Abstract
Objective
To determine the efficacy of teaching patients with bipolar disorder (manic-depressive psychosis) to identify early symptoms of relapse and seek prompt treatment from health services.
Design
Single blind randomised controlled trial with matching on four baseline variables using a minimisation algorithm.
Setting
Mental health services in four NHS trusts (one teaching, three non-teaching).
Subjects
69 patients with bipolar disorder who had had a relapse in the previous 12 months.
Interventions
Seven to 12 individual treatment sessions from a research psychologist plus routine care or routine care alone.
Main outcome measures
Time to first manic or depressive relapse, number of manic or depressive relapses, and social functioning examined by standardised interviews every six months for 18 months.
Results
25th centile time to first manic relapse in experimental group was 65 weeks compared with 17 weeks in the control group. Event curves of time to first manic relapse significantly differed between experimental and control groups (log rank 7.04, df=1, P=0.008), with significant reductions in the number of manic relapses over 18 months (median difference 30% (95% confidence interval 8% to 52%), P=0.013). The experimental treatment had no effect on time to first relapse or number of relapses with depression, but it significantly improved overall social functioning (mean difference 2.0 (0.7 to 3.2), P=0.003) and employment (mean difference 0.7 (0.1 to 1.3), P=0.030) by 18 months.
Conclusion
Teaching patients to recognise early symptoms of manic relapse and seek early treatment is associated with important clinical improvements in time to first manic relapse, social functioning, and employment.
Key messages
Relapse rates in bipolar disorder are high despite modern drug treatment
Early prodromal symptoms are idiosyncratic to the patient and consistently develop in the weeks before manic or depressive relapse
This study found that teaching patients to recognise manic prodromes and seek early treatment significantly increased time to the next manic relapse and reduced the number of relapses
Teaching patients to recognise depressive prodromes and seek early antidepressant treatment did not significantly affect depressive relapses and increased the use of antidepressants
Teaching patients to recognise prodromes and seek early treatment improved social function and performance in employment
Introduction
Bipolar disorder (manic-depressive psychosis) is a common serious mental illness characterised by two types of relapse, mania (elation with disinhibited, overactive behaviour) and depression.1 Relapse rates of 50% at one year2–6 and 70% at five years4,7 after a manic episode suggest the need for more effective therapeutic strategies to prevent relapses in bipolar disorder. Three retrospective studies8–10 and two prospective studies11,12 showed identifiable and consistent prodromal symptoms of manic or depressive relapse at two to four weeks before full relapse in most patients with bipolar disorder. These prodromal symptoms are idiosyncratic to both the patient and to the type of relapse (mania or depression). We conducted a randomised controlled trial of the efficacy of recognising prodromal symptoms of manic or depressive relapse followed by early conventional treatment.
Patients and methods
Patients who had a clinical diagnosis of manic-depressive psychosis (bipolar disorder) and who might be eligible for the study were systematically identified from computerised patient records of hospital admissions to three NHS trusts in the north west of England. Patients were approached if their consultant psychiatrist and keyworker agreed. In addition, patients were referred by consultant psychiatrists and mental health workers in these trusts, with two patients being referred by a consultant psychiatrist in a neighbouring trust. Inclusion criteria were a lifetime diagnosis of bipolar disorder1 elicited by a trained research assistant (EMcC, KL, AP) using a standardised psychiatric interview13; two or more relapses,1 one in the previous 12 months; and age 18 to 75 years. Exclusion criteria were an inability to read or write in English; drug or alcohol misuse or dependence1 as a primary problem; and an organic cerebral cause for bipolar disorder—for example, multiple sclerosis or stroke. The study was approved by a medical ethics committee in each NHS trust. Each patient gave written informed consent to the trial.
