Abstract
Background
Asian Americans suffer from liver and cervical cancer, both vaccine preventable, yet their awareness of such vaccines has not been described.
Methods
Cross-sectional survey (English and 5 Asian languages, 380 women, age 18+).
Results
Those with limited English proficiency (LEP) were less likely to have accurate knowledge of a cervical cancer vaccine (44 vs 76%, among the 34% reporting awareness of any cancer preventive vaccines); they were also more likely to believe vaccines existed for non-vaccine-preventable cancers. Moreover, despite high rates of hepatitis B-related liver cancer among Asians, awareness that a vaccine could prevent liver cancer was very low for both LEP and non-LEP women (under 30% among those aware of cancer vaccines).
Conclusion
This study highlights the need to educate and correct misconceptions about vaccine-preventable cancers among Asian American women, especially those who are LEP.
Introduction
Cancer is a leading cause of mortality in the US, and ethnic minorities are at risk for worse outcomes than majority individuals (1-3). Asian Americans have a higher incidence of some cancers than the general population. For example, in the California Cancer Registry (2000-2002), liver cancer rates were over 3 times higher for Asians/Pacific Islanders (API) than non-Hispanic Whites (NHW). Vietnamese men had an age-adjusted incidence 54.3 per 100,000; meanwhile, the rate for NHW was 6.8. Also, cervical cancer incidence is higher for Korean American and Vietnamese American women (11.4 and 14.0, respectively), but 7.3 for NHW (4). These findings for API in the US are consistent with international data showing high cervical cancer rates in Korea, South Asia, and Southeast Asia (1).
At present, only two FDA-licensed vaccines are available for prevention of cancer (5). These vaccines target cancer-causing infections: hepatitis B (HBV; hepatocellular carcinoma) and Human Papillomavirus (HPV; cervical cancer). While HBV vaccine was not heavily marketed for its cancer-preventive effects, the recent FDA approval of a quadrivalent HPV vaccine (6) has resulted in a flurry of mainstream discussion about prevention of cervical cancer through vaccination.
Minority communities with high rates of liver and cervical and cancers would benefit greatly from knowledge about HPV and HBV vaccine. However, linguistically isolated immigrants are not exposed to the same information sources as the general population. The purpose of the present study is to understand the level of awareness of vaccines to prevent cancer among Asian Americans.
Materials and Methods
A brief self-administered questionnaire was developed to collect data about awareness about anti-cancer vaccines. In addition to basic demographics, the following study questions were asked: “Have you heard about a vaccine against cancer?” and “If yes, what type of cancer does this vaccine protect against?” For the second question, respondents were asked to respond yes or no for the presence of a vaccine against each of the following cancers: colon, prostate, breast, stomach, cervix, lung, and liver. The questionnaire was translated from English to Cambodian, Chinese, Indonesian, Korean, and Vietnamese. Study questions were independently back-translated for confirmation. The number of questions was kept to a minimum due to community partner concerns about participant burden in a population unaccustomed to lengthy surveys.
A convenience sample of Asian Americans was recruited at an outreach event in May 2007. The event was an Asian women’s breast health event and included workshops about mammography and breast cancer prevention/early detection; women were also given an opportunity to register for free mammograms; vaccines were not part of the workshop curriculum. The event was publicized in ethnic newspapers as well as through 63 community partner organizations serving a variety of Asian immigrant communities with a linguistic mix consistent with the languages mentioned above. A total of 537 Asian American men and women attended the workshops. All attendees were invited to complete the questionnaire at the conclusion of the event (in their language of choice), and participants were given a tote bag as a token of thanks for their time.
Data were double-entered into a spreadsheet and analyzed using Intercooled Stata for Windows v8.2 (2005, StataCorp, College Station, TX). Demographics included gender, language of questionnaire, age, education, health insurance status, and self-reported English speaking ability. Limited English proficiency (LEP) was defined as ability to speak English “not well” or “not at all”, using a standard self-reported item. Since Cantonese and Mandarin use the same written language, they were combined as Chinese for data entry/analysis. Analysis included frequency calculations, cross-tabulations, and Pearson chi2 tests (Fisher’s exact test for cell counts < 5). In addition, unadjusted and multivariable logistic regression was performed to identify predictors of key dichotomous outcomes (awareness of anti-cancer vaccines and accurate knowledge of what types of cancer such vaccines prevent). Potential interactions were also evaluated, but final regression models included no interaction terms. All significance testing was based on α = 0.05.
This report is limited to the women who participated in the survey, due to the small number of men (42) as well as concerns that their responses might not be entirely independent of those provided by the women they accompanied (almost all men who attended did so because they were accompanying a female attendee).
