Abstract
There is now a large body of data that indicates that the CB2 cannabinoid receptor type 2 (CB2) is linked to a variety of immune functional events. This functional relevance appears to be most salient in the course of inflammation, a process during which there is an increased number of receptors that are available for activation. Studies aimed at elucidating signal transductional events resulting from CB2 interaction with its native ligands, and of the role of exogenous cannabinoids in modulating this process, are providing novel insights into the role of the CB2 in maintaining a homeostatic immune balance within the host. Furthermore, these studies suggest that the CB2 may serve as a selective molecular target for therapeutic manipulation of untoward immune responses including those associated with a variety of neuropathies that exhibit a hyperinflammatory component.
Keywords: AIDS, Alzheimer’s disease, ALS, amyotrophic lateral sclerosis, anandamide, 2-arachidonoylglycerol, cannabinoid receptors, CB2, delta-9-tetrahydrocannabinol, Δ9-THC, endocannabinoids, granulomatous amebic encephalitis, HIV encephalitis, multiple sclerosis, neuroinflammation
INTRODUCTION
Cannabinoids and Cannabinoid Receptors
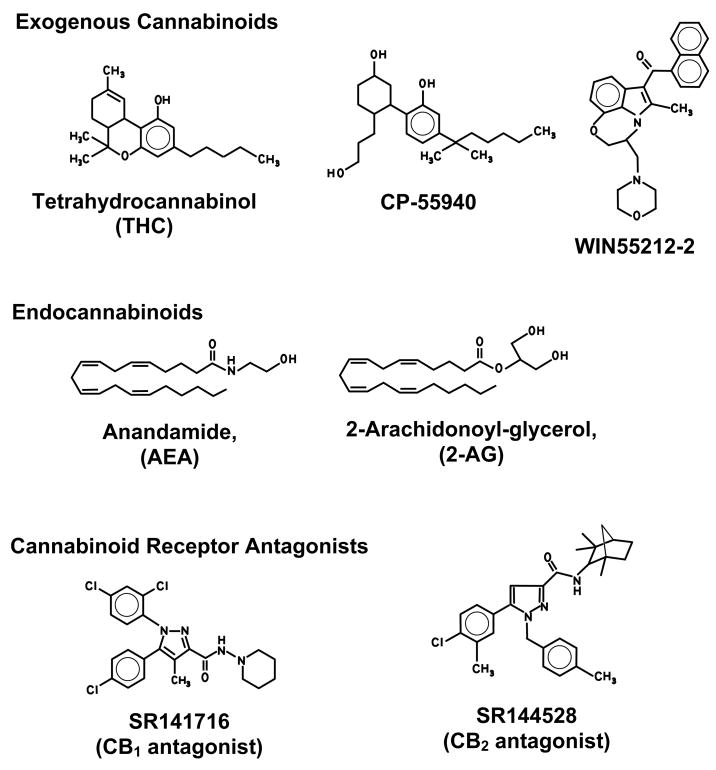
Cannabinoids are highly lipophilic molecules that have been shown to alter the functional activities of immune cells in vitro and in vivo. The term “exogenous cannabinoid” has been applied to cannabinoids that are extracted from the marijuana plant Cannabis sativa or are synthesized in the laboratory. Delta-9-tetrahydrocannabinol (Δ9-THC), cannabinol (CBN), and cannabidiol (CBD) have been the most studied exogenous cannabinoids. Δ9-THC is the major psychoactive and immunomodulatory component in marijuana and has been attributed primarily as exerting immunosuppressive effects on immune cells at peripheral sites and within the central nervous system (CNS). Synthetic exogenous cannabinoids that have been used widely in research include CP55940, WIN55212-2, SR141716A, and SR144528 (Figure 1).
Figure 1.
Representative Cannabinoids. Delta-9-tetrahydrocannabinol (Δ9-THC) is a partial agonist for CB1 and CB2. CP55940: (−)-cis-3-[2-Hydroxy-4-(1,1- dimethylheptyl)phenyl]-trans-4-(3-hydroxypropyl)cyclohexanol and WIN55212-2: (R)- (+)-[2,3-Dihydro-5-methyl-3-(4-morpholinylmethyl)pyrrolo[1,2,3-de)-1,4-benzoxazin-6- yl]-1-napthalenylmethanone are full agonists for CB1 and CB2. Arachidonoylethanolamide (Anandamide, AEA) and 2-Arachidonoylglycerol (2-AG) show agonist behavior at CB1 and CB2. SR141716A: 5-(4-Chlorophenyl)-1-(2,4- dichlorophenyl)-4 methyl-N-(1-piperidyl)pyrazole-3-carboxamide hydrochloride is an antagonist for CB1. SR144528: (1S-endo)-5-(4-Chloro-3-methylphenyl)-1-((4- methylphenyl)methyl)-N-(1,3,3-trimethylbicyclo(2.2.1)hept-2-yl)-1H-pyrazole-3- carboxamide is an antagonist for CB2.
Endocannabinoids (“endogenous cannabinoids”) constitute a second group of cannabinoids that are found natively in vertebrate systems. These molecules are constituent elements of the “endocannabinoid system” that also encompasses mediators responsible for their synthesis, metabolism and catabolism, and the cannabinoid receptors that serve as their molecular targets. Endocannabinoids are derivatives of integral components of cellular membranes and act as hydrophobic lipid messengers. Due to their hydrophobicity, these molecules are not able to translocate in aqueous environments and, upon release, activate cannabinoid receptors locally or on nearby cells. Within the central nervous system (CNS), these bioactive lipids act as retrograde messengers or synaptic modulators, but unlike other synaptic messengers such as the neurotransmitters acetylcholine and dopamine, endocannabinoids are not presynthesized and stored in vesicles but are produced “on demand”. The first endocannabinoid to be identified was arachidonoylethanolamide (AEA; anandamide), which was isolated from porcine brain (Ref. 1). AEA is the amide component of arachidonic acid and ethanolamine. The second endocannabinoid to be identified was 2-arachidonoylglycerol (2-AG) which was isolated from canine gut (Ref. 2). 2-AG is an ester derivative of arachidonic acid and glycerol, and is synthesized from the hydrolysis of 1, 2-diacylglycerol (DAG) by a DAG lipase. Endocannabinoids are produced by a variety of cell types including endothelial cells (Ref. 3), adipocytes (Ref. 4), glial cells (Ref. 5), macrophages (Ref. 6), and Purkinje cells (Ref. 7). In the brain, 2-AG is more bioactive and abundant as compared to AEA. Both AEA and 2-AG are transported across the cell membrane before being degraded by fatty acid amide hydrolase (FAAH), although 2-AG can also be degraded by monoacylglycerol lipase (MGL), a serine hydrolase (Refs 8, 9, 10).
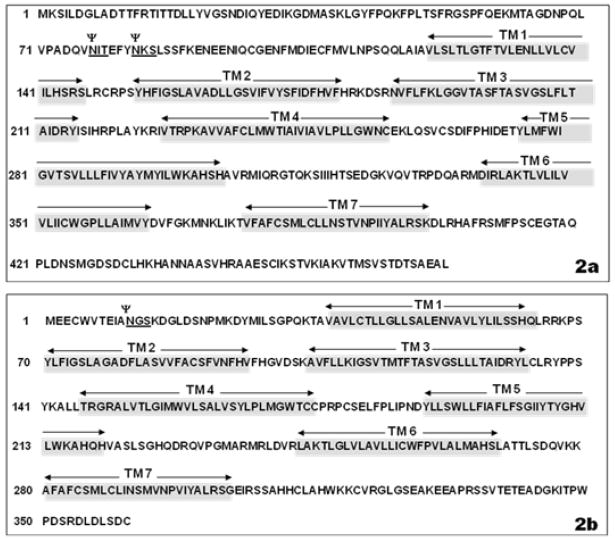
The initial evidence for the existence of a cannabinoid receptor was obtained from pharmacological studies. Treatment of neuroblastoma cells with Δ9-THC, or with the synthetic compounds levonantradol and desacetyllevonantradol, demonstrated inhibition of plasma membrane activity of adenylate cyclase, the enzyme that catalyzes the conversion of ATP to 3′,5′-cyclic AMP (cAMP) and pyrophosphate (Refs 11, 12). However, dextronantradol was shown to have no effect on this activity as compared to levonantradol indicating that the inhibition was stereoselective, a requisite condition for involvement of a receptor-mediated action. Additional studies demonstrated that the putative cannabinoid receptor was coupled to an inhibitory guanine nucleotide binding complex (Gi)because treatment with pertussis toxin reversed the inhibitory effect on adenylate cyclase (Ref. 13). Through the use of radioligand binding assay and in situ mRNA hybridization it was demonstrated that the receptor was distributed throughout the brain and was localized predominantly to the cerebellum, cerebral cortex, hippocampus, basal ganglia and spinal cord (Refs 1, 14, 15, 16). Subsequently, the receptor was isolated and cloned from a rat brain complementary DNA (cDNA) library (Ref. 14), revealing encoding for a 473 amino acid long, 7-transmembrane G-protein coupled protein (Figure 2a). This receptor was referred to initially as the “neuronal” or “central” cannabinoid receptor and has since been designated cannabinoid receptor 1 (CB1).
Figure 2.
Figures 2a and 2b. Panel 2a. Human cannabinoid receptor 1 (CB1). Amino acid sequence of the full-length human CB1 receptor. The putative asparagine-linked glycosylation sites are shown as Ψ. The seven trans-membrane domains are highlighted and noted TM 1 through TM 7. The Genebank accession numbers are NM_016083, NM_001840 and NP_057167.2. Panel 2b. Human cannabinoid receptor 2 (CB2). Amino acid sequence of the full-length human CB2 receptor. The putative asparagine-linked glycosylation site is shown as Ψ. The seven trans-membrane domains are highlighted and noted TM 1 through TM 7. The Genebank accession numbers are NM_001841 and NP_001832.
The CB1 (encoded by the CNR1 gene) negatively regulates neurotransmitter release by inhibiting the phosphorylation of A-type potassium channels. It has been reported that continuous potassium currents from unphosphorylated A-type potassium channels may prevent neurotransmission (Refs 17, 18). N-type calcium channels also are inhibited by CB1 through direct interaction with the inhibitory G protein (Gi/o). CB1- mediated restriction of neurotransmission via potassium and calcium channels accounts for cognitive impairment and sedative-like effects experienced by marijuana users (Refs 18, 19).
Following the identification of CB1, a “peripheral” or “non-neuronal” cannabinoid receptor was cloned from a human promyelocytic cell line (HL60) cDNA library, and was designated cannabinoid receptor 2 (CB2) (Ref. 20). The gene for this receptor (CNR2) was shown to encode for a 360 amino acid long, 7-transmembrane G-protein coupled receptor (Figure 2b) that comparable to CB1, was found to have an extracellular, glycosylated N-terminus and an intracellular C-terminus. Unlike CB1, there is a considerable level of sequence variation for CB2 among human, mouse and rat species, particularly when comparing rat and human sequences. There is 81% amino acid identity between rat and human CB2, as compared to 93% amino acid identity between rat and mouse CB2 (Ref. 21). It has been reported that the rat CB2 sequence demonstrates disparate sequence identity in the carboxy terminus when compared to mouse and human CB2 sequences, and that the presence of intronic DNA in the rat CB2 results in a greater distinction of its carboxy terminus sequence in comparison to that of mouse and human (Ref. 22). It has been documented that the carboxy terminus of the CB2 plays a critical role in regulating receptor desensitization and internalization (Ref. 23); therefore, sequence variation within this region should be taken into consideration when investigating physiological, pharmacological and immunological responses of CB2 in diverse species. Another distinctive feature of CB2 in comparison to CB1 is that its distribution is predominantly in cells and tissues of the immune system including the thymus, tonsils, B lymphocytes, T lymphocytes, macrophages, monocytes, natural killer (NK) cells, and polymorphonuclear cells. B lymphocytes have been shown to express the highest amounts of CB2, followed by NK cells, macrophages, and T lymphocytes, in that order (Refs 24, 25). Recent studies have demonstrated that CB2 is expressed also within the CNS and that this expression occurs during various states of inflammation (Refs 26, 27, 28, 29). This expression of CB2 has been localized primarily to microglia, the resident macrophages of the CNS. CB2 expression is detected in these cells upon activation by various insults and stimuli, but measurable levels of CB2 expression cannot be detected in resident, unstimulated microglia. In addition, during neuroinflammation, infiltrating immunocytes from peripheral non-neuronal sites that influx into the brain as a result of breakdown of the blood-brain barrier (BBB), contribute to the overall expression of CB2. The CB2, in part, exerts its effects through initiation of phospholipase C (PLC) and inositol 1, 4, 5-triphosphate (IP3) signaling pathways that result in increased levels of intracellular calcium (Ref. 30). Table 1 lists select references for reports of the distribution of CB1 and CB2 in various immune tissues and cell types.
Table 1.
