Introduction
In 2003, the National Assessment of Adult Literacy (NAAL) found that approximately 90 million Americans have basic or below basic literacy skills and that 110 million have basic or poor quantitative (numeracy) skills.1 Low literacy and numeracy skills are independently associated with poor understanding of health information, poor health behaviors, and poor clinical outcomes.2 In the context of nutrition and obesity, low health literacy/numeracy is associated with worse knowledge about breastfeeding, difficulty understanding food labels and portion sizes and higher body mass index (BMI) in adults.3–5 In 2003, Surgeon General Richard Carmona acknowledged that health literacy is a major problem in the United States, and recognized that low health literacy is likely “one of the largest contributors to our nation’s epidemic of overweight and obesity.”6
The Importance of Health Literacy
Literacy is defined as “an individual’s ability to read, write, and speak in English, and compute and solve problems at levels of proficiency necessary to function on the job and in society, to achieve one’s goals, and develop one’s knowledge and potential.”1 Adult patients with low literacy have greater reading prescriptions, following medical instructions, and navigating the healthcare system. Patients with low literacy have less disease-specific knowledge, report lower quality of life, and have poorer health-related outcomes—even after adjusting for potential confounders such as education, insurance, and other factors.2 If adults with low health literacy have difficulty caring for their own medical conditions, then, it is likely that parents with low health literacy have difficulty caring for their children’s medical conditions.
The prevalence of low health literacy among parents of young children is similar to that of the general population. The National Adult Literacy Survey (NALS) performed in 1993 and the more recent NAAL estimate that between 31% and 37% of young adults have low literacy skills. According to the NAAL, 1 in 10 young adults cannot complete “below basic” health literacy tasks, such as using the dosage chart on an over-the-counter medication, and more than 1 in 3 cannot complete “basic” health literacy tasks, such as understanding an immunization schedule.1 According to the NAAL, the prevalence of low health literacy among families eligible for Medicaid who are most at risk for child health problems is 60%.1
Most child health information is too complex for caregivers to understand and use appropriately. While the median adult reading level is at the eighth-grade level, common parent information sheets—including those produced by the American Academy of Pediatrics (AAP), the Injury Prevention Program (TIPP), and state newborn screening programs—are written at tenth-grade level or higher. Several studies have demonstrated that caregivers with low literacy are also significantly less likely to understand other critical aspects of pediatric anticipatory guidance, including the risks and benefits of routine vaccinations, how to do a home safety check, and how to handle common household emergencies.
Low caregiver health literacy is independently associated with poor family health behaviors and poor child health outcomes. One study reported an independent association between low maternal health literacy and a decreased likelihood of breastfeeding.3 Adjusted for socioeconomic status and ethnicity, mothers with low health literacy skills are also more likely to smoke and to have depressive symptoms.7,8 Children of caregivers with low health literacy have more unmet healthcare needs, more preventable use of the emergency room, and poor control of asthma and type 1 diabetes.9,10
Most of the studies to date on the role of literacy in healthcare have focused specifically on literacy with little examination of quantitative skills. There is a strong correlation between literacy and quantitative skills,11 however, there are many patients who have adequate literacy but who have below basic or basic quantitative skills or are easily intimidated by the use of basic mathematics.4 Numeracy is an important component of literacy and can be broadly defined as the ability to use numbers in everyday life. Health numeracy is using numbers in a health-related context that may involve calculations, dates, hierarchy, risk statements, tables, and graphs.12
Obesity in Young Children
The impact of the obesity epidemic is particularly concerning among the youngest children. Over 26% of preschool children are overweight (BMI ≥ 85th percentile) or obese (BMI ≥ 95th percentile), as defined by the most recent HHS/CDC expert panel.13 Furthermore, the prevalence of obesity in this age group continues to increase each year. According to a recent report, 28 states have a prevalence of preschool obesity of more than 10%, which is up from only 11 states in 1989. Rates of overweight and obesity are even higher among children from lower socioeconomic strata or ethnic/minority populations, and the rate of childhood obesity among Latino children is nearly twice that of non-Latino children.
Many of the interventions developed to prevent or treat obesity in pediatric populations have had only modest, if any, impact. The most effective interventions for overweight children are time- and resource-intensive and therefore impractical for inclusion in routine primary care. Most experts agree that there are likely untapped (and better) opportunities to address obesity in clinic-based interventions via prevention. A few studies of early childhood obesity prevention that have focused on behavioral theory, multicomponent interventions, and parental involvement have had modest success.
