Abstract
State tobacco control programs provide an important laboratory for the development, implementation, and evaluation of comprehensive tobacco control interventions. Studies have demonstrated that states and municipalities with aggressive tobacco control programs have experienced more rapid decreases in per capita cigarette sales, smoking prevalence, lung cancer, and heart disease than entities without such programs. Despite strong evidence that population-level interventions are critical in achieving large and sustained reductions in tobacco use, states do not fund tobacco control efforts at levels recommended by the CDC. Research on the effectiveness and cost-effectiveness of these activities is essential to inform and strengthen tobacco control at the state-level. A workshop, co-organized by ACS, NCI, AACR, and CDC, was held in Philadelphia in December, 2007 to discuss the topic “Linking tobacco control policies and practices to early cancer endpoints: Surveillance as an agent for change”. Participants represented three different disciplines. Tobacco surveillance researchers described the data currently collected on state-level tobacco control policies, pro-tobacco countermeasures by the industry, public attitudes towards tobacco use and measures of smoking prevalence and consumption. Cancer registry experts described the geographic coverage of high quality, population-based cancer registries. Mathematical modeling experts discussed various modeling approaches that can be used to relate upstream tobacco promotion and control activities to downstream measures such as public attitudes, changes in tobacco use, and trends in tobacco-related diseases. The most important recommendation of the Workshop was a call for national leadership to enhance the collection and integration of data from multiple sources as a resource to further study and strengthen the scientific basis for tobacco control.
Background
The history of tobacco control over the last two decades has demonstrated that policy-level interventions are critical to achieve large scale reductions in tobacco usage [1–5]. Effective measures include excise taxes to increase the price of tobacco products, state and local ordinances that prohibit smoking in public spaces and protect non-smokers from second-hand smoke, mass media campaigns that change social norms about smoking, and comprehensive state tobacco control programs that help to integrate these activities, promote partnerships and strengthen tobacco control capacity at the state level. All of these measures attack the root causes of tobacco use, i.e. the cultural, social, economic, political and physical factors that influence whether adolescents initiate tobacco use or addicted smokers successfully quit.
Substantial evidence demonstrates that states and municipalities with aggressive tobacco control programs have experienced more rapid decreases in per capita cigarette sales, smoking prevalence, lung cancer, and heart disease than states or communities without such programs [4–6]. This evidence has prompted the Institute of Medicine (IOM) [2], the Centers for Disease Control (CDC) [3], and the National Cancer Institute [1,7] to recommend policy interventions that, if implemented, would further reduce tobacco use and the resultant burden of tobacco-related diseases in the United States. Despite this, states have been slow to implement such programs, do not fund tobacco control at levels recommended by the CDC, and investment in tobacco control programs by most States remained flat or decreased from 2002 to 2006 [8].
It is essential that population-level, tobacco control interventions continue to be evaluated for their effectiveness and cost-effectiveness in the prevailing environment of shrinking public health resources and unstable funding. Tobacco control can be analyzed on multiple levels. State-level programs, the focus of this Workshop, provide an unusual opportunity for such evaluations, due to the diversity of the programs and the availability of surveillance data for many of the relevant parameters. Many factors complicate these evaluations, however. Tobacco control programs may involve a patchwork of state and local laws that change over time and include a mix of policy, media, and programmatic components. There is no standardized approach for weighting the separate components or for integrating these into a combined summary index [1]. States vary with regard to the public’s and government’s receptivity of tobacco control policies. The quality and coordination of state tobacco control activities are more difficult to measure than their quantity in terms of budget and/or staff. Little information is publically available on promotional activities by the tobacco industry, especially within states [9,10]. These can include point of sale discounts, coupons and advertising in local communities [11] or glamorization of smoking in movies that are distributed nationally [12]. Downstream changes in tobacco use or disease endpoints often occur first in certain age and socioeconomic subgroups, rather than simultaneously across the entire population, and may coincide with other changes in the population [1].
The statistical approaches used to model these dynamic relationships are also inherently complex and not well suited to conventional epidemiological approaches [13]. Multiple feedback loops exist by which tobacco control policies influence and are influenced by public attitudes and smoking behaviors [1, 13, 14].
Workshop objectives
The meeting’s objectives were to: 1) review the strengths and limitations of data currently being collected on tobacco control policies, tobacco industry promotional efforts, and indicators of tobacco use at the state and local level (information that is presented in detail elsewhere [15]: 2) describe the current status of population-based cancer registries in the United States and provide guidance about how incidence and mortality data on lung cancer at younger ages (30–39 years) can be linked to surveillance data on tobacco control and promotion at the state level [16]: 3) identify statistical modeling approaches that can relate upstream events (tobacco control and tobacco promotion) to various indices of tobacco use and/or early adverse health consequences: and 4) encourage greater use of surveillance data and statistical modeling to assess the impact of population-level interventions on public attitudes about tobacco, usage patterns and early cancer endpoints.