Distribution of Cannabinoid Receptors in the Immune System
| Cell type/tissue | Species | Receptor | Reference |
|---|---|---|---|
| B lymphocytes | human | CB2 | Galiegue et al., 1995 (Ref. 24) Carayon et al. 1998 (Ref. 166) |
| T4 lymphocytes | human | CB2 | Galiegue et al. 1995 (Ref. 24) |
| T8 lymphocytes | human | CB2 | Galiegue et al. 1995 (Ref. 24) |
| Leukocytes | human | CB2 | Bouaboula et al. 1993 (Ref. 167) |
| Macrophages | human, mouse | CB2 | Galiegue et al 1995 (Ref. 24) Lee et al. 2001a,b (Refs. 168, 169) Carlisle et al. 2002 (Ref. 92) |
| Microglia | rat | CB1, CB2 | Sinha et al. 1998 (Ref. 170) Waksman et al. 1999 (Ref. 157) Carlisle et al 2002 (Ref. 92) |
| Mononuclear cells | human, rat | CB2 | Galiegue et al. 1995 (Ref. 24) Facci et al. 1995 (Ref. 171) |
| Mast cells | rat | CB2 | Facci et al. 1995 (Ref. 171) |
| Natural Killer (NK) cells | human | CB2 | Galiegue et al. 1995 (Ref. 24) |
| Peyer’s Patches | rat | CBa | Lynn and Herkenham 1994 (Ref. 172) |
| Spleen | human, mouse, rat | CB1, CB2 | Kaminski et al. 1992 (Ref. 173) Munro et al. 1993 (Ref. 20) Galiegue et al. 1995 (Ref. 24) Facci et al. 1995 (Ref. 171) Lynn and Herkenham 1994 (Ref. 172) Galiegue et al. 1995 (Ref. 24) |
| Thymus | human | CB2 | Galiegue et al. 1995 (Ref. 24) |
| Tonsils | human | CB2 | Lynn and Herkenham 1994 (Ref. 172) |
| Lymph nodes | rat | CBa |
Cannabinoid receptor type not specified.
There is accumulating evidence that additional cannabinoid receptors exist. This evidence has been obtained primarily from studies in which CB1 knockout or CB1/CB2 double-knockout mice have been used to investigate the pharmacology and pharmacokinetics of Δ9-THC, AEA, and cannabinoid analogs. Recently, it has been suggested that the G-protein coupled receptor GPR55, first cloned and identified in silico from an expressed sequence tags (EST) database (Refs 31, 32, 33), may be a novel cannabinoid receptor. Comparable to CB1 and CB2, GPR55 has seven conserved transmembrane sequences and has been shown to be activated by plantonic and synthetic exogenous cannabinoids such as Δ9-THC, cannibidiol, abnormal cannabidiol, HU-210, and CP55940, and by the endogenous cannabinoids anandamide, 2-AG and noladin ether (Ref. 34). Unlike CB1 and CB2, GPR55 is not activated by the synthetic agonist WIN55212-2, but is coupled to a G-alpha (Gα ) protein instead of a Gi/o protein (Ref. 34) and has been shown to increase intracellular calcium levels upon activation (Ref. 35). GPR55 expression has been identified in a variety of tissues including spleen, gastrointestine and brain (Ref. 32). However, the physiological and pharmacological functional relevance of GPR55 has yet to be elucidated. Another receptor reported to be a candidate cannabinoid receptor is the transient receptor potential vanilloid 1 (TRVP1) receptor, a ligand-gated cation channel and a member of the transient receptor potential channel family (Ref. 36). TRVP1 receptors are inherently activated by naturally occurring compounds such as capsaicin, vanilloids and resiniferatoxin (Ref. 37). Its implied role as a cannabinoid receptor is based on the ability of the endogenous cannabinoid anandamide, shown to be structurally similar to capsaicin, to bind and activate this receptor (Refs 38, 39, 40, 41). Nevertheless, in spite of the various speculative reports of additional cannabinoid receptor subtypes, a novel cannabinoid receptor that meets rigid criteria pharmacologically and functionally has yet to be identified (Refs 42, 43, 44, 45).
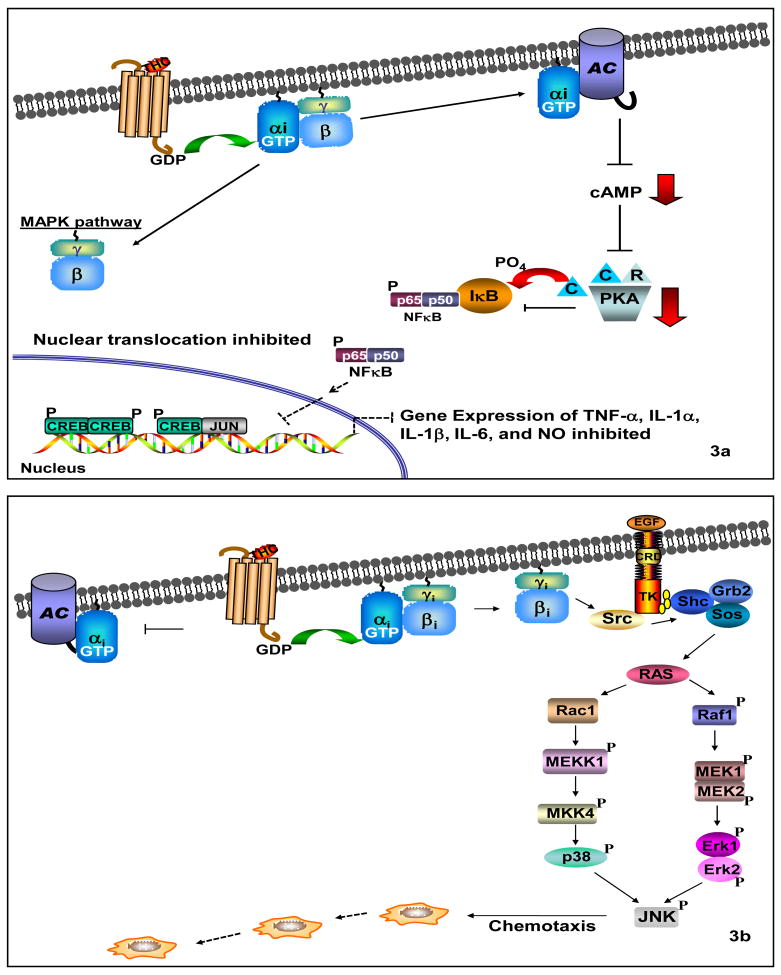
Cannabinoid Receptor Signaling
Both CB1 and CB2 are involved in regulating signaling cascades that include adenylate cyclase and cAMP, mitogen-activated protein (MAP) kinase, and modulation of levels of intracellular calcium (Refs 18, 30, 46, 47, 48). Upon cannabinoid receptor interaction with its cognate ligand, the receptor-coupled G protein exchanges the inactive guanine nucleotide GDP for its active form GTP, and the heterotrimeric G-protein dissociates into α and βγ subunits (Figure 3a). The βγ subunits are believed to take part in signaling pathways distinctive from those of the α subunit, such as the regulation of phospholipase C (PLC) isoforms and activation of the mitogen-activated protein kinase (MAPK) signaling network (Ref. 17) (Figure 3b). The α subunit binds to, and inhibits the activity of adenylate cyclase, thereby preventing synthesis of the second messenger cAMP and negatively affecting downstream cAMP-dependent signaling events. As a decrease in cAMP production underlies a mechanism in which CB1 prevents neurotransmitter release and maintains the homeostatic integrity of the CNS, decreased cAMP production also may represent a mode by which CB2 signaling in response to endocannabinoids maintains immunological homeostasis or, alternatively, in response to exogenous cannabinoids such as Δ9-THC superimposes a perturbing immunosuppressive effect (Ref. 49).
Figure 3.
Figures 3a and 3b. Panel 3a. Cannabinoid Receptor Signaling. Panel 3a. Gi-alpha signaling down-regulates the pro-inflammatory immune response via adenylate cyclase. Upon cannabinoid receptor activation, the α subunit of the Gi protein interacts with adenylate cyclase to inhibit its activity. This results in a decrease of cAMP production, which leads to inactivation of protein kinase A (PKA). IκB-α remains unphosphorylated due to PKA inactivation, thus preventing activation, nuclear translocation and DNA binding of NFκB and other transcription factors. These events ultimately lead to the down-regulation of pro-inflammatory mediator gene expression. Panel 3b. Gi- beta/gamma signaling induces chemotaxis via RAS-dependent MAP kinase (MAPK) signaling. Following cannabinoid receptor activation, the beta/gamma subunit of the Gi protein induces RAS-dependent MAP kinase (MAPK) signaling pathways. The Src kinase is activated upon interaction with Gi-beta/gamma, and phosphorylates tyrosine residues of the EGF receptor. The Shc/Sos/Grb2 trimer binds the EGF receptor via the SHC adaptor protein, while the guanine nucleotide exchange factor Sos interacts with Ras-GTPases to activate RAS. Following Ras activation, two independent signaling pathways initiate that lead to the activation of p38 and Erk 1 and 2, respectively. Both p38 and Erk 1 and 2 can activate JNK which induces chemotaxis of immune cells.
ROLE OF CANNABINOID RECEPTOR 2 (CB2) IN IMMUNE MODULATION
Effect of Exogenous Cannabinoids on Host Resistance and Immunity
Exogenous cannabinoids have been shown to decrease host resistance to a variety of infectious agents. Administration of Δ9-THC to mice has been reported to lessen their ability to resist infection with the bacterial agent Listeria monocytogenes and the herpes simplex virus-2 (HSV-2) (Refs 50, 51). Studies using mice and guinea pig models of genital herpes have demonstrated an increased incidence of viral lesions and recurrences for animals treated with Δ9-THC (Refs 52, 53). It has been reported, also, that cannabinoids compromise host resistance to Legionella pneumophila, Staphylococcus albus, Treponema pallidum, Friend leukemia virus and Acanthamoeba (Refs 50, 54, 55, 56, 57, 58). These collective observations are consistent with exogenous cannabinoids as possessing properties that affect the activities of immune cells. Indeed, in vitro studies using cells of human and rodent origin have demonstrated that cannabinoids alter the functionality of a diverse array of immune cells. Δ9-THC and the synthetic cannabinoids CP55940 and HU-210 have been shown to inhibit cell contact-dependent cytolysis of tumor cells that is mediated by macrophages and macrophage-like cells (Refs 59, 60). Δ9-THC also has been reported to suppress proliferation of B and T lymphocytes in response to cell-specific mitogens (Refs 59, 60, 61, 62), to suppress the cytolytic activity of NK cells (Ref. 61), and to inhibit cell-killing activity, proliferation and maturation of cytotoxic T lymphocytes (CTLs) (Ref. 61). In addition, it has been indicated that exogenous cannabinoids affect immune cell recruitment and chemotaxis to sites of infection and/or injury (Refs 63, 64). In murine models of Granulomatous Amebic Encephalitis (GAE) and atherosclerosis, macrophages and macrophage-like cells exposed to Δ9-THC have been reported to display less migration to sites of infection (Refs 65, 66, 67, 68). Thus, the collective data suggest that exogenous cannabinoids such as Δ9-THC inhibit the functional activities of a variety of immunocytes, an outcome that is consistent with these compounds as playing a role in decreased host resistance to infectious agents. The recognition that select exogenous cannabinoids acted as anti-inflammatory agents and that immune cells also expressed cannabinoid receptors served as an impetus for studies aimed at defining a functional linkage between these two events.
Role of CB2 on Cell-Mediated and Humoral Immunity
The preponderance of studies to date indicates that the cannabinoid receptor that is linked to modulation of the majority of immune functional responses is the CB2. A number of reports have indicated that cannabinoids suppress the antibody response of humans and animals (Refs 69, 70). This suppression of the humoral immune response by cannabinoids has been attributed as mediated, at least in part, through the inhibition of adenylate cyclase by a pertussis-toxin-sensitive G-protein-coupled mechanism (Ref. 71). In contrast, the partial agonist Δ9-THC, as well as the full cannabinoid agonists CP55940 and WIN55212-2, have been found to enhance human tonsillar B-cell growth when used at nanomolar concentrations (Ref. 72). This enhancement was reported to occur in a mode that was linked to CB2. In addition, it has been demonstrated that the CB2 is down- regulated at the mRNA and protein levels during B-cell differentiation. Furthermore, the CB2-selective antagonist SR144528 reversed the stimulating effects of CP55940 on human tonsillar B-cell activation. Collectively, these observations suggested that the CB2 plays a role in B-cell differentiation.
Cannabinoids also have been reported to suppress a variety of activities of T lymphocytes in a mode that appears to be linked functionally to CB2. For example, it has been indicated that in vivo administration of Δ9-THC to mice results in significant inhibition of NK cytolytic activity without affecting ConA-induced splenocyte proliferation (Ref. 73). Concomitant with this inhibition, it was noted that levels of interferon-gamma (IFNγ) were reduced significantly and that administration of CB1 and CB2 antagonists resulted in a complete reversal in the reduction of levels of this cytokine. In view of these observations, it was suggested that both the CB1 and CB2 were involved in the network that mediates NK cytolytic activity. Thus, these and other studies have indicated that cannabinoids not only exert direct effects on immune cells, but also alter the expression of chemokines and cytokines which are involved in a complex network of cross-signaling among immune cells that plays a critical role in homeostatic balance between pro-inflammatory (Th1) and anti-inflammatory (Th2) activities. For example, it has been reported that Δ9-THC treatment of BALB/c mice results in a decrease in levels of IFNγ, interleukin (IL)-12, and IL-12 receptor b2 in response to Legionella pneumophila infection (Ref. 74). Through the use of cannabinoid receptor antagonists it was indicated that both CB1 and CB2 were linked functionally to the suppression of Th1 immunity to Legionella that accounted for the decrease in levels of IFNγ and IL-12. Studies employing a tumor model, on the other hand, have indicated that CB2 is the receptor that is linked functionally to Δ9-THC-mediated inhibition of immunity by a cytokine-dependent pathway (Ref. 75). In these studies, using a weakly immunogenic mouse lung cancer model, it was shown that Δ9-THC decreased tumor immunogenicity. Levels of the immune inhibitory Th2 cytokines, IL-10 and transforming growth factor (TGF) were augmented, whereas those of the immune stimulatory Th1 cytokine IFNγ were down-regulated. These events were observed at both the tumor site and in spleens of Δ9-THC-treated mice. In vivo administration of the CB2 antagonist SR144528 blocked the effects of Δ9-THC, suggesting that Δ9-THC promoted tumor growth by inhibiting antitumor immunity through a CB2-mediated, cytokine-dependent pathway. Collectively, the results from a number of studies suggest that exogenous cannabinoids elicit a shift in the cytokine expression profile from that which is Th1 proinflammatory to one that is Th2 anti-inflammatory and that the CB2 may be linked to this effect.