After assessment at baseline each patient was sequentially entered into the study and randomly allocated to either the experimental or control group using the principle of minimisation.14 Allocation was based on four stratification factors: age (18 to 40 years v 41 to 75 years),15 sex,15 prescription of lithium,16 and presence or absence of a carer (minimum of 10 hours of contact with patient).17 A research assistant (AP) typed the relevant details of each patient suitable for randomisation into a dedicated computer program, which computed the group to which the patient should be allocated. This information was displayed on the computer monitor and recorded. The study was single blind: the study raters (EMcC, KL) were denied access to the randomisation and treatment until the study was completed but therapists and patients knew the treatment allocation immediately after randomisation.
Fifty patients were required in each treatment group to have a power of 80% in detecting a reduction in overall (mania and depression) relapse rate at 12 months from 50% in the control group2–6 to 25% in the experimental group at a significance level of 5% in two tailed tests.
Treatment
The experimental treatment18 was a collaboration between the patient and a research psychologist with little previous clinical experience (AP). Treatment occurred in two stages: training the patient to identify prodromal symptoms (prodromes) of manic or depressive relapse separately and producing and rehearsing an action plan once prodromes had been recognised by the patient. A history was obtained of life circumstances and symptoms leading to previous manic and depressive relapses. The nature and timing of the prodromal symptoms were elicited by using a standard checklist9 and a card sorting exercise19 in which the patient placed prodromal symptoms written on cards in temporal order of occurrence. Diaries were kept to distinguish symptoms associated with normal mood variation from prodromes. Three symptoms or life situations which reliably occur early in the manic or depressive prodrome constituted a warning stage for the patient to increase monitoring from weekly to daily. Three further symptoms or life situations occurring later in the prodrome constituted an action stage to seek help from a health professional of the patient’s choice.
The therapist and patient identified three health professionals for seeking early treatment, one of whom would be available at all times—for example, a general practitioner or a doctor in an accident and emergency department. The full relapse plan of warning and action stage prodromal symptoms for manic and depressive relapse with the plan for seeking treatment was recorded on a card in laminated plastic, which was carried by the patient. The therapist then informed the health staff who would be called on to treat the patient (always informing consultant psychiatrist, key worker, and general practitioner). We compared the combination of experimental treatment and routine treatment with routine treatment alone. Routine care delivered by psychiatrists and key workers consisted of drug treatment, monitoring of mood and adherence to treatment, support, education about bipolar disorder, and if necessary inpatient care.
Assessment
All patients in both groups were assessed with standardised psychiatric13 and social functioning20 interviews by a trained research assistant (EMcC, KL) at baseline and at six, 12, and 18 months after randomisation. A relapse was defined as a minimum of five days of symptoms of mania, hypomania, mixed affective disorder, or major depression according to the standardised symptom criteria (the two week duration criterion for major depression was ignored). The social functioning interview examined behaviour on a four point scale in eight areas of social activity (household management, employment, management of money, child care, intimate relationship with spouse or partner, non-intimate relationship with another adult, social presentation to other people, and coping with an emergency).20 On each scale, 0 indicated fair to good performance, 1 a serious problem on occasions but sometimes managing quite well, 2 serious problems most of the time, and 3 inability to carry out the social activity. Serious problems on the employment scale included timekeeping, unauthorised absence, relations with peers and supervisors, and quantity or quality of output. An overall score of social functioning was obtained by summing the scores of the eight areas.
Each month the research assistant (EMcC, KL) contacted each patient’s consultant psychiatrist and key worker (community psychiatric nurse, social worker, community occupational therapist) to identify contacts between these health professionals and the patient and determine whether he or she had had a relapse. If there was evidence of relapse, the patient was interviewed by the research assistant using the standardised psychiatric interview before the next six month assessment to date the relapse accurately. During each period of six months the research assistant checked the patient’s notes recording drug treatment, all contacts with mental health services, and admissions to hospital. Drug treatment was recorded in mg equivalents of imipramine (antidepressants), chlorpromazine (neuroleptics), diazepam (benzodiazepines), procyclidine (anticholinergics), lithium, carbamazepine, and valproate.21 The newest serum concentration of lithium, carbamazepine, and valproate was recorded from the patient’s notes and compared with the hospital laboratory’s reference range as a check on patients’ adherence to their drug regimen to stabilise mood.