All study materials were approved by the institutional review board of the University of Pennsylvania.
Results
Table 1 presents the demographics of the sample. A total of 380 women completed questionnaire forms (response rate 79%). Responses were categorized by language of administration, and there was a substantial difference in response rate between groups: 55% English, 63% Cambodian, 88% Chinese, 100% Indonesian, 40% Korean, and 68% Vietnamese. Although few people completed forms in English, a substantial number who completed forms in other languages reported being proficient in English.
Table 1.
Sample Characteristics
| Number of women (% of total) |
|
|---|---|
| Total | 380 (100%) |
| Language of questionnaire | |
| English | 5 (1.3%) |
| Cambodian | 90 (23.7%) |
| Chinese | 156 (41.1%) |
| Indonesian | 105 (27.6%) |
| Korean | 4 (1.1%) |
| Vietnamese | 20 (5.3%) |
| Age | |
| 29 and younger | 27 (7.3%) |
| 30 to 39 | 40 (10.9%) |
| 40 to 49 | 72 (19.6%) |
| 50 and over | 229 (62.2%) |
| Do you have health insurance? | 217 (58.5%) |
| Did you finish high school? | 193 (53.%) |
| How well do you speak English? | |
| not at all | 127 (34.7%) |
| not well | 167 (45.6%) |
| well | 44 (12.%) |
| very well | 28 (7.7%) |
Thirty-four percent of women in the sample reported awareness of a vaccine against cancer. Uninsured women were less likely to report awareness of an anti-cancer vaccine than insured women (23% vs 43%; chi2 p < 0.001). There was no significant variation based on age, high school education, or English proficiency. Multivariable logistic regression revealed a significant effect for uninsured status (OR 0.52; 95% confidence interval 0.28-0.97).
With respect to awareness of vaccines targeting specific cancers, substantial differences emerged with respect to English proficiency (see Figure 1). Among the women who reported awareness of any cancer vaccines, LEP women were more likely to incorrectly think a vaccine was available to prevent breast, colon, lung, prostate, or stomach cancer (40% vs 8% among the 34% reporting vaccine awareness; Fisher’s exact p = 0.002). Meanwhile, they were less likely to know that a vaccine can prevent cervical cancer (44% vs 76%; chi2 p = 0.004). No such difference existed with regard to knowledge about vaccine-preventable liver cancer (p > 0.05). Multivariable logistic regression (including independent variables for English proficiency, age, health insurance status, and education) revealed that LEP, age under 30, and uninsured status all significantly predicted identification of an incorrect target or failure to correctly identify cervix as a target for a cancer protection vaccine (OR 0.10, 0.05, and 0.16, respectively); assessment of interaction terms was not possible due to inadequate representation in some of the subgroups (e.g., LEP women under 40 with correct responses regarding cervical cancer). Meanwhile, the only significant predictor related to identification of liver as a target was high school education (OR 8.23). Language of questionnaire was not included in this regression due to small subgroup counts.
Figure 1. Belief in existence of a vaccine to prevent “x” cancer, by ability to speak English [all women].
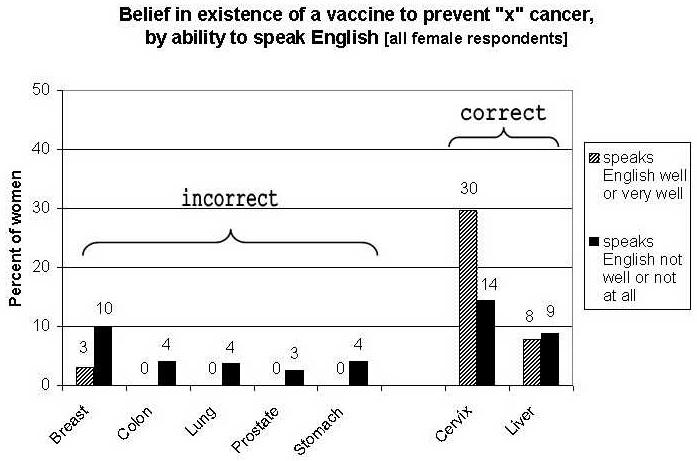
Striped bars represent women who speak English “well” or “very well”. Solid bars represent women who speak English “not well” or “not at all”.
Discussion
This study highlights the present need to ensure that linguistically isolated communities can benefit equally from advances in medical technology such as the new HPV vaccine. In a busy healthcare environment, providers are more likely to discuss preventive health issues when patients ask about them specifically (7); thus, it is critical to inform limited English proficient patients about available treatments so that they can advocate for their own care.