Endocannabinoids also have been reported to affect immune function in a mode that, for the most part, is linked to CB2. The effects of AEA and palmitoylethanolamide, as well as Δ9-THC, on the production of tumor necrosis factor (TNF)- α , IL-4, IL-6, IL-8, IL-10, IFNγ, p55, and p75 TNF-α soluble receptors have been examined (Ref. 76). AEA was shown to diminish production of IL-6 and IL-8 at low nanomolar concentrations and to inhibit that of TNF-α , IFNγ, IL-4, and p75 TNF-α soluble receptors at micromolar concentrations. Palmitoylethanolamide, at concentrations similar to those of AEA, inhibited the synthesis of IL-4, IL-6, and IL-8 and the production of p75 TNF-α soluble receptors. However, palmitoylethanolamide did not affect TNF-α and IFNγ production. Neither AEA nor palmitoylethanolamide had an effect on IL-10 synthesis. Δ9-THC, on the other hand, exerted a biphasic effect on the production of proinflammatory cytokines. The synthesis of TNF-α , IL-6, and IL-8 was inhibited maximally at nanomolar levels of Δ9-THC but was stimulated by this cannabinoid when used at micromolar levels, an event consistent with Δ9-THC as exerting biphasic effects. The level of IL-4, IL-10, and p75 TNF-α soluble receptors was diminished by micromolar levels of Δ9-THC. In addition, [3H]arachidonate release was stimulated at high concentrations of Δ9-THC and AEA. Based on these observations, it was suggested that the inhibitory properties of AEA, palmitoylethanolamide and Δ9-THC were due to activation of CB2 and that various endogenous fatty acid ethanolamides participated in the regulation of the immune response. AEA also has been shown to exert an inhibitory effect on chemokine-elicited lymphocyte migration (Ref. 77). The inhibition of stromal derived factor 1 (SDF-1)- induced migration of CD8+ T lymphocytes was found to be mediated through the CB2. However, there also are reports that AEA can exert potentiating effects. It has been reported that AEA acts as a synergistic growth factor for primary murine marrow cells and hematopoietic growth factor (HGF)-dependent cell lines (Ref. 78). AEA also has been found to augment production of IL-6 by astrocytes that have been infected with Theiler’s murine encephalomyelitis virus (Ref. 79). However, in these studies the enhancing effect of AEA was shown to be blocked by the CB1 antagonist SR141716A suggesting involvement of the CB1, rather than the CB2, in the elevation of levels of this pleiotropic cytokine.
In contrast to AEA, 2-AG has been associated primarily with augmentation of immune responses. It has been reported that 2-AG stimulates the release of nitric oxide (NO) from human immune and vascular tissues and from invertebrate immunocytes by a mode that is linked to CB1 (Ref. 80) and that hematopoietic cells expressing CB2 migrate in response to 2-AG (Ref. 81 ). Distinct profiles for CB2 expression in lymphoid tissues have been reported to be dependent on the state of receptor activation, and it has been proposed that cell migration constitutes a major function of CB2 upon stimulation with 2-AG (Ref. 82). Furthermore, it has been demonstrated that 2-AG induces the migration of human peripheral blood monocytes and promyelocytic leukemia HL60 cells that have been differentiated into macrophage-like cells (Ref. 68). This activity has been implicated as occurring through a CB2-dependent mechanism. Subsequent studies have demonstrated that 2-AG causes accelerated production of chemokines by the HL-60 cells (Ref. 83). In addition, rat microglia have been reported to synthesize 2-AG in vitro, an event that has been attributed as linked to increased proliferation through a CB2- dependent mechanism (Ref. 84).
Role of CB2 In Neuroinflammation
The early studies that were conducted to define the functional relevance of CB1 and CB2 suggested that the CB1 was compartmentalized to the CNS while the expression of the CB2 was limited to cells and tissues of the immune system. The development of phenotypically normal CB2 knockout mice (Ref. 85) was a major breakthrough that contributed to elucidation of the role of CB2 in immune modulation within the CNS. In addition to the CB2 knockout mouse strain developed by Buckley and colleagues (Ref. 85), Deltagen (San Mateo, CA) developed a CB2 knockout mouse strain that is commercially available through Jackson Laboratories (Bar Harbor, ME) (Ref. 86). These CB2 knockout mice strains have mutations in the carboxy and amino termini, respectively. The tissues from these mice have been employed extensively in studying CB2 function and CB2-mediated responses. In addition, CB2 knockout mice have been utilized to study the specificity of various CB2 antibodies. However, CB2 localization within the CNS has proven to be an elusive target. While some laboratories have reported detection of the CB2 in the brain (Refs 86, 87, 88), other laboratories have not been able to identify this protein, raising concern as to the reliability and specificity of the CB2 antibodies used in studies. In the studies performed that identified the CB2 protein in brainstem neurons, a polyclonal antibody against the carboxy terminus was used to identify this receptor, and the CB2 knockout strain developed by Buckley and colleagues and wild-type mice were used as the knockout and positive controls, respectively, to confirm the specificity of the polyclonal CB2 antibody. The knockout control was appropriate for those experiments since this knockout strain has a deletion in the carboxy terminus of the CB2 protein (Refs 86, 87). In other studies, CB2 protein has been identified in various brain regions using an antibody specific for the amino terminus of the CB2 protein; however, a knockout control using tissues from CB2 knockout mice was not used to confirm the specificity of this antibody (Refs 86, 88). The investigators from the same study used another CB2 receptor antibody that was raised against the carboxy terminus of the protein to demonstrate CB2 protein expression in the brain of wild-type mice, and the specificity of this antibody was confirmed in CB2 knockout mice (Refs 86, 88, 89, 90). These collective studies highlight the importance of employing specific cannabinoid receptor antibodies whose specificity can be confirmed using appropriate knockout controls, particularly when investigating the complex arena of the CNS. Similar potentially confounding issues have been raised for CB1 antibodies. Grimsey and colleagues demonstrated that various CB1-specific antibodies used in immunostaining and Western blot analyses displayed a multitude of variability in expression profiles, an outcome that was attributed to possible conformational changes, dimerization with other G-protein coupled receptors, or post-translational modifications (Ref. 91). It was postulated that such factors, separately or combined, could result in epitope masking or insufficient binding of antibody (Ref. 91).
Studies performed with CB2 knockout mice for functional assessment of immune function have proven less elusive. Experiments conducted with the knockout mouse developed by Buckley and colleagues revealed that their macrophages in their role of helper T-cell activation are not sensitive to the inhibitory effects of Δ9-THC as compared to macrophages from their wild-type counterparts (Ref. 85). Additionally, it has been reported from in vitro studies that microglia, cells that serve as resident macrophages in the CNS, express CB2 (Ref. 92). CB2 has since been identified in neurons, oligodendrocytes and other glial cells (Refs 26, 27, 28). This receptor can be induced on demand during early inflammatory events (Refs 27, 29) and has been shown to be linked to attenuation of pro-inflammatory cytokine production by microglia (Refs 93, 94. 95, 96, 97). Comparable to macrophages at peripheral sites, microglia are able to phagocytose and process antigens, and upon activation produce pro-inflammatory factors including the cytokines IL-1, IL-6, and TNF-α (Refs 98, 99). Pro-inflammatory mediators released from microglia are cytotoxic and also can secondarily activate astrocytes leading to a further induction of the expression of inflammatory factors. The resultant “storm” of pro-inflammatory mediators contributes to breakdown of the BBB and plays a critical role in promoting influx into the CNS of immunocytes from peripheral non-neuronal sites that also express CB2.
Microglia are believed to play a major role in many neuropathogenic diseases and disorders such as Alzheimer’s disease (AD), Multiple Sclerosis (MS), Amyotrophic Lateral Sclerosis (ALS), and HIV Encephalitis (HIVE). AD is the most common neurodegenerative disorder that causes senile dementia. The defining neuropathologic features of the disease are the presence of extracellular neuritic amyloid plaques and intracellular neurofibrillary tangles (NFTs) in the brain. As neurodegeneration progresses, there is accelerated neurofibrillary tangle formation, neuroinflammation, and neuronal loss. It has been reported that cannabinoids can be neuroprotective in AD by inhibiting the activation of microglia (Ref. 27) induced by amyloid plaques consisting of extracellular aggregates of amyloid β (Aβ) peptides (Refs 100, 101, 102). Recently, it was indicated that the CB1/CB2 agonist CP55940 and the CB2 agonist JWH-015 protect and rescue peripheral blood lymphocytes from Aβ and H2O2-induced apoptosis by two alternative mechanisms (Ref. 103). A receptor-independent pathway was implicated through the demonstration of no-dihydrorhodamine oxidation into fluorescent rhodamine 123 as a result of cannabinoid inhibition of Aβ-generated H2O2 while a receptor-dependent pathway was implicated through demonstration of NFκB activation and p53 downregulation involving phosphoinositide 3-kinase. These results suggested that cannabinoids have potential as neuroprotective compounds in AD.
Multiple sclerosis, also known as “disseminated sclerosis” or “encephalomyelitis disseminate”, is a chronic, inflammatory demyelinating disease of the human CNS that primarily affects adults (Refs 104, 105, 106). MS is characterized by T-cell mediated degeneration of the myelin sheath that covers axons, resulting in an inflammatory process that stimulates other immune cells to secrete pro-inflammatory mediators and antibodies, breakdown of the BBB, activation of macrophages, and production of “cytotoxic” proteins such as metalloproteinases (Refs 107, 108). A significantly greater density of CB2-immunoreactive microglia/macrophages has been identified in affected regions of human MS post-mortem spinal cord (Ref. 109). However, most studies aimed at assessment of effects of cannabinoids on MS, and the role of CB2 in this process, have involved the use of mouse models. The principal mouse model that has been used is the Experimental Autoimmune Encephalomyelitis (EAE) model, which exhibits a CD4+ T lymphocyte-mediated autoimmune disease (Ref. 105). Δ9-THC has been reported to markedly inhibit neurodegeneration in the EAE model and to reduce the associated induced elevated level of glutamate in cerebrospinal fluid (Ref. 110). CB2 mRNA expression and protein internalization have been observed as upregulated significantly in activated microglia of mice experiencing EAE, implicating the involvement of CB2 during this disease (Ref. 111). It has been reported that the cannabinoid WIN55212-2 ameliorates EAE and diminishes cell infiltration of the spinal cord. WIN55212-2 was found to induce encephalitogenic T cell apoptosis through a mechanism in which the CB2 was partially involved (Ref. 112). More recently, it has been proposed that the CB2 plays a protective role in EAE pathology by targeting myeloid progenitor trafficking and its contribution to microglial activation in the CNS (Ref. 113). In Theiler’s virus infection of murine CNS, another mouse model for human MS, improved neurological deficits, concomitant with reduced microglial activation, MHC class II expression and T-lymphocyte infiltration were observed following treatment of mice with the synthetic cannabinoids WIN55212-2, ACEA (a CB1-selective agonist) and JWH-015 (a CB2- selective agonist) (Refs 114, 115). Using the Theiler’s model of MS, it has been demonstrated that clinical signs and axonal damage in the spinal cord are reduced by the AMPA (amino-3-hydroxy-5-methyl-4-isoxazolepropionate) glutamatergic receptor antagonist, NBQX (Ref. 116). The cannabinoid HU-210 was shown to ameliorate symptomology that was accompanied by a reduction of axonal damage. Furthermore, the HU-210-mediated reduction in AMPA-induced excitotoxicity in vivo and in vitro was found to be linked to CB1 and CB2.
Amyotrophic Lateral Sclerosis (ALS) is another neurodegenerative disease that has an inflammatory component. It is characterized pathologically by progressive degeneration of cortical motor neurons (upper motor neurons) and clinically by muscle wasting, weakness, and spasticity that progresses to complete paralysis (Ref. 117). A pathological hallmark of ALS is neuroinflammmation, a process that is mediated by pro-inflammatory cytokines, prostaglandins, and nitric oxide (NO) (Ref. 118). It has been reported that CBN delays the onset of symptoms in mice suffering from experimentally-induced ALS without affecting survival (Ref. 119), and that treatment of mice with WIN55212-2 after onset of symptoms delays overall disease progression (Ref. 120). It has been reported, also, that the CB2 agonist AM-1241 prolongs survival in a G93A- SOD1 mutant transgenic mouse model of ALS when administered at onset of disease symptoms (Ref. 121). Messenger RNA and receptor binding of CB2 were selectively up- regulated in spinal cords of these mice in a fashion that paralleled disease progression. Daily injections of AM-1241 initiated at onset of symptoms increased the survival interval after disease onset by 56%. Collectively, the results suggested that the CB2 agonist extended the interval for motor neuron degeneration and prolonged function in these affected mice.
