Abstract
OBJECTIVE
Interest continues to grow regarding the therapeutic potential for umbilical cord blood therapies to modulate autoimmune disease. We conducted an open-label phase I study using autologous umbilical cord blood infusion to ameliorate type 1 diabetes.
RESEARCH DESIGN AND METHODS
Fifteen patients diagnosed with type 1 diabetes and for whom autologous umbilical cord blood was stored underwent a single intravenous infusion of autologous cells and completed 1 year of postinfusion follow-up. Intensive insulin regimens were used to optimize glycemic control. Metabolic and immunologic assessments were performed before infusion and at established time periods thereafter.
RESULTS
Median (interquartile range [IQR]) age at infusion was 5.25 (3.1–7.3) years, with a median postdiagnosis time to infusion of 17.7 (10.9–26.5) weeks. No infusion-related adverse events were observed. Metabolic indexes 1 year postinfusion were peak C-peptide median 0.50 ng/ml (IQR 0.26–1.30), P = 0.002; A1C 7.0% (IQR 6.5–7.7), P = 0.97; and insulin dose 0.67 units · kg−1 · day−1 (IQR 0.55–0.77), P = 0.009. One year postinfusion, no changes were observed in autoantibody titers, regulatory T-cell numbers, CD4-to-CD8 ratio, or other T-cell phenotypes.
CONCLUSIONS
Autologous umbilical cord blood transfusion in children with type 1 diabetes is safe but has yet to demonstrate efficacy in preserving C-peptide. Larger randomized studies as well as 2-year postinfusion follow-up of this cohort are needed to determine whether autologous cord blood–based approaches can be used to slow the decline of endogenous insulin production in children with type 1 diabetes.
Type 1 diabetes is an autoimmune disorder characterized by T-cell–mediated destruction of insulin-producing β-cells and lifelong dependence on exogenous insulin administration. To date, the majority of efforts seeking to ameliorate the autoimmune process and reverse hyperglycemia have focused on the use of immunosuppressive or immunomodulatory drugs (1–4). Although several agents have shown and continue to show promise, no single agent has succeeded in demonstrating long-term success in preventing or reversing type 1 diabetes as a means of standard medical practice. More recently, efforts have focused on the use of either autologous or allogeneic hematopoietic stem/progenitor cells as potential immunoregulatory agents to reverse this disease. Whereas hematopoietic stem cells have successfully been directed in vitro to differentiate into insulin- and C-peptide–producing cells (5), and infusion of human hematopoietic stem cells into diabetic animals has demonstrated reversal of disease (6,7), the potential of such cells to provide a source of safe and effective immunomodulation may be of the greatest importance in treating type 1 diabetes, but this has yet to be realized (8–10).
Among the broad array of potential cell-based therapies, the use of autologous umbilical cord blood as a source of immunomodulatory cells for the treatment of autoimmune diseases has become increasingly popular (11–14), this based on the potential for umbilical cord blood to restore proper immune regulation. Umbilical cord blood contains a robust population of immature unprimed highly functional regulatory T-cells (Tregs) (15). These highly functional Tregs could, in theory, limit inflammatory cytokine responses and anergize effector T-cells, which are thought to play a key role in cellular-mediated autoimmune processes (16,17). As such, umbilical cord blood Tregs have become a major focus of our work in designing cell-based therapies for children with type 1 diabetes (18).
Practical matters provide an additional rationale for umbilical cord blood–based therapies. First, the lack of low-risk (i.e., safe) diabetes intervention trials seeking to reverse disease, especially for young children with type 1 diabetes, renders the potential use of umbilical cord blood particularly appealing. Second, as the rates of umbilical cord blood storage continue to increase exponentially, the number of potential subjects for autologous umbilical cord blood–based clinical trials continues to grow. Third, the fact that umbilical cord blood is stored at birth without need for additional intervention (i.e., bone marrow biopsy or stem cell mobilization and aphaeresis) is an additional practical advantage in considering a cell-based therapy for children. Finally, as umbilical cord blood storage facilities continue to reevaluate storage methods that would allow for multiple withdrawals, potential exists for protocols that involve cell expansion and/or multiple cell infusions.