Manic and depressive relapses were treated as independent outcomes because both the experimental and control treatments differed qualitatively for mania and depression. Time to relapse was plotted on event curves, which were analysed with the log rank test. The highly skewed data on relapse and treatment were analysed using χ2 tests, Mann-Whitney U tests, and median differences with 95% confidence intervals. Data on relapse were complete except for one patient who died of ischaemic heart disease in the experimental group before the first assessment at six months. Scores on the patient’s previous assessment were substituted when data on the social function scale were missing. Changes in the data from the social functioning interview were almost normally distributed. They were examined using mean differences with 95% confidence intervals and factorial analysis of variance with the experimental treatment as the between subjects factor.
Results
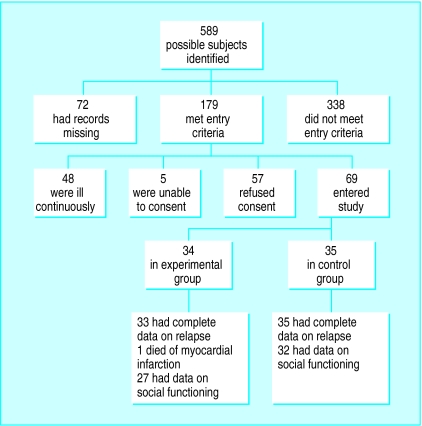
Figure 1 shows the flow of subjects recruited to the study. The study was carried out between March 1994 and April 1997. Table 1 shows that demographic data and baseline variables were not significantly different between the experimental and control groups. There were no clinically important age and sex differences between study subjects and refusers (mean age 43 (SD 15) years, 39/57 (68%) women). Percentage agreement (interrater reliability) between a psychiatrist (RM) and the three research assistants using the standardised psychiatric interview13 to rate the presence or absence of 70 current or past psychiatric episodes was 95% (kappas 0.84, 0.93, and 0.94).
Figure 1.
Flow chart of subjects recruited to study
Table 1.
Demographic and clinical characteristics at baseline. Values are numbers (percentages) of patients unless stated otherwise
| Variable | Experimental group (n=34) | Control group (n=35) |
|---|---|---|
| Mean (SD) age (years) | 44 (13) | 45 (11) |
| Women | 23 (68) | 24 (69) |
| Prescribed lithium | 23 (68) | 25 (71) |
| Contact with carer for ⩾10 h/week | 23 (68) | 21 (60) |
| Married or cohabiting | 22 (65) | 21 (60) |
| White ethnic origin | 30 (88) | 33 (94) |
| Education over 16 years old | 16 (47) | 13 (37) |
| Employed | 9 (26) | 6 (17) |
| Median duration of illness (range) (years) | 11 (2-41) | 12 (2-34) |
| Type of bipolar illness: | ||
| I* | 30 (88) | 33 (94) |
| II† | 4 (12) | 2 (6) |
| Median No of bipolar episodes (range) | 6 (2-25) | 5 (2-17) |
| Median No of psychiatric admissions (range) | 5 (1-21) | 5 (0-19) |
| Mean (SD) No of weeks since last relapse | 25 (16) | 25 (18) |
| Personality disorder | 3 (9) | 4 (11) |
| Other psychiatric disorder‡ | 7 (21) | 6 (17) |
| Prescribed mood stabilising drugs | 30 (88) | 31 (89) |
Recurrent mania requiring admission together with major depression.
Recurrent major depression with occasional hypomania not requiring admission
Obsessive compulsive disorder (n=4), social phobia (n=3), generalised anxiety disorder (n=2), anxiety disorder not otherwise specified (n=2), simple phobia (n=2).