HIV Encephalitis (HIVE), also known as Acquired Immune Deficiency Syndrome (AIDS)-dementia complex is a disease that results in progressive memory loss, intellectual deterioration, behavioral changes, and motor deficits (Ref. 122). The neuropathology of HIVE is characterized by neuronal loss, glial activation, presence of multinucleated giant cells, perivascular mononuclear infiltration, and in some cases, vacuolar myelopathy and myelin pallor (Ref. 122). The production of pro-inflammatory cytokines such as TNF-α by activated monocytes and microglia, and neurotoxins such as glutamate and NO, is the primary cause of brain damage associated with this disorder. In addition, HIV-specific gene products such as the transactivator tat and the envelope glycoprotein gp120 that are released from infected monocytes and microglia contribute to neuropathology. The simian immunodeficiency model comes closest to replicating events that are associated with HIV infection of the human CNS. Examination of brains of macaques with Simian Immunodeficiency Virus (SIV)-induced encephalitis has led to the suggestion that the endocannabinoid system participates in the development of HIV-induced encephalitis (Ref. 123). In this infectivity model, expression of CB2 was found to be induced in perivascular macrophages, microglial nodules, and T-lymphocytes. It was proposed that activation of CB2, expressed by perivascular macrophages that play a critical role in viral entry into the CNS (Refs 124, 125), likely led to reduction of their antiviral response thus favoring the entry of infected monocytes into the CNS (Ref. 123). In addition, the endogenous cannabinoid-degrading enzyme FAAH was reported as overexpressed in perivascular astrocytes as well as in astrocytic processes reaching cellular infiltrates (Ref. 123). It also has been reported that activation of CB2 results in inhibition of the transendothelial migration of Jurkat T cells and primary human T-lymphocytes by interfering with the CXCL12/CXCR4 chemokine receptor system (Ref. 126). These observations suggest that activation of CB2 can alter the activation of other G protein-coupled receptors, such as CXCR4 that functions as a co-receptor for T lymphotropic HIV. A similar observation in terms of a linkage to CB2 has been made for the chemokine receptor CCR5 that acts as the co-receptor for monotropic HIV (Ref. 63). Activation of CB2 with Δ9-THC, CP55940, or with the CB2-selective compound O-2137 resulted in inhibition of the activation of CCR5 by its native chemokine ligand CCL5 (RANTES). Collectively, these results indicate that the CB2 as a Gi/o protein-coupled receptor “crosstalks” with a number of other G protein-coupled receptors, especially chemokine receptors, such as to alter the activation of heterologous signal transduction pathways. Furthermore, these interactions may have implications for HIV infection, particularly for those receptors such as CXCR4 and CCR5 that act in a co-receptor capacity for HIV. Additionally, possible therapeutic implications of “cross-talk” between cannabinoid receptors and other cellular receptors was reported by Rubio-Araiz and colleagues in which their studies suggested that CB2, along with CB1, could play a role in linking the endocannabinoid sytem with the modulation of neural stem cell proliferation through bi-directional ‘crosstalk” with TNF receptors (Ref. 127).
In summary, cannabinoid receptors appear to play an important role in neuropathological diseases. The CB1 has been reported to be critical for the overall homeostatic balance and regulation of the CNS, while the CB2 has been implicated as playing a functionally relevant role during neuroinflammation. Microglia, as resident macrophages in the CNS, not only play a role in host defense and tissue repair but also have been implicated as contributive to, if not causative of, a variety of inflammatory neuropathological processes. In these cells CB1 appears to be present at constitutive and relatively low levels while the CB2 is expressed inducibly during the inflammatory process and at relatively high levels. Immune responses during the early phase of neuropathological processes appear to involve preponderantly the CB2 and levels and functional relevance of this receptor may be amplified as disease progresses to later stages of inflammation. The recognition that immunocytes resident within the brain express CB2 during the inflammatory process suggests the existence of a temporal window during which these cells may be susceptible to therapeutic manipulation through the use of CB2-selective agonists. That is, selective targeting of the CB2 could result in dampening of untoward immune responses such as elicitation of a chemokine/cytokine “storm” within the CNS that would result in breakdown of the BBB and influx of immunocytes from peripheral, non-neuronal sites that would contribute to further inflammation.
Mechanism of CB2-Mediated Immune Modulation
The CB2 is Differentially Expressed by Macrophages and Macrophage-like Cells
A major target of the action of exogenous and endogenous cannabinoids appears to be cells of macrophage lineage. Cannabinoids have been shown to suppress macrophage functions such as phagocytosis, bactericidal activity, and spreading (Refs 69, 128), to interfere with macrophage cell contact-dependent lysis of tumor cells, herpesvirus-infected cells, and amebae, and to deplete macrophage-elicited soluble tumoricidal activity (Refs 59, 129). These observations are consistent with reports that Δ9-THC inhibits the synthesis of proteins associated with primed and activated macrophages (Ref. 130), alters cytokine secretion by activated macrophages (Refs 131, 132), and inhibits cytokine gene expression by microglia (Ref. 133). Cannabinoids also have been found to affect the production of NO by macrophages and macrophage-like cells (Refs 60, 134). Although it is now evident that cannabinoids exert a variety of effects on the activities of macrophage and macrophage-like cells, a picture is emerging as to the role of CB2 in these processes and the state of cell activation under which it is functionally relevant.
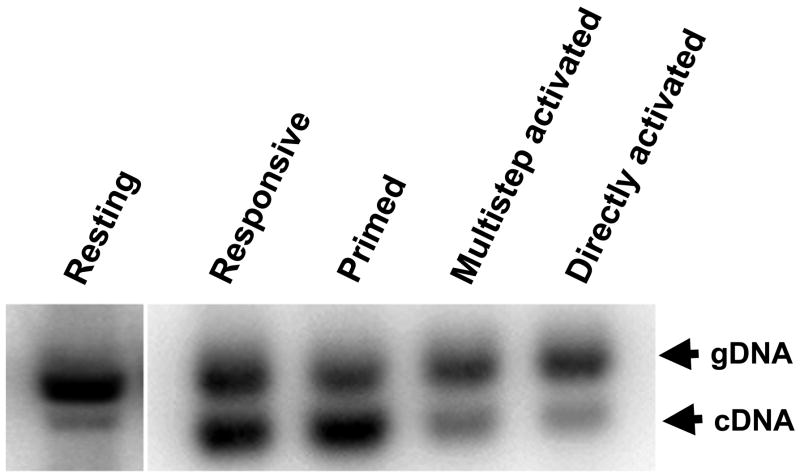
Macrophages and macrophage-like cells such as microglia undergo a maturation, differentiation, and activation process which is characterized by differential gene expression and the acquisition of correlative distinctive functional capabilities (Refs 135, 136, 137). These cells can be driven sequentially in response to multiple signals from “resting” to “responsive”, “responsive” to “primed”, and “primed” to “fully” activated states, a process that mimics events in vivo. Using in vitro models, it has been shown that levels of CB2 receptor mRNA and protein are modulated differentially in relation to cell activation state (Ref. 92). The CB2 is not detected in “resting” cells, is present at high levels in “responsive” and “primed” cells, and is identified at greatly diminished levels in “fully” activated cells (Figure 4). These observations suggest that the CB2 is expressed “on demand” and that the modulation of CB2 levels is a feature common to cells of macrophage lineage as they participate in the inflammatory response and undergo differential gene expression and acquisition of distinctive functional properties. Furthermore, the relatively high levels of CB2 recorded for macrophages when in “responsive” and “primed” states suggest that these cells, and possibly other immune cell types, exhibit a functionally relevant “window” of CB2 expression during which they are most susceptible to cannabinoid-mediated action. Furthermore, since the CB1 is expressed at low and constitutive levels in microglia as compared to the CB2, the kinetics of expression of the two receptors as linked to immune functional activities may be distinctive.
Figure 4.
Levels of CB2 receptor mRNA are modulated differentially in relation to macrophage activation state. The CB2 is detected at low levels in “resting” cells, is present at high levels in “responsive” and “primed” cells, and is identified at greatly diminished levels in cells that have been subjected to multi-step activation or direct activation. The “resting” state was achieved by growing cells on an agar substratum while the “responsive state” was obtained by growing cells on a plastic surface. Cells were treated with IFNγ (100 U/ml), IFNγ (100 U/ml) plus LPS (100 ng/ml), or LPS (100 ng/ml) to obtain “primed”, “multi-step” activated, or “directly” activated states, respectively. Southern blot analysis was performed on mutagenic reverse transcriptase-polymerase chain reaction (MRT-PCR) products of total RNA from mouse peritoneal macrophages (Ref 92). The upper band of each doublet (i.e., gDNA) represents amplified genomic DNA used as an internal quantitative standard. The lower band of each doublet (i.e., cDNA) represents amplified product from messenger RNA (mRNA).
Chemotaxis as a Signature Activity of “Responsive” Macrophages
Chemotaxis and antigen presentation are signature activities of macrophages and macrophage-like cells when in “responsive” and “primed” states of activation, states that are associated with early stages of the inflammatory response. Chemotaxis describes the ability of cells to migrate toward an increasing concentration gradient of stimulating agent (Refs 138, 139, 140, 141) and is distinctive from chemokinesis which represents stimulus-dependent random cellular motion (Refs 142, 143, 144, 145). During chemotaxis, macrophage interaction with a chemoattractant results in the initiation of a rapid and directed movement that is associated with a complex array of cellular events that includes changes in ion fluxes, alterations in integrin avidity, production of superoxide anions, and secretion of lysosomal enzymes (Ref. 146). “Classical” chemoattractants include bacterial-derived N-formyl peptides, the complement fragment peptides C5a and C3a, and lipids such as leukotriene B4 and platelet-activating factor (Refs 147, 148, 149, 150). Chemokines, cytokines of 8- to 17-kDa molecular mass range that are selective for leucocytes in vitro and which elicit accumulation of inflammatory cells in vivo, represent a second group of chemoattractants (Refs 151, 152, 153, 154). As in the case of cannabinoid binding to cannabinoid receptors, the specific effects of chemokines on target cells are mediated by G-protein-coupled receptors (Refs 146, 155). Ligation of chemokines to their cognate receptors initiates a series of signal transductional events that results in regulation of leucocyte trafficking in inflammation, tissue injury, tumor development and host response to infection (Ref. 155).
The current data indicate that cannabinoids act through CB2 to alter macrophage migration, with exogenous cannabinoids such as Δ9-THC exerting an inhibitory effect and, conversely, endocannabinoids such as 2-AG eliciting a stimulatory effect. For example, it has been reported that in vivo and in vitro treatment of rat peritoneal macrophages with CP55940 results in decreased migration in vitro to the peptide formal-methionyl-leucine-phenylalanine (fMLP) in a mode that is linked primarily to CB2 (Ref. 64). The chemotactic response of mouse macrophages to fMLP also has been shown to be decreased by cannabidiol (Ref. 156), a cannabinoid that binds weakly to CB2. A linkage to CB2 was implicated in this response since the CB2-selective antagonist SR144528 prevented the decrease in migration. In contrast to events observed for Δ9- THC, it has been found that 2-AG triggers migration of microglia and that CB2 is involved in this effect (Ref. 5). Recently, in studies that utilized a pharmacological approach in concert with a genetic approach that employed macrophages from knockout mice, it was demonstrated that Δ9-THC and CP55940 mediated inhibition of mouse peritoneal macrophage chemotaxis to RANTES/CCL5 in a mode that was linked to CB2 (Ref. 63). The Δ9-THC and CP55940 deactivation of migratory responsiveness to the chemokine RANTES/CCL5, an event that is mediated through activation of the cognate G protein-coupled chemokine receptor CCR5, suggested that signaling through CB2 leads to “cross-talk” between that receptor and CCR5. Thus, these, and other studies, implicate the CB2 as representing a constituent element of a network of G protein-coupled receptor signal transductional systems, inclusive of chemokine receptors, that act coordinately to modulate macrophage migration.
It has been shown also that the CB2 is involved in cannabinoid-mediated inhibition of processing of antigens by macrophages. In studies performed to examine the effect of Δ9-THC on the processing of intact lysozyme by macrophages, it was demonstrated that Δ9-THC impaired the ability of a macrophage hybridoma to function as an antigen-presenting cell based on its ability to secrete IL-2 upon stimulation of a soluble protein antigen-specific helper T cell hybridoma (Ref. 62). Δ9-THC exposure resulted in a significant reduction in the T cell response to the native form of lysozyme after pretreatment of the macrophages with nanomolar drug concentrations. However, Δ9- THC did not affect IL-2 production when the macrophages presented a synthetic peptide of the antigen to T cells, suggesting that the drug interfered with antigen processing, not peptide presentation. The cannabinoid inhibition of the T cell response to native lysozyme was stereoselective, consistent with the involvement of a cannabinoid receptor in that bioactive CP55940 diminished T cell activation whereas the relatively inactive stereoisomer CP56667 did not. The macrophage hybridoma expressed mRNA for CB2 but not for CB1. Furthermore, the CB1-selective antagonist SR141716A did not reverse the suppression caused by Δ9-THC while the CB2-selective antagonist SR144528 completely blocked the Δ9-THC suppression of the T cell response. Collectively, these results implicated macrophages as the target of cannabinoid inhibition of antigen processing in a mode that was linked functionally to CB2.