Although we focused our interest on the notion that umbilical cord blood Tregs might affect tolerance, we also considered that autologous umbilical cord blood transfusion in the setting of type 1 diabetes may help mitigate the autoimmune process by a variety of mechanisms beyond those of direct immune modulation (19). First, umbilical cord blood stem cells may migrate to the damaged pancreas, where they could differentiate into insulin-producing β-cells (2). In addition, umbilical cord blood stem cells might act as nurse cells to foster the proliferation or replication of new β-cells from remnant viable tissue (20). Finally, umbilical cord blood Tregs may facilitate bystander suppression of effector T-cells, allowing for the restoration of tolerance by their inhibitory effects on multiple cell types (21).
Based on available preclinical data and the agreement that infusion of minimally manipulated autologous umbilical cord blood was likely to be extremely safe, we performed an unblinded observational pilot study to determine whether autologous umbilical cord blood infusion could impede the type 1 diabetes autoimmune process and preserve remaining endogenous insulin production. Peak C-peptide after a standard mixed-meal tolerance test (MMTT), A1C, and daily insulin requirement were set as the primary outcome variables, with a variety of immunologic markers assessed for their potential mechanistic insights.
RESEARCH DESIGN AND METHODS
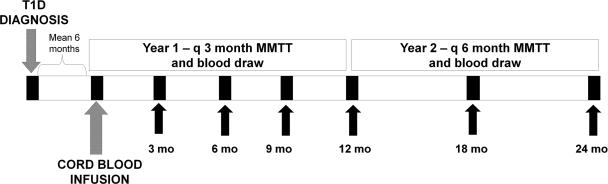
A detailed description of the study protocol's design, without results, has been published previously (18). The study timeline is displayed in Fig. 1. Briefly, subjects aged >1 year with type 1 diabetes (established by clinical presentation and presence of type 1 diabetes–associated autoantibodies) and for whom autologous umbilical cord blood had been stored in an American Association of Blood Banks (AABB)- or Foundation for the Accreditation for Cellular Therapy (FACT)-recognized cord blood bank, were recruited for participation in this single-center study (NCT00305344; FDA IND BB-11918). This Federal Drug Administration (FDA)-approved study of 23 subjects completed enrolment in November 2008. Follow-up for the entire cohort will continue until all subjects have reached the 2-year postinfusion study visit. For this report, the first 15 of these 23 subjects who completed at least 1 year postinfusion follow-up are reported herein. In addition, because the FDA and institutional review board did not allow, on this occasion, for the implementation of a placebo-controlled investigation, for comparative purposes we collected retrospective data on type 1 diabetic subjects matched 2:1 (control subjects to umbilical cord blood recipients) for age and duration of disease.
Figure 1.
Autologous cord blood infusion in type 1 diabetes: study timeline. Our study was designed as a 2-year observational study of the effects of autologous cord blood infusion in children with type 1 diabetes. Each child was followed every 3 months during the first year postinfusion and every 6 months during the second year postinfusion. Blood was obtained for metabolic and immunologic studies at each visit. Mean time from type 1 diabetes diagnosis to umbilical cord blood infusion was 6 months. Herein, we report 1 year postinfusion data on the first 15 umbilical cord blood recipients to reach 1 year of post–cord blood infusion follow-up. T1D, type 1 diabetes; UCB, umbilical cord blood; q, every.
After eligible subjects were identified and provided consent, peripheral blood and an aliquot of umbilical cord blood from the subject were shipped to the University of Florida stem cell laboratory where infectious disease testing, HLA confirmation, and screening for viability were performed. Thereafter, the subject's remaining umbilical cord blood unit was shipped to the University of Florida and stored until transfused. Subjects were then scheduled to perform a standard 2-h MMTT to determine baseline endogenous insulin production and A1C values. Additional blood was drawn for routine clinical assessments as well as metabolic and immunologic analyses.
