled in GoKinD by either recruitment center had type 1 diabetes diagnosed before age 31 years, began insulin treatment within 1 year of diagnosis, and were between 18 and 59 years of age at the time of enrollment. Case subjects with advanced diabetic nephropathy had either persistent proteinuria, defined by a urinary albumin-to-creatinine ratio (ACR) ≥300 μg/mg in two of the last three measurements taken at least 1 month apart, or ESRD (dialysis or renal transplant). Control subjects had type 1 diabetes for at least 15 years and normoalbuminuria, defined by an ACR <20 μg/mg in two of the last three measurements taken at least 1 month apart (if a third measurement was required, a value <40 μg/mg was necessary for inclusion), without ever having been treated with ACE inhibitors or angiotensin receptor blockers and not being treated with antihypertensive medication at the time of recruitment into the study. A total of 1,705 individuals (885 control subjects and 820 advanced diabetic nephropathy case subjects, including 284 with proteinuria and 536 with ESRD) of European ancestry (confirmed by population ancestry and substructure analysis using EIGENSOFT; for further details see Pezzolesi et al. [15]) were included in the current study (Table 1).
TABLE 1.
Baseline clinical characteristics of the GoKinD collection
| GoKinD collection |
P | ||
|---|---|---|---|
| Control subjects | Case subjects | ||
| n | 885 | 820 | |
| Men/women | 363/522 | 423/397 | <0.0001 |
| Age at type 1 diabetes diagnosis (years) | 12.9 ± 7.4 | 11.8 ± 6.7 | 0.0008 |
| Duration of type 1 diabetes (years)* | 25.4 ± 7.8 | 26.5 ± 7.7 | 0.003 |
| Age at examination (years) | 38.3 ± 8.7 | 43.1 ± 6.9 | <0.0001 |
| Laser treatment (%) | 17 | 85 | <0.0001 |
| A1C (%)† | 7.4 ± 1.2 | 8.3 ± 1.6 | <0.0001 |
| ACR (μg/mg) | |||
| Control subjects | 6.5 ± 3.7 | ||
| Proteinuric subjects | 1,520 ± 1,478 | ||
| Systolic blood pressure (mmHg) | 117.6 ± 11.9 | 131.1 ± 18.9 | <0.0001 |
| Diastolic blood pressure (mmHg) | 71.4 ± 7.8 | 74.3 ± 10.8 | <0.0001 |
| Case subjects with proteinuria/ESRD | — | 284/536 | |
| ESRD duration (years) | — | 7.3 ± 5.5 | |
| Kidney transplant (%)‡ | — | 92 | |
Data are means ±SD unless otherwise indicated.
*The duration of type 1 diabetes in control and proteinuric subjects is based on the duration at examination. Among ESRD case subjects, this is based on the duration of type 1 diabetes at the onset of ESRD. All other clinical characteristics are based on measurements performed at examination.
†Mean A1C values do not include data from case subjects that have undergone pancreas transplantation (32%).
‡Percentages are of ESRD group.
Genotyping and imputation.
The GoKinD collection was genotyped on the Affymetrix 5.0 500K SNP Array, a genotyping platform with estimated single- and multimarker genomic coverage of 76 and 84%, respectively, by the Genetic Association Information Network (GAIN) genotyping laboratory at the Eli and Edythe L. Broad Institute (Cambridge, MA) (17). After internal quality control, the GAIN genotyping laboratory released genotypes for 467,144 single nucleotide polymorphisms (SNPs). Details of the quality control criteria applied to these data have been published previously (15). Briefly, the application of quality control metrics for minor allele frequency (MAF) <0.01, rejection of Hardy-Weinberg assumptions (P ≤ 10−5), and differential rates of missing data (by case/control subject status) resulted in high-quality genotypic data for 359,193 autosomal SNPs.
Genotypic data for all SNPs with a minor allele frequency >0.05 that mapped to the ELMO1 locus, including 50 kb of flanking sequence (chromosome 7 position 36,810,486 to 37,505,036, in reference to NCBI Build 36.1), were extracted from the GWAS data. Within this 694.5-kb region, a total of 106 genotyped SNPs were obtained. Because none of the SNPs previously reported to be associated with diabetic nephropathy were genotyped on the Affymetrix 5.0 platform, the genotypes for these SNPs were imputed using MaCH (www.sph.umich.edu/csg/abecasis/MACH/) software. Three SNPs (rs3807163, rs4723593, and rs1541727) were not genotyped in HapMap and, therefore, were not able to be imputed in the GoKinD collection. In total, 118 SNPs (106 genotyped and 12 imputed) with an average intermarker distance of 5.9 kb were included in our association analysis.