The median number of experimental sessions lasting one hour each was nine (range 0-12). The completed experimental treatment was between seven and 12 sessions of one hour each (median 9, range 0-12). The variation occurred because patients who had only manic relapses had fewer sessions, patients who had relapses during treatment had extra revision sessions, and some patients took longer to identify prodromal symptoms. Seven patients were allocated to the experimental treatment but did not complete it, five because of time commitments (two had no sessions, two one session, and one three sessions), one because she became pregnant and stopped attending (five sessions), and one because she became depressed and did not find the sessions helpful (six sessions).
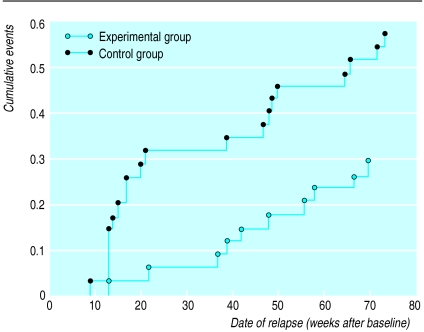
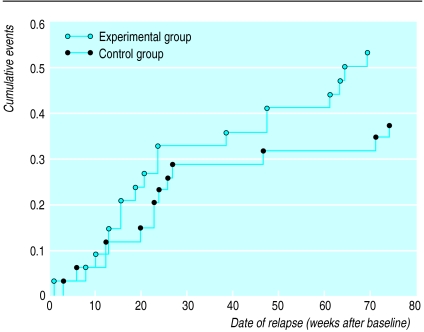
Figure 2 shows that the 25th centile time to first manic relapse was 65 weeks in the experimental group and 17 weeks in the control group. In contrast, figure 3 shows that the 25th centile time to first depressive relapse was 21 weeks in the experimental group and 26 weeks in the control group. The event curves for the experimental and control groups were significantly different for time to first manic relapse (log rank 7.04, df=1, P=0.008) but not for time to first depressive relapse (log rank 1.65, df=1, P=0.19).
Figure 2.
Event plot of time to first manic relapse in experimental and control groups
Figure 3.
Event plot of time to first depressive relapse in experimental and control groups
Table 2 shows significant reductions in the total number of manic relapses between baseline and each six month period up to 18 months in the experimental group compared with the control group but no significant differences in the length of each manic relapse if it occurred. There were no significant changes in the number or length of depressive relapses. In 18 months 3 (9%) patients in the experimental group and 2 (6%) in the control group had a relapse of mixed affective disorder.
Table 2.
Intention to treat analysis of relapse and treatment in experimental and control groups
| Outcome measure (unit) | No (%) with relapse or who received treatment
|
Median difference (95% CI) | P value† | Median (range) length of relapse or treatment (days)
|
Median difference (95% CI) | P value‡ | ||
|---|---|---|---|---|---|---|---|---|
| Experimental (n=33)* | Control (n=35) | Experimental | Control | |||||
| Baseline to 6 months | ||||||||
| Mania (No of days) | 2 (6) | 11 (31) | −25 (−43 to −8) | 0.008 | 15 (10-18) | 39 (7-76) | Not computable | 0.28 |
| Depression (No of days) | 11 (33) | 9 (26) | 8 (−14 to 29) | 0.49 | 66 (8-124) | 18 (10-82) | 21 (−5 to 77) | 0.17 |
| Baseline to 12 months | ||||||||
| Mania (No of days) | 6 (18) | 16 (46) | −28 (−49 to −6) | 0.016 | 15 (10-56) | 45 (7-106) | −19 (−61 to 3) | 0.14 |
| Depression (No of days) | 16 (48) | 11 (31) | 11 (−12 to 34) | 0.35 | 48 (7-233) | 25 (10-187) | 12 (−11 to 71) | 0.081 |
