Abstract
We report colonoscopic features of an intussuscepted Meckel’s diverticulum, presenting with hematochezia. A 35-year-old woman presented to the emergency room with acute onset, transient, sharp, severe epigastric pain that began 6 h earlier. Colonoscopy revealed a reddish, soft, fist-sized polypoid lesion in the terminal ileum. The lesion was misinterpreted as a hematoma by an inexperienced endoscopist. The patient began to complain of intermittent, severe periumbilical pain following the colonoscopic examination. Subsequent computed tomography showed an enteric intussusception. An exploratory laparotomy revealed an intussuscepted Meckel’s diverticulum, with transmural infarction. Colonoscopy was of little use in assessing the intussusception. However, colonoscopic examination may be performed initially, especially in an intussuscepted Meckel’s diverticulum presenting with hematochezia. Endoscopists should note the endoscopic features of an intussuscepted Meckel’s diverticulum.
Keywords: Colonoscopy, Intussusception, Meckel’s diverticulum
INTRODUCTION
Abdominal computed tomography (CT) is currently considered the most sensitive radiological method for confirming intussusception[1,2]. However, it is quite possible for colonoscopy to be selected as the initial diagnostic method when intussusception presents primarily as hematochezia. Colonoscopy may be useful for confirming the presence of intussusception, localizing the disease, and demonstrating the underlying organic lesion serving as the lead point. Intussusception might be misinterpreted as another lesion, such as a hematoma or polyp, on a colonoscopic examination, especially by an inexperienced endoscopist. Here, we report a colonoscopic feature of an intussuscepted Meckel’s diverticulum, presenting with hematochezia, which was initially misinterpreted as a hematoma on colonoscopic examination.
CASE REPORT
A 35-year-old woman presented to the emergency room with acute onset hematochezia that occurred over a weekend. She first noticed the hematochezia accompanied by transient, sharp, severe epigastric pain 6 h earlier. On physical examination, she was a lean young woman with stable vital signs. Her abdomen was soft with no tenderness or muscle guarding. Bowel sounds were hypoactive with a normal pitch. Digital rectal examination showed bright red stools on the glove. Laboratory tests revealed normal peripheral blood cell counts and blood chemistry, except for leukocytosis with a white blood count of 145 000/mm3. Because she was admitted at a weekend, endoscopy was performed by an inexperienced endoscopist who had trained at our endoscopic center for 2 years. Gastroscopy was negative. Colonoscopy revealed blood and mucus throughout the colon. At colonoscopy, a reddish, soft, fist-sized polypoid was found 30 cm into the terminal ileum (Figure 1). Forcing forceps against the lesion depressed the lesion. The endoscopist tried to remove the lesion using various endoscopic accessories, because it was misdiagnosed as a hematoma. The patient began to complain of intermittent, severe periumbilical pain following the colonoscopic examination. Subsequent CT showed a typical inhomogeneous target-shaped soft-tissue mass with a layering effect, suggestive of enteric intussusception (Figure 2). An exploratory laparotomy revealed enteric intussusception, with gangrene. Segmental resection of the small intestine was performed. The pathology revealed an intussuscepted Meckel’s diverticulum with transmural infarction along the antimesenteric border (Figure 3). Microscopic examination disclosed an ectopic gastric mucosa and a complete proper muscle layer in the diverticular wall (Figure 4). The patient had an uneventful postoperative course and was discharged on the ninth post-operative day.
Figure 1.