Statistical analysis.
Linkage disequilibrium (LD) blocks were defined using the method of Gabriel et al. (18) as implemented in Haploview version 4.1 (19). All SNPs were analyzed using stratified additive tests of association (adjusting for both sex and JDC/GWU strata) using the Cochran-Mantel-Haenzel test procedure to calculate combined P values and odds ratios (ORs). Associations with diabetic nephropathy were also assessed under both dominant and recessive genetic models. All statistical and haplotype analyses were performed using PLINK (19).
RESULTS
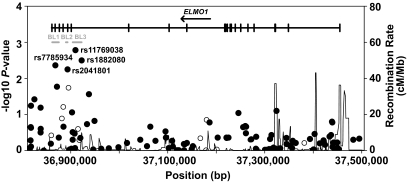
Genotypic association with diabetic nephropathy for all 118 SNPs in ELMO1 under an additive genetic model is shown in Fig. 1 (also see supplemental Table S1 in the online appendix, available at http://diabetes.diabetesjournals.org/content/early/2009/08/02/db09-0641/suppl/DC1). A total of eight SNPs showed nominal evidence of association with diabetic nephropathy (P < 0.05) among the 885 control and 820 case subjects (Table 2). The strongest associations occurred at rs11769038 (OR 1.24; P = 1.7 × 10−3) and rs1882080 (OR 1.23; P = 3.2 × 10−3). These two SNPs map to intron 16 (located ∼12.5 kb apart) and are in near-complete LD (r2 = 0.98). Two additional SNPs, rs2041801 (intron 18) and rs7785934 (intron 20), were also associated with diabetic nephropathy in the GoKinD samples (OR 1.22, P = 5.6 × 10−3 and OR 1.22, P = 4.4 × 10−3, respectively). Although rs2041801 is in tight LD with rs11769038 and rs1882080 (r2 = 0.97), LD among these three variants and rs7785934 is diminished (r2 = 0.60–0.62). The four associated SNPs localize to three distinct LD blocks. Haplotype analysis of these three blocks (using representative tagging SNPs) did not yield more significant differences between case and control subjects than our single SNP analysis (data not shown). Two-SNP haplotype analysis of rs7785934 in combination with either rs11769038 (P = 2.5 × 10−4) or rs1882080 (P = 3.7 × 10−4) yielded more significant differences between case and control subjects than the single-SNP analysis of these variants.
FIG. 1.
Summary of association results for SNPs in the ELMO1 locus in the GoKinD collection. GWAS and imputed data for 118 SNPs across the ELMO1 locus on chromosome 7p are presented. Shaded circles represent SNPs genotyped on the Affymetrix array (n = 106), and unshaded circles represent imputed SNPs from previous reports by Shimazaki et al. and Leak et al. (10,14) (n = 12). The strongest associations in GoKinD occurred at rs7785934, rs2041801, rs11769038, and rs1882080 and localize to three LD blocks (BL1, BL2, and BL3; shown in gray) that span introns 16–21 of the ELMO1 gene.
TABLE 2.