Providers are advised to counsel families to adopt evidence-based behaviors to promote healthy weight, specifically, those recommended by the Committee on Nutrition of the American Academy of Pediatrics (AAP) and other experts. These behaviors include increasing physical activity, limiting television viewing, and promoting healthy eating patterns including limiting sugar-sweetened drinks. Interventions that are sensitive to literacy and numeracy skills of the caregiver may have greater impact in parents with low literacy and numeracy than interventions tested in the past.
Literacy and Numeracy Skills in Healthy Weight Management
In preschool children, parental influence is especially important in healthy weight management activities. Low parental literacy or numeracy skills may inadvertently create a home environment that promotes weight gain. In addition, parents with low literacy or numeracy skills may have difficulty understanding and incorporating healthy weight lifestyle recommendations from providers. These parents may be unable to read food labels to determine the appropriateness of food choices. Provider education about appropriate weight based on growth charts may be difficult for low literacy or numeracy patients to comprehend. This may reduce parental awareness of childhood obesity and lessen the impact of the healthy weight management education.
Numeracy skills may be particularly important for parents seeking to prevent childhood obesity because of the importance of interpreting food labels, understanding portion size, limiting television viewing time, and understanding growth charts. These skills often require parents to deduce what arithmetic skills are needed for certain situations and to then perform complex, multistep, math-related tasks. For example, caregivers may have difficulty understanding instructions from providers about restriction of fats and sugars in their families’ diets or in the amount of exercise needed to promote a healthy weight. To date, however, there have been limited published studies that rigorously measure numeracy’s role in dietary or physical activity-related behaviors. Rothman, et al.4 recently demonstrated that low numeracy skills are significantly associated with worse understanding of food labels in adult primary care patients.
Preliminary results from another recent study from our group found that parents of children aged 0 to 1 year who had low healthy literacy and numeracy had greater difficulty understanding baby formula instructions, interpreting growth tables, and determining the amount of vitamin C in a food item from a food label.14 The inability to understand and implement provider recommendations could lead to a home environment that promotes weight gain.
Addressing Health Literacy and Numeracy in the Prevention of Childhood Obesity
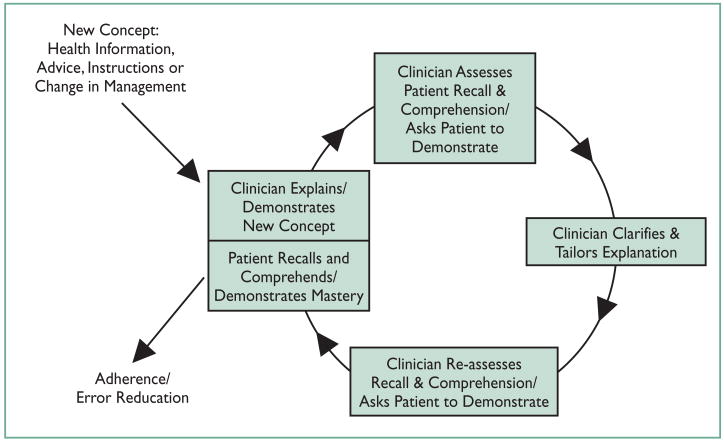
Innovative approaches to obesity prevention during early childhood are critically needed. Addressing literacy and numeracy through improved healthcare provider communication skills and improved educational materials is a potentially successful strategy. As suggested by the Institute of Medicine (IOM) report and other related literature reviews, literacy-based interventions should include the following elements: (1) reducing the complexity of health information (e.g., pictograms, videos, interactive computer programs); (2) improving the communication skills of health providers (e.g., teaching “teach back” (Figure 1), the effective use of printed materials); and (3) easing navigation of the healthcare environment (e.g., patient navigators, improved access to existing resources).15 Limiting the discussion to two or three key points will also improve understandability and the patient’s ability to remember the recommendations given.
Figure 1.
