Abstract
Objective
The primary aim of this study was to examine whether one week of continuous auricular acupuncture could reduce low back and posterior pelvic pain associated with pregnancy.
Study Design
A randomized controlled trial was conducted on pregnant women suffering from lower back and posterior pelvic pain. These women were randomized into an acupuncture group, a sham acupuncture group, or a waiting list control group. All participants were followed for 2 weeks.
Results
Baseline and Day 7 showed significant group differences in pain [F= 15, P<0.0001] and in the disability rating index score [F=7, p<0.0001]. The participants in the acupuncture group reported a significant reduction of pain and improvement of functional status as compared to those in the sham acupuncture and control groups.
Conclusion
One week of continuous auricular acupuncture decreases the pain and disability experienced by women with pregnancy related low back and posterior pelvic pain.
Keywords: Auricular acupuncture, pregnancy related low back pain and posterior pelvic pain, pain relief, pregnancy
Introduction
Low back pain is the second most common neurological ailment in the United States1 and pregnancy is also considered as one of the major contributing factors to the development of this clinical entity.2.3 Pregnancy-related low back and posterior pelvic pain (PRLP) consists of generalized lower back pain and distinct pains located in the posterior pelvic area distal and lateral to the lumbar-sacral junction.4 In the United States, more than 2 million pregnant women are affected by PRLP annually2 and PRLP is reported to be one of the most common reasons for sick leave during pregnancy.5–7 The current literature supports that the earlier the onset of PRLP, the more severe the pain and disability becomes as the pregnancy progresses and the greater the incidence of prolonged postpartum low back pain and chronic low back pain.8 Further more, 10–20% of women suffering from chronic low back pain report that the onset of the pain originated during their pregnancy.9
Chronic/recurrent low back pain is often initiated by an acute episode of low back pain with local irritation and inflammation followed by immobilization and abnormal posture caused by this pain.10 The immobilization and abnormal posture leads to worsening of local irritation and inflammation, ultimately resulting in the development of chronic low back pain.11 If an effective intervention that reduces pain is applied at the onset of acute low back pain, it may facilitate the early resumption of daily activities and lead to a decrease in the incidence of recurrent and chronic low back pain.10,11 The introduction of drug therapy during pregnancy, however, is challenging due to the uniqueness of the maternal-fetal circulation and the potential for drug transfer to the fetus.12 This means that non-pharmacological treatment for PRLP is potentially very attractive, both as a means to decrease pain during pregnancy and also to decrease the risk of chronic back pain throughout life. Although massage, yoga, acupuncture and related interventions have been recommended as potential treatments for this clinical entity,13–15 there is a paucity of randomized control trials to support the benefit of using any of these interventions in pregnant women. In fact, two recent review articles reveal that there is an urgent need for high quality clinical trials in the evaluation of the current treatment options for PRLP. 14,15
Several clinical studies and two review articles indicate that traditional body acupuncture may serve as a treatment for PRLP,14–19 but only one study has used auricular acupuncture as an adjunct for body acupuncture. Wedenberg and colleagues16 showed that the combination of auricular and body acupuncture was superior to physiotherapy in relieving the severity of pain and the disability related to PRLP but the intervention protocol was very time consuming, often consisting of 1 hour treatments and 10 treatments per month of acupuncturist office visits. Sato-Katzenschlager et al.20 demonstrated that auricular acupuncture was effective in providing relief to non-pregnant patients with chronic back pain. Auricular acupuncture21 is preferable to body acupuncture because it is easy to apply without undressing the patient or utilizing sophisticated needle manipulations as in traditional body acupuncture. Lastly, the use of auricular press needles (Small, Seirin Pyonex; Shizuoka, Japan) (Figure 1) allows the provision of continuous acupuncture intervention while the patient continues with her daily activities. These observations provided the basis for this study of whether auricular acupuncture alone can be used as a treatment for PRLP.
Figure 1.
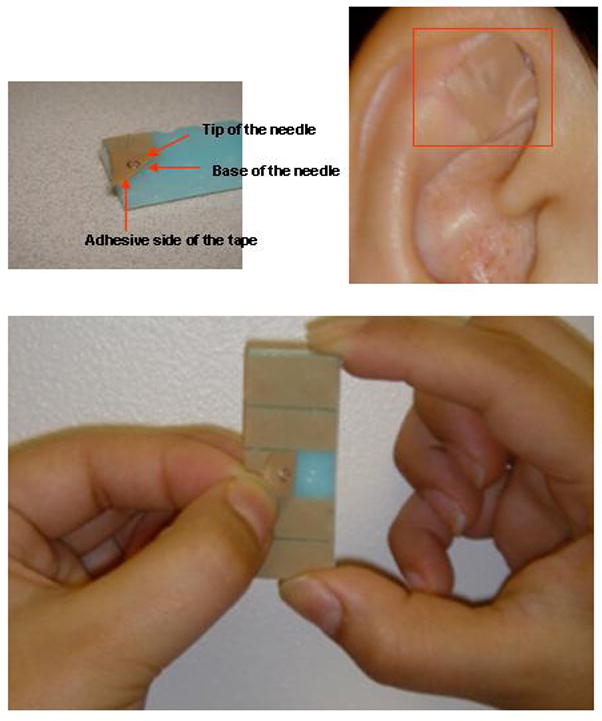
The press needle-semi-permanent needles
The primary hypothesis of this study is that one week of continuous acupuncture stimulation at three specific auricular points will reduce the severity of pain in pregnant women with late trimester PRLP. The secondary hypothesis of this study is that an effective reduction of pain caused by PRLP would be concomitant with an improvement in the functional status of these women.