Summary of association results for ELMO1 SNPs in the GoKinD collection (P < 0.05)
| SNP | Position | Location | Risk allele (nonrisk allele) | GoKinD collection |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Control vs. all case subjects |
Control vs. proteinuric subjects |
Control vs. ESRD subjects |
|||||||||
| Control subjects (n = 885) | All case subjects (n = 820) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | ||||
| rs10255208 | 36,825,168 | 3' flanking region | G(A) | 0.49 | 0.53 | 0.04 | 1.15 (1.01–1.32) | 0.45 | 1.08 (0.89–1.31) | 0.03 | 1.18 (1.01–1.38) |
| rs7785934 | 36,868,104 | Intron 20 | C(T) | 0.43 | 0.48 | 4.4 × 10−3 | 1.22 (1.06–1.40) | 0.77 | 1.03 (0.85–1.26) | 3.3 × 10−4 | 1.33 (1.14–1.55) |
| rs7782979 | 36,871,575 | Intron 20 | A(C) | 0.48 | 0.52 | 0.02 | 1.18 (1.03–1.35) | 0.37 | 1.09 (0.90–1.33) | 0.01 | 1.22 (1.04–1.42) |
| rs2041801 | 36,893,366 | Intron 18 | A(G) | 0.52 | 0.56 | 5.6 × 10−3 | 1.22 (1.06–1.39) | 0.16 | 1.15 (0.95–1.40) | 6.2 × 10−3 | 1.24 (1.06–1.45) |
| rs7799004* | 36,895,489 | Intron 17 | T(C) | 0.79 | 0.82 | 0.02 | 1.23 (1.04–1.46) | 0.17 | 1.19 (0.93–1.53) | 0.02 | 1.26 (1.03–1.53) |
| rs11769038 | 36,909,839 | Intron 16 | T(G) | 0.51 | 0.56 | 1.7 × 10−3 | 1.24 (1.09–1.42) | 0.07 | 1.20 (0.98–1.46) | 2.9 × 10−3 | 1.27 (1.08–1.48) |
| rs1882080 | 36,922,366 | Intron 16 | A(G) | 0.52 | 0.56 | 3.2 × 10−3 | 1.23 (1.08–1.41) | 0.12 | 1.17 (0.96–1.43) | 4.0 × 10−3 | 1.26 (1.08–1.47) |
| rs10268319 | 36,937,360 | Intron 16 | C(T) | 0.53 | 0.57 | 0.03 | 1.17 (1.02–1.34) | 0.25 | 1.12 (0.92–1.37) | 0.03 | 1.19 (1.02–1.39) |
The most strongly associated ELMO1 SNPs (P < 0.05) in the GoKinD collection are presented for all case, proteinuric, and ESRD subjects. P values and ORs (95% CIs) for all case, proteinuric, and ESRD subjects vs. control subjects were calculated using stratified additive tests of association using the Cochran-Mantel-Haenszel method, adjusting for both sex and JDC/GWU strata. SNP positions and locations are in reference to NCBI Build 36.1.
*rs7799004 also reported by Shimazaki et al. (10).
Because recent studies have suggested that the development of proteinuria and its progression to ESRD may be influenced by different genetic factors, we analyzed the eight nominally significant ELMO1 SNPs for association with prevalent proteinuria (n = 284) and ESRD (n = 536) (Table 2) (20,21). Only SNP rs7785934 was found to be primarily associated with ESRD (OR 1.33, P = 3.3 × 10−4 vs. OR 1.03, P = 0.77 in proteinuria). Additionally, analysis of the two-SNP haplotypes formed by rs7785934 and either rs11769038 or rs1882080 was more strongly associated with ESRD than the individual SNPs (P = 1.3 × 10−5 and P = 1.7 × 10−5, respectively), whereas no association of these haplotypes was observed in patients with proteinuria (P = 0.36 and P = 0.43, respectively). We also examined the effects of this exposure on the SNPs (Table 2) by stratifying case and control subjects across tertiles of diabetes duration (at the onset of ESRD or at enrollment into GoKinD for proteinuric and control subjects) (22). The strength of the associations was consistent across these strata (data not shown). Finally, we investigated whether differences in A1C levels between case and control subjects contributed to the associations at these SNPs. No evidence of interaction was observed with this quantitative trait (P = 0.18–0.98).
The ELMO1 variants previously shown to be associated with diabetic nephropathy in type 2 diabetes were examined for evidence of association under additive, dominant, and recessive genetic models (Table 3). Three variants that had been reported to be associated with diabetic nephropathy in Japanese case subjects with type 2 diabetes (rs1558688, rs741301, and rs7799004) achieved nominal significance in the GoKinD collection (P ≤ 0.03); however, the SNP genotypes had an opposite direction of genetic effect in this collection and, thus, did not confirm the previous associations (supplemental Table S2 in the online appendix). The allele frequencies of these three variants in both the GoKinD and CEU HapMap (www.hapmap.org) populations are similar (data not shown).
TABLE 3.