Conceptual models of nicotine addiction and tobacco control
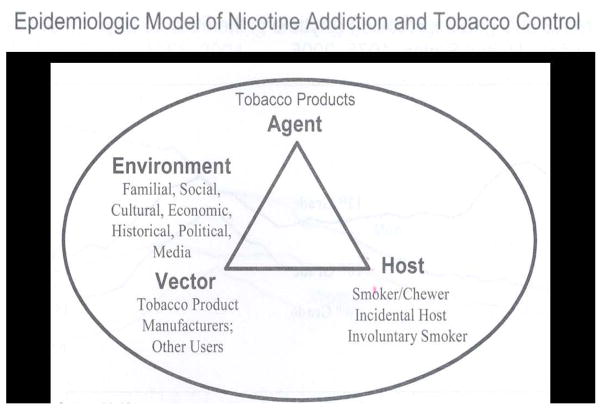
The first session of the Workshop was organized according to an epidemiological model originally proposed by Orleans and Slade [17], that characterizes the basic elements of nicotine/tobacco addiction in terms conventionally reserved for infectious disease epidemics (Figure 1) [14]. These include agent, vector, host, and environment.
Figure 1.
In this instance, the agent represents tobacco products rather than a microbial pathogen, the vector represents the manufacturers and producers of these products, and the host represents the consumer who uses these products, or the bystander who is involuntarily exposed to smoke. Transmission of exposure to tobacco use, experimentation, and addiction is facilitated or inhibited by factors in the familial, social, cultural, political and economic environment. These include interventions that increase excise taxes, strengthen smoke-free legislation, expand tobacco cessation services, and counter pro-tobacco influences. While there appears to be little variation in tobacco products among states, there are major differences in state-level tobacco control activities, many components of which are measured by ongoing surveillance activities [15]. Various indices of tobacco use have been measured at the state level for almost two decades and are readily available on the internet [15, 18–20]
In contrast, little state-level information is available to health researchers regarding pro-tobacco activities by the tobacco companies. These include price-oriented activities (coupons, free samples, point of sale discounts), promotional activities at the retail and wholesale level, sponsorships and direct mail, political contribution and campaigns to defeat smoke free initiatives, and image oriented activities such as glamorization of smoking in movies. Data that are collected are typically limited and dispersed across multiple sources that are not publically accessible [10].
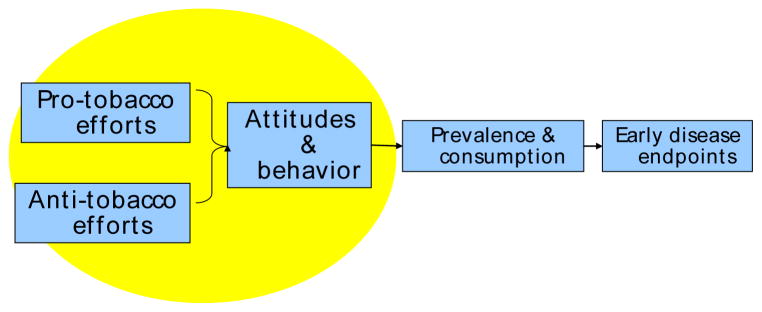
A second only slightly less basic model is shown in Figure 2 which adds the link to disease endpoints. Figure 2 also explicitly highlights the opposing influences of pro- and anti-tobacco efforts which together with “Attitudes and Behavior” are enclosed in a circle that represents prominent feedback loops and interactions. This model presumes a sequence of events in which factors considered to be “upstream” (pro- and anti-tobacco activities) affect first the intermediate “downstream” sequellae (attitudes, beliefs, social norms and measures of tobacco usage), and ultimately the disease endpoints related to tobacco. Figure 2 recognizes the importance of feedback loops in which tobacco control programs influence social norms, expectations, self-efficacy, and receptivity [2, 5], and these in turn affect public support for such programs. However, it too oversimplifies the complexity of these dynamic relationships. Each of the major components and transitions could be further subdivided to indicate the various stages of addiction, attitudinal and behavioral changes, continuation or cessation of smoking, disease development and ultimately death.
Figure 2.
