Abstract
Purpose
Behçet's disease (BD) is a chronic, relapsing, multi-system vasculitis of unknown aetiology with complicated and diversified clinical features predominantly involving oral and genital ulcers, and ocular and cutaneous lesions. The clinical features of this disease have been described to be different according to geographical areas and gender. We investigated the specific clinical features of BD patients in Northeastern China.
Materials and Methods
116 patients involved in this study fulfilled the classification criteria of the International Study Group for BD. The clinical manifestations and results of laboratory tests of BD were recorded in each patient.
Results
The onset was typically between 20-39 years with a slight female predominance. Oral ulcers were the most common manifestation, followed by skin lesions, positive pathergy reaction/genital ulcers, and ocular lesions. Vascular lesion and epididymitis were rare in patients with BD. The frequency of erythema nodosum-like lesion and articular involvement were significantly higher in females, while gastrointestinal involvement was significantly higher in males. The results of laboratory tests showed that the human leukocyte antigen (HLA)-B*51 alleles were positive in 30.9% of patients and the immunological abnormities were present in some patients.
Conclusion
The clinical features of BD showed geographical and gender difference. Genetic and immune factors might participate in aetiopathogenesis of BD.
Keywords: Behçet's disease, clinical feature, autoimmune disease
INTRODUCTION
Behçet's disease (BD) is a chronic, relapsing, multi-system inflammatory disorder of unknown aetiology with complicated and diversified clinical features of mucocutaneous lesions and ocular, vascular, articular, gastrointestinal, urogential, pulmonary and neurological involvement.1-5 The pathogenesis of BD is probably mediated by a combination of factors involving genetic factors, immune factors, environmental factors and infectious agents.6 The disease exhibits a distinct geographic variation. It is particularly prevalent along the ancient "Silk Road" countries from Northwest China to the Mediterranean basin, although BD has been reported all over the world. Turkey has the highest incidence of BD in the world (80-300 per 100,000).1 In contrast, the prevalence is quite low in USA (1 : 1, 500,000).7 Some clinical features of this disease have been described to be different according to the geographical areas.1,2 The pathergy reaction is considered to be highly sensitive and specific for BD in patients from Japan and Turkey and is rare in patients from Western countries, the frequency of gastrointestinal involvement is much lower in the Mediterranean than that in Far East, ocular involvement is more severe in Japanese patients compared with that in patients from the United Kingdom. Moreover, regional differences in the prevalence of the disease within a country have been reported from Korea and Japan.8,9 The clinical feature of BD also shows a gender difference.10-12 Male preponderance has been reported in the Middle Eastern countries, but women are more commonly affected in Japan and Korea.2,12 Eye disease, arthritis, folliculitis and vascular involvement are more common among males, while erythema nodosum were more frequent in females11,12 The mean age at the onset of patients with the worst prognosis is younger in males.12 Because of the lack of a universally recognized pathognomonic laboratory test, the diagnosis of BD is mainly based on the characteristic clinical features and criteria plus the judgment of experienced physicians through mucocutaneous manifestations. In 1990, the International Study Group for BD proposed the criteria for the diagnosis that have been accepted and used worldwide.13
We aimed to investigate the specific clinical features of BD patients in Northeastern China so as to make sure whether there are gender differences in clinical features of BD and try to identify the effects of various factors, such as genetic, and immune factors in aetiopathogenesis of BD. China is one of East Asian countries, near Korea and Japan. We also compared the results with those of various areas in China, Korea and Japan in the literature in order to find out geographical differences in clinical features of BD.
MATERIALS AND METHODS
Subjects
Total 116 patients with BD (52 male, 64 female) who attended the Department of Dermatology, No.1 Hospital of China Medical University in Shenyang, China and Department of Dermatology, No.1 Affiliated Hospital of Dalian Medical University in Dalian, China between 2002 and 2006, fulfilled the classification criteria of the International Study Group for BD13 and were involved in the study. The presence, absence and characteristics of each clinical manifestation were evaluated by specialists of related symptoms such as ophthalmologist for ocular lesion, and rheumatologist for articular involvement. The pathergy reaction was performed using a 20-gauge needle which was intradermally introduced obliquely on the flexor forearm under sterile conditions and read 24-48 h later by a physician. The appearance of a papule or pustule was considered to be a positive reaction.