Summary of associations for SNPs reported by Shimazaki et al. and Leak et al. in the GoKinD collection
| SNP | Position | Location | Risk allele (nonrisk allele) | Genetic model |
||
|---|---|---|---|---|---|---|
| Additive | Dominant | Recessive | ||||
| Shimazaki et al. (ref. 10): Japanese, type 2 diabetes, diabetic nephropathy* | ||||||
| rs7804092 | 36,859,757 | 3' flanking region | T(A) | 0.38 | 0.56 | 0.20 |
| rs1558688 | 36,881,710 | Intron 19 | C(T) | 0.13 | 0.55 | 0.03 |
| rs741301 | 36,884,520 | Intron 18 | T(C) | 0.06 | 0.33 | 0.03 |
| rs7799004 | 36,895,489 | Intron 17 | T(C) | 0.02 | 0.06 | 0.05 |
| rs11983698 | 36,915,072 | Intron 16 | T(C) | 0.25 | 0.52 | 0.06 |
| rs4723596 | 36,917,569 | Intron 16 | T(C) | 0.51 | 0.81 | 0.17 |
| Leak et al. (ref. 14): African American, type 2 diabetes, ESRD | ||||||
| rs1345365 | 37,167,138 | Intron 13 | G(A) | 0.46 | 0.54 | 0.81 |
| rs1981740 | 37,178,829 | Intron 13 | C(A) | 0.97 | 0.98 | 0.89 |
| rs10951509 | 37,180,008 | Intron 13 | G(A) | 0.14 | 0.12 | 0.94 |
| rs2058730 | 37,201,281 | Intron 13 | T(C) | 0.94 | 0.54 | 0.32 |
| rs2717972 | 37,270,120 | Intron 5 | A(G) | 0.50 | 0.54 | 0.79 |
| rs9969311 | 37,381,582 | Intron 1 | G(A) | 0.62 | 0.97 | 0.05 |
SNP positions and locations are in reference to NCBI Build 36.1.
*Three SNPs reported by Shimazaki et al. (ref. 10) (rs3807163, rs4723593, and rs1541727) were not genotyped in HapMap and, therefore, were not imputed in the GoKinD collection.
DISCUSSION
Genetic variants in ELMO1 have recently been shown to be associated with diabetic nephropathy in two independent and ethnically distinct collections of patients with type 2 diabetes (10,14). In this report, we examined whether variants in this same gene are associated with the risk of diabetic nephropathy in patients with type 1 diabetes. Through our comprehensive analysis of this locus, we extend these previous findings by demonstrating that variants in ELMO1 are also associated with the risk of diabetic nephropathy in Caucasian type 1 diabetic patients.
We investigated the role of 118 SNPs in ELMO1, including 12 SNPs previously reported to be associated with diabetic nephropathy in type 2 diabetes. Our analysis identified associations at several intronic SNPs (rs7785934, rs2041801, rs11769038, and rs1882080; P = 1.7 × 10−3 to 5.6 × 10−3). Although none of these SNPs met stringent criteria for significance following adjustment for multiple testing (P < 0.05/118 = 4.3 × 10−4), this threshold was exceeded by one SNP (rs7785934) when our analysis was limited to case subjects with ESRD. Moreover, the modest effect size of this variant (OR 1.33) is consistent with those previously reported in two independent African American ESRD populations (14), suggesting a comparable effect in the two populations. Additionally, the two-SNP haplotypes formed by rs7785934 and either rs11769038 or rs1882080 were more strongly associated with ESRD than these individual SNPs, suggesting that the LD block containing these SNPs forms a larger haplotype that either contains or is in tight LD with the causal variant at this locus. Together, these data also suggest that ELMO1 may have a role in the advanced stages of diabetic nephropathy, perhaps contributing to renal function decline, rather than its initiation. We acknowledge, however, that the GoKinD collection is heavily weighted with case subjects with ESRD. The small number of case subjects with proteinuria may have limited our ability to detect ELMO1 variants that are primarily associated with the risk of proteinuria. Despite this limitation, functional studies have demonstrated that ELMO1 contributes to the progression of chronic glomerular injury through its dysregulation of extracellular matrix (ECM) metabolism, resulting in renal ECM accumulation (11). This accumulation contributes to both glomerular and tubular basement membrane thickening, two well-established hallmarks of advanced diabetic nephropathy (23).
Our investigation marks the third report of genetic associations in ELMO1 with diabetic nephropathy, further establishing its role in conferring increased susceptibility to this disease. Previous reports (10,14) identified their strongest associations at variants located more than 280 kb apart in introns 17 and 13. Although our strongest associations are located near the associated SNP reported by Shimazaki et al. (10), our most associated SNPs are independent of those reported in this study. Furthermore, no evidence of association for the variants reported in either type 2 diabetic population was identified in our collection. The associations at ELMO1 across each study are consistent with allelic heterogeneity, likely contributed by the diverse ancestral genetic backgrounds of the different ethnic groups. Examination of the associated SNPs from each study in the available HapMap populations (www.hapmap.org) confirms the variable allele frequencies of these variants among different ethnic and racial groups (data not shown). We hypothesize that rare polymorphisms in ELMO1, either the same variants or those in strong or complete LD, may be common to each ethnic group and merely tagged by the common variants identified in each study. Further investigation of rare SNPs at the ELMO1 locus is necessary to fully understand the commonality of these associations and to elucidate the mechanism(s) underlying their role in diabetic nephropathy.