Basic Conceptual Framework for Modeling
Cancer Registry and State Cancer Profiles Data
Speakers described the coverage of state and national cancer registry programs that could be used for analyses of trends in tobacco related cancers, particularly lung cancer in young adults. The NCI SEER program has monitored cancer trends on approximately ten percent of the U.S. population since 1975 [21] and provides the only data for studying long term trends. The National Program of Cancer Registries (NPCR), with support from CDC, operates population-based registries in 45 states, Metropolitan areas, and the District of Columbia [22]. When combined, the high quality registries of SEER and NPCR in the National Association of Central Cancer Registries (NAACR) now cover approximately 80% of the U.S. population [23] (http://apps.nccd.cdc.gov/uscs/). Cancer registries do not collect information on tobacco use but their data can be used to investigate incidence, mortality, survival, and prevalence and to make projections in the overall population or for demographic groups of interest. Information on how to access registry data is available on NAACCR’s Website (www.naaccr.org). The State Cancer Profiles Web Site (statecancerprofiles.cancer.gov) provides dynamic views of cancer statistics for over 20 cancer sites and risk factors at the national, state, and county level. State and regional data [15, 18–20] can be used to examine relationships between tobacco use, tobacco control policies, socioeconomic factors, and lung cancer. For example, states in the southeastern United States have the highest youth and adult tobacco usage, the lowest tobacco excise taxes, weakest clean indoor air laws, highest poverty rates, lowest education, and highest lung cancer rates.
Modeling Tobacco Control & Health Outcomes
Various modeling approaches have been used to study the complex interactions between policies and smoking behaviors or health endpoints in subgroups of the population over time. The program SimSmoke [24] simulates cigarette use and smoking-related deaths over time at the state or national level. SimSmoke models have been developed at the national level for the U.S. and 11 other countries. Each model begins in a specified year with a population of never-, current, and ex-smokers of various ages. The population then moves through time as initiation, cessation, relapse, births and deaths affect smoking practices. Policy elements include cigarette taxes, media campaigns, clean air laws, youth access policies, and cessation/treatment. The estimates of smoking-attributable deaths depend on smoking rates and relative risks. Smoking data in this model were derived from the Tobacco Use Supplement of the Current Population Survey (TUS-CPS) [20]. Validation of the model considered percent changes in smoking rates over time in the TUS-CPS and Behavioral Risk Factor Surveillance System (BRFSS).
Another statistical modeling endeavor is the Cancer Intervention & Surveillance Modeling Network (CISNET), in which some participating researchers develop models that predict national lung cancer incidence and mortality rates in the United States 1985–2000, based on various hypothetical scenarios of population smoking behavior from 1975–85 [25]. Some of these models, like SimSmoke, focus on upstream factors that affect smoking behavior, whereas others focus on downstream transitions in carcinogenesis [26]. Birth cohort-specific data can be valuable input to models giving important insights that age-related changes over time can miss. One current emphasis is on how growing public awareness of the detrimental effects of tobacco on health, starting in the 1950s, relate to lung cancer risk.
Finally, a model was discussed that illustrates how multiple risk factors and social determinants interact to affect the frequency of cardiovascular events and their direct and indirect costs [27]. The model will ultimately help national, state, and local public health agencies prioritize the allocation of policy resources to influence both individual behaviors (including smoking, diet, and physical activity) and population-level risk factors (including secondhand smoke and particulate air pollution). The model was commissioned in 2007 by the CDC’s Division of Heart Disease and Stroke Prevention, with support from the NIH’s Office of Behavioral and Social Science Research, and in collaboration with researchers and local health officials in Austin, Texas.
Conclusions and recommendations
The central conclusion of the Workshop was that surveillance and research on tobacco control policy interventions comprise a critically important area of health research, on a par with the value of cancer registries and population-based surveillance of risk factors and the utilization of screening tests. Participants called for stronger national leadership and technical and financial support to enhance the collection and integration of data from multiple sources. An inventory of these data has recently been compiled [15], which will facilitate making the information more accessible through either a single platform such as the addition of a population science grid to the NCI caBIG Initiative [28] or linkages with other sources. The most critical gap in surveillance data on tobacco concerns the promotional activities of the tobacco industry at the state and local level. At a minimum, the industry should be required to provide at least annual, state-level data on: (a) political lobbying, campaign contributions, activities to defeat tax increases and smoke-free laws: (b) per capita tobacco marketing expenditures overall, and component amounts for price discounts, email relationships, and direct marketing: and (c) accurate information on the real price of cigarettes and other tobacco products by major brand categories and manufacturer. Reporting should also be required for (a) pro-tobacco advertisements and coverage of tobacco issues within all major media markets (and state estimates where market areas do not conform with state boundaries): and (b) data on screening of movies that contain smoking and audience levels at the state or national level to allow meaningful estimates of population exposure. Such information cannot be obtained without strict regulatory requirements for transparency about tobacco industry promotions at the state and national level, whether by FDA or FTC.