Laboratory tests
Laboratory tests of all the patient with BD were carried out in the Clinical Laboratory, and Immunology Laboratory of Department of Dermatology, No.1 Hospital of China Medical University, and included blood and urine routine examination, erythrocyte sedimentation rate (ESR), serum immunoglobulin (Ig)G, IgA, IgM, C3, C4, antinuclear antibody (ANA), anti-double stranded DNA (ds DNA) antibody and anti-extractable nuclear antigen (ENA) antibodies. In addition, HLA-B typing in 68 patients was performed by LABType™ SSO method in Liaoning Province Blood Center. One hundred ethnically and regionally matched, unrelated healthy voluntary blood donors served as controls.
Statistical analysis
The t test was used to analyze the continuous variables. The chi-square test was used to analyze the categorical variables. Differences were defined as statistically significant at p < 0.05. All data were assessed on computer using a SPSS 12.0 software package.
RESULTS
Clinical manifestations
All 116 patients with BD (52 male, 64 female: male to female ratio of 0.81) were 5-60 years of disease onset (mean ± SD age 28.0 ± 12.4 years) with no significant difference (p > 0.05) between male (26.5 ± 13.1 years) and female patients (29.2 ± 12.0 years). There were 32 patients with disease onset at below 20 years, 67 patients at 20-39 years, 15 patients at 40-59 years and 2 patient over 60 years. There were no significant differences (p > 0.05) between male (6.1 ± 5.3 years) and female patients (6.4 ± 7.8 years) among BD patients with the duration of 0.25-30 years (6.2 ± 6.3 years).
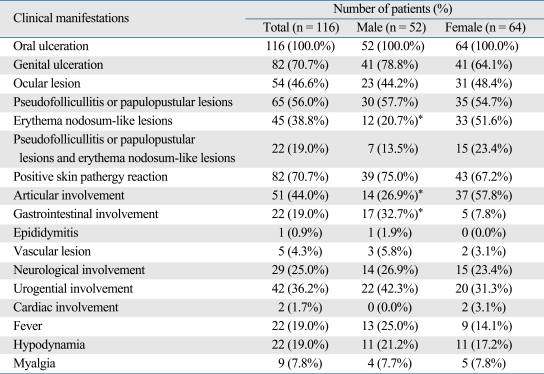
The clinical findings in 116 patients with BD are shown in Table 1. Oral ulcers were seen in all 116 patients with BD during the clinical course and were the initial symptom of the disease in 100 patients (86.2%). Oral ulcers often appeared in buccal mucosa, gingivae, tongue, lips and soft palate. Ninety four (81.0%) of 116 patients with BD had cutaneous lesions, mainly manifesting as pseudofollicullitis or papulopustular lesions, erythema nodosum-like lesions and erythema multiforme-like lesions, whereas a minority as ecchymosis, blister, ulcer, psoriasisform lesions and sweet disease-like lesions. Female patients with nodosum-like lesions were significantly higher than males (p < 0.05). Eighty two (70.7%) of 116 patients with BD had positive skin pathergy reaction. Of 116 patients, 82 patient (70.7%) were found to have genital ulcers. Genital ulcers were the initial manifestation of 10 patients (9.5%) with BD, commonly seen in scrotum, penis and glans in male and labia, vagina and cervix uteri in female. Fifty four (46.6%) of 116 patients with BD had ocular lesions, including posterior uveitis such as retinal vasculitis, vitritis, optic neuritis and anterior uveitis, including iridocyclitis, hypopyon, conjunctivitis, keratitis, and scleritis.
Table 1.
The Clinical Manifestations in 116 Patients with BD
BD, Behçet's disease.
*p < 0.05 indicated that male patients were significantly different from female patients.
Involvement of the joint occurred in 51 patients (44.0%), manifesting asymmetric arthritis. The most common site was knees, followed by the ankles, elbows, wrists and coxa. Joint involvement was more frequent in females than in males (p < 0.05). Twenty two patients with gastrointestinal involvement had the symptoms of abdominal pain, distension, discomfort, diarrhea, constipation, and hematochezia. Eight male patients among them were found with gastric/duodenal ulcer, revealed by gastroscopy, and 1 female patients with colonic ulcer was confirmed by colonoscopy. Gastrointestinal involvement was more frequent in males than in females (p < 0.05). Of 116 patients, only 1 patient (0.9%) suffered from epididymitis, complaining of swelling and pain. Five patients (4.3%) were found to have vascular lesion, occurring in lower limbs as superficial thrombophlebitis. Twenty nine patients (25.0%) were found with neurological involvement, and most of them with feeled headache and dizzy. Only two patients had severe symptoms: one with psychiatric symptoms and the other with unstable walk and trouble in speaking, and magnetic resonance imaging showed brain atrophy. Forty two patients (36.2%) with urogential involvement manifested asymptomatic proteinuria and/or simple hematuria. Two case (1.7%) were found with cardiac involvement, and both of them felt recurrent precordial distress and electrocardiogram showed myocardial ischemia. In addition, 22 patients (19.0%) with fever, 22 patients (19.0%) with hypodynamia, and 9 patients (7.8%) with myalgia were included.