CLINICAL IMPLICATIONS/APPLICATIONS
Cannabinoids, as ligands that signal through cannabinoid receptors, may be particularly useful as agents for therapeutic manipulation of hyperinflammatory immune responses within the CNS. These compounds are highly lipophilic and in this context readily penetrate the BBB, a challenge that is posed to a variety of agents that have therapeutic potential. Furthermore, through the application of appropriately engineered molecules, it may be possible to specifically target the CB2, a condition that would obviate generation of untoward psychotropic effects that could be engendered if the CB1 were activated also. The principal potential cellular target in the CNS for these compounds, as applies to early stages of the inflammatory response resulting in generation of a cascade of inflammatory factors and which expresses the CB2, is the microglial cell. Microglia, as macrophage-like cells, during activation also up-regulate an array of cell-surface receptors that may be critical in regeneration and/or degeneration of the CNS. Included among these are immunoglobulin (Ig) superfamily receptors, complement receptors, Toll-like receptors, cytokine/chemokine receptors, and opioid receptors. These cells, in addition to expressing both the CB1 and the CB2 in vitro (Refs 92, 157), also produce the endocannabinoids 2-AG as well as AEA, although the latter is generated in lesser quantities (Ref. 84). Thus, microglia appear to harbor a fully constituted system of endogenous cannabinoid ligands and cognate receptors. Activation of CB2 on these cells appears to promote migration and proliferation. It has been demonstrated that 2-AG induces migration of microglia and that this occurs through the CB2 and abnormal-cannabidiol-sensitive receptors which subsequently leads to activation of the extracellular signal-regulated kinase (ERK)1/2 (encoded by the MAPK1 and MAPK2 genes, respectively) signal transduction pathway (Ref. 5). Furthermore, it has been shown that microglia expresses the CB2 at the leading edge of lamellipodia, consistent with their involvement in cell migration. There is accumulating evidence that the CB2 also is expressed in the CNS in vivo. The expression of the CB2 in microglial, astrocyte and neuronal subpopulations has been identified in a variety of neurodegenerative disease models (Ref. 29). This expression of the CB2 in vivo has been attributed, in large measure, to microglia. In several neurodegenerative diseases, up-regulation of microglial CB2 has been observed (Refs 109, 123, 158, 159, 160, 161). In studies investigating the expression profile of FAAH and the CB2 in postmortem brain tissues from AD patients, it was observed that congregated microglia associated with neuritic plaques selectively over-expressed CB2 (Ref. 162). In addition, CB2-positive microglia have been identified dispersed within active MS plaques and in the periphery of chronic active plaques (Ref. 159).
The collective findings support the concept that the CB2 has a functionally relevant role in the CNS in addition to the CB1. This functionally relevant role appears to play out during the inflammatory process associated with a variety of neuropathies. In this context, it has been proposed that the role of the CB2 in immunity in the CNS is primarily one that is anti-inflammatory (Ref. 163). Since microglia exhibit phenotypic and functional properties of macrophages and inducibly express CB2 at maximal levels when in “responsive” and “primed” states, a “window” of functional relevance for this receptor may be operative comparably to that for macrophages at peripheral sites. That is, antigen processing and/or chemotaxis by these cells may also be susceptible to cannabinoids in a mode that is linked to activation of CB2. Indeed, studies using a mouse model of GAE, a chronic progressive human infection of the CNS that is caused by the opportunistic pathogen Acanthamoeba, revealed a paucity of Mac-1+ cells at focal sites containing Acanthamoeba in the brains of infected mice treated with Δ9-THC as compared to vehicle-treated Acanthamoeba-infected controls (Ref. 57). These observations indicated that microglia (and possibly macrophages introduced from peripheral sites) either did not migrate to infected areas or were selectively targeted by the Acanthamoeba and destroyed. Treatment of neonatal rat cerebral cortex microglial cultures with Δ9-THC resulted in inhibition of the migratory response to Acanthamoeba-conditioned medium (CM) that harbors proteases and other factors released from amebae that serve as chemotactic stimuli (Ref. 49). In addition, treatment with the potent CB1/CB2 agonist CP55940 resulted in a significant concentration-related decrease in microglial migration in response to CM. The highly selective CB2 ligand O-2137 exerted a profound and significant inhibition in the microglial migratory response to CM while treatment with the CB1-selective ligand ACEA had a minimal effect. Finally, treatment of microglia with the CB1 antagonist SR141716A did not block the inhibitory effect of CP55940 while treatment with the CB2-specific antagonist SR144528 resulted in a reversal of the inhibitory effect of CP55940. These collective results indicated that the cannabinoid-mediated inhibition of the CM-stimulated microglial response to A. culbertsoni in mouse brain was linked, at least in part, to the CB2. The mode by which Δ9-THC and other exogenous cannabinoids such as CP55940 signal through CB2 to inhibit the chemotactic response of microglia to Acanthamoeba remains to be defined. However, it is known that Acanthamoeba produce proteases, phospholipases, and other factors (Ref. 164) that may act on phospholipids in microglial membranes, generating cleavage products (Ref. 165). It is postulated that bioactive lipid mediators thus generated include the endocannabinoid 2-AG that serves to drive chemotaxis by autocrine and/or paracrine activation of CB2. The exogenous cannabinoid Δ9-THC may alter this chemotactic response, as well as chemotactic resonses to other stimuli, by superimposing an inhibitory effect consequent of signal transductional activation of CB2. That is, Δ9-THC could inhibit the synthesis and/or release of 2-AG or, alternatively, by virtue of its relative long half-life as compared to that of 2-AG, pre-empt this endocannabinoid from ligating to CB2.
SUMMARY, RESEARCH IN PROGRESS, AND OUTSTANDING RESEARCH QUESTIONS
There is currently a large body of data indicating that the CB2 plays a functionally relevant role during inflammation. This role is especially evident for cells of myeloid lineage, including macrophages and macrophage-like cells, as well as microglia that are resident in the CNS. These latter cells are morphologically, phenotypically, and functionally related to macrophages. The CB2 is differentially expressed by macrophages and macrophage-like cells, with highest levels detected when these cells are in “responsive” and “primed” states, suggesting the existence of a “window” of functional relevance during which activation of the CB2 modulates macrophage activities. Signature activities of “responsive” and “primed” macrophages are chemotaxis and antigen processing, respectively. The endocannabinoid 2-AG, elicited from macrophages and microglia during the activation process, has been reported to stimulate a chemotactic response from these cells through the CB2. In contrast, exogenous cannabinoids such as Δ9-THC and CP55940 have been reported to inhibit the chemotactic response as well as antigen processing of antigens, through activation of the CB2. It is postulated that exogenous cannabinoids such as Δ9-THC superimpose an inhibitory effect on pro- chemotactic endocannabinoids.
Although in recent years major advances have been made regarding the functional relevance of the CB2, a number of outstanding research questions remains. Principal among these is definition of the mechanism through which exogenous cannabinoids such as Δ9-THC superimpose an inhibitory effect on endocannabinoid-mediated immune functional activities. In this context, are there differential signal transductional pathways that are involved following CB2 activation by Δ9-THC versus endocannabinoids? Do exogenous cannabinoids by virtue of their relatively long half-life as compared to endocannabinoids persist in cells so as to affect receptor-mediated endocytosis and recycling of receptor-ligand complexes? In addition, what is the extent of the ability of the CB2 to “cross-talk” with other G protein-coupled receptors, especially chemokine receptors such as CxCR4 and CCR5 that also serve as co-receptors for HIV? Do the endocannabinoids AEA and 2-AG exert differential effects on immune function, thereby acting in an immune homeostatic role? That is, does AEA act in an anti-inflammatory capacity while 2-AG acts as a pro-inflammatory agent as is typical for other bioactive lipids such as select prostaglandins that exert pro-inflammatory versus anti-inflammatory activities? These are but a few of the salient questions that await resolution.
Acknowledgments
Supported in part by NIDA/NIH award R01 DA005832
ABBREVIATIONS
- 2-AG
2-arachidonoylglycerol
- ACEA
arachidonyl-2-chloroethylamide
- AD
Alzheimer’s disease
- AIDS
Acquired Immune Deficiency Syndrome
- ALS
Amyotrophic Lateral Sclerosis
- AMPA
α-amino-3-hydroxy-5-methylisoxazole 4- propionic acid receptor
- Anandamide
arachidonoyl ethanolamide
- ATP
adenosine triphosphate
- BBB
blood brain barrier
- cAMP
3′,5′-cyclic-adenosine monophosphate
- CB1
cannabinoid receptor 1
- CB2
cannabinoid receptor 2
- CBD
cannabidiol
- CBN
cannabinol
- cDNA
complementary DNA
- CNS
central nervous system
- CTL
cytotoxic T lymphocyte
- EAE
Experimental Autoimmune Encephalomyelitis
- ERK
extracellular signal-regulated kinase
- FAAH
fatty acid amide hydrolase
- GAE
Granulomatous Amebic Encephalitis
- HIV
Human Immunodeficiency Virus
- HIVE
HIV Encephalitis
- IFNγ
interferon-gamma
- IL-1
interleukin-1
- IL-4
interleukin-4
- IL-6
interleukin-6
- IL-8
interleukin-8
- IL-10
interleukin-10
- MAP
mitogen-activated protein
- MAPK
mitogen-activated protein kinase
- MGL
monoacylglycerol lipase
- MHC
major histocompatibility complex
- mRNA
messenger RNA
- MS
Multiple Sclerosis
- NBQX
2,3-dihydroxy-6-nitro-7-sulfamoyl-benzo[f]quinoxaline-2,3-dione
- NFκB
nuclear factor of kappa light chain gene enhancer in B-cells
- NFTs
neurofibrillary tangles
- NK
natural killer
- PLC
phospholipase C
- RANTES
Regulated upon Activation, Normal T-cell Expressed, and Secreted
- Δ9-THC
Delta-9-tetrahydrocannabinol, TNF-α tumor necrosis factor-alpha
RELEVANT FURTHER READING AND RESOURCES
Further Reading
Klein, T.W. (2005) Cannabinoid-based drugs as anti-inflammatory therapeutics. Nat Rev Immunol 5, 400–411. This review article discusses the immunosuppressive and anti-inflammatory properties of cannabinoids, and the feasibility of employing cannabinoid-based drugs as therapeutics for chronic inflammatory diseases.
Ashton, J.C. and Glass, M. (2007) The Cannabinoid CB2 Receptor as a target for inflammation-dependent neurodegeneration. Curr Neuropharmacol 5, 73–80. This review highlights both in vivo and in vitro studies of CB2 expression in microglia during brain injury and inflammation as well as after injury.
Arevalo-Martin, A. et al. (2008) CB2 cannabinoid receptors as an emerging target for demyelinating diseases: from neuroimmune interactions to cell replacement strategies. Br J Pharmacol 153, 216–225. This review discusses the role of immune-modulatory cannabinoid compounds on demyelinating diseases (i.e., Multiple Sclerosis) induced by inflammation.