Despite the high prevalence of HPV infection among the American population, numerous surveys have documented relatively low levels of knowledge about the virus or its consequences. The Henry J. Kaiser Family Foundation in 2004 found that 70% of women had never heard of HPV and almost 90% had never discussed HPV with a healthcare provider (8). More recent data shows that HPV awareness is increasing, although many Americans remain unaware of the virus or its strong ties to cervical cancer (9-11). Results of a national survey of more than 3,000 women in 2005 showed that 40% of women had heard of HPV, but of those who had, less than 50% knew it caused cervical cancer and only 64% knew it was sexually transmitted (12). Unfortunately, we are aware of no published studies to date that have examined knowledge and exposure specifically among Asian Americans, and particularly those with LEP.
To compare our results to national data, we looked at data from the March-July 2007 iterations of the Annenberg National Health Communication Survey (ANHCS), an online health survey with a nationally representative panel of adults (unpublished observations). Specific data on Asian respondents were not available, so we examined the “other” race category (non-Hispanic, non-Black, non-White). In response to the question, “Have you heard anything about a vaccine that prevents cervical cancer or HPV, the virus that causes it?”, only 60.9% answered yes, as compared to 71.2% of NHW (n=23 other, 490 NHW). However, ANHCS is limited to English-proficient participants.
Young women would benefit most from HPV vaccination, yet they seem least informed in our Asian American sample. While younger White women tend to have higher levels of knowledge about HPV than their older peers, younger minority women, such as Asian Americans, frequently report lower levels of knowledge(12). This could be due to cultural differences within the Asian family or community that limit discussions about STIs or the lack of HPV vaccination campaigns targeting Asian American youth. Prior efforts targeting youth for hepatitis B vaccination have been effective in Asian American communities (13) and could become a model for the development of HPV campaigns. At the same time, educating older women can still be important. In traditional Asian households, the advice of parents and grandparents holds tremendous weight (14); thus, increased knowledge among older adults can still potentially lead to improved HPV vaccination rates among younger females.
At the same time, the apparently low awareness of Hepatitis B vaccine and its potential role in the prevention of hepatocellular carcinoma is troubling. Genetically-engineered hepatitis B vaccination has been licensed for use in the U.S. since 1987 (15), but knowledge about this cancer prevention tool appears to be low in the high risk Asian American population.
Also, a minority of LEP women incorrectly believed that vaccines existed to prevent breast, colon, lung, prostate and stomach cancer, suggesting that while some messages about cancer preventive vaccines might be reaching these women, the message likely is incomplete and resulting in confusion.
Our findings also emphasize the continuing need to address the nation’s health insurance crisis. Insurance status was an important predictor of both general cancer vaccine awareness and awareness of vaccines to prevent cervical cancer. It is uncertain whether insured women heard this information from insurance mailings, from doctors, or from other sources. It would be helpful to understand current health communication streams better in order to take advantage of existing avenues of dissemination. One should also remember that, even if uninsured women wanted to be vaccinated, it is likely that cost would be a significant barrier. Policy changes to make health insurance and primary healthcare more accessible to these communities could lead to improvements in awareness, knowledge, and vaccine uptake.
This study is limited by the fact that participants were recruited using convenience sampling rather than population-based sampling. However, participants were recruited to the event by 63 partner organizations having extensive experience in reaching the most isolated and at-risk communities, and we are confident that our sample includes many of the hardest-to-reach segments of the Asian American population. In addition, we used self-administered paper-based questionnaires, thus limiting this study to women who were literate. It is possible that knowledge rates among illiterate populations could be substantially worse.
There is a possibility of selection bias in our sample, since the women who attended the event knew that it was a special program focusing on Asian women’s health, including breast health education and the opportunity to register for free mammograms. These women likely had an elevated level of interest in health and prevention. However, one might expect that women with increased interest in health would have high knowledge of the vaccines, but this did not seem to be the case. Another limitation is that this sample did not include women with preference for South Asian languages (Gujurati, Hindi, Punjabi, etc.). Therefore, we cannot comment on whether South Asian women might be similar to the East and Southeast Asian women described here.
Our sample represents the most disadvantaged segments of the Asian American population. For example, only 59% reported having health insurance, while national reports suggest nearly 70% of API have health insurance (16). Also, our sample is more linguistically isolated than the general API population (17). Thus, our study provides a greater understanding of an often under-studied portion of the Asian American population. With over 12 million Americans identifying as Asian, it is estimated that over 4 million Asian Americans do not speak English very well (17).