The Teach Back Method. Source: www.webmm.ahrq.gov/case.aspx?caseID=53
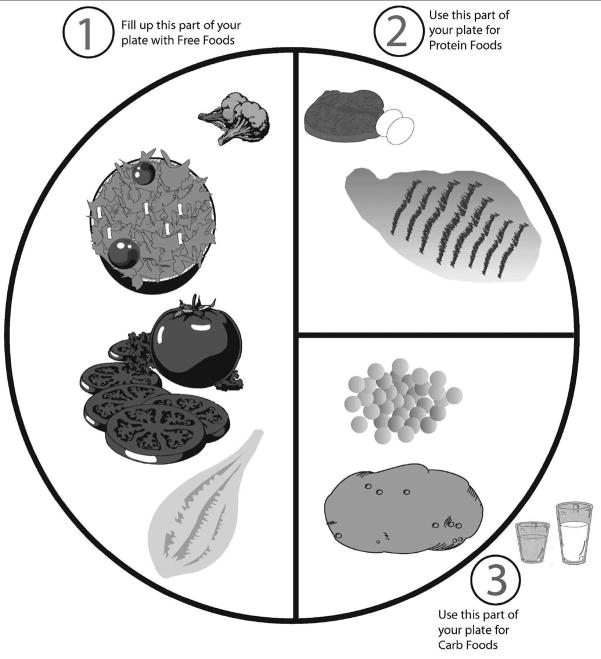
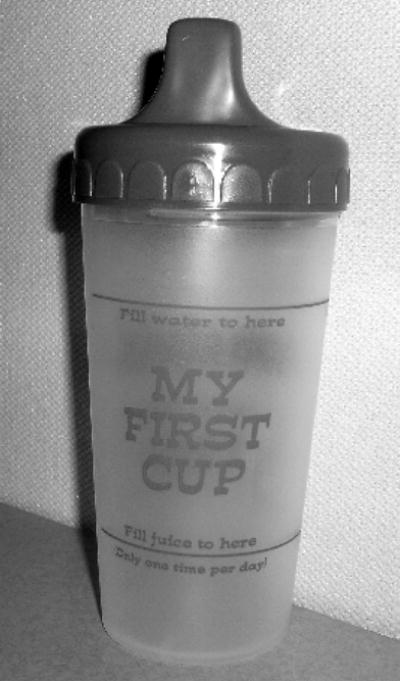
For the prevention of early childhood obesity, interventions should primarily target the parent or caregiver and material should be literacy- and numeracy-sensitive to the parent’s skill level. In addition, the material should be culturally relevant. For example, information for Latino parents and their children should contain information about healthy food choices from commonly consumed food from their culture. Parents need practical tools that they can use to aid in the interpretation of food labels and in meal planning. They also need aids to understand the proper caloric intake and body composition of small children. In focus groups, low-income mothers with low health literacy reported that infant nutrition and physical activity messages were confusing. Mothers reported that they were provided vouchers for juice from the Women, Infant, Children (WIC) program but were not given information about how much juice to give their child daily. Sanders et al. developed “My First Cup” to help caregivers understand the proper amount of juice for their children (Figure 2). Pictures and simple instructions can also help the provider have meaningful discussions with the parents of their patients (Figure 3).
Figure 2.
“My First Cup.” Designed to aid low literacy parents determine the proper daily amount of juice for their children.
Figure 3.
Example of simplified portion size education. Source:www.mc.vanderbilt.edu/diabetes/drtc/preventionandcontrol/tools.php
Low literacy and numeracy skills are common and it may be difficult or embarrassing for the patient or the patient’s parent to test their literacy and numeracy skills. Simply asking about the education history is not sufficient, because many people who have completed high school have low health literacy and numeracy skills. Experts in the field recommend “universal precautions.” This means that clear communication techniques should be given to all patients by all providers in the healthcare system. This assumes that all patients will understand health-related information better if given in a simple and concise manner without extraneous information.
Many providers may be uncomfortable providing education about diet and exercise for children. Despite the high prevalence of overweight and obesity, pediatricians often underdiagnose and undertreat overweight and obesity.16 The undertreatment of overweight and obesity may be due to lack of confidence by the provider. Medical schools and residency programs provide little training in the management of obesity; pediatric training provides little in the evaluation of obesity and the behavioral strategies used to treat obesity.17 One tool that has been used that is literacy and numeracy sensitive is the color-coded BMI chart. It provides color-coded information about the child’s BMI so that parents can understand if their child’s weight is in a healthy range. Educational materials that are literacy- and numeracy-sensitive may allow providers to educate patients and their families about healthy weight management with more confidence, and these materials are currently undergoing efficacy testing in several National Institutes of Health (NIH) studies.
Parents with limited literacy skills are less likely to read to themselves or to their children and increased television viewing is associated with decreased literacy skills.18–20 Children of parents with low literacy may be more exposed to television. These findings have important implications for family-centered messages about obesity prevention in early childhood. Reducing television exposure may be difficult in families with a caregiver who has low literacy and they may be more reliant on television for information. These families may be more receptive to video-formatted messages about healthy lifestyle habits.
Conclusion
Providers should be sensitive to the literacy and numeracy skills of their patients and the patients’ families as instructions and information are given. As many as 1 in 4 parents have limited health literacy and numeracy skills, and these limited skills are associated with worse child health outcomes. Low parental literacy may also be associated with childhood obesity. Changing parental perceptions about a child’s healthy weight, reducing television use, and promoting appropriate portion sizes may be particularly difficult in families with limited literacy or numeracy skills. The best evidence from health-communications research supports “universal precautions,” or enhanced communication techniques, by all providers in the healthcare system. Child obesity-prevention interventions should integrate these proven strategies—such as using pictures or drawings in the examination room, plain-language handouts, and the teach-back method.