Electronic Databases
Amyotrophic Lateral Sclerosis (ALS) http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=105400
Multiple Sclerosis (MS) http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=126200
Cannabinoid Receptor 1 (CB1) http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=114610
Cannabinoid Receptor 2 (CB2) http://www.ncbi.nlm.nih.gov/entrez/dispomim.cgi?id=605051
Additional Resources
National Institute of Drug Abuse http://www.nida.nih.gov/funding/clintrials.html
National Multiple Sclerosis Society http://www.nationalmssociety.org
References
- 1.Devane WA, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- 2.Mechoulam R, et al. Identification of an endogenous 2-monoglyceride present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol. 1995;50:83–90. doi: 10.1016/0006-2952(95)00109-d. [DOI] [PubMed] [Google Scholar]
- 3.Gauthier KM, et al. Endothelium-derived 2-arachidonylglycerol: an intermediate in vasodilatory eicosanoid release in bovine coronary arteries. Am J Physiol Heart Circ Physiol. 2005;288:H1344–H1351. doi: 10.1152/ajpheart.00537.2004. [DOI] [PubMed] [Google Scholar]
- 4.Gonthier MP, et al. Identification of endocannabinoids and related compounds in human fat cells. Obesity. 2007;15:837–845. doi: 10.1038/oby.2007.581. [DOI] [PubMed] [Google Scholar]
- 5.Walter L, et al. Nonpsychotropic cannabinoid receptors regulate microglial cell migration. J Neurosci. 2003;23:1398–1405. doi: 10.1523/JNEUROSCI.23-04-01398.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Marzo V, et al. Biosynthesis and inactivation of the endocannabinoid 2-arachidonoylglycerol in circulating and tumoral macrophages. Eur J Biochem. 1999;264:258–267. doi: 10.1046/j.1432-1327.1999.00631.x. [DOI] [PubMed] [Google Scholar]
- 7.Maejima T, et al. Presynaptic inhibition caused by retrograde signal from metabotropic glutamate to cannabinoid receptors. Neuron. 2001;31:463 –475. doi: 10.1016/s0896-6273(01)00375-0. [DOI] [PubMed] [Google Scholar]
- 8.Dinh TP, et al. Brain monoglyceride lipase participating in endocannabinoid inactivation. Proc Natl Acad Sci U S A. 2002a;99:10819–10824. doi: 10.1073/pnas.152334899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dinh TP, et al. A role for monoglyceride lipase in 2-arachidonoylglycerol inactivation. Chem Phys Lipids. 2002b;121:149–158. doi: 10.1016/s0009-3084(02)00150-0. [DOI] [PubMed] [Google Scholar]
- 10.Saario SM, et al. Monoglyceride lipase-like enzymatic activity is responsible for hydrolysis of 2-arachidonoylglycerol in rat cerebellar membranes. Biochem Pharmacol. 2004;67:1381–1387. doi: 10.1016/j.bcp.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Howlett AC, Fleming RM. Cannabinoid inhibition of adenylate cyclase. Pharmacology of the response in neuroblastoma cell membranes. Mol Pharmacol. 1984;26:532–538. [PubMed] [Google Scholar]
- 12.Howlett AC. Cannabinoid inhibition of adenylate cyclase. Biochemistry of the response in neuroblastoma cell membranes. Mol Pharmacol. 1985;27:429–436. [PubMed] [Google Scholar]
- 13.Howlett AC, Qualy JM, Khachatrian LL. Involvement of Gi in the inhibition of adenylate cyclase by cannabimimetic drugs. Mol Pharmacol. 1986;29:307–313. [PubMed] [Google Scholar]
- 14.Matsuda LA, et al. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346:561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- 15.Herkenham M, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA. 1990;87:1932–1936. doi: 10.1073/pnas.87.5.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Westlake TM, et al. Cannabinoid receptor binding and messenger RNA expression in human brain: an in vitro receptor autoradiography and in situ hybridization histochemistry study of normal aged and Alzheimer’s brains. Neurosci. 1994;63:637–652. doi: 10.1016/0306-4522(94)90511-8. [DOI] [PubMed] [Google Scholar]
- 17.Howlett AC, Mukhopadhyay S. Cellular signal transduction by anandamide and 2-arachidonoylglycerol. Chem Phys Lipids. 2000;108:53–70. doi: 10.1016/s0009-3084(00)00187-0. [DOI] [PubMed] [Google Scholar]
- 18.Demuth DG, Molleman A. Cannabinoid signalling. Life Sci. 2006;78:546–563. doi: 10.1016/j.lfs.2005.05.055. [DOI] [PubMed] [Google Scholar]
- 19.Gifford AN, et al. In vivo imaging of the brain cannabinoid receptor. Chem Phys Lipids. 2002;121:65–72. doi: 10.1016/s0009-3084(02)00148-2. [DOI] [PubMed] [Google Scholar]
- 20.Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365:61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- 21.Griffin G, et al. Cloning and pharmacological characterization of the rat CB2 cannabinoid receptor. J Pharmacol Exp Ther. 2000;292:888–894. [PubMed] [Google Scholar]
- 22.Brown SM, et al. Cloning and molecular characterization of the rat CB2 cannabinoid receptor. Biochim Biophys Acta. 2002;1576:255–264. doi: 10.1016/s0167-4781(02)00341-x. [DOI] [PubMed] [Google Scholar]
- 23.Bouaboula M, et al. Regulation of peripheral cannabinoid receptor CB2 phosphorylation by the inverse agonist SR144528. Implications for receptor biological responses. J Biol Chem. 1999;274:20397–20405. doi: 10.1074/jbc.274.29.20397. [DOI] [PubMed] [Google Scholar]
- 24.Galiegue S, et al. Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem. 1995;232:54–61. doi: 10.1111/j.1432-1033.1995.tb20780.x. [DOI] [PubMed] [Google Scholar]
- 25.Schatz AR, et al. Cannabinoid receptors CB1 and CB2: a characterization of expression and adenylate cyclase modulation within the immune system. Toxicol Appl Pharmacol. 1997;142:278–287. doi: 10.1006/taap.1996.8034. [DOI] [PubMed] [Google Scholar]
- 26.Nunez E, et al. Cannabinoid CB2 receptors are expressed by perivascular microglial cells in the human brain: an immunohistochemical study. Synapse. 2004;53:208–213. doi: 10.1002/syn.20050. [DOI] [PubMed] [Google Scholar]
- 27.Ramirez BG, et al. Prevention of Alzheimer’s disease pathology by cannabinoids: neuroprotection mediated by blockade of microglial activation. J Neurosci. 2005;25:1904–1913. doi: 10.1523/JNEUROSCI.4540-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cabral GA, Marciano-Cabral F. Cannabinoid receptors in microglia of the central nervous system: immune functional relevance. J Leukoc Biol. 2005;78:1192–1197. doi: 10.1189/jlb.0405216. [DOI] [PubMed] [Google Scholar]
- 29.Fernandez-Ruiz J, et al. Cannabinoid CB2 receptor: a new target for controlling neural cell survival? Trends Pharmacol Sci. 2007;28:39–45. doi: 10.1016/j.tips.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 30.Zoratti C, et al. Anandamide initiates Ca(2+) signaling via CB2 receptor linked to phospholipase C in calf pulmonary endothelial cells. Br J Pharmacol. 2003;140:1351–1362. doi: 10.1038/sj.bjp.0705529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sawzdargo M, et al. Identification and cloning of three novel human G protein-coupled receptor genes GPR52, PsiGPR53 and GPR55: GPR55 is extensively expressed in human brain. Mol Brain Res. 1999;64:193–198. doi: 10.1016/s0169-328x(98)00277-0. [DOI] [PubMed] [Google Scholar]
- 32.Baker D, et al. In silico patent searching reveals a new cannabinoid receptor. Trends Pharmcol Sci. 2006;27:1–4. doi: 10.1016/j.tips.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 33.Pertwee RG. GPR55: a new member of the cannabinoid receptor clan? Br J Pharmacol. 2007;152:984–986. doi: 10.1038/sj.bjp.0707464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryberg E, et al. The orphan receptor GPR55 is a novel cannabinoid receptor. Br J Pharmacol. 2007;152:1092–1101. doi: 10.1038/sj.bjp.0707460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lauckner JE, et al. GPR55 is a cannabinoid receptor that increases intracellular calcium and inhibits M current. PNAS. 2008;105:2699–2704. doi: 10.1073/pnas.0711278105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caterina MJ, et al. The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature. 1997;389:816–824. doi: 10.1038/39807. [DOI] [PubMed] [Google Scholar]
- 37.Szallasi A. Vanilloid (capsaicin) receptors in health and disease. Am J Clin Pathol. 2002;118:110–121. doi: 10.1309/7AYY-VVH1-GQT5-J4R2. [DOI] [PubMed] [Google Scholar]
- 38.Melck D, et al. Unsaturated long-chain N-acyl-vanillyl-amides (N-AVAMs): vanilloid receptor ligands that inhibit anandamide-facilitated transport and bind to CB1 cannabinoid receptors. Biochem Biophys Res Commun. 1999;262:275–284. doi: 10.1006/bbrc.1999.1105. [DOI] [PubMed] [Google Scholar]
- 39.Zygmunt PM, et al. Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature. 1999;400:452–457. doi: 10.1038/22761. [DOI] [PubMed] [Google Scholar]
- 40.Smart D, et al. The endogenous lipid anandamide is a full agonist at the human vanilloid receptor (hVR1) Br J Pharmacol. 2000;129:227–230. doi: 10.1038/sj.bjp.0703050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ross RA. Anandamide and vanilloid TRVP1 receptors. Br J Pharmacol. 2003;140:790–801. doi: 10.1038/sj.bjp.0705467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jarai Z, et al. Cannabinoid-induced mesenteric vasodilation through an endothelial site distinct from CB1 or CB2 receptors. Proc Natl Acad Sci. 1999;96:14136–14141. doi: 10.1073/pnas.96.24.14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Di Marzo V, et al. Levels, metabolism, and pharmacological activity of anandamide in CB(1) cannabinoid receptor knockout mice: evidence for non-CB(1), non-CB(2) receptor-mediated actions of anandamide in mouse brain. J Neurochem. 2000;75:2434–2444. doi: 10.1046/j.1471-4159.2000.0752434.x. [DOI] [PubMed] [Google Scholar]
- 44.Breivogel CS, et al. Evidence for a new G protein-coupled cannabinoid receptor in mouse brain. Mol Pharmacol. 2001;60:155–163. [PubMed] [Google Scholar]
- 45.Wiley JL, Martin BD. Cannabinoid pharmacology: implications for additional cannabinoid receptor subtypes. Chem Phys Lipids. 2002;121:57–63. doi: 10.1016/s0009-3084(02)00146-9. [DOI] [PubMed] [Google Scholar]
- 46.Bayewitch M, et al. The peripheral cannabinoid receptor: adenylate cyclase inhibition and G protein coupling. FEBS Letter. 1995;375:143–147. doi: 10.1016/0014-5793(95)01207-u. [DOI] [PubMed] [Google Scholar]
- 47.Slipetz DM, et al. Activation of the human peripheral cannabinoid receptor results in inhibition of adenylyl cyclase. Mol Pharmacol. 1995;48:352–361. [PubMed] [Google Scholar]
- 48.Bouaboula M, et al. Signaling pathway associated with stimulation of CB2 peripheral cannabinoid receptor. Involvement of both mitogen-activated protein kinase and induction of Krox-24 expression. Eur J Biochem. 1996;237:704–711. doi: 10.1111/j.1432-1033.1996.0704p.x. [DOI] [PubMed] [Google Scholar]
- 49.Cabral GA, et al. CB2 receptors in the brain: role in central immune function. Br J Pharmacol. 2008;153:240–251. doi: 10.1038/sj.bjp.0707584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cabral GA, Staab A. Effects on the immune system. Handb Exp Pharmacol. 2005;168:385–423. doi: 10.1007/3-540-26573-2_13. [DOI] [PubMed] [Google Scholar]
- 51.Morahan PS, et al. Effects of cannabinoids on host resistance to Listeria monocytogenes and herpes simplex virus. Infect Immun. 1979;23:670–674. doi: 10.1128/iai.23.3.670-674.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Juel-Jensen BE. Cannabis and recurrent herpes simplex. Br Med J. 1972:4–296. doi: 10.1136/bmj.4.5835.296-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cabral GA, Dove-Pettit DA. Drugs and immunity: cannabinoids and their role in decreased resistance to infectious disease. J Neuroimmunol. 1998;83:116–123. doi: 10.1016/s0165-5728(97)00227-0. [DOI] [PubMed] [Google Scholar]
- 54.Klein TW, Newton C, Friedman H. Cannabinoid receptors and immunity. Immunol Today. 1998;19:373–381. doi: 10.1016/s0167-5699(98)01300-0. [DOI] [PubMed] [Google Scholar]
- 55.Arata S, et al. Enhanced growth of Legionella pneumophila in tetrahydrocannabinol-treated macrophages. Proc Soc Exp Biol Med. 1992;199:65–67. doi: 10.3181/00379727-199-43330. [DOI] [PubMed] [Google Scholar]
- 56.Arata S, et al. Tetrahydrocannabinol treatment suppresses growth restriction of Legionella pneumophila in murine macrophage cultures. Life Sci. 1991;49:473–479. doi: 10.1016/0024-3205(91)90590-8. [DOI] [PubMed] [Google Scholar]
- 57.Marciano-Cabral F, et al. Delta-9-tetrahydrocannabinol (THC), the major psychoactive component of marijuana, exacerbates brain infection by Acanthamoeba. J Eukaryot Microbiol Suppl. 2001:4S–5S. doi: 10.1111/j.1550-7408.2001.tb00433.x. [DOI] [PubMed] [Google Scholar]
- 58.Newton CA, Klein T, Friedman H. Secondary immunity to Legionella pneumophila and Th1 activity are suppressed by delta-9-tetrahydrocannabinol injection. Infect Immun. 1994;62:4015–4020. doi: 10.1128/iai.62.9.4015-4020.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Burnette-Curley D, Cabral GA. Differential inhibition of RAW264.7 macrophage tumoricidal activity by delta 9tetrahydrocannabinol. Proc Soc Exp Biol Med. 1995;210:64–76. doi: 10.3181/00379727-210-43926. [DOI] [PubMed] [Google Scholar]