On the subsequent day, the subject's autologous umbilical cord blood was thawed and washed per standard operation procedures of the University of Florida stem cell laboratory. An aliquot of cells was analyzed for viability, CD34 percentage, and Treg frequency (i.e., percentage of CD3+CD4+CD25+FOXP3+ cells). After the preparation of the unit, subjects received pretreatment with diphenhydramine and acetaminophen. No chemotherapy or other preparative therapy was given. The thawed umbilical cord blood cells (typically <100 ml) were then infused through a peripheral intravenous drip over 10–20 min. After infusion, subjects were observed closely for at least 6 h prior to being discharged.
Subjects returned for follow-up testing every 3 months in the first postinfusion year and every 6 months in the second postinfusion year. MMTT, complete blood count, basic metabolic panel, and A1C were performed at each visit. In addition, whole blood collected in EDTA tubes was analyzed by flow cytometry with staining for the cell surface markers CD3, CD4, CD8, and CD25 as well as the intracellular marker FOXP3 using standard techniques (21–23). Throughout the study, subjects were encouraged to use any combination of available intensive insulin regimens to achieve the best possible glycemic control. Use of hypoglycemic agents other than insulin or any immunosuppressive agents was not permitted.
Statistical analysis
Because of the propensity for outliers in several of the outcome variables, medians and quartiles were reported rather than means and SDs. To determine changes from baseline to 12 months, we calculated the fractional change for each subject as [(Y12/Y0) − 1], where the subscript is the month number. These fractional changes were then tested for a target population null hypothesis of a median of zero by the two-sided Wilcoxon sign-rank test, a nonparametric procedure. The pilot nature of this study dictated against controlling study-wide errors via either a Bonferroni correction or formal multivariate analysis. Historical control comparisons used the two-sided two-sample Wilcoxon test.
RESULTS
Between 24 August 2005 and 21 November 2008, 23 children with type 1 diabetes (10 male and 13 female) underwent a single autologous umbilical cord blood transfusion at the University of Florida. As of January 2009, 15 subjects (7 male and 8 female) completed 1 year of postinfusion study follow-up. Baseline and 1-year postinfusion characteristics of these 15 subjects are provided in Table 1.
Table 1.
Baseline and 1-year postinfusion characteristics of autologous umbilical cord blood recipients (n = 8 male and 7 female)
| Preinfusion | 1-year postinfusion | (Preinfusion-to–1 year postinfusion ratio) −1 | P vs. baseline | |
|---|---|---|---|---|
| Age (years) | 5.5 (3.1–7.3) | — | — | — |
| Time from diagnosis to infusion (months) | 4.1 (2.5–7.1) | — | — | — |
| A1C (%) | 7.0 (6.1–8.3) (15) | 7.0 (6.5–7.7) (15) | 0.035 (−0.07 to 0.125) (15) | 0.45 |
| Insulin use (units · kg−1 · day−1) | 0.42 (0.21–0.55) (15) | 0.67 (0.55–0.77) (15) | 0.52 (0.00–1.56) (15) | 0.0085 |
| Peak C-peptide (ng/ml) | 0.93 (0.7–2.03) (14) | 0.50 (0.26–1.30) (12) | −0.53 (−0.72 to −0.32) (12) | 0.0024 |
| IA-2 | 9.5 (1.8–20.6) (11) | 9.8 (0.7–14.47) (9) | −0.48 (−0.58 to −0.10) (8) | 0.20 |
| GAD | 4.2 (0.9–11.4) (13) | 3.5 (0.45–33.5) (12) | −0.44 (−0.63 to 0.34) (11) | 0.52 |
| WBC (cell × 109/l) | 5.5 (4.9–7.3) (14) | 4.9 (4.2–6.3) (14) | −0.13 (−0.29 to 0.14) (14) | 0.031 |
| CD4-to-CD8 ratio | 2.0 (1.7–2.6) (14) | 1.9 (1.6–2.2) (12) | −0.03 (−0.13 to 0.11) (12) | 0.86 |
| Peripheral blood Treg (%) | 5.4 (2.4–7.0) (12) | 5.0 (4.1–7.2) (13) | 0.31 (−0.06 to 2.00) (11) | 0.12 |
Data are median (IQR) (n). IA-2, insulinoma-associated protein 2 autoantibody; WBC, white blood cell count.