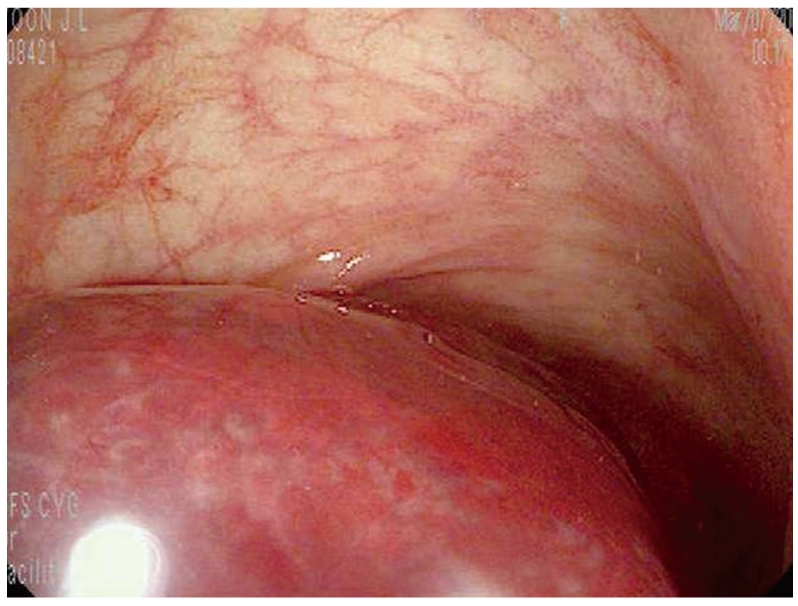
A polypoid lesion in the terminal ileum.
Figure 2.

Contrast-enhanced abdominal CT showed massive invagination of long segmental ileal loops.
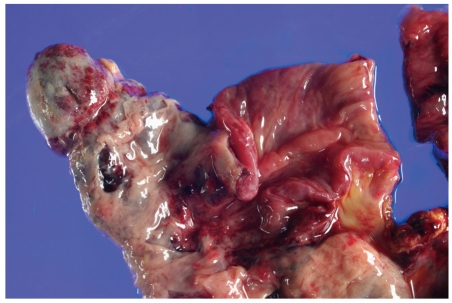
Figure 3.
Macroscopically, a diverticular sac was noted along the antimesenteric border. The entire wall of both the diverticulum and intestine was affected by hemorrhagic infarction and the luminal surfaces were covered with a necrotic exudate.
Figure 4.
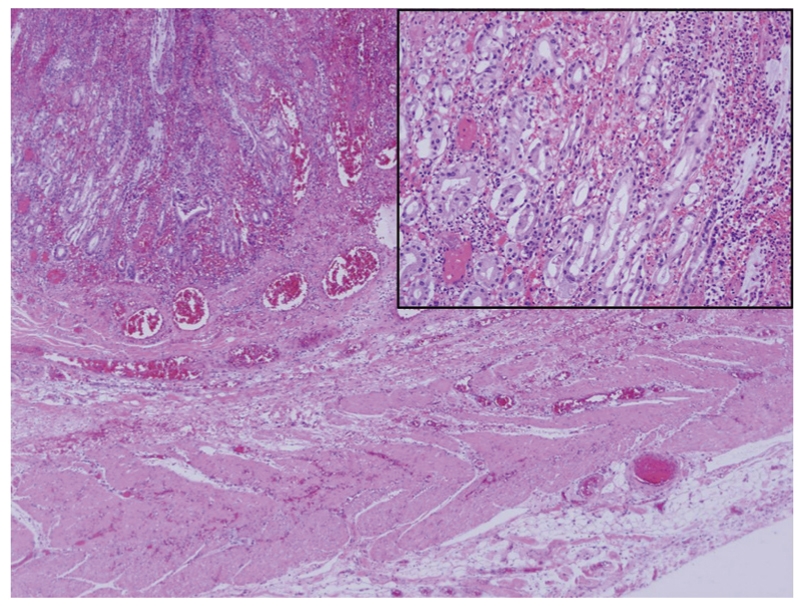
Microscopically, the diverticular sac was totally involved in transmural infarction. Its wall had a continuous proper muscle layer and heterotopic gastric mucosa (Inset). (HE, × 40; inset × 200).