In summary, our study provides the first comprehensive analysis of genetic variants at the ELMO1 locus in a Caucasian population with diabetic nephropathy and type 1 diabetes. Our analysis identified several associations that are independent of those previously identified in other ethnic groups with diabetic nephropathy and type 2 diabetes; however, our examination of this locus in the GoKinD collection further supports its potential role in this disease. Confirmation of the associations identified in our study in additional collections, including ethnically diverse populations with either type 1 or type 2 diabetes, is necessary to better understand the role of these variants, and, perhaps, rare variants yet to be examined may underlie the genetic susceptibility of diabetic nephropathy attributed to this locus.
Supplementary Material
Acknowledgments
We acknowledge grant support from the National Institutes of Health (NIH) (DK77532 to A.S.K.) and from the Foundation for NIH (FNIH) (06GAIN0 to J.H.W.). We also acknowledge the Joslin Diabetes Center's NIH Training Grant T32 (DK007260-31 to M.G.P.) and support from the Juvenile Diabetes Research Foundation (3-2009-397 to J.S.).
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Krolewski AS, Warram JH: Clinical features and epidemiology of diabetic nephropathy In Textbook of Diabetes 2nd ed Pickup JC, Williams G. Eds. Oxford, Blackwell Scientific Publications, 1997, p. 53.51–53.13 [Google Scholar]
- 2.Parving HH, Mauer M, Ritz E: Diabetic nephropathy In Brenner and Rector's The Kidney 7th ed.Brenner BM. Ed. Philadelphia, Elsevier, 2004, p. 1777–1818 [Google Scholar]
- 3.Jones CA, Krolewski AS, Rogus J, Xue JL, Collins A, Warram JH: Epidemic of end-stage renal disease in people with diabetes in the United States population: do we know the cause? Kidney Int 2005;67:1684–1691 [DOI] [PubMed] [Google Scholar]
- 4.Seaquist ER, Goetz FC, Rich S, Barbosa J: Familial clustering of diabetic kidney disease: evidence for genetic susceptibility to diabetic nephropathy N Engl J Med 1989;320:1161–1165 [DOI] [PubMed] [Google Scholar]
- 5.Borch-Johnsen K, Norgaard K, Hommel E, Mathiesen ER, Jensen JS, Deckert T, Parving HH: Is diabetic nephropathy an inherited complication? Kidney Int 1992;41:719–722 [DOI] [PubMed] [Google Scholar]
- 6.Freedman BI, Tuttle AB, Spray BJ: Familial predisposition to nephropathy in African-Americans with non-insulin-dependent diabetes mellitus Am J Kidney Dis 1995;25:710–713 [DOI] [PubMed] [Google Scholar]
- 7.McCance DR, Hanson RL, Pettitt DJ, Jacobsson LT, Bennett PH, Bishop DT, Knowler WC: Diabetic nephropathy: a risk factor for diabetes mellitus in offspring Diabetologia 1995;38:221–226 [DOI] [PubMed] [Google Scholar]
- 8.Quinn M, Angelico MC, Warram JH, Krolewski AS: Familial factors determine the development of diabetic nephropathy in patients with IDDM Diabetologia 1996;39:940–945 [DOI] [PubMed] [Google Scholar]
- 9.Rich SS: Genetics of diabetes and its complications J Am Soc Nephrol 2006;17:353–360 [DOI] [PubMed] [Google Scholar]
- 10.Shimazaki A, Kawamura Y, Kanazawa A, Sekine A, Saito S, Tsunoda T, Koya D, Babazono T, Tanaka Y, Matsuda M, Kawai K, Iiizumi T, Imanishi M, Shinosaki T, Yanagimoto T, Ikeda M, Omachi S, Kashiwagi A, Kaku K, Iwamoto Y, Kawamori R, Kikkawa R, Nakajima M, Nakamura Y, Maeda S: Genetic variations in the gene encoding ELMO1 are associated with susceptibility to diabetic nephropathy Diabetes 2005;54:1171–1178 [DOI] [PubMed] [Google Scholar]
- 11.Shimazaki A, Tanaka Y, Shinosaki T, Ikeda M, Watada H, Hirose T, Kawamori R, Maeda S: ELMO1 increases expression of extracellular matrix proteins and inhibits cell adhesion to ECMs Kidney Int 2006;70:1769–1776 [DOI] [PubMed] [Google Scholar]