With the exception of one autologous umbilical cord blood unit recovered from a public bank, the remaining 22 units were stored in private cord blood facilities throughout the U.S., Canada, and Mexico. The median infused total nucleated cell count in those subjects with 1 year of follow-up was 1.50 × 107 cells/kg. Median viability was 96% (range 92–99%). Overall, the total nucleated cell count recovered was commonly 1– to 2–log-fold less than that typically observed in samples obtained from public banks (24).
All aliquots of umbilical cord blood had negative gram stains, and none grew pathogenic organisms when cultured for virus, bacteria, or fungus. No adverse events were observed in association with autologous umbilical cord blood infusion. None of the 23 subjects receiving the cellular infusion developed fever, hypo- or hypertension, nausea or vomiting, abnormalities in serum creatinine, or clinically relevant changes in complete blood count parameters. Furthermore, no subject reported a severe hypoglycemic event (seizure or hypoglycemia requiring assistance) or admission for treatment of diabetic ketoacidosis throughout the first year of follow-up.
In the 15 subjects with at least 1 year of study follow-up (average 18 months postdiagnosis), median peak C-peptide (interquartile range [IQR]) at the time of autologous umbilical cord blood infusion was 0.93 (0.7–2.03 ng/ml). At the 1 year post–umbilical cord blood infusion visit, median peak C-peptide was 0.5 (0.26–1.30 ng/ml). The fractional change in peak C-peptide from infusion to 1 year was −53% (P = 0.0024). The fractional change of area under the curve C-peptide over the 1 year after umbilical cord blood infusion was −69.4% (P = 0.0007). For the same group of study subjects, initial median A1C was 7.0% and 1 year post–umbilical cord blood infusion A1C was 7.0%. Median fractional change in A1C was 0.035% (P = 0.45). Initial median insulin requirement was 0.42 units · kg−1 · day−1 with 1 year post–umbilical cord blood insulin requirements of 0.67 units · kg−1 · day−1. The median fractional increase in insulin requirement over 1 year was 52% (P = 0.0085).
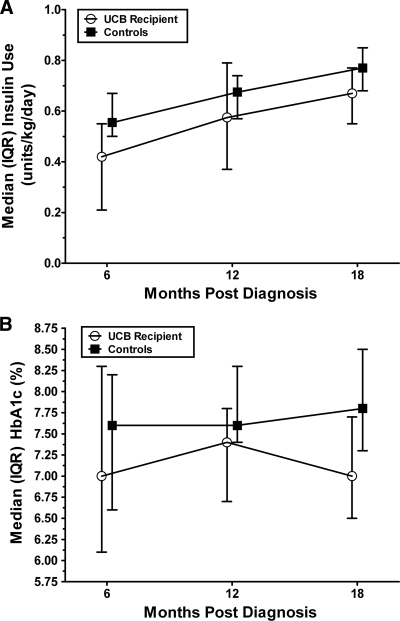
In order to further identify a potential clinical benefit for this procedure, a comparative analysis of A1C and insulin use in this group of umbilical cord blood–treated subjects versus a historical control group of 30 type 1 diabetic patients was also performed. Because the average time from type 1 diabetes diagnosis to umbilical cord blood infusion was 6 months, comparisons were made between umbilical cord blood recipients at 0, 6, and 12 months postinfusion and control subjects at 6, 12, and 18 months post–type 1 diabetes diagnosis. In this group of control subjects (mean age 5.28 years at diagnosis), median A1C and insulin use 18 months after diagnosis were 7.8 and 0.77% units · kg−1 · day−1, respectively. Umbilical cord blood recipients demonstrated lower preinfusion insulin requirements (P = 0.011) but similar A1C (P = 0.16) when compared with the historical control subjects. Whereas the A1C was, as noted earlier, stable over the 1 year of follow-up in umbilical cord blood recipients, the percent change in A1C and insulin use were not significantly different when comparing umbilical cord blood recipients and control subjects at the 12-month follow-up visit (Table 2, Fig. 2A and B). Fractional changes in A1C and insulin requirement at 6 months postinfusion were also not significantly different between umbilical cord blood recipients and historical control subjects (data not shown).