Material and Methods
Design and Settings
This randomized controlled clinical trial was conducted at The Center for The Advancement of Perioperative Health at Yale New Haven Hospital after obtaining approval from Human Investigation Committee at Yale University School of Medicine. Participants were randomized to receive one of the following three interventions; a) acupuncture at specific auricular points, b) acupuncture at non-specific auricular points, or c) no-intervention control. To reduce bias affecting the study results, all prospective participants were informed that they had a 33.3% chance of receiving no treatment until after the completion of a 2-week study period.
Subjects
Participants were pregnant women with a gestational age of 25 to 38 weeks who suffered from lower back and/or posterior pelvic pain. All participants were healthy women with a physical status II in the American Society of Anesthesiologists (ASA) classification, and had no prior experience with acupuncture. PRLP was classified based on the classification defined by Norén22 and exclusion criteria included any associated nerve root syndrome, neurological deficit, fever, abdominal pain, other systemic manifestations and active uterine contractions.
Group Assignments
Acupuncture group
Participants in this group received auricular press needles at three points (kidney, analgesia, and shenmen) (Figure 2). These points were selected not only based on the close location to the auricular somatotopic map of the hip and the lumbar spine21 but were also pre-tested on 50 pregnant women with PRLP during the preparation phase of this randomized trial by our research group.
Figure 2.
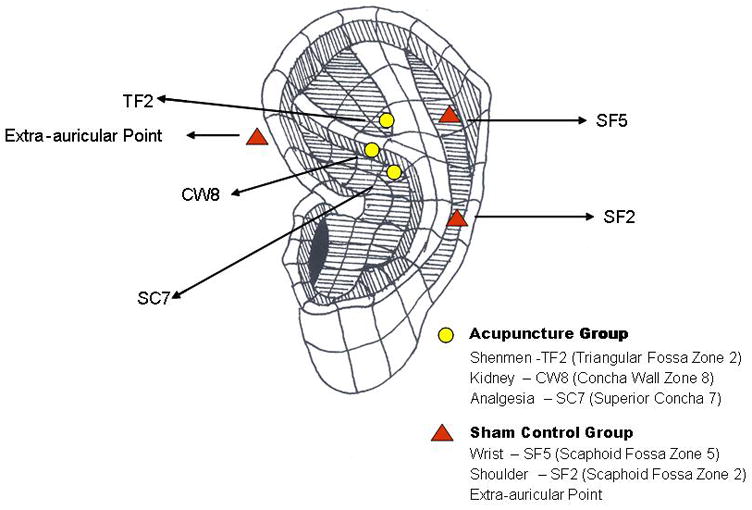
The locations of auricular acupuncture points
Sham acupuncture group
Participants in this group received auricular press needles at three non-specific auricular acupuncture points (shoulder, wrist and extra-auricular point) that were used in previous studies and showed a minimum effect (Figure 2).23,24 The sham acupuncture group was included as a control to address issues specifically related to the clinical acupuncture trial such as placebo effects, blinding and subject’s beliefs.
Control group
Participants in this group received no acupuncture treatment. No treatment control group was included because several clinical acupuncture studies have suggested that any needle intervention might result in some physiological responses and pain relief.25
Measures
Background Characteristic
The questionnaire was designed to gather demographic information as well as State and Trait Anxiety Inventory (STAI).26
Visual Analog Scale for Pain (VAS-P):27
The VAS rating system consists of a 100 mm line that represents 2 extremes, i.e. no pain (a score of 0) and extreme pain (a score of 100). There are ample data regarding the excellent reliability and validity of this instrument.
Disability Rating Index (DRI):28
This instrument contains twelve common daily activities and requires the participants to rate their level of disability in each activity with 0 denoting no disability, and 100 denoting maximum disability (i.e., inability). The measure has demonstrated satisfactory test-retest and inter/intra-rater reliabilities, and internal consistency.