Moreover, we found that 15 patients (12.9%: 8 male, 7 female) had family history of recurrent oral ulcer in their first-degree relatives, in which 4 (3.4%) were confirmed BD cases.
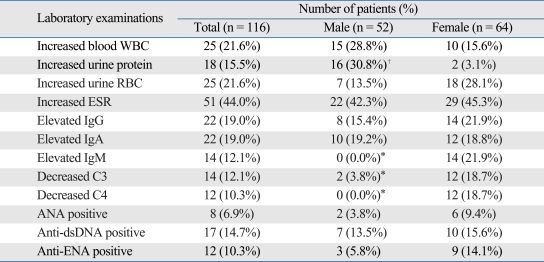
Laboratory examinations
Peripheral blood WBC in 25 of 116 patients (21.6%) was increased, and 18 patients (15.5%) showed increased urine protein ranging from trace (150 mg/24 h) to 2+, and increased urine protein was more frequent in males than in females (p < 0.05). Twenty five patients (21.6%) had increased urinary red blood cell (RBC), 51 patients (44.0%) increased ESR, 22 cases (19.0%) IgG type, 22 cases (19.0%) IgA type, and 14 cases (12.1%) IgM type. Increased IgM was more frequent in females than in males (p < 0.05). C3 was decreased in 14 cases (12.1%), while C4 in 12 cases (10.3%). Decreased C3 and C4 were more frequent in females than in males (p < 0.05, respectively). The positive rates of ANA, anti-dsDNA, and anti-ENA were 6.9%, 14.7% and 10.3%, respectively (Table 2).
Table 2.
The Results of Laboratory Examinations
WBC, white blood cell; RBC, red blood cell; ESR, erythrecyte sedimentation rate, Ig, immunoglobulin, ANA, antinuclear antibody; ds-DNA, double stranded DNA; ENA, extractable nuclear antigen.
*p < 0.05, †p < 0.01 indicated that male patients were significantly different from female patients.
Total 68 patients and 100 controls were studied for HLA-B alleles, in which 21 patients (30.9%) and 12 controls (12%) had positive HLA-B*51 alleles. The gene frequency of HLA-B*51 was significantly higher in BD patients than those in controls (p < 0.05). The frequency of HLA-B*51 alleles in male and female patients was 35.1% and 25.8%, respectively, indicating no gender difference (p > 0.05).
DISCUSSION
In this study, we evaluated clinical features of BD patients in Northeastern China, and also compared the results with those of various areas in China, Korea, and Japan. The comparative data of clinical features of BD are presented in Table 3.14-18 It suggested that there were certain differences in clinical features of BD among different regions in East Asia.
Table 3.
Clinical Features in Different Regions of East Asia
*described as skin lesions.
In our study, recurrent oral ulceration was the most common basic symptom, followed by skin lesions, genital ulceration/positive skin pathergy reaction, and ocular lesion. Oral ulcerations were found in 100% of patients, indicating key bases of diagnosing BD. Genital ulceration was less significant, compared with oral ulceration. Solitary genital ulceration hardly suggested BD, and diagnosis could not easily be made based on genital ulceration, and similar diseases should be ruled out. Pseudofollicullitis and papulopustular lesions were frequent occurrence in skin lesions, followed by erythema nodosum-like lesions. These results differed from those in other parts of China,16-18 however, similar with the report from Turkey.19 It was quite common for ocular lesion to be a slight symptom. Since only 6 patients with ocular involvement were severe: 3 cases with iridocyclitis, one case with hypopyon, iridocyclitis, lens opacity and vitreous opacity, one case with vitreous opacity, and corneal macula, and another one with secondary complications of cataract and maculopathy. Five above-mentioned cases were treated timely with corticosteroids and didn't lose their eyesight during follow-up. Pathergy, the occurrence of a pustular lesion 24 hours after cutaneous trauma, has been found to be useful as a diagnostic marker in some studies. In 1990, the International Study Group Criteria were published to include a positive pathergy test as one of the criteria to establish the diagnosis of BD. It is thought to denote increased neutrophi chemotaxis with an infiltration of polymorphonuclear leukocytes (PMNLs) first followed by mononuclear and mast cells.20 It is also related with disease activity and systemic involvement. Although positive pathergy reaction occurs much more commonly in Turkish and German,19,21 it only occurs in about 15% of Korean patients,14 and 44% of Japanese patients,15 reducing its diagnostic value in these groups. In our study we found pathergy in 82 of 116 patients with BD, and it also showed a high incidence in other regions of China,16-18 suggesting that it has a diagnostic value and is specific to BD in China.