Table 2.
Historical control subjects (n = 30)
| 6 months postdiagnosis |
18 months postdiagnosis |
(Baseline-to–1 year ratio) −1 |
|||
|---|---|---|---|---|---|
| Median (IQR) | P | Median (IQR) | Median (IQR) | P | |
| A1C (%) | 7.6 (6.6–8.2) | 0.16 | 7.8 (7.3–8.5) | 0.040 (−0.076 to 0.146) | 0.73 |
| Insulin use (units · kg−1 · day−1) | 0.56 (0.50–0.67) | 0.011 | 0.77 (0.68 to 0.85) | 0.41 (0.15–0.59) | 0.50 |
Comparisons were made using 6 months and 18 months postdiagnosis time points because these correlated with average time from diagnosis to infusion and average time from diagnosis to 1 year postinfusion in the umbilical cord blood recipients. P values are by two-sided Wilcoxon tests vs. umbilical cord blood recipients. See Table 1 for descriptive statistics for umbilical cord blood recipients.
Figure 2.
Insulin use (A) and A1C (B) in umbilical cord blood recipients and historical control subjects over 1 year. Data are medians with error bars showing IQRs and are presented for the sake of comparison with clinical expectations. Because the average time from diagnosis to umbilical cord blood infusion was 6 months, comparisons correlate with 6, 12, and 18 months post–type 1 diabetes diagnosis in both umbilical cord blood recipients and historical control subjects. Whereas the absolute value of A1C and insulin requirement in umbilical cord blood recipients was lower than that in control subjects at baseline, 6 months, and 12 months, the relevant statistical comparison of percent change was no different over time (Table 2).
Primary analyses examined changes in serum and peripheral blood immune markers from cord blood infusion to the 1 year postinfusion visit. Baseline and 12-month median total peripheral white blood cell count were 5.5 × 109 cells/l and 4.9 × 109 cells/l, respectively, indicative of a −12.9 fractional change (P = 0.03). Median and 12-month post-infusion serum GAD antibody concentrations were 4.2 units/ml and 3.5 units/ml, respectively (P = 0.52). Serum insulinoma-associated protein 2 autoantibody at infusion and 12 months later were unchanged at 9.5 units/ml and 9.8 units/ml, respectively (P = 0.20). CD4-to-CD8 ratio was 1.98 at screening and 1.93 12 months after cord blood infusion (P = 0.85). CD4+CD25+FOXP3+ (Treg) percentages in peripheral blood at infusion and after 12 months were 5.4 and 5.0%, respectively (P = 0.12) (Table 1). No changes in peripheral blood CD45RA (naïve) or CD45RO (memory) cells were observed when comparing baseline and 12-month postinfusion data (data not shown). Hypothesis-generating analysis of the changes in peripheral blood Treg concentration demonstrated a 42% fractional increase of Treg during the 6 months immediately after cord blood infusion (P = 0.06) with the majority of that increase occurring between the 3 and 6 months visits (fractional increase in Treg 35.6%; P = 0.01). No changes in CD4-to-CD8 ratio, CD45RA, or CD45RO cells were seen when comparing data at infusion, 3 months, or 6 months.