Study Protocol
Prenatal health care providers referred all participants to the study who suffered from back pain without any suspected obstetric and/or medical reasons. Prospective participants were instructed by their prenatal care providers to call the PRLP hotline where a research assistant would explain the nature of the study and conduct a preliminary interview of participants’ symptoms and conditions. If inclusion criteria were met, the women were invited to participate in the study and verbal consent was obtained. Prospective participants followed up with an appointment with one of the physician co-investigators for further evaluation and possible enrollment. A detailed history and a general physical examination combined with special focus on neurological testing pertinent to back and lower extremities were conducted to ensure these potential participants met the enrollment criteria. After this evaluation, one pregnant woman was referred for further workup because of the more complicated nature of her back pain and one pregnant woman decided not to participate in the study because she was not comfortable signing the HIPPA consent.
Once a participant was enrolled, a written consent was obtained and baseline assessments of anxiety (STAI), pain (VAS-P), and functional status (DRI) were completed. Participants were randomized into one of the three treatment groups based on a computer generated randomization sheet. The acupuncturist (SMW)* applied three auricular press needles to the respective auricular points in the acupuncture and sham acupuncture groups based upon the randomization scheme. Because of the inconsistencies and non-specifics of commercial-made skin conductors in the literature,29 the auricular points used were identified based on the auricular zone system.21 In order to avoid any bias caused by the acupuncturist and the assessor (research assistant), the acupuncturist adhered to scripted speech during interaction with the participants and inserted the needles without the presence of the assessor. If a participant was to receive acupuncture or sham acupuncture treatment, the acupuncturist told her that a total of three auricular press needles would be inserted into one side of her ear and these needles would be left in place for a one-week period before being removed. After the placement of these auricular press needles, the acupuncturist instructed the participants to inspect the integrity of the occlusive tape over these needles daily but not to apply any pressure or manipulation over the needle insertion site. If any adverse reaction such as local redness or increased pain occurred, the participant was instructed to contact the study center immediately and return for reinspection, adjustment, and/or possible removal of the press needles. All participants including those in the control group were told that they would be asked to report their average level of pain (VAS-P) and functional status (DRI) on day 7 and again their average level of pain on day 14 after enrollment in the study. The assessor telephoned every participant including participants in the control group daily over the study period to ensure the study protocol was followed. The participants in the control group, after the two week observation, were offered to return to the center and receive auricular acupuncture treatment.
All participants were directed to adhere to PRLP self-care i.e. continuing to rest as desired, taking acetaminophen 650 mg every 6 hours if needed, and/or applying topical warm and cold compresses to relieve low back pain during the two week study period. However, participants were instructed not to use any other complementary and alternative treatments (CAM) such as massage, chiropractic manipulations, or physical therapy.
Blinding and Credibility
To test blinding to treatment and to assess the credibility of the respective treatment methods,30–32 all participants that received auricular acupuncture treatment were asked to complete a credibility questionnaire (appendix I) on day 7 after the removal of auricular press needles. All assessors were blinded to the group assignment. The statistician who performed the final analysis was blinded to the group assignment.
Sample Size and Statistical Analysis
The primary aim of this study was to compare one-week changes from baseline in pain scores measured by a VAS-P. The secondary aims for this study were to assess the functional status of the participants one week after intervention as measured by DRI, and to determine the therapeutic effect of a one-week auricular intervention. Sample size was calculated using Sample Power statistical software version 1.2 (SPSS Inc, Chicago, IL). A 30% reduction in VAS-P (primary outcome)33 from the baseline was considered to be clinically meaningful for the purpose of the study. The estimated standard deviation of change from baseline is about 25 for VAS in a previous study.16 As enrollment gestational age in this study ranged from 25 weeks to 38 weeks, we stratified participants into 3 groups: 25–29 weeks gestation, 30–34 weeks gestation and 35–38 weeks gestation. With a power of 0.85 and a significance level of 0.05, calculations based on previous data yielded a sample size of 135 women for the trial. Given an estimated dropout rate of 15%, however, we recruited an additional 24 patients for a total of N=159.
Baseline demographic data, prognostic variables, and credibility evaluations were compared using t-tests and chi-square tests as deemed appropriate. A mixed effect model with random intercept analysis34 was performed for the outcomes and the therapeutic effect of 1-week intervention predictors included the indicator variables of all three groups, at Day 7 and Day 14, and the interaction terms between the indicator variables of time and group. Subject was treated as a random effect to account for within-subject correlation. If any measure for a time point was missing, the mixed model accounted for the mechanism of missing-at-random. After an overall test of treatment effect, Fischer’s protected test was used for pairwise comparisons to determine the group differences. P less than 0.05 was considered significant and SPSS was used for analysis (SPSS Inc, Chicago, IL).
Results
Between February 1, 2005 and January 31, 2008, a total of 311 pregnant women with lower back/posterior pelvic pain were referred as potential participants for this study. Following an initial telephone screening, 172 subjects who had met the inclusion criteria were invited to participate in the study. A total of 161 subjects presented for the pre-enrollment appointment, 159 subjects enrolled into the study and 152 subjects completed the two-week study period (retention rate of 95.6%)(Figure 3). There were no significant differences in baseline variables between the three study groups (Table 1).
Figure 3.