| Baseline to 18 months | ||||||||
| Mania (No of days) | 9 (27) | 20 (57) | −30 (−52 to −8) | 0.013 | 21 (10-137) | 36 (5-133) | −11 (−40 to 20) | 0.54 |
| Depression (No of days) | 18 (55) | 13 (37) | 17 (−6 to 41) | 0.15 | 48 (7-238) | 61 (10-187) | 2 (−42 to 46) | 0.92 |
| Admission (No of days) | 12 (36) | 15 (43) | −6 (−30 to 17) | 0.16 | 49 (2-137) | 49 (5-117) | 3 (−30 to 40) | 0.77 |
| Psychiatric outpatient visits (No) | 32 (97) | 35 (100) | −3 (−9 to 28) | 0.49 | 9 (4-88) | 8 (2-33) | 1 (−1 to 3) | 0.31 |
| Community contacts (No)§ | 16 (48) | 18 (51) | 3 (−21 to 27) | 0.72 | 41 (3-116) | 28 (1-83) | 12 (−10 to 37) | 0.28 |
| Prescribed lithium (mg/day) | 24 (73) | 26 (74) | −2 (−23 to 19) | 0.88 | 800 (93-1600) | 800 (34-1336) | 0 (−200 to 191) | 0.92 |
| Carbamazepine (mg/day) | 13 (39) | 18 (51) | −12 (−36 to 12) | 0.32 | 400 (12-900) | 447 (4-1200) | −1 (−300 to 200) | 0.92 |
| Antidepressants (mg/day)¶ | 17 (52) | 14 (40) | 12 (−12 to 35) | 0.34 | 168 (34-332) | 88 (4-303) | 73 (16 to 131) | 0.024 |
| Neuroleptics (mg/day)** | 25 (76) | 24 (69) | 7 (−14 to 28) | 0.69 | 113 (3-591) | 153 (9-668) | −37 (−116 to 28) | 0.86 |
One patient died of ischaemic heart disease in first six months. †χ2 test. ‡Mann-Whitney U test. §Community psychiatric nurses, mental health social workers, occupational therapists.
mg equivalents of imipramine per day. **mg equivalents of chlorpromazine per day.
Table 2 also shows that there were few differences in other outcome measures between the experimental and control groups over the 18 months. The experimental group received significantly higher dosages of antidepressants than the control group. There was negligible use of benzodiazepines, valproate, anticholinergic drugs, electroconvulsive therapy, and day hospitals in both groups. Compliance with taking mood stabilising drugs as measured by the latest recorded blood concentration did not significantly differ between the two groups (data not shown).
Table 3 shows that there were significant improvements in overall social functioning and employment20 in the experimental group compared with the control group 18 months after the baseline assessment.
Table 3.
Intention to treat analysis of social functioning and employment
| Mean (SD) score | Experimental group (n=34) | Control group (n=35) | Mean difference (95% CI) |
|---|---|---|---|
| Social function* | |||
| Total at baseline | 3.74 (2.62) | 3.14 (3.03) | — |
| Change at: | |||
| 6 months | −0.23 (2.60) | 0.20 (2.43) | 0.44 (−0.78 to 1.65) |
| 12 months | −0.47 (2.67) | 0.77 (2.90) | 1.24 (−0.10 to 2.58) |
| 18 months | −1.03 (2.55) | 0.94 (2.68) | 1.97 (0.71 to 3.23) |
| Employment† | |||
| Total at baseline | 1.68 (1.45) | 1.51 (1.48) | — |
| Change at: | |||
| 6 months | −0.24 (1.16) | 0.09 (1.22) | 0.32 (−0.25 to 0.89) |
| 12 months | −0.44 (1.08) | 0.17 (1.65) | 0.61 (−0.06 to 1.29) |
| 18 months | −0.59 (1.13) | 0.11 (1.47) | 0.70 (0.07 to 1.33) |
Maximum range 1-24. †Maximum range 0-3.