CONCLUSIONS
As the first study of a cell-based therapy in children with type 1 diabetes, the most important and robust observation our phase I study provides is that autologous umbilical cord blood infusion in young children with type 1 diabetes is feasible and safe. However, the potential efficacy of autologous umbilical cord blood infusion in the type 1 diabetes setting remains less clear. The currently available data suggest that autologous umbilical cord blood infusion fails to preserve C-peptide levels in young children 1 year after infusion. As such, the 2 years postinfusion data for the entire 23-subject cohort of umbilical cord blood recipients will be important in more conclusively documenting the efficacy of autologous umbilical cord blood infusion in type 1 diabetes.
Because neither the FDA nor our local institutional review board would allow for a randomized or blinded study, we were unable to perform age-matched comparisons of meal-stimulated endogenous insulin production. Furthermore, the lack of comparative meal-stimulated C-peptide data in young children with type 1 diabetes made historical comparisons impossible. Comparison to an age-matched group of type 1 diabetic patients demonstrated that subjects receiving umbilical cord blood infusion maintained A1C and insulin requirements below what most clinicians would expect in such young children. Nevertheless, among umbilical cord blood recipients, peak and area under the curve C-peptide levels 1 year post–umbilical cord blood infusion declined significantly when compared with baseline and fractional changes in A1C, and insulin requirement were no different when comparing umbilical cord blood recipients and historical control subjects.
As we further explore potential applications of autologous umbilical cord blood in treating type 1 diabetes, practical considerations will continue to drive our approach. Notably, the cell counts recovered from privately banked cord blood units used in our study were routinely an order of magnitude lower than cell counts from publicly banked units prepared using the same techniques. This should not necessarily impugn private cord blood banks for providing substandard storage but more likely reflects the frequency of low cell counts at collection and explains why public banks collect and then discard a large percentage of donated units. The relatively low cell counts used in this phase I study may indicate that much higher cell counts are needed to induce relevant immunologic or metabolic effects. Additional efforts to improve collection, storage (i.e., multiple aliquots), cell recovery, and expansion of umbilical cord blood are urgently needed to allow for the development of additional applications beyond traditional umbilical cord blood transplantation.
Additionally, the dictum of primum non nocere must remain paramount when discussing interventional therapies for young children with type 1 diabetes. The development of both safe and effective therapies to preserve β-cell function in patients with type 1 diabetes presents a formidable catch-22. Although high-potency immunosuppressive and immunomodulatory cocktails may indeed be able to preserve C-peptide levels in recently diagnosed patients (14), such approaches are associated with considerable risk of morbidity and even mortality. Type 1 diabetes is inarguably a disease with substantial short-term and long-term complications. Nevertheless, insulin is fairly effective, albeit a cumbersome and imperfect therapy. Our group has long espoused the need to use combination approaches much like those that have proven effective in treating cancer or HIV (25). Still, we must recall that type 1 diabetes is neither cancer nor HIV. Potential combination approaches, including those that include cell therapy, should be associated with appropriately low risk profiles, especially when being considered for use in children.
The potential of umbilical cord blood to participate in the future of type 1 diabetes interventional therapies exists. Nevertheless, multiple therapeutic avenues will need to be explored, and several modalities will likely need to be combined to achieve the dream of safely and permanently reversing or preventing type 1 diabetes. Future efforts to use autologous umbilical cord blood in the treatment of type 1 diabetes will continue with emphasis on mechanistic studies, establishment of age-appropriate comparative groups, and addition of multiple safe therapies (i.e., vitamin D and n-3 fatty acids) in hopes of achieving synergy.
Acknowledgments
This study was funded by Juvenile Diabetes Research Foundation (JDRF) Innovative Grant 1-2005-362, JDRF Center Grant 4-2007-1065, National Institutes of Health (NIH) Contract M01RR00082, and NIH Grant 1R21DK077580–01.