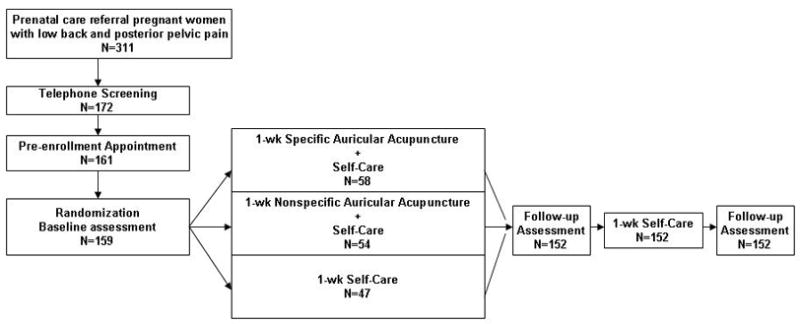
Trial flow chart
Table 1.
Baseline Characteristics of the participants
| Acupuncture Group (N=58) | Sham Acupuncture Group (N=54) | Control Group (N=47) | |
|---|---|---|---|
| Age, mean(SD), yr | 33(5) | 32(5) | 32(5) |
| Gestational Age(%) | |||
| 25–29 wk | 42 | 40 | 51 |
| 30–34 wk | 36 | 42 | 30 |
| 35–38 wk | 22 | 18 | 19 |
| mean(SD), wk | 30(5) | 29(7) | 29(5) |
| Location of pain(%) | |||
| Lumbar back pain (LBP) | 47 | 38 | 57 |
| Posterior pelvic pain((PPP) | 42 | 38 | 28 |
| LBP+PPP | 6 | 8 | 11 |
| Nonspecific lower back pain | 5 | 0 | 4 |
| Previous lower back pain(%) | |||
| Yes | 47 | 46 | 55 |
| No | 53 | 54 | 45 |
| Previous pregnancy lower back pain(%) | |||
| Yes | 26 | 28 | 20 |
| No | 21 | 29 | 24 |
| Not applicable | 53 | 43 | 56 |
| First pregnancy(%) | |||
| Yes | 53 | 43 | 56 |
| No | 47 | 57 | 44 |
| Beliefs in acupuncture, mean(SD) | 7(2) | 7(2) | 7(2) |
| Baseline Anxiety | |||
| State, mean(SD) | 35(9) | 35(9) | 38(11) |
| Trait, mean(SD) | 37(8) | 37(8) | 37(9) |
| Education level, mean(SD), yr | 16(3) | 16(3) | 16(3) |
| Baseline VAS-Pain, mean(SD) | 70(20) | 62(22) | 66(26) |
| Baseline DRI, mean(SD) | 63(25) | 57(28) | 63(28) |
No statistically differences between the groups, P>.05
Primary Outcome
Pain at Day 7
As can be seen in Figure 4, participants in all groups reported a decrease in pain in varying degrees [F=186, p<0.0001] and the participants in the acupuncture group reported a significant reduction in pain as compared to those of the sham acupuncture group (p=0.001) and those of the control group (p<0.0001). In contrast, the reduction of pain between the sham acupuncture and control groups (p=0.46) was not significant. A mixed model analysis demonstrated that there is a significant group × time interaction [F=15, P<0.0001]. More participants in the acupuncture group had a clinically significantly reduction in pain (e.g. 30% reduction) than those of the sham acupuncture group and the control group (81% vs. 59% vs. 47%, p=0.015). In addition, 37% of participants in the acupuncture group, 22% of participants in the sham acupuncture group and 9% of participants in the control group became pain-free (VAS-P score=0) at day 7 (p=0.003).
Figure 4.
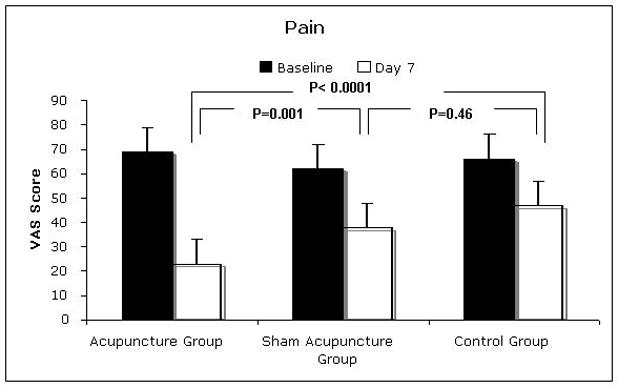
The level of pain at baseline and Day 7
Secondary Outcomes
a. Functional Status at Day 7
Similarly, all the participants, regardless of their group assignment, reported improvement in the functional status after the first week [F=126, p<0.0001]. As can be seen in Figure 5, participants in the acupuncture group reported a significant improvement of functional status as compared to those of sham acupuncture and control groups, p=0.03 and p=0.001, respectively. In contrast, the differences of functional status between the sham acupuncture and control groups did not reach statistical significance (p=0.60). A mixed model analysis reveals a significant group × time interaction [F=7, p<0.0001].