Discussion
The experimental treatment was effective in reducing manic but not depressive relapses because manic prodromes are more distinct11 and longer than depressive prodromes8,9 and acute mania can be treated more quickly and effectively than acute depression.22 An increased awareness of depressive symptoms without the skills to cope with them may be wasteful since the experimental group received significantly higher doses of antidepressants. The intervention probably improved social function by increasing confidence in coping with relapse, which confirms the results from cross sectional studies.10 Cumulative improvements in social function imply a specific treatment effect rather than the non-specific effects of support from an empathic therapist.
The sample is representative of patients with bipolar disorder who are in contact with hospital services in terms of the ratio of women to men (2:1)15,23 and of rates of manic to depressive relapse (about equal).2 We may, however, have missed some brief relapses with our method of follow up assessment. Non-participation because of the length of the intervention resulted in lower recruitment than our power calculation (which assumed modest effects from treatment compared with analogous results from research into schizophrenia24) but all participants who completed the experimental treatment reported treatment gains. The effects of the experimental treatment were large and may have been reduced because some patients in the control group will have probably tried to recognise prodromal symptoms of relapse on their own.10
The experimental treatment does not require a skilled therapist, but attention to detail is essential to identify accurately the nature and timing of prodromal symptoms of manic relapse. Cost effectiveness studies of the identification of manic prodromes followed by early treatment are required before the intervention is systematically introduced into the NHS.
Acknowledgments
We thank Brian Faragher for statistical advice and our colleagues in South Manchester, Guild (Preston), Trafford, and Stockport NHS Trusts who referred patients.
Footnotes
Funding: This study was funded by a project grant awarded by the North West Regional Health Authority.
Competing interests: None declared.
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders, third edition revised. Washington, DC: APA; 1987. [Google Scholar]
- 2.Coryell W, Keller M, Endicott J, Andreasen N, Clayton P, Hirschfeld R. Bipolar II illness: course and outcome over a five year period. Psychol Med. 1989;19:129–141. doi: 10.1017/s0033291700011090. [DOI] [PubMed] [Google Scholar]
- 3.Harrow M, Goldberg JF, Grossman LS, Meltzer HY. Outcome in manic disorders. A naturalistic follow-up study. Arch Gen Psychiatry. 1990;47:665–671. doi: 10.1001/archpsyc.1990.01810190065009. [DOI] [PubMed] [Google Scholar]
- 4.Tohen M, Waternaux GM, Tsuang MT. Outcome in mania: a 4 year prospective follow-up of 75 patients utilising survival analysis. Arch Gen Psychiatry. 1990;47:1106–1111. doi: 10.1001/archpsyc.1990.01810240026005. [DOI] [PubMed] [Google Scholar]
- 5.Keller MB, Lavori PW, Coryell W, Endicott J, Mueller TI. Bipolar I: a five year prospective follow up. J Nerv Ment Dis. 1993;181:238–245. doi: 10.1097/00005053-199304000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Gitlin MJ, Swendsen J, Heller TL, Hammen C. Relapse and impairment in bipolar disorder. Am J Psychiatry. 1995;152:1635–1640. doi: 10.1176/ajp.152.11.1635. [DOI] [PubMed] [Google Scholar]
- 7.Keck PE, McElroy SL, Strakowski SM, West SA, Sax KW, Hawkins JM, et al. 12 month outcome of patients with bipolar disorder following hospitalisation for a manic or mixed episode. Am J Psychiatry. 1998;155:646–652. doi: 10.1176/ajp.155.5.646. [DOI] [PubMed] [Google Scholar]