Acknowledgments
This article is the summary of the workshop. The views presented here are those of the authors and not necessarily those of the co-organizing and funding agencies. Financial and staff support for this meeting were provided by the National Cancer Institute, the American Cancer Society and the American Association for Cancer Research.
We wish to acknowledge Drs. Margaret Foti and Andrew Dannenberg for scheduling this Workshop as a satellite meeting of the AACR Frontiers in Cancer Prevention Research conference.
* Organizing Committee
Co-chairs
Anne M. Hartman - National Cancer Institute
Michael J. Thun - American Cancer Society
Members
Rachel Ballard-Barbash - National Cancer Institute
Brenda Edwards - National Cancer Institute
Eric J. Feuer - National Cancer Institute
Lisa N. Haubein - American Association for Cancer Research
Ann Malarcher - Centers for Disease Control and Prevention
Stephen Marcus - National Cancer Institute
Michelle Murray - NOVA Research Company
Terry Pechacek - Centers for Disease Control and Prevention
Dean Post - American Association for Cancer Research
Kathy Sedgwick - NOVA Research Company
Sonja Stringer - National Cancer Institute
Speakers & Facilitators (other than members of the Organizing Committee)
David Abrams - National Institutes of Health (currently at American Legacy Foundation)
Lois Biener - University of Massachusetts at Boston
David Burns - University of California at San Diego
Pamela Clark - Battelle Centers for Public Health Research & Evaluation (currently at University of Maryland, College Park)
Gary Giovino - University at Buffalo, The State University of New York
Jack Homer - Homer Consulting
Holly Howe - NAACCR, Inc.
David Levy - Pacific Institute for Research and Evaluation
Suresh Moolgavkar - Fred Hutchinson Cancer Research Center
Nathaniel Osgood - University of Saskatchewan
John Pierce - University of California at San Diego
Sherri Stewart - Centers for Disease Control and Prevention
David Stinchcomb - National Cancer Institute
Other Acknowledgements
Kathy Sedgwick, Scientific Meeting Recorder/Writer – NOVA Research Company
Stephanie Craver, Travel Meeting Support – National Cancer Institute
Emily Dowling, Administrative Management Support- National Cancer Institute
Shawna Johnson, On-Site Meeting Support – NOVA Research Company
Meredith Morrissette, Meeting Support – National Cancer Institute
Michael Pleasant, Awardee Meeting Support – American Cancer Society
References
- 1.National Cancer Institute. Tobacco Control Monograph 17. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2006. Evaluating ASSIST: A Blueprint for Understanding State-level Tobacco Control. NIH Pub No. 06-6058. [Google Scholar]
- 2.Institute of Medicine. Ending the Tobacco Problem: A Blueprint for the Nation. Washington, D.C.: National Academy Press; 2007. p. 636. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Best Practices for Comprehensive Tobacco Control Programs. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health; Atlanta, GA: 2007. [Google Scholar]
- 4.Messer K, et al. The California Tobacco Control Program’s effect on adult smokers: (1) Smoking cessation. Tob Control. 2007;16(2):85–90. doi: 10.1136/tc.2006.016873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Backinger C, O’Connell M, Warner K, editors. Am J Preventive Med. 6 Suppl. Vol. 33. 2007. National Institutes of Health State-of the Science Statement on Tobacco Use, Prevention, Cessation, and Control; pp. S311–S424. [Google Scholar]
- 6.Jemal A, et al. Annual report to the nation on the status of cancer, 1975–2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Res. 2008 doi: 10.1093/jnci/djn389. (In review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stillman FA, et al. Evaluation of the American Stop Smoking Intervention Study (ASSIST): a report of outcomes. J Natl Cancer Inst. 2003;95(22):1681–91. doi: 10.1093/jnci/djg098. [DOI] [PubMed] [Google Scholar]
- 8.Farrelly MC, et al. The impact of tobacco control programs on adult smoking. Am J Public Health. 2008;98(2):304–9. doi: 10.2105/AJPH.2006.106377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giovino G, Biener L, Hartman AM, Marcus S, Schooley M, Pechacek T, Vallone D. Overview In Monitoring the Tobacco Use Epidemic: Optimizing Measurement to Facilitate Change. Preventive Medicine. 2008;(Suppl) doi: 10.1016/j.ypmed.2008.08.007. (In editorial review) [DOI] [PubMed] [Google Scholar]