Figure 5.
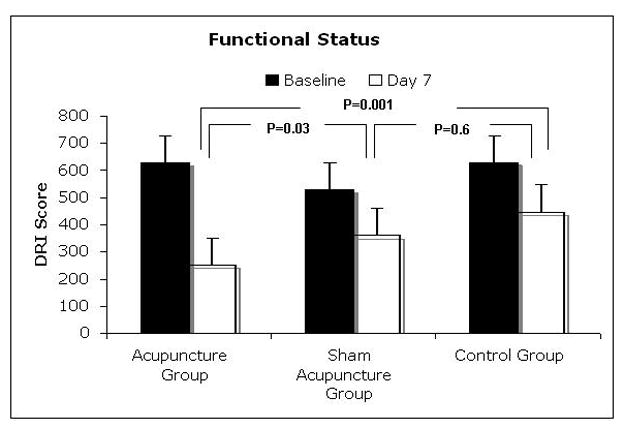
The functional status at baseline and Day 7
b. Therapeutic Outcome During 2-Week Study Period
A mixed model analysis indicated a significant reduction of pain over time [F=42.7, p<0.0001] in all three groups and a significant group × time interaction [F=4.7, p=0.013] (Figure 6). At Day 14, 68% of participants in the acupuncture group had a clinically significant reduction of pain while only 32% of participants in the sham acupuncture group (p=0.02) and 18% of participants in the control group had a clinically significant reduction of pain (p<0.001). However, the number of participants who remained pain-free at Day 14 did not show a significant difference among the groups (16% vs. 9% vs. 6%, p =0.25).
Figure 6.
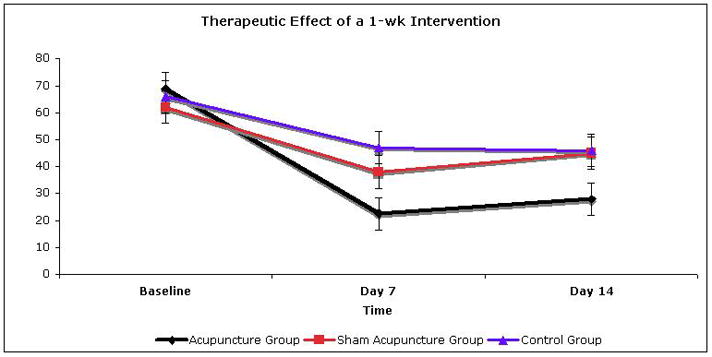
The therapeutic effect of 1-week intervention
Only three participants in the study (acupuncture vs. sham acupuncture vs. control =1 vs. 2 vs. 0) used acetaminophen as an adjunct for pain treatment. The total consumption of acetaminophen ranged between 1300 mg to 1950 mg and none of the participants reported that acetaminophen was helpful for their back pain.
Adverse Effects Experienced During Study Period and Postpartum
During the first week of the study period, 1/54 participants in acupuncture group and 3/50 participants in the sham acupuncture group experienced transient ear tenderness that resolved spontaneously. No participants experienced preterm labor. However, 1/54 participants in the acupuncture group, 1/50 participants in the sham acupuncture group, and 1/47 participants in the control group were placed on bed rest later after the study period was completed. No adverse pregnancy outcomes were reported.
Comment
Under the conditions of this study, we found that pregnant women who received a one-week continuous auricular acupuncture treatment reported significantly less pain as compared to those of the sham acupuncture and control groups. At the Day 7 follow-up, we found that about 80% of the participants in the acupuncture group experienced a clinically significant reduction in pain as compared to 56% of participants in the sham acupuncture group and 36% of participants in the control group. This clinically important outcome was associated with an improvement in functional status as the pain decreased. The reduction of pain continued to the Day 14 follow-up. However, the reduction of pain was not sustained for every participant, as the number of the participants who remained pain-free was fewer at Day 14 than Day 7. This observation suggests that after removing press needles, there was a returning of pain in some of the participants. Thus it is important to explore whether an extended continuous auricular acupuncture is needed to have a sustained effect as well as the characteristics of acupuncture responders vs. non-responders in future studies.
Since there are no safety data using auricular press needles in delivering auricular acupuncture continuously in pregnant women, we chose one week as the treatment period, which was derived from our clinical experience as a conservative treatment duration. Based on the results of this study, we are confident that a one-week auricular acupuncture can be safely administered in pregnant women with low back and posterior pelvic pain at the last trimester of pregnancy, since we did not observe any major local irritation, infection, or adverse outcome in pregnancy. For a majority of participants receiving therapeutic acupuncture, pain relief was substantial and led to improvement of functional status. Hence, this study supports that use of acupuncture at specific auricular points is a safe and effective non-pharmacologic treatment of an important clinical entity for which there are currently few, if no effective treatments. Interestingly, participants in the control group also experienced reduction of pain without additional treatment other than PRLP-self care. This reduction of pain may be caused by the self-care package prescribed in this study or by the daily inquiry performed by the assessor, or the combination of both. The psychological impact and effect of daily inquiry should be assessed in a future study. While an economical analysis was beyond the scope of this study, the cost for the auricular acupuncture press needle is about $17–20 dollars for 100/pack and this intervention can be administered in 3 minutes by an experienced operator Thus, a future, large-scale randomized controlled trial is definitely indicated to confirm the potential benefits of using this intervention.