No potential conflicts of interest relevant to this article were reported.
The sponsors of the study had no role in the study design, data collection, data analysis, interpretation of data, or writing of the report.
We acknowledge the assistance of Hilla-Lee Viener (laboratory technician), Douglas Theriaque (data manager), the stem cell laboratory staff and nurses, the General Clinical Research Center staff and nurses, and, most importantly, the children and families who participated in this phase I trial.
Footnotes
Clinical trial reg. no. NCT00305344, clinicaltrials.gov.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
See accompanying editorial, p. 2138.
References
- 1. Silverstein J, Maclaren N, Riley W, Spillar R, Radjenovic D, Johnson S: Immunosuppression with azathioprine and prednisone in recent-onset insulin-dependent diabetes mellitus. N Engl J Med 1988;319:599–604 [DOI] [PubMed] [Google Scholar]
- 2. Ludvigsson J, Faresjö M, Hjorth M, Axelsson S, Chéramy M, Pihl M, Vaarala O, Forsander G, Ivarsson S, Johansson C, Lindh A, Nilsson NO, Aman J, Ortqvist E, Zerhouni P, Casas R: GAD treatment and insulin secretion in recent-onset type 1 diabetes. N Engl J Med 2008;359:1909–1920 [DOI] [PubMed] [Google Scholar]
- 3. Skyler JS, Krischer JP, Wolfsdorf J, Cowie C, Palmer JP, Greenbaum C, Cuthbertson D, Rafkin-Mervis LE, Chase HP, Leschek E: Effects of oral insulin in relatives of patients with type 1 diabetes: the Diabetes Prevention Trial–Type 1. Diabetes Care 2005;28:1068–1076 [DOI] [PubMed] [Google Scholar]
- 4. Herold KC, Gitelman SE, Masharani U, Hagopian W, Bisikirska B, Donaldson D, Rother K, Diamond B, Harlan DM, Bluestone JA: A single course of anti-CD3 monoclonal antibody hOKT3gamma1(Ala-Ala) results in improvement in C-peptide responses and clinical parameters for at least 2 years after onset of type 1 diabetes. Diabetes 2005;54:1763–1769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Denner L, Bodenburg Y, Zhao JG, Howe M, Cappo J, Tilton RG, Copland JA, Forraz N, McGuckin C, Urban R: Directed engineering of umbilical cord blood stem cells to produce C-peptide and insulin. Cell Proliferation 2007;40:367–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Beilhack GF, Scheffold YC, Weissman IL, Taylor C, Jerabek L, Burge MJ, Masek MA, Shizuru JA: Purified allogeneic hematopoietic stem cell transplantation blocks diabetes pathogenesis in NOD mice. Diabetes 2003;52:59–68 [DOI] [PubMed] [Google Scholar]
- 7. Hess D, Li L, Martin M, Sakano S, Hill D, Strutt B, Thyssen S, Gray DA, Bhatia M: Bone marrow-derived stem cells initiate pancreatic regeneration. Nat Biotechnol 2003;21:763–770 [DOI] [PubMed] [Google Scholar]
- 8. Limbert C, Päth G, Jakob F, Seufert J: Beta-cell replacement and regeneration: Strategies of cell-based therapy for type 1 diabetes mellitus. Diabetes Res Clin Pract 2008;79:389–399 [DOI] [PubMed] [Google Scholar]
- 9. Hussain MA, Theise ND: Stem-cell therapy for diabetes mellitus. Lancet 364:203–205 [DOI] [PubMed] [Google Scholar]
- 10. Couri CE, Foss MC, Voltarelli JC: Secondary prevention of type 1 diabetes mellitus: stopping immune destruction and promoting beta-cell regeneration. Braz J Med Biol Res 2006;39:1271–1280 [DOI] [PubMed] [Google Scholar]