DISCUSSION
Adult intussusception constitutes 5% of all cases of intussusception and accounts for only 1%-5% of intestinal obstructions in adults[3]. Almost 90% of the cases of intussusception in adults are secondary to a pathological condition that serves as a lead point, such as carcinomas, polyps, Meckel’s diverticulum, colonic diverticulum, and strictures or benign tumors, which are usually discovered intraoperatively[4-6]. A Meckel’s diverticulum is a remnant of the omphalomesenteric duct, which is normally obliterated by the 5th-8th wk of gestation. It is seen in 2% of the population. The lifetime risk of complications in patients with a Meckel’s diverticulum is only 4%[7]. Thus, an intussuscepted Meckel’s diverticulum is very rare, despite the well-known association of enteric intussusception and Meckel’s diverticulum.
Abdominal CT can help to confirm the presence of intussusception and distinguish between lead point and non-lead point intussusception and can potentially eliminate unnecessary surgery[7]. Colonoscopy is of little use for assessing intussusception. There are few reports on the colonoscopic features of an intussuscepted Meckel’s diverticulum[8,9]. An inexperienced endoscopist might be unfamiliar with these features, which appear to depend on the severity, chronicity, and etiology of the intussusception. A spring-shaped polypoid mass with surface erosion or a large number of blood vessels has been seen at colonoscopy in intussuscepted Meckel’s diverticulum without complications[8,9]. Incidental snare polypectomy might be performed in patients with chronic intussusception that presents as a polypoid mass on a barium or endoscopic examination[10]. This poses a high risk of perforation in a background of chronic tissue ischemia and possible necrosis of the intussuscepted bowel segment wall. An intussuscepted Meckel’s diverticulum, with gangrene, such as in our case, might be misdiagnosed as a hematoma at colonoscopy, because of the severe hyperemic and edematous mucosal changes. In conclusion, endoscopists should be aware of the endoscopic features of an intussuscepted Meckel’s diverticulum, because a colonoscopic examination can be performed initially, especially in an intussuscepted Meckel’s diverticulum presenting with hematochezia.
Footnotes
Peer reviewer: Takayuki Yamamoto, MD, Inflammatory Bowel Disease Center, Yokkaichi Social Insurance Hospital, 10-8 Hazuyamacho, Yokkaichi 510-0016, Japan
S- Editor Tian L L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Agha FP. Intussusception in adults. AJR Am J Roentgenol. 1986;146:527–531. doi: 10.2214/ajr.146.3.527. [DOI] [PubMed] [Google Scholar]
- 2.Kim YH, Blake MA, Harisinghani MG, Archer-Arroyo K, Hahn PF, Pitman MB, Mueller PR. Adult intestinal intussusception: CT appearances and identification of a causative lead point. Radiographics. 2006;26:733–744. doi: 10.1148/rg.263055100. [DOI] [PubMed] [Google Scholar]
- 3.Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226:134–138. doi: 10.1097/00000658-199708000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Akçay MN, Polat M, Cadirci M, Gencer B. Tumor-induced ileo-ileal invagination in adults. Am Surg. 1994;60:980–981. [PubMed] [Google Scholar]
- 5.Stubenbord WT, Thorbjarnarson B. Intussusception in adults. Ann Surg. 1970;172:306–310. doi: 10.1097/00000658-197008000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531–535. doi: 10.1016/0002-9610(71)90133-4. [DOI] [PubMed] [Google Scholar]
- 7.Turgeon DK, Barnett JL. Meckel's diverticulum. Am J Gastroenterol. 1990;85:777–781. [PubMed] [Google Scholar]
- 8.Lu CL, Chen CY, Chiu ST, Chang FY, Lee SD. Adult intussuscepted Meckel's diverticulum presenting mainly lower gastrointestinal bleeding. J Gastroenterol Hepatol. 2001;16:478–480. doi: 10.1046/j.1440-1746.2001.02335.x. [DOI] [PubMed] [Google Scholar]
- 9.Molnár T, Nagy F, Lonovics J, Tiszlavicz L. Intussusception and bleeding of a Meckel's diverticulum diagnosed by colonoscopy. Gastrointest Endosc. 2007;65:920; discussion 921. doi: 10.1016/j.gie.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407–411. doi: 10.3748/wjg.15.407. [DOI] [PMC free article] [PubMed] [Google Scholar]