The major pathologic process of BD is vasculitis characterized by multisystemic involvement. Our results showed that articular, urogential, neurological and gastrointestinal involvements were common, however, the prevalence of epididymitis, vascualr and cardic involvement was low. Pulmonary involvement was not found. As many as 44.0% of patients with BD had arthritis. The knees and ankles were most commonly involved, although smaller joints also were affected in a few patients. The arthritis was typically oligoarticular in the majority of patients. No patients experienced destructive, deforming arthritis of small joints. Spondyloarthristides was not seen. Renal vasculitis was characterized by diffuse or focal glomerular abnormalities. Although renal involvement was common in the present study, most patients with renal involvement had slight symptoms and showed mild proteinuria and microscopic hematuria with normal renal function, consistent with previous report.22 Gastrointestinal involvement in BD is characterized by ulceration along the gastrointestinal tract, and we found 8 patients with gastric/duodenal ulcer, 1 patient with colonic ulcer, and other patients with functional abnormalities. Most neurological manifestations of this group of patients included headaches and dizzy without specificity. Only 2 cases showed serious symptoms, and brain stem involvement was not seen. Epididymitis and vascular involvements were also rare: only one patient suffered from epididymitis, similar to reports from Korea,14 and 5 patients were found to have superficial thrombophlebiti. Further follow-up will be required to investigate whether other vascular involvement experiences longer time.
The diagnosis of BD has been based on clinical criteria and no pathognomonic laboratory fingdings. Several laboratory tests have been studied, but none has been found to be specific for BD. Abnormal values such as leukocytosis, increased erythrocyte sedimentation rate, and elevated IgG, IgA, and IgM are often seen in disease exacerbations. In our study, the presence of elevated IgG, IgA, and IgM, and decreased C3, C4 and some autoantibody such as ANA, anti-dsDNA and anti-ENA indicated that immunological mechanisms might play a major part in aetiopathogenesis of BD. HLA-B*51, the genetic marker of BD, has been reported to exhibit strong association with the disease in different ethnic groups.23 The frequency of HLA-B*51 in patients with BD was 25-80%.24-28 HLA-B*51 in the present study was positive in 30.9% of BD patients, while the frequency of HLA-B*51 alleles in controls was only 12%. On the other hand, familial recurrent oral ulcer was described in 12.9% of patients with BD. These results suggested that genetic factor might be associated with BD. The difference in the frequency of HLA-B*51 between our study and literatures indicated that the association between HLA-B*51 and BD had ethnic and geographic differences. Our findings suggested that both genetic and environmental factors might contribute to the occurrence and development of the disease.
The clinical features of BD are different according to the gender.10-12 In the present study, female patients were slightly more than males, however, there were no differences in mean age of disease onset and mean duration between male and female patients. These results differed from previous observation on a lower age of BD onset in men.29 As for clinical findings, female patients with nodosum-like lesions were significantly higher than males. The difference in oral ulcers, genital ulcers, ocular lesion, and positive skin pathergy reaction between male and female patients could not be found. Nevertheless, genital ulcers occurring in women were usually deeper and larger than those in men, while 6 patients with serious ocular involvement were all men. The strong reaction of skin pathergy such as pustule formation was significantly more common in male patients. There was no difference in other manifestations between male and female patients, apart from joint involvement which was more common in women, and gastrointestinal involvement which was more common in men. Eight patients with gastric/duodenal ulcer were all male, while only one female patient with colonic ulcer was found. Laboratory test showed that more male patients than female ones were positive for increased urine protein, but female patients were more than male ones for elevated IgM and decreased C3, and C4. Although positive HLA-B*51 was encountered more commonly in male patients in the current study, there was no statistical significance.