- 60.Coffey RG, et al. Tetrahydrocannabinol inhibition of macrophage nitric oxide production. Biochem Pharmacol. 1996;52:743–751. doi: 10.1016/0006-2952(96)00356-5. [DOI] [PubMed] [Google Scholar]
- 61.Klein TW, et al. Marijuana components suppress induction and cytolytic function of murine cytotoxic T cells in vitro and in vivo. J Toxicol Environ Health. 1991;32:465–477. doi: 10.1080/15287399109531496. [DOI] [PubMed] [Google Scholar]
- 62.McCoy KL, et al. Cannabinoid inhibition of the processing of intact lysozyme by macrophages: evidence for CB2 receptor participation. J Pharmacol Exp Ther. 1999;289:1620–1625. [PubMed] [Google Scholar]
- 63.Raborn ES, et al. The Cannabinoid delta-9-tetrahydrocannabinol Mediates Inhibition of Macrophage Chemotaxis to RANTES/CCL5: Linkage to the CB(2) Receptor. J Neuroimmune Pharmacol. 2008;3:117–129. doi: 10.1007/s11481-007-9077-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sacerdote P, et al. In vivo and in vitro treatment with the synthetic cannabinoid CP55, 940 decrease the in vitro migration of macrophages in the rat: involvement of both CB1 and CB2 receptors. J Neuroimmunol. 2000;109:155–163. doi: 10.1016/s0165-5728(00)00307-6. [DOI] [PubMed] [Google Scholar]
- 65.Ullrich O, et al. Immune control by endocannabinoids - new mechanisms of neuroprotection? J Neuroimmunol. 2007;184:127–135. doi: 10.1016/j.jneuroim.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 66.Cabral GA, Marciano-Cabral F. Cannabinoid-mediated exacerbation of brain infection by opportunistic amebae. J Neuroimmunol. 2004;147:127–130. doi: 10.1016/j.jneuroim.2003.10.027. [DOI] [PubMed] [Google Scholar]
- 67.Steffens S, et al. Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice. Nature. 2005;434:782–786. doi: 10.1038/nature03389. [DOI] [PubMed] [Google Scholar]
- 68.Kishimoto S, et al. 2-arachidonoylglycerol induces the migration of HL-60 cells differentiated into macrophage-like cells and human peripheral blood monocytes through the cannabinoid CB2 receptor-dependent mechanism. J Biol Chem. 2003;278:24469–24475. doi: 10.1074/jbc.M301359200. [DOI] [PubMed] [Google Scholar]
- 69.Friedman H, et al. Immunosuppression by marijuana components. In: Ader R, Felten DL, Cohen N, editors. Psychoneuroimmunology. Academic Press; 1991. pp. 931–953. [Google Scholar]
- 70.Klein T, et al. Marijuana, immunity and infection. J Neuroimmunol. 1998b;83:102–115. doi: 10.1016/s0165-5728(97)00226-9. [DOI] [PubMed] [Google Scholar]
- 71.Kaminski N, et al. Suppression of the humoral immune response by cannabinoids is partially mediated through inhibition of adenylate cyclase by a pertussis toxin-sensitive G-protein coupled mechanism. Biochem Pharmacol. 1994;48:1899–1908. doi: 10.1016/0006-2952(94)90588-6. [DOI] [PubMed] [Google Scholar]
- 72.Derocq J, et al. Cannabinoids enhance human B-cell growth at low nanomolar concentrations. FEBS Lett. 1995;369:177–182. doi: 10.1016/0014-5793(95)00746-v. [DOI] [PubMed] [Google Scholar]
- 73.Massi P, et al. Relative involvement of cannabinoid CB(1) and CB(2) receptors in the Delta(9)-tetrahydrocannabinol-induced inhibition of natural killer activity. Eur J Pharmacol. 2000;387:343–347. doi: 10.1016/s0014-2999(99)00860-2. [DOI] [PubMed] [Google Scholar]
- 74.Klein TW, et al. Delta-9-tetrahydrocannabinol treatment suppresses immunity and early IFN-gamma, IL-12, and IL-12 receptor beta 2 responses to Legionella pneumophila infection. J Immunol. 2000;164:6461–6466. doi: 10.4049/jimmunol.164.12.6461. [DOI] [PubMed] [Google Scholar]
- 75.Zhu LX, et al. Delta-9-tetrahydrocannabinol inhibits antitumor immunity by a CB2 receptor-mediated, cytokine-dependent pathway. J Immunol. 2000;165:373–380. doi: 10.4049/jimmunol.165.1.373. [DOI] [PubMed] [Google Scholar]
- 76.Berdyshev EV, et al. Influence of fatty acid ethanolamides and delta9-tetrahydrocannabinol on cytokine and arachidonate release by mononuclear cells. Eur J Pharmacol. 1997;330:231–240. doi: 10.1016/s0014-2999(97)01007-8. [DOI] [PubMed] [Google Scholar]
- 77.Joseph J, et al. Anandamide is an endogenous inhibitor for the migration of tumor cells and T lymphocytes. Cancer Immunol Immunother. 2004;53:723–728. doi: 10.1007/s00262-004-0509-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Valk P, et al. Anandamide, a natural ligand for the peripheral cannabinoid receptor is a novel synergistic growth factor for hematopoietic cells. Blood. 1997;90:1448–1457. [PubMed] [Google Scholar]
- 79.Molina-Holgado F, et al. The endogenous cannabinoid anandamide potentiates interleukin-6 production by astrocytes infected with Theiler’s murine encephalomyelitis virus by a receptor-mediated pathway. FEBS Lett. 1998;433:139–142. doi: 10.1016/s0014-5793(98)00851-5. [DOI] [PubMed] [Google Scholar]
- 80.Stefano GB, et al. 2-Arachidonyl-glycerol stimulates nitric oxide release from human immune and vascular tissues and invertebrate immunocytes by cannabinoid receptor 1. Pharmacol Res. 2000;42:317–322. doi: 10.1006/phrs.2000.0702. [DOI] [PubMed] [Google Scholar]
- 81.Jorda MA, et al. Hematopoietic cells expressing the peripheral cannabinoid receptor migrate in response to the endocannabinoid 2-arachidonoylglycerol. Blood. 2002;99:2786–2793. doi: 10.1182/blood.v99.8.2786. [DOI] [PubMed] [Google Scholar]
- 82.Rayman N, et al. Distinct expression pro les of the peripheral cannabinoid receptor in lymphoid tissues depending on receptor activation status. J Immunol. 2004;172:2111–2117. doi: 10.4049/jimmunol.172.4.2111. [DOI] [PubMed] [Google Scholar]
- 83.Kishimoto S, et al. 2-Arachidonoylglycerol, an endogenous cannabinoid receptor ligand, induces accelerated production of chemokines in HL-60 cells. J Biochem (Tokyo) 2004;135:517–524. doi: 10.1093/jb/mvh063. [DOI] [PubMed] [Google Scholar]
- 84.Carrier EJ, et al. Cultured rat microglial cells synthesize the endocannabinoid 2-arachidonylglycerol, which increases proliferation via a CB2 receptor-dependent mechanism. Mol Pharmacol. 2004;65:999–1007. doi: 10.1124/mol.65.4.999. [DOI] [PubMed] [Google Scholar]
- 85.Buckley NE, et al. Immunomodulation by cannabinoids is absent in mice deficient for the cannabinoid CB(2) receptor. Eur J Pharmacol. 2000;396:141–149. doi: 10.1016/s0014-2999(00)00211-9. [DOI] [PubMed] [Google Scholar]
- 86.Buckley NE. The peripheral cannabinoid receptor knockout mice: an update. Eur J Pharmacol. 2008;153:309–318. doi: 10.1038/sj.bjp.0707527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Van Sickle MD, et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310:329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- 88.Gong JP, et al. Cannabinoid CB2 receptors: Immunohistochemical localization in rat brain. Brain Res. 2006;1071:10–23. doi: 10.1016/j.brainres.2005.11.035. [DOI] [PubMed] [Google Scholar]
- 89.Onaivi ES. Neuropsychobiological evidence for the functional presence and expression of cannabinoid CB2 receptors in the brain. Neuropsychobiol. 2006;54:231–246. doi: 10.1159/000100778. [DOI] [PubMed] [Google Scholar]
- 90.Onaivi ES, et al. Discovery of the presence and functional expression of cannabinoid CB2 receptors in the brain. Ann NY Acad Sci. 2006;1074:514–536. doi: 10.1196/annals.1369.052. [DOI] [PubMed] [Google Scholar]
- 91.Grimsey NL, et al. Specific detection of CB1 receptors; cannabinoid CB1 receptor antibodies are not all created equal! J Neurosci Methods. 2008;171:78–86. doi: 10.1016/j.jneumeth.2008.02.014. [DOI] [PubMed] [Google Scholar]
- 92.Carlisle S, et al. Differential expression of the CB2 cannabinoid receptor by rodent macrophages and macrophage-like cells in relation to cell activation. Int Immunopharmacol. 2002;2:69–82. doi: 10.1016/s1567-5769(01)00147-3. [DOI] [PubMed] [Google Scholar]
- 93.Shohami E, et al. Cytokine production in the brain following closed head injury: dexanabinol (HU-211) is a novel TNF-alpha inhibitor and an effective neuroprotectant. J Neuroimmunol. 1997;72:169–177. doi: 10.1016/s0165-5728(96)00181-6. [DOI] [PubMed] [Google Scholar]
- 94.Cabral GA, et al. Cannabinoid-mediated inhibition of inducible nitric oxide production by rat microglial cells: evidence for CB1 receptor participation. Adv Exp Med Biol. 2001;493:207–214. doi: 10.1007/0-306-47611-8_24. [DOI] [PubMed] [Google Scholar]
- 95.Molina-Holgado F, et al. Role of CB1 and CB2 receptors in the inhibitory effects of cannabinoids on lipopolysaccharide-induced nitric oxide release in astrocyte cultures. J Neurosci Res. 2002;67:829–36. doi: 10.1002/jnr.10165. [DOI] [PubMed] [Google Scholar]
- 96.Klegeris A, et al. Reduction of human monocytic cell neurotoxicity and cytokine secretion by ligands of the cannabinoid-type CB2 receptor. Br J Pharmacol. 2003;139:775–786. doi: 10.1038/sj.bjp.0705304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sheng WS, et al. Synthetic cannabinoid WIN55,212-2 inhibits generation of inflammatory mediators by IL-1beta-stimulated human astrocytes. Glia. 2005;49:211–219. doi: 10.1002/glia.20108. [DOI] [PubMed] [Google Scholar]
- 98.Kreutzberg GW. Microglia: a sensor for pathological events in the CNS. Trends Neurosci. 1996;19:312–318. doi: 10.1016/0166-2236(96)10049-7. [DOI] [PubMed] [Google Scholar]
- 99.Benveniste EN. Role of macrophages/microglia in multiple sclerosis and experimental allergic encephalomyelitis. J Mol Med. 1997;75:165–173. doi: 10.1007/s001090050101. [DOI] [PubMed] [Google Scholar]
- 100.Giulian D, Baker TJ. Characterization of ameboid microglia isolated from developing mammalian brain. J Neurosci. 1986;6:2163–2178. doi: 10.1523/JNEUROSCI.06-08-02163.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dickson DW. Neuropathological diagnosis of Alzheimer’s disease: a perspective from longitudinal clinicopathological studies. Neurobiol Aging. 1997;18:S21–S26. doi: 10.1016/s0197-4580(97)00065-1. [DOI] [PubMed] [Google Scholar]
- 102.Selkoe DJ. The cell biology of beta-amyloid precursor protein and presenilin in Alzheimer’s disease. Trends Cell Biol. 1998;8:447–453. doi: 10.1016/s0962-8924(98)01363-4. [DOI] [PubMed] [Google Scholar]
- 103.Velez-Pardo C, Del Rio MJ. Avoidance of Abeta[(25–35)]/(H2O2)- induced apoptosis in lymphocytes by the cannabinoid agonists CP55,940 and JWJ-015 via receptor-independent and PI3K-dependedent mechanisms: role of NF-kappaB and p53. Med Chem. 2006;2:471–479. doi: 10.2174/157340606778250171. [DOI] [PubMed] [Google Scholar]
- 104.Raine CS, Wu E. Multiple sclerosis: remyelination in acute lesions. J Neuropathol Exp Neurol. 1993;52:199–204. [PubMed] [Google Scholar]
- 105.Racke MK. Experimental autoimmune encephalomyelitis (EAE) Curr Protoc Neurosci. 2001;9 doi: 10.1002/0471142301.ns0907s14. Unit 9.7. [DOI] [PubMed] [Google Scholar]
- 106.Calderon TM, et al. A role for CXCL12 (SDF-1alpha) in the pathogenesis of multiple sclerosis: regulation of CXCL12 expression in astrocytes by soluble myelin basic protein. J Neuroimmunol. 2006;177:27–39. doi: 10.1016/j.jneuroim.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 107.Kieseier BC, et al. Matrix metalloproteinases exhibit different expression patterns in inflammatory demyelinating diseases of the central and peripheral nervous system. Ann N Y Acad Sci. 1999;878:567–570. doi: 10.1111/j.1749-6632.1999.tb07729.x. [DOI] [PubMed] [Google Scholar]
- 108.Anthony DC, et al. The evidence for primary axonal loss in multiple sclerosis. Rev Neurol. 2000;30:1203–1208. [PubMed] [Google Scholar]
- 109.Yiangou Y, et al. COX-2, CB2 and P2X7-immunoreactivities are increased in activated microglial cells/macrophages of multiple sclerosis and amyotrophic lateral sclerosis spinal cord. BMC Neurol. 2006;6:12. doi: 10.1186/1471-2377-6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fujiwara M, Egashira N. New perspectives in the studies on endocannabinoid and cannabis: abnormal behaviors associate with CB1 cannabinoid receptor and development of therapeutic application. J Pharmacol Sci. 2004;96:362–366. doi: 10.1254/jphs.fmj04003x2. [DOI] [PubMed] [Google Scholar]
- 111.Ehrhart J, et al. Stimulation of cannabinoid receptor 2 (CB2) suppresses microglial activation. J Neuroinflammation. 2005;2:29. doi: 10.1186/1742-2094-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Sanchez AJ, et al. R-(+)-[2,3-Dihydro-5-methyl-3-(4-morpholinylmethyl)-pyrrolo-[1,2,3-de]-1,4-benzoxazin-6-yl]-1-naphtalenylmethanone (WIN-2) ameliorates experimental autoimmune encephalomyelitis and induces encephalitogenic T cell apoptosis: partial involvement of the CB(2) receptor. Biochem Pharmacol. 2006;72:1697–1706. doi: 10.1016/j.bcp.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 113.Palazuelos J, et al. The CB(2) cannabinoid receptor controls myeloid progenitor trafficking: involvement in the pathogenesis of an animal model of multiple sclerosis. J Biol Chem. 2008;283:13320–13329. doi: 10.1074/jbc.M707960200. [DOI] [PubMed] [Google Scholar]