- 12.Bowden DW, Colicigno CJ, Langefeld CD, Sale MM, Williams A, Anderson PJ, Rich SS, Freedman BI: A genome scan for diabetic nephropathy in African Americans Kidney Int 2004;66:1517–1526 [DOI] [PubMed] [Google Scholar]
- 13.Placha G, Poznik GD, Dunn J, Smiles A, Krolewski B, Glew T, Puppala S, Schneider J, Rogus JJ, Rich SS, Duggirala R, Warram JH, Krolewski AS: A genome-wide linkage scan for genes controlling variation in renal function estimated by serum cystatin C levels in extended families with type 2 diabetes Diabetes 2006;55:3358–3365 [DOI] [PubMed] [Google Scholar]
- 14.Leak TS, Perlegas PS, Smith SG, Keene KL, Hicks PJ, Langefeld CD, Mychaleckyj JC, Rich SS, Kirk JK, Freedman BI, Bowden DW, Sale MM: Variants in intron 13 of the ELMO1 gene are associated with diabetic nephropathy in African Americans Ann Intern Med 2009;73:152–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pezzolesi MG, Poznik GD, Mychaleckyj JC, Paterson AD, Barati MT, Klein JB, Ng DP, Placha G, Canani LH, Bochenski J, Waggott D, Merchant ML, Krolewski B, Mirea L, Wanic K, Katavetin P, Kure M, Wolkow P, Dunn JS, Smiles A, Walker WH, Boright AP, Bull SB, Doria A, Rogus JJ, Rich SS, Warram JH, Krolewski AS: Genome-wide association scan for diabetic nephropathy susceptibility genes in type 1 diabetes Diabetes 2009;58:1403–1410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mueller PW, Rogus JJ, Cleary PA, Zhao Y, Smiles AM, Steffes MW, Bucksa J, Gibson TB, Cordovado SK, Krolewski AS, Nierras CR, Warram JH: Genetics of Kidneys in Diabetes (GoKinD) study: a genetics collection available for identifying genetic susceptibility factors for diabetic nephropathy in type 1 diabetes J Am Soc Nephrol 2006;17:1782–1790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.GAIN Collaborative Research Group. New models of collaboration in genome-wide association studies: the Genetic Association Information Network Nat Genet 2007;39:1045–1051 [DOI] [PubMed] [Google Scholar]
- 18.Gabriel SB, Schaffner SF, Nguyen H, Moore JM, Roy J, Blumenstiel B, Higgins J, DeFelice M, Lochner A, Faggart M, Liu-Cordero SN, Rotimi C, Adeyemo A, Cooper R, Ward R, Lander ES, Daly MJ, Altshuler D: The structure of haplotype blocks in the human genome Science 2002;296:2225–2229 [DOI] [PubMed] [Google Scholar]
- 19.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, Sham PC: PLINK: a tool set for whole-genome association and population-based linkage analyses Am J Hum Genet 2007;81:559–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Placha G, Canani LH, Warram JH, Krolewski AS: Evidence for different susceptibility genes for proteinuria and ESRD in type 2 diabetes Adv Chronic Kidney Dis 2005;12:155–169 [DOI] [PubMed] [Google Scholar]
- 21.Al-Kateb H, Boright AP, Mirea L, Xie X, Sutradhar R, Mowjoodi A, Bharaj B, Liu M, Bucksa JM, Arends VL, Steffes MW, Cleary PA, Sun W, Lachin JM, Thorner PS, Ho M, McKnight AJ, Maxwell AP, Savage DA, Kidd KK, Kidd JR, Speed WC, Orchard TJ, Miller RG, Sun L, Bull SB, Paterson AD: Multiple superoxide dismutase 1/splicing factor serine alanine 15 variants are associated with the development and progression of diabetic nephropathy: the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Genetics study Diabetes 2008;57:218–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rogus JJ, Warram JH, Krolewski AS: Genetic studies of late diabetic complications: the overlooked importance of diabetes duration before complication onset Diabetes 2002;51:1655–1662 [DOI] [PubMed] [Google Scholar]
- 23.Caramori ML, Kim Y, Huang C, Fish AJ, Rich SS, Miller ME, Russell G, Mauer M: Cellular basis of diabetic nephropathy. 1. Study design and renal structural–functional relationships in patients with long-standing type 1 diabetes Diabetes 2002;51:506–513 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.