- 11. Ende N, Chen R, Reddi AS: Effect of human umbilical cord blood cells on glycemia and insulitis in type 1 diabetic mice. Biochem Biophys Res Commun 2004;325:665–669 [DOI] [PubMed] [Google Scholar]
- 12. Haller M, Viener H, Brusko T, Wasserfall C, McGrail K, Staba S, Cogle C, Atkinson M, Schatz D: Insulin requirements, HbA1c, and stimulated C-peptide following autologous umbillical cord blood transfusion in children with type 1 diabetes (Abstract). Diabetes 2007;56(Suppl. 1):A82 [Google Scholar]
- 13. Viener H, Brusko T, Wasserfall C, McGrail K, Staba S, Cogle CA, MA, Schatz D, Haller M: Changes in regulatory T cells following autologous umbillical cord blood transfusion in children with type 1 diabetes (Abstract). Diabetes 2007;56(Suppl. 1):A82 [Google Scholar]
- 14. Voltarelli JC, Couri CE, Stracieri AB, Oliveira MC, Moraes DA, Pieroni F, Coutinho M, Malmegrim KC, Foss-Freitas MC, Simões BP, Foss MC, Squiers E, Burt RK: Autologous nonmyeloablative hematopoietic stem cell transplantation in newly diagnosed type 1 diabetes mellitus. JAMA 2007;297:1568–1576 [DOI] [PubMed] [Google Scholar]
- 15. Godfrey WR, Spoden DJ, Ge YG, Baker SR, Liu B, Levine BL, June CH, Blazar BR, Porter SB: Cord blood CD4(+)CD25(+)-derived T regulatory cell lines express FoxP3 protein and manifest potent suppressor function. Blood 2005;105:750–758 [DOI] [PubMed] [Google Scholar]
- 16. Fruchtman S: Stem cell transplantation. Mt Sinai J Med 2003;70:166–170 [PubMed] [Google Scholar]
- 17. Han P, Hodge G, Story C, Xu X: Phenotypic analysis of functional T-lymphocyte subtypes and natural killer cells in human cord blood: relevance to umbilical cord blood transplantation. Br J Haematol 1995;89:733–740 [DOI] [PubMed] [Google Scholar]
- 18. Haller MJ, Viener HL, Wasserfall C, Brusko T, Atkinson MA, Schatz DA: Autologous umbilical cord blood infusion for type 1 diabetes. Exp Hematol 2008;36:710–715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Group D-S. The Diabetes Prevention Trial Type 1 Diabetes (DPT-1). Diabetes 1994;43(Suppl. 1):159A [Google Scholar]
- 20. Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA: Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 1998;338:1650–1656 [DOI] [PubMed] [Google Scholar]
- 21. Brusko T, Atkinson M: Treg in type 1 diabetes. Cell Biochem Biophys 2007;48:165–175 [DOI] [PubMed] [Google Scholar]
- 22. Brusko T, Wasserfall C, McGrail K, Schatz R, Viener HL, Schatz D, Haller M, Rockell J, Gottlieb P, Clare-Salzler M, Atkinson M: No alterations in the frequency of FOXP3+ regulatory T-cells in type 1 diabetes. Diabetes 2007;56:604–612 [DOI] [PubMed] [Google Scholar]
- 23. Brusko TM, Wasserfall CH, Clare-Salzler MJ, Schatz DA, Atkinson MA: Functional defects and the influence of age on the frequency of CD4+ CD25+ T-cells in type 1 diabetes. Diabetes 2005;54:1407–1414 [DOI] [PubMed] [Google Scholar]
- 24. Smith L, Haller MJ, Staba-Kelly S: Characteristics and cell composition of privately banked autologus cord blood (UCB) units utilized for autologous infusion in children with type I diabetes. Biol Blood Marrow Transplant 2008;14:75 18158964 [Google Scholar]
- 25. Schatz D, Gale EA, Atkinson MA: Why can't we prevent type 1 diabetes?: maybe it's time to try a different combination. Diabetes Care 2003;26:3326–3328 [DOI] [PubMed] [Google Scholar]