- 10.Cruz T. Monitoring the tobacco industry: data sources and recommendations for research. In Monitoring the Tobacco Use Epidemic: Optimizing Measurement to Facilitate Change. Preventive Medicine. 2008;(Suppl) doi: 10.1016/j.ypmed.2008.10.002. (In editorial review) [DOI] [PubMed] [Google Scholar]
- 11.Slater S, Chaloupka FJ, Wakefield M. State variation in retail promotions and advertising for Marlboro cigarettes. Tob Control. 2001;10(4):337–9. doi: 10.1136/tc.10.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charlesworth A, Glantz SA. Smoking in the movies increases adolescent smoking: a review. Pediatrics. 2005;116(6):1516–28. doi: 10.1542/peds.2005-0141. [DOI] [PubMed] [Google Scholar]
- 13.National Cancer Institute. Tobacco Control Monograph 18. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2007. Greater than the Sum: Systems Thinking in Tobacco Control. NIH Pub No. 06-6085. [Google Scholar]
- 14.Giovino G. Background and overview: the tobacco epidemic in the United States. American Journal of Preventive Medicine. 2007;33(6S):S318–326. doi: 10.1016/j.amepre.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 15.Giovino G, editor. Preventive Medicine. Suppl. 2008. Monitoring the tobacco use epidemic: optimizing measurements to facilitate change. (In editorial review) [DOI] [PubMed] [Google Scholar]
- 16.Jemal A, Cokkinedes VE, Shafey O, Thun MJ. Lung cancer trends in young adults: an early indicator of progress in tobacco control. Cancer Causes & Control. 2003;14:579–85. doi: 10.1023/a:1024891201329. [DOI] [PubMed] [Google Scholar]
- 17.Orleans CT, Slade J. Nicotine Addiction: Principles and Management. ix. New York: Oxford University Press 1993; 1993. p. ix. [Google Scholar]
- 18.CDC State Profiles. http://statecancerprofiles.cancer.gov
- 19.CDC State Tobacco Activities Tracking and Evaluation (STATE) System http://www.cdc.gov/tobacco/statesystem and related CDC State Highlights, http://www.cdc.gov/tobacco/data_statistics/state_data/data_highlights/2006/index.htm
- 20.U.S. Department of Commerce, C.B., National Cancer Institute sponsored series of Tobacco Use Supplements to the Current Population Survey (1992–2003); cosponsored with Centers of Disease Control and Prevention 2001–2003: http://riskfactor.gov/studies/tus-cps/. Data files (AND/OR) technical documentation (technical documentation website: http://riskfactor.cancer.gov/studies/tus-cps/info.html).
- 21.Surveillance, Epidemiology, and End Results (SEER) Program, SEER*. Stat Database: Incidence - SEER 9 Regs Public Use, Nov 2007 Sub (1973–2005) National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch; 2008. [Google Scholar]
- 22.U.S. Cancer Statistics Working Group. United States Cancer Statistics: 2002 Incidence and Mortality. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; Atlanta: 2005. [Google Scholar]
- 23.Hotes J, et al., editors. North American Association of Cancer Registries (NAACR) Cancer Incidence in North America, 2001–2005. NAACR; 2008. (In press) [Google Scholar]
- 24.Levy DT, Bauer JE, Lee HR. Simulation modeling and tobacco control: creating more robust public health policies. Am J Public Health. 2006;96(3):494–8. doi: 10.2105/AJPH.2005.063974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Cancer Institute, DCCPS, Surveillance Program, Statistical Research Applications Branch, Cancer Intervention and Surveillance Modeling Network (CISNET). http://cisnet.cancer.gov/
- 26.Hazelton WD, Clements MS, Moolgavkar SH. Multistage carcinogenesis and lung cancer mortality in three cohorts. Cancer Epidemiol Biomarkers Prev. 2005;14(5):1171–81. doi: 10.1158/1055-9965.EPI-04-0756. [DOI] [PubMed] [Google Scholar]
- 27.Homer J, Milstein B, Wile K, Pratibhu P, Farris R, Orenstein D. Modeling the Local Dynamics of Cardiovascular Health: Risk Factors, Context, and Capacity. Preventing Chronic Disease. 2008;5(2):1–6. [PMC free article] [PubMed] [Google Scholar]
- 28.National Institutes of Health, NCI, Cancer Biomedical Informatics Grid https://cabig.nci.nih.gov/overview ; http://cagrid-portal.nci.nih.gov/web/guest/home