- 8.Molnar G, Feeney M, Fava G. The duration and symptoms of bipolar prodromes. Am J Psychiatry. 1988;145:1575–1578. doi: 10.1176/ajp.145.12.1576. [DOI] [PubMed] [Google Scholar]
- 9.Smith J, Tarrier N. Prodromal symptoms in manic depressive psychosis. Soc Psychiatry Psychiatric Epidemiol. 1992;27:245–248. doi: 10.1007/BF00788937. [DOI] [PubMed] [Google Scholar]
- 10.Lam D, Wong G. Prodromes, coping strategies, insight and social functioning in bipolar affective disorders. Psychol Med. 1997;27:1091–1100. doi: 10.1017/s0033291797005540. [DOI] [PubMed] [Google Scholar]
- 11.Altman ES, Rea MM, Mintz J, Miklowik DJ, Goldstein MJ, Hwang S. Prodromal symptoms and signs of bipolar relapse: a report based on prospectively collected data. Psychiatr Res. 1992;41:1–8. doi: 10.1016/0165-1781(92)90012-r. [DOI] [PubMed] [Google Scholar]
- 12.Keller MB, Lavori PW, Kane JM, Gelenberg AJ, Rosenbaum JF, Walzer EA, et al. Subsyndromal symptoms in bipolar disorder: a comparison of standard and low serum levels of lithium. Arch Gen Psychiatry. 1982;49:371–376. doi: 10.1001/archpsyc.1992.01820050035005. [DOI] [PubMed] [Google Scholar]
- 13.Spitzer RL, Williams JBW, Gibbon M, First MB. Structured clinical interview for DSM-III-R, patient edition. Washington, DC: APA; 1990. [Google Scholar]
- 14.Pocock ST. Clinical trials: a practical guide. Chichester: Wiley; 1983. [Google Scholar]
- 15.Kessing LV. Recurrence in affective disorder. II. Effect of age and gender. Br J Psychiatry. 1998;172:29–34. doi: 10.1192/bjp.172.1.29. [DOI] [PubMed] [Google Scholar]
- 16.Maj M, Pirozzi R, Magliano L, Bartoli L. Long-term outcome of lithium prophylaxis in bipolar disorder: a 5-year prospective study of 402 patients at a lithium clinic. Am J Psychiatry. 1998;155:30–36. doi: 10.1176/ajp.155.1.30. [DOI] [PubMed] [Google Scholar]
- 17.Miklowitz D, Goldstein M, Nuechterlein K, Snyder M, Mintz J. Family factors and the course of bipolar affective disorders. Arch Gen Psychiatry. 1988;45:225–230. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- 18.Perry A, Tarrier N, Morriss R. Identification of prodromal signs and symptoms and early intervention in manic depressive psychosis patients: a case example. Behav Cognit Psychother. 1995;23:399–409. [Google Scholar]
- 19.Young MA, Grabler P. Rapidity of symptom onset in depression. Psychiatr Res. 1985;16:309–315. doi: 10.1016/0165-1781(85)90122-2. [DOI] [PubMed] [Google Scholar]
- 20.Hurry J, Sturt E, Bebbington P, Tennant C. Socio-demographic associations with social disablement in a community sample. Soc Psychiatry. 1983;18:113–121. doi: 10.1007/BF00583561. [DOI] [PubMed] [Google Scholar]
- 21.World Health Organisation. Anatomical therapeutic chemical (ATC) classification index including defined daily doses (DDDs) per plan substances. Oslo: WHO Collaborating Centre for Drug Statistics and Methodology; 1994. [Google Scholar]
- 22.Hlastala SA, Frank E, Mallinger AG, Thase ME, Ritenour AM, Kupfer DJ. Bipolar depression: an underestimated treatment challenge. Depression Anxiety. 1997;5:73–83. [PubMed] [Google Scholar]
- 23.Gater RA, Dean C, Morris J. The contribution of childbearing to the sex difference in first admission rates for affective psychosis. Psychol Med. 1989;19:719–724. doi: 10.1017/s0033291700024314. [DOI] [PubMed] [Google Scholar]
- 24.Tarrier N, Yusupoff L, Kinney C, McCarthy E, Gledhill A, Haddock G, et al. Randomised controlled trial of intensive cognitive behaviour therapy for patients with chronic schizophrenia. BMJ. 1998;317:303–307. doi: 10.1136/bmj.317.7154.303. [DOI] [PMC free article] [PubMed] [Google Scholar]