The availability of vaccines that can prevent liver and cervical cancer presents a great opportunity to improve the health of Asian American populations in an area where significant disparities currently exist. By addressing issues of health insurance and language access, and by creating health communication interventions that target linguistically isolated communities, we have the potential to create a positive change for an at-risk and often neglected population.
Acknowledgments
Supported by a Cancer Control Career Development Award from the American Cancer Society (GTN, CCCDA-05-161-01), a Pfizer Fellowship in Health Literacy/Clear Health Communication (GTN), the National Cancer Institute (AEL, P50CA095856) and the Annenberg Foundation Trust at Sunnylands (AEL). The data were collected at a community outreach event sponsored by the American Cancer Society Pennsylvania Division Southeast Region and Susan G. Komen for the Cure Philadelphia Affiliate. The authors wish to thank the community partners/event volunteers for participant recruitment and Bryan Anmuth for data entry. We also thank Drs. Marjorie Bowman, Diane Harper, and Joshua Metlay for review of earlier versions of this manuscript.
Footnotes
Presented at the American Association for Cancer Research Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved, Atlanta, GA, November 2007.
References
- 1.American Cancer Society Cancer Facts and Figures 2005. American Cancer Society: Atlanta. 2005 [Google Scholar]
- 2.Chen MS., Jr. Cancer health disparities among Asian Americans: what we do and what we need to do. Cancer. 2005;104(12 Suppl):2895–902. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- 3.Freeman HP, Wingrove BK. National Cancer Institute, Center to Reduce Cancer Health Disparities (NIH, US Department of Health and Human Services); Rockville (MD): 2005. Excess cervical cancer mortality: A marker for low access to health care in poor communities. [Google Scholar]
- 4.McCracken M, et al. Cancer Incidence, Mortality, and Associated Risk Factors Among Asian Americans of Chinese, Filipino, Vietnamese, Korean, and Japanese Ethnicities. CA Cancer J Clin. 2007;57(4):190–205. doi: 10.3322/canjclin.57.4.190. [DOI] [PubMed] [Google Scholar]
- 5.National Cancer Institute NCI Cancer Vaccine Fact Sheet Internet web site 2006http://www.cancer.gov/cancertopics/factsheet/cancervaccine(accessed 7/17/2007).
- 6.Dunne EF, Markowitz LE. Genital human papillomavirus infection. Clinical Infectious Diseases. 2006;43(5):624–9. doi: 10.1086/505982. [DOI] [PubMed] [Google Scholar]
- 7.Guerra CE, et al. Are Physicians Discussing Prostate Cancer Screening with Their Patients and Why or Why Not? A Pilot Study. Journal of General Internal Medicine. 2007;22(2) doi: 10.1007/s11606-007-0142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henry J. Henry J. Kaiser Family Foundation; Washington, DC: 2004. Kaiser Family Foundation, National survey of public knowledge of HPV, the human papillomavirus. [Google Scholar]
- 9.National Cervical Cancer Coalition . NCCC; Van Nuys, CA: 2006. National quorum - expectations and awareness of medical technologies, cervical cancer screening, HPV testing. [Google Scholar]
- 10.National Cancer Institute . National Cancer Institute, National Institutes of Health; Bethesda, MD: 2006. Health Information National Trends Survey: Briefs, No.3. [Google Scholar]
- 11.Friedman AL, Shepeard H. Exploring the Knowledge, Attitudes, Beliefs, and Communication Preferences of the General Public Regarding HPV: Findings From CDC Focus Group Research and Implications for Practice. Health Education and Behavior. 2007;34(3):471–485. doi: 10.1177/1090198106292022. [DOI] [PubMed] [Google Scholar]
- 12.Tiro JA, et al. What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiology, Biomarkers & Prevention. 2007;16(2):288–94. doi: 10.1158/1055-9965.EPI-06-0756. [DOI] [PubMed] [Google Scholar]
- 13.Hsu LD, et al. Student leadership in public health advocacy: lessons learned from the hepatitis B initiative. American Journal of Public Health. 2003;93(8):1250–2. doi: 10.2105/ajph.93.8.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng S-T, Chan ACM. Filial piety and psychological well-being in well older Chinese. Journals of Gerontology Series B-Psychological Sciences & Social Sciences. 2006;61(5):P262–9. doi: 10.1093/geronb/61.5.p262. [DOI] [PubMed] [Google Scholar]
- 15.Stehnlin D, Hepatitis B.Available Vaccine Safe and Underused 1990http://www.fda.gov/bbs/topics/CONSUMER/CON00062.html(accessed 6/20/2008). [PubMed]
- 16.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Affairs. 2005;24(2):398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 17.US Census Bureau The American Community - Asians: 2004, in American Community Survey Reports. 2007.