Acknowledgments
Mary Margaret Huizinga, M.D., M.P.H., supported by NIEHS grant 1K12ES015855-01.
Biographies

Mary Margaret Huizinga, M.D., M.P.H.

Stephen Pont, M.D., M.P.H.
Russell L. Rothman, M.D., M.P.P.

Eliana Perrin, M.D., M.P.H.

Lee Sanders, M.D., M.P.H.

Bettina Beech, Dr.PH., M.P.H.
References
- 1.Kutner M, Greenberg E, Jin Y, Paulsen C. Results from the 2003 National Assessment of Adult Literacy. National Center for Education Statistics; Sep 6, 2006. The Health Literacy of America’s Adults. NCES 2006483. [Google Scholar]
- 2.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: A systematic review of the literature. J Gen Intern Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaufman H, Skipper B, Small L, Terry T, McGrew M. Effect of literacy on breast-feeding outcomes. South Med J. 2001;94:293–296. [PubMed] [Google Scholar]
- 4.Rothman RL, Housam R, Weiss H, Davis D, Gregory R, Gebretsadik T, Shintani A, Elasy TA. Patient understanding of food labels: The role of literacy and numeracy. Am J Prev Med. 2006;31:391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 5.Carlisle A, Huizinga M, Davis D, Gregory R, Rothman R. Are literacy and numeracy associated with worse portion size estimation skills? J Gen Intern Med. 2007;22:100. [Google Scholar]
- 6.Carmona RH. Health Literacy in America: The Role of Health Care Professionals. [Accessed February 1, 2008];American Medical Association House of Delegates Meeting. [webpage - speech] 61403 www.surgeongeneral.gov/news/speeches/ama061403.htm.
- 7.Fredrickson DD, Washington RL, Pham N, Jackson T, Wiltshire J, Jecha LD. Reading grade levels and health behaviors of parents at child clinics. Kans Med. 1995;96:127–129. [PubMed] [Google Scholar]
- 8.Bennett I, Switzer J, Aguirre A, Evans K, Barg F. ‘Breaking it down’: Patient-clinician communication and prenatal care among African American women of low and higher literacy. Ann Fam Med. 2006;4:334–340. doi: 10.1370/afm.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7:25–31. doi: 10.1016/j.ambp.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ross LA, Frier BM, Kelnar CJ, Deary IJ. Child and parental mental ability and glycaemic control in children with Type 1 diabetes. Diabet Med. 2001;18:364–369. doi: 10.1046/j.1464-5491.2001.00468.x. [DOI] [PubMed] [Google Scholar]
- 11.Kirsch I, Jungeblut A, Jenkins L, Kolstad A. A First Look at the Findings of the National Adult Literacy Survey. National Center for Education Statistics, US Department of Education; Aug 30, 1993. Adult Literacy in America. [Google Scholar]
- 12.Rothman R, Montori V, Cherrington A, Pignone M. Perspective: The role of numeracy in health care. J Health Commun. doi: 10.1080/10810730802281791. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 14.Kumar D, Sanders L, Lokker NL, Patterson BL, Gunn VL, Miller MS, Perrin EM, Rothman RL. Literacy, Numeracy, and the Pediatric Health Activities Test (PHAT). 2007 Pediatric Academic Societies’ Annual Meeting; Toronto. May 5–8, 2007. [Google Scholar]
- 15.Mayeaux EJ, Jr, Murphy PW, Arnold C, Davis TC, Jackson RH, Sentell T. Improving patient education for patients with low literacy skills. Am Fam Physician. 1996;53:205–211. [PubMed] [Google Scholar]
- 16.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:e154–159. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 17.Gahagan S. Child and adolescent obesity. Curr Probl Pediatr Adolesc Health Care. 2004;34:6–43. doi: 10.1016/j.cppeds.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 18.Bennett IM, Robbins S, Al-Shamali N, Haecker T. Screening for low literacy among adult caregivers of pediatric patients. Fam Med. 2003;35:585–590. [PubMed] [Google Scholar]
- 19.Hancox RJ, Milne BJ, Poulton R. Association of television viewing during childhood with poor educational achievement. Arch Pediatr Adolesc Med. 2005;159:614–618. doi: 10.1001/archpedi.159.7.614. [DOI] [PubMed] [Google Scholar]
- 20.Sanders LM, Zacur G, Haecker T, Klass P. Number of children’s books in the home: an indicator of parent health literacy. Ambul Pediatr. 2004;4:424–428. doi: 10.1367/A04-003R.1. [DOI] [PubMed] [Google Scholar]