With regard to the treatment of this group of patients, tripterygium wilfordii, compound Glycyrrhizin, and transfer factor were effective for mucococutaneous manifestation. Systemic corticosteroids and/or immunosuppressive agents, including azathioprine, methotrexate, cyclophosphamide, cyclosporin, and immunomodulators including interferon, were used when eye, brain, kidney and gastrointestinal tract were severely involved and genital ulcerations were large, deep and severely painful. Non-steroidal anti-inflammatory drugs were also an effective alterative treatment for joint involvement and erythema nodosum-like lesion. At the same time, topical therapy was administered. These treatments seemed to be variably effective without obvious side-effects during follow-up.
ACKNOWLEDGEMENTS
The authors thank Ning Zhai, Department of Dermatology, NO.1 Hospital of China Medical University, and Jianping Li, Liaoning Provincial Blood Center for their excellent technical assistance.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Sakane T, Takeno M, Suzuki N, Inaba G. Behçet's disease. N Engl J Med. 1999;341:1284–1291. doi: 10.1056/NEJM199910213411707. [DOI] [PubMed] [Google Scholar]
- 2.Kaklamani VG, Vaiopoulos G, Kaklamanis PG. Behçet's disease. Semin Arthritis Rheum. 1998;27:197–217. doi: 10.1016/s0049-0172(98)80001-2. [DOI] [PubMed] [Google Scholar]
- 3.Yurdakul S, Hamuryudan V, Yazici H. Behcet syndrome. Curr Opin Rheumatol. 2004;16:38–42. doi: 10.1097/00002281-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Krause I, Leibovici L, Guedj D, Molad Y, Uziel Y, Weinberger A. Disease patterns of patients with Behçet's disease demonstrated by factor analysis. Clin Exp Rheumatol. 1999;17:347–350. [PubMed] [Google Scholar]
- 5.Yazici H, Yurdakul S, Hamuryudan V. Behçet's disease. Curr Opin Rheumatol. 2001;13:18–22. doi: 10.1097/00002281-200101000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Ghate JV, Jorizzo JL. Behçet's disease and complex aphthosis. J Am Acad Dermatol. 1999;40:1–18. doi: 10.1016/s0190-9622(99)70523-2. [DOI] [PubMed] [Google Scholar]
- 7.Chamberlain MA. Behçet's syndrome in 32 patients in Yorkshire. Ann Rheum Dis. 1977;36:491–499. doi: 10.1136/ard.36.6.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang HK, Kim JW. The clinical features of Behçet's disease in Yongdong districts: analysis of a cohort followed from 1997 to 2001. J Korean Med Sci. 2002;17:784–789. doi: 10.3346/jkms.2002.17.6.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamamoto S, Toyokawa H, Matsubara J. A nationwide survey of Behcet's disease in Japan. Jap J Opthalmol. 1974;18:282–290. [Google Scholar]
- 10.Evereklioglu C. Current concepts in the etiology and treatment of Behçet disease. Surv Ophthalmol. 2005;50:297–350. doi: 10.1016/j.survophthal.2005.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Yazici H, Tüzün Y, Pazarli H, Yurdakul S, Ozyazgan Y, Ozdoğan H, et al. Influence of age of onset and patient's sex on the prevalence and severity of manifestations of Behçet's syndrome. Ann Rheum Dis. 1984;43:783–789. doi: 10.1136/ard.43.6.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bang DS, Oh SH, Lee KH, Lee ES, Lee SN. Influence of sex on patients with Behçet's disease in Korea. J Korean Med Sci. 2003;18:231–235. doi: 10.3346/jkms.2003.18.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Study Group for Behçet's disease. Criteria for diagnosis of Behçet's Disease. Lancet. 1990;335:1078–1080. [PubMed] [Google Scholar]