Other methodological issues related to this study that should be addressed are: (1) Issues related to VAS-P as the primary measuring tool for pain disorders. Although pain disorders are generally considered to have more than one dimension, e.g. affective and sensory aspects, we used the VAS-P as the assessment tool for the primary outcome of this study because it is not only effective in assessing the improvement of pain in clinical settings,33, 35–37 but also is well defined in assessing the clinical significance of pain reduction.33 Thus, the results of this study can be more meaningful for the practitioners who encounter PRLP on a daily basis. As pain disorders are usually complex, VAS-P might not be ideal. Future studies should also consider additional multi-dimensional pain assessment tools such as the Brief Pain Inventory,38 McGill Pain Scale,39 etc. to address different aspects of pain. (2) Issues related to credibility testing. While the credibility test is critical in assessing the successfulness of blinding for clinical acupuncture studies,25 auricular acupuncture performed in this study is different from the traditional acupuncture, e.g. the type and manipulation of needles as well as the duration of the needles’ retention. Furthermore, there are no data in the literature to determine whether the intervention technique and duration introduced in this study are acceptable treatment strategies for pregnant women with PRLP. Thus, some of the questions in the credibility test32 were modified to answer our inquiry. (3) Issues related to single acupuncturist. Although only one acupuncturist performed all the auricular acupuncture interventions, the participants not only think the treatment strategy was acceptable but also believe the intervention they received improved their lower back and pelvic pain regardless of the group assignment (both the acupuncture and sham acupuncture groups). Therefore, we are confident that neither the acupuncturist nor the intervention selected in this study introduced any bias to the participants who received the auricular acupuncture intervention or affected the validity of the study results.
In summary, we found that the participants who received a one-week continuous acupuncture treatment at the specific auricular points had a significant reduction in pain as compared to those of the sham acupuncture and control groups, but the treatment effect was not sustained in some of the pregnant women. Thus, long-term efficacy of auricular acupuncture as a treatment for pregnancy related lower back and posterior pelvic pain is still inconclusive but clearly shows promise. A future large-scale randomized control study is indicated to explore the characteristics of acupuncture responders vs. non-responders, the optimal duration of treatment to achieve the sustained therapeutic effect, and the potential mechanisms of auricular acupuncture analgesia as well as detailing the pregnancy outcomes.
Table 2.
Credibility Test
| Acupuncture Group (N=54) | Sham Acupuncture Group (N=50) | P | |
|---|---|---|---|
| Think the treatment received is a reasonable strategy | 9(2) | 8(2) | 0.2 |
| Relieves lower back pain | 8(3) | 7(3) | 0.2 |
| Will use the treatment again | 9(3) | 9(2) | 0.9 |
| Will recommeded to a friend | 9(2) | 8(3) | 0.6 |
| Satisfied with the treatment | 8(3) | 8(3) | 0.6 |
All Rating scale based on 0=not at all and 10=definitely; data are mean(SD)
Acknowledgments
Financial support and role of funding source: This study is supported by National Center for the Complementary and Alternative Medicine R21 AT001613-03. The sponsor of this study had no role in study design, data collection, data analysis and data interpretation or writing of the reports. The authors have full access to all the data in the study and the corresponding author is responsible for the decision to submit for publication.
The investigators would like to express our gratitude to the referring network of prenatal care providers and participants for their support as well as Dr. James Dziura at the Yale Center for Clinical Trial for statistical support and Mrs. Annette Forte, for her administrative assistance.
APPENDIX
Answer each question by circling the number that seems to best fit your opinion about the acupuncture treatment you received:
| 1. Did this seem like a reasonable strategy to reduce the level of low back pain during pregnancy? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| reasonable | very reasonable | ||||||||
| 2. How much did this treatment help you reduce your low back pain? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| not at all | very much so | ||||||||
| 3. Would you recommend this treatment to a friend who might be having low back pain during pregnancy? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| would not recommend | definitely would recommend | ||||||||
| 4. Was this treatment what you had expected? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| not what I expect | just what I expect | ||||||||
| 5. Was the time involved reasonable? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Unreasonable | very reasonable | ||||||||
| 6. If you had more back pain in the future, would you try this treatment again? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| not at all | definitely | ||||||||
| 7. How satisfied are you with this way of treating low back pain? | |||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| not at all | very Satisfied | ||||||||
Footnotes
The acupuncturist (SMW) is a board certified anesthesiologist and a certified acupuncturist who has 9 years of clinical acupuncture experience.