- 114.Arevalo-Martin A, et al. Therapeutic action of cannabinoids in a murine model of multiple sclerosis. J Neurosci. 2003;23:2511–2516. doi: 10.1523/JNEUROSCI.23-07-02511.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Croxford JL, Miller SD. Immunoregulation of a viral model of multiple sclerosis using the synthetic cannabinoid R+WIN55,212. J Clin Invest. 2003;111:1231–1240. doi: 10.1172/JCI17652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Docagne F, et al. Excitotoxicity in a chronic model of multiple sclerosis: Neuroprotective effects of cannabinoids through CB1 and CB2 receptor activation. Mol Cell Neurosci. 2007;34:551–561. doi: 10.1016/j.mcn.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 117.Kuncl RW, et al. Motor Neuron Disease. In: Asbury AK, McKhann GM, McDonald WI, editors. Diseases of the Nervous System. 2. W. B. Saunders; 1992. pp. 1179–1208. [Google Scholar]
- 118.Babu GN, et al. Elevated inflammatory markers in a group of amyotrophic lateral sclerosis patients from northern India. Neurochem Res. 2008;33:1145–1149. doi: 10.1007/s11064-007-9564-x. [DOI] [PubMed] [Google Scholar]
- 119.Weydt P, et al. Cannabinol delays symptom onset in SOD1 (G93A) transgenic mice without affecting survival. Amyotroph Lateral Scler Motor Neuron Disord. 2005;6:182–184. doi: 10.1080/14660820510030149. [DOI] [PubMed] [Google Scholar]
- 120.Bisland LG, et al. Increasing cannabinoid levels by pharmacological and genetic manipulation delay disease progression in SOD1 mice. FASEB J. 2006;20:1003–1005. doi: 10.1096/fj.05-4743fje. [DOI] [PubMed] [Google Scholar]
- 121.Shoemaker JL, et al. The CB2 cannabinoid agonist AM-1241 prolongs survival in a transgenic mouse model of amyotrophic lateral sclerosis when initiated at symptom onset. J Neurochem. 2007;101:87–98. doi: 10.1111/j.1471-4159.2006.04346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Spencer DC, Price RW. Human immunodeficiency virus and the central nervous system. Annu Rev Microbiol. 1992;46:655–693. doi: 10.1146/annurev.mi.46.100192.003255. [DOI] [PubMed] [Google Scholar]
- 123.Benito C, et al. A glial endogenous cannabinoid system is upregulated in the brains of macaques with simian immunodeficiency virus-induced encephalitis. J Neurosci. 2005;25:2530–2536. doi: 10.1523/JNEUROSCI.3923-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Williams K, et al. Central nervous system perivascular cells are immunoregulatory cells that connect the CNS with the peripheral immune system. Glia. 2001a;36:156–164. doi: 10.1002/glia.1105. [DOI] [PubMed] [Google Scholar]
- 125.Williams KC, et al. Perivascular macrophages are the primary cell type productively infected by simian immunodeficiency virus in the brains of macaques: implications for the neuropathogenesis of AIDS. J Exp Med. 2001b;193:905–915. doi: 10.1084/jem.193.8.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ghosh S, et al. Cannabinoid receptor CB2 modulates the CXCL12/CXCR4-mediated chemotaxis of T lymphocytes. Mol Immunol. 2006;43:2169–2179. doi: 10.1016/j.molimm.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 127.Rubio-Araiz A, et al. The endocannabinoid system modulates a transient TNF pathway that induces neural stem cell proliferation. Mol Cell Neurosci. 2008;38:374–380. doi: 10.1016/j.mcn.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 128.Klein TW, Friedman H. Modulation of murine immune cell function by marijuana components. In: Watson R, editor. Drugs of Abuse and Immune Function. CRC Press; 1990. pp. 87–111. [Google Scholar]
- 129.Burnette-Curley D, et al. Delta-9-tetrahydrocannabinol inhibits cell contact-dependent cytotoxicity of Bacillus Calmette-Guerin-activated macrophages. Int J Immunopharmacol. 1993;15:371–382. doi: 10.1016/0192-0561(93)90048-4. [DOI] [PubMed] [Google Scholar]
- 130.Cabral GA, Mishkin EM. Delta-9-tetrahydrocannabinol inhibits macrophage protein expression in response to bacterial immunomodulators. J Toxicol Environ Health. 1989;26:175–182. doi: 10.1080/15287398909531243. [DOI] [PubMed] [Google Scholar]
- 131.Watzl B, et al. Influence of marijuana components (THC and CBD) on human mononuclear cell cytokine secretion in vitro. In: Friedman H, Specter S, Klein TW, editors. Advances in Experimental Medicine and Biology. Plenum Press; 1991. pp. 63–70. [DOI] [PubMed] [Google Scholar]
- 132.Nakano Y, et al. Modulation of interleukin 2 activity by delta 9-tetrahydrocannabinol after stimulation with concanavalin A, phytohemagglutinin, or anti-CD3 antibody. Proc Soc Exp Biol Med. 1992;201:165–168. doi: 10.3181/00379727-201-43494c. [DOI] [PubMed] [Google Scholar]
- 133.Puffenbarger RA, et al. Cannabinoids inhibit LPS-inducible cytokine mRNA expression in rat microglial cells. Glia. 2000;29:58–69. [PubMed] [Google Scholar]
- 134.Jeon YJ, et al. Attenuation of inducible nitric oxide synthase gene expression by delta 9-tetrahydrocannabinol is mediated through the inhibition of nuclear factor-κB/Rel activation. Mol Pharmacol. 1996;50:334–341. [PubMed] [Google Scholar]
- 135.Adams DO, Hamilton TA. The cell biology of macrophage activation. Annu Rev Immunol. 1984;2:283–318. doi: 10.1146/annurev.iy.02.040184.001435. [DOI] [PubMed] [Google Scholar]
- 136.Hamilton TA, Adams DO. Molecular mechanisms of signal transduction in macrophages. Immunol Today. 1987;8:151–158. doi: 10.1016/0167-5699(87)90145-9. [DOI] [PubMed] [Google Scholar]
- 137.Hamilton TA, et al. Effects of bacterial lipopolysaccharide on protein synthesis in murine peritoneal macrophages: Relationship to activation for macrophage tumoricidal function. J Cell Physiol. 1986;128:9–17. doi: 10.1002/jcp.1041280103. [DOI] [PubMed] [Google Scholar]
- 138.Harris H. Chemotaxis of monocytes. Br J Exp Pathol. 1953;34:276–279. [PMC free article] [PubMed] [Google Scholar]
- 139.Harris H. Role of chemotaxis in inflammation. Physiol Rev. 1954;34:529–562. doi: 10.1152/physrev.1954.34.3.529. [DOI] [PubMed] [Google Scholar]
- 140.Jin T, Hereld D. Moving toward understanding eukaryotic chemotaxis. Eur J Cell Biol. 2006;85:905–913. doi: 10.1016/j.ejcb.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 141.Kehrl JH. Chemoattractant receptor signaling and the control of lymphocyte migration. Immunol Res. 2006;34:211–227. doi: 10.1385/IR:34:3:211. [DOI] [PubMed] [Google Scholar]
- 142.Becker EL. Stimulated neutrophil locomotion: chemokinesis and chemotaxis. Arch Pathol Lab Med. 1977;101:509–513. [PubMed] [Google Scholar]
- 143.Keller HU, et al. Distinct chemokinetic and chemotactic responses in neutrophil granulocytes. Eur J Immunol. 1978;8:1–7. doi: 10.1002/eji.1830080102. [DOI] [PubMed] [Google Scholar]
- 144.Lauffenburger DA, Horwitz AF. Cell migration: A physically integrated molecular process. Cell. 1996;84:359–369. doi: 10.1016/s0092-8674(00)81280-5. [DOI] [PubMed] [Google Scholar]
- 145.Mitchison TJ, Cramer LP. Actin-based cell motility and cell locomotion. Cell. 1996;84:371–379. doi: 10.1016/s0092-8674(00)81281-7. [DOI] [PubMed] [Google Scholar]
- 146.Murdoch C, Finn A. Chemokine receptors and their role in inflammation and infectious disease. Blood. 2000;95:3032–3043. [PubMed] [Google Scholar]
- 147.Schiffmann E, et al. N-formyl-methionyl peptides as chemoattractants for leucocytes. Proc Natl Acad Sci USA. 1975;72:1059–1062. doi: 10.1073/pnas.72.3.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Goldman DW, Goetzl EJ. Specific binding of leukotriene B4 to receptors on human polymorphonuclear leukocytes. J Immunol. 1982;129:1600–1604. [PubMed] [Google Scholar]
- 149.Hanahan DJ. Platelet activating factor: A biologically active phosphoglyceride. Annu Rev Biochem. 1986;55:483–509. doi: 10.1146/annurev.bi.55.070186.002411. [DOI] [PubMed] [Google Scholar]
- 150.Gerard C, Gerard NP. C5A anaphylatoxin and its seven transmembrane-segment receptor. Annu Rev Immunol. 1994;12:775–808. doi: 10.1146/annurev.iy.12.040194.004015. [DOI] [PubMed] [Google Scholar]
- 151.Baggiolini M, et al. Interleukin-8 and related chemotactic cytokines CXC and CC chemokines. Adv Immunol. 1994;55:97–179. [PubMed] [Google Scholar]
- 152.Baggiolini M, et al. Human chemokines: an update. Annu Rev Immunol. 1997;15:675–705. doi: 10.1146/annurev.immunol.15.1.675. [DOI] [PubMed] [Google Scholar]
- 153.Kim CH. Chemokine-chemokine receptor network in immune cell trafficking. Curr Drug Targets Immune Endocr Metabol Disord. 2004;4:343–361. doi: 10.2174/1568008043339712. [DOI] [PubMed] [Google Scholar]
- 154.Le Y, et al. Chemokines and chemokine receptors: their manifold roles in homeostasis and disease. Cell Mol Immunol. 2004;1:95–104. [PubMed] [Google Scholar]
- 155.Charo IF, Ransohoff RM. Mechanisms of disease: The many roles of chemokines and chemokine receptors in inflammation. N Engl J Med. 2006;354:610–621. doi: 10.1056/NEJMra052723. [DOI] [PubMed] [Google Scholar]
- 156.Sacerdote P, et al. The nonpsychoactive component of marijuana cannabidiol modulates chemotaxis and IL-10 and IL-12 production of murine macrophages both in vivo and in vitro. J Neuroimmunol. 2005;159:97–105. doi: 10.1016/j.jneuroim.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 157.Waksman Y, et al. The central cannabinoid receptor (CB1) mediates inhibition of nitric oxide production by rat microglial cells. J Pharmacol Exp Ther. 1999;288:1357–1366. [PubMed] [Google Scholar]
- 158.Zhang J, et al. Induction of CB2 receptor expression in the rat spinal cord of neuropathic but not inflammatory chronic pain models. Eur J Neurosci. 2003;17:2750–2754. doi: 10.1046/j.1460-9568.2003.02704.x. [DOI] [PubMed] [Google Scholar]
- 159.Benito C, et al. Cannabinoid CB1 and CB2 receptors and fatty acid amide hydrolase are specific markers of plaque cell subtypes in human multiple sclerosis. J Neurosci. 2007;27:2396–2402. doi: 10.1523/JNEUROSCI.4814-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Maresz K, et al. Modulation of the cannabinoid CB2 receptor in microglial cells in response to inflammatory stimuli. J Neurochem. 2005;95:437–445. doi: 10.1111/j.1471-4159.2005.03380.x. [DOI] [PubMed] [Google Scholar]
- 161.Ashton JC, et al. Cerebral hypoxia-ischemia and middle cerebral artery occlusion induce expression of the cannabinoid CB2 receptor in the brain. Neurosci Lett. 2007;412:114–117. doi: 10.1016/j.neulet.2006.10.053. [DOI] [PubMed] [Google Scholar]
- 162.Benito C, et al. Cannabinoid CB2 receptors and fatty acid amide hydrolase are selectively overexpressed in neuritic plaque-associated glia in alzheimer’s disease brains. J Neurosci. 2003;23:11136–11141. doi: 10.1523/JNEUROSCI.23-35-11136.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Carrier EJ, et al. Endocannabinoids in neuroimmunology and stress. Curr Drug Targets CNS Neurol Disord. 2005;4:657–665. doi: 10.2174/156800705774933023. [DOI] [PubMed] [Google Scholar]
- 164.Marciano-Cabral F, Cabral GA. Acanthamoeba spp. as agents of disease in humans. Clin Microbiol Rev. 2003;16:273–307. doi: 10.1128/CMR.16.2.273-307.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Cabral GA. Lipids as bioeffectors in the immune system. Life Sci. 2005;77:1699–1710. doi: 10.1016/j.lfs.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 166.Carayon P, et al. Modulation and functional involvement of CB2 peripheral cannabinoid receptors during B-cell differentiation. Blood. 1998;92:3605–3615. [PubMed] [Google Scholar]
- 167.Bouaboula M, et al. Cannabinoid-receptor expression in human leukocytes. Eur J Biochem. 1993;214:173–180. doi: 10.1111/j.1432-1033.1993.tb17910.x. [DOI] [PubMed] [Google Scholar]
- 168.Lee SF, et al. Downregulation of cannabinoid receptor 2 (CB2) messenger RNA expression during in vitro stimulation of murine splenocytes with lipopolysaccharide. Adv Exp Med Biol. 2001a;493:223–228. doi: 10.1007/0-306-47611-8_26. [DOI] [PubMed] [Google Scholar]
- 169.Lee SF, et al. Differential expression of cannabinoid CB(2) receptor mRNA in mouse immune cell subpopulations and following B cell stimulation. Eur J Pharmacol. 2001b;423:235–241. doi: 10.1016/s0014-2999(01)01122-0. [DOI] [PubMed] [Google Scholar]
- 170.Sinha D, et al. Expression of the CB1 cannabinoid receptor in macrophage-like cells from brain tissue: immunochemical characterization by fusion protein antibodies. J Neuroimmunol. 1998;82:13–21. doi: 10.1016/S0165-5728(97)00181-1. [DOI] [PubMed] [Google Scholar]
- 171.Facci L, et al. Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. Proc Natl Acad Sci USA. 1995;92:3376–3380. doi: 10.1073/pnas.92.8.3376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Lynn AB, Herkenham M. Localization of cannabinoid receptors and nonsaturable high-density cannabinoid binding sites in peripheral tissues of the rat: implications for receptor-mediated immune modulation by cannabinoids. J Pharmacol Exp Ther. 1994;268:1612–1623. [PubMed] [Google Scholar]
- 173.Kaminski NE, et al. Identification of a functionally relevant cannabinoid receptor on mouse spleen cells that is involved in cannabinoid-mediated immune modulation. Mol Pharmacol. 1992;42:736–742. [PMC free article] [PubMed] [Google Scholar]