- 14.Bang D, Lee JH, Lee ES, Lee S, Choi JS, Kim YK, et al. Epidemiologic and clinical survey of Behcet's disease in Korea: the first multicenter study. J Korean Med Sci. 2001;16:615–618. doi: 10.3346/jkms.2001.16.5.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nakae K, Masaki F, Hashimoto T, Inaba G, Mochizuki M, Sakane T. Recent epidemiological features of Behçet's disease in Japan. In: Wechsler B, Godeau P, editors. Behçet's disease. Amsterdam: Excerpta Medica; 1993. pp. 145–151. [Google Scholar]
- 16.Dai Lie, Tang Meian, Yin Peida, Liu Yaguang. Clinical analysis on 60 case of Behcet's disease. Chin J Rheumatol. 1997;2:13–16. [Google Scholar]
- 17.Liu Xiangyuan, Li Shengguang, Shi Guiying, Huang Cibo, Yuan Guohua, Huang Feng. Comparative study on male and female patients with Behcet's disease. Chin J Rheumatol. 2000;4:82–84. [Google Scholar]
- 18.Chen Lan, Ye Lan, Chen Xinping, Xu Zhusen. A retrospective study on 58 patients with Behcet's disease. Chin J Lepr Skin Dis. 2003;19:25–27. [Google Scholar]
- 19.Gürler A, Boyvat A, Türsen U. Clinical manifestations of Behçet's disease: an analysis of 2147 patients. Yonsei Med J. 1997;38:423–427. doi: 10.3349/ymj.1997.38.6.423. [DOI] [PubMed] [Google Scholar]
- 20.Ozen S. Vasculopathy, Behçet's syndrome, and familial Mediterranean fever. Curr Opin Rheumatol. 1999;11:393–398. doi: 10.1097/00002281-199909000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Zouboulis CC, Kötter I, Djawari D, Kirch W, Kohl PK, Ochsendorf FR, et al. Epidemiological features of Adamantiades-Behçet's disease in Germany and in Europe. Yonsei Med J. 1997;38:411–422. doi: 10.3349/ymj.1997.38.6.411. [DOI] [PubMed] [Google Scholar]
- 22.Grenier P, Bletry O, Cornud F, Godeau P, Nahum H. Pulmonary involvement in Behcet disease. AJR Am J Rosentgenol. 1981;137:565–569. doi: 10.2214/ajr.137.3.565. [DOI] [PubMed] [Google Scholar]
- 23.Mizuki N, Inoko H, Mizuki N, Tanaka H, Kera J, Tsuiji K, et al. Human leukocyte antigen serologic and DNA typing of Behçet's disease and its primary association with B51. Invest Ophthalmol Vis Sci. 1992;33:3332–3340. [PubMed] [Google Scholar]
- 24.Verity DH, Wallace GR, Vaughan RW, Kondeatis E, Madanat W, Zureikat H, et al. HLA and tumour necrosis factor (TNF) polymorphisms in ocular Behçet's disease. Tissue Antigens. 1999;54:264–272. doi: 10.1034/j.1399-0039.1999.540307.x. [DOI] [PubMed] [Google Scholar]
- 25.Mizuki N, Ohno S, Ando H, Chen L, Palimeris GD, Stavropoulos-Ghiokas E, et al. A strong association between HLA-B*5101 and Behçet's disease in Greek patients. Tissue Antigens. 1997;50:57–60. doi: 10.1111/j.1399-0039.1997.tb02835.x. [DOI] [PubMed] [Google Scholar]
- 26.Kötter I, Günaydin I, Stübiger N, Yazici H, Fresko I, Zouboulis CC, et al. Comparative analysis of the association of HLA-B*51 suballeles with Behçet's disease in patients of German and Turkish origin. Tissue Antigens. 2001;58:166–170. doi: 10.1034/j.1399-0039.2001.580304.x. [DOI] [PubMed] [Google Scholar]
- 27.Choukri F, Chakib A, Himmich H, Hüe S, Caillat-Zucman S. HLA-B*51 and B*15 alleles confer predisposition to Behçet's disease in Moroccan patients. Hum Immunol. 2001;62:180–185. doi: 10.1016/s0198-8859(00)00249-4. [DOI] [PubMed] [Google Scholar]
- 28.Kilmartin DJ, Finch A, Acheson RW. Primary association of HLA-B51 with Behçet's disease in Ireland. Br J Ophthalmol. 1997;81:649–653. doi: 10.1136/bjo.81.8.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krause I, Uziel Y, Guedj D, Mukamel M, Molad Y, Amit M, et al. Mode of presentation and multisystem involvement in Behçet's disease: the influence of sex and age of disease onset. J Rheumatol. 1998;25:1566–1569. [PubMed] [Google Scholar]