Presentation: Partial data were presented at the American Society of Anesthesiology Annual Meeting October 2007. San Francisco, CA.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Peggy Dizinno, Women’s Education and life Learning Center, Yale-New Haven Hospital. New Haven, CT 06520
Eric C. Lin, Department of Anesthesiology, Yale School of Medicine, New Haven, CT 06520
Haiqun Lin, Department of Epidemiology and Public Health, Yale School of Medicine. New Haven, CT 06520
James J. Yue, Department of Orthopaedics and Rehabilitation, Yale School of Medicine. New Haven, CT 06520.
Michael R. Berman, Department of Obstetrics and Gynecology, Yale School of Medicine., New Haven, CT 06520
Ferne Braveman, Departments of Anesthesiology and Obstetrics and Gynecology, Yale School of Medicine. New Haven, CT 06520.
Zeev N. Kain, Departments of Anesthesiology, Pediatrics, Psychiatry and Human Behavior, University of California School of Medicine. Irvine, CA 92603
References
- 1.Data adopted from the National Institutes of Neurological disorders and stroke. www.ninds.nih.gov.
- 2.Ostgaard HC, Anderson GBJ, Karlson K. Prevalence of back pain in pregnancy. Spine. 1991;16:95–101. doi: 10.1097/00007632-199105000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Wang SM, Dezinno P, Maranets I, et al. Low back pain during pregnancy: prevalence, risk factors, and outcomes. Obstet Gyn. 2004;104:65–70. doi: 10.1097/01.AOG.0000129403.54061.0e. [DOI] [PubMed] [Google Scholar]
- 4.Norén L, Ostgaard S, Johansson G, Ostgaard HC. Lumbar back and posterior pelvic pain during pregnancy: a 3-year follow-up. Eur Spine J. 2002;11:267–71. doi: 10.1007/s00586-001-0357-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Synsjo A, Sydsjo G, Wijma B. High Sick leave during pregnancy in an extensive compensation system. Lakartidningen. 1989;86:4141–4. [PubMed] [Google Scholar]
- 6.Noren L, Ostgaard S, Nielsen T, Ostgaard HC. Reduction of sick leave for lumbar back and posterior pelvic pain in pregnancy. Spine. 1997;22:2157–60. doi: 10.1097/00007632-199709150-00013. [DOI] [PubMed] [Google Scholar]
- 7.Sydsjo A, Sydsjo G, Wijma B. Increase in sick leave rates caused by back pain among pregnant Swedish women after amelioration of social benefit. Spine. 1998;23:1986–90. doi: 10.1097/00007632-199809150-00014. [DOI] [PubMed] [Google Scholar]
- 8.Brynhildsen J, Hansson A, Persson A, Hammar M. Follow up of patients with low back pain during pregnancy. Obstet Gyn. 1998;91:182–6. doi: 10.1016/s0029-7844(97)00630-3. [DOI] [PubMed] [Google Scholar]
- 9.Sevensson HO, Andersson GB, Hagstad A, Jasson PO. The relationship of low-back pain to pregnancy and gynecologic factors. Spine. 1990;15:371–5. doi: 10.1097/00007632-199005000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Swinkels-Meewisse IE, Roelofs J, Oostendorp RA, et al. Acute low back pain: pain related fear and pain catastrophizing influence physical performance and perceived disability. Pain. 2006;120:36–43. doi: 10.1016/j.pain.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Langevin HM, Sherman KJ. Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Med Hypothesis. 2007;68:74–80. doi: 10.1016/j.mehy.2006.06.033. [DOI] [PubMed] [Google Scholar]
- 12.Rathmell JP, Viscomi CM, Ashburn MA. Management of Non-obstetric pain during pregnancy and lactation. Anesth Analg. 1997;85:1074–87. doi: 10.1097/00000539-199711000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Wang SM, DeZinno P, William K, et al. Complementary medicine and alternative medicine for low back pain in pregnancy- A cross sectional survey. J Altern Complem Med. 2005;11:459–64. doi: 10.1089/acm.2005.11.459. [DOI] [PubMed] [Google Scholar]
- 14.Pennick V, Young G. Interventions for preventing and treating pelvic and back pain in pregnancy. The Cochrane Database Syst Rev. 2007;2:CD001139. doi: 10.1002/14651858.CD001139.pub2. (Review) [DOI] [PubMed] [Google Scholar]
- 15.Ee CC, Manheimer E, Pirotta MV, Whilte AR. Acupuncture for pelvic and back pain in pregnancy: a systemic review. AJOG. 2008;198:254–259. doi: 10.1016/j.ajog.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Wedenberg K, Moen B, Norling A. A prospective randomized study comparing acupuncture with physiotherapy for low-back and pelvic pain in pregnancy. Acta Obstet Gyn Scan. 2000;79:331–5. [PubMed] [Google Scholar]
- 17.Kvorning N, Holmberg C, Grenner L, et al. Acupuncture relieves pelvic and low back pain in late pregnancy. Acta Obstet Gynecol Scan. 2004;83:246–50. doi: 10.1111/j.0001-6349.2004.0215.x. [DOI] [PubMed] [Google Scholar]
- 18.Elden H, Ladfors L, Olsen M, et al. Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. Brit Med J. 2005;330:761–5. doi: 10.1136/bmj.38397.507014.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lund I, Lundeberg T, Lonnberg L, Svensson E. Decrease of pregnant women’s pelvic pain after acupuncture: a randomized controlled single-bind study. Acta Obstet Gynecol Scan. 2006;85:12–9. doi: 10.1080/00016340500317153. [DOI] [PubMed] [Google Scholar]
- 20.Sator-Katzenschlager S, Szeles J, Scharbert G, et al. Electrical stimulation of auricular acupuncture points is more effective than conventional manual auricular acupuncture in chronic cervical pain: a pilot study. Anesth Analg. 2003;97:1469–73. doi: 10.1213/01.ANE.0000082246.67897.0B. [DOI] [PubMed] [Google Scholar]
- 21.Oleson T. Auriculotherapy manual: Chinese and Western Systems of ear acupuncture. 2. Los Angeles: Health Care Alternative; 1996. [Google Scholar]
- 22.Norén L, Östgaard S, Nelsen TF, Östgaard HC. Reduction of sick leave for lumbar back and posterior pelvic pain in pregnancy. Spine. 1997;22:2157–60. doi: 10.1097/00007632-199709150-00013. [DOI] [PubMed] [Google Scholar]
- 23.Wang SM, Peloquin C, Kain ZN. The use of auricular acupuncture to reduce preoperative anxiety. Anesth Analg. 2001;93:1178–80. doi: 10.1097/00000539-200111000-00024. [DOI] [PubMed] [Google Scholar]
- 24.Wang SM, Maranets I, Weinberg ME, et al. Parental auricular acupuncture as an adjunct for parental presence during induction of anesthesia. Anesthesiology. 2004;100:1399–404. doi: 10.1097/00000542-200406000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Birch S, Hammerschlag R, Trinh K, Zaslawski C. The non-specific effects of acupuncture treatment: When and how to control for them. Clin Acup Orient Med. 2002;3:20–25. [Google Scholar]
- 26.Spielberger C. Pal Alto. California: Consulting Psychologist Press; 1983. Manual for state-trait anxiety inventory (STAI: Form Y) [Google Scholar]
- 27.Abu-Saas H. Assessing children’s responses to pain. Pain. 1984;19:163–71. doi: 10.1016/0304-3959(84)90836-4. [DOI] [PubMed] [Google Scholar]
- 28.Salén B, Spangfort E, Nygren A, Nordemar R. The disability rating index: An instrument for the assessment of disability in clinical setting. J Clin Epidemiol. 1994;47:1423–34. doi: 10.1016/0895-4356(94)90086-8. [DOI] [PubMed] [Google Scholar]
- 29.Ahn A, Colbert A, Anderson B, et al. Electrical Properties of acupuncture points and meridians: A systemic review. Bioelectromagnetics. 2008;29:245–56. doi: 10.1002/bem.20403. [DOI] [PubMed] [Google Scholar]
- 30.Borkovec TD, Nau SD. Credibility of analogue and therapy rationales. J Behav Ther Exp Psy. 1972;3:257–60. [Google Scholar]
- 31.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psy. 2000;31:73–86. doi: 10.1016/s0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- 32.Vincent C. Credibility assessment in trials of acupuncture. Complem Med Res. 1990;4:8–11. [Google Scholar]
- 33.Turner JA, Turk DC. The significance of clinical significance. Pain. 2008;137:467–8. doi: 10.1016/j.pain.2008.03.029. [DOI] [PubMed] [Google Scholar]
- 34.Fitzmaurice G, Molenberghs G. Advances in longitudinal data analysis. In: Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G, editors. Longitudinal Data Analysis: A Handbooks of Modern Statistical Methods. Boca Raton: Chapman & Hall/CRC; 2008. pp. 7–8. [Google Scholar]
- 35.Gallagher EJ, Bijur PE, Latimer C, Silver W. Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Am J Emer Med. 2002;20:287–90. doi: 10.1053/ajem.2002.33778. [DOI] [PubMed] [Google Scholar]
- 36.Gift AG. Visual Analog Scale for measurement of Subjective. Phenomena. 1989;38:286–288. [PubMed] [Google Scholar]
- 37.Bidian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain. Anesthesiology. 2001;95:1356–61. doi: 10.1097/00000542-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 38.Keller S, Bann C, Dodd S. Validity of the Brief Pain Inventory for use in clinical trials of nonmalignant pain therapy. Qual Life Res. 2000;9:245–367. [Google Scholar]
- 39.Melzack R. The Short-Form McGill pain questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]


