Abstract
Objective To assess the effectiveness of acute geriatric units compared with conventional care units in adults aged 65 or more admitted to hospital for acute medical disorders.
Design Systematic review and meta-analysis.
Data sources Medline, Embase, and the Cochrane Library up to 31 August 2008, and references from published literature.
Review methods Randomised trials, non-randomised trials, and case-control studies were included. Exclusions were studies based on administrative databases, those that assessed care for a single disorder, those that evaluated acute and subacute care units, and those in which patients were admitted to the acute geriatric unit after three or more days of being admitted to hospital. Two investigators independently selected the studies and extracted the data.
Results 11 studies were included of which five were randomised trials, four non-randomised trials, and two case-control studies. The randomised trials showed that compared with older people admitted to conventional care units those admitted to acute geriatric units had a lower risk of functional decline at discharge (combined odds ratio 0.82, 95% confidence interval 0.68 to 0.99) and were more likely to live at home after discharge (1.30, 1.11 to 1.52), with no differences in case fatality (0.83, 0.60 to 1.14). The global analysis of all studies, including non-randomised trials, showed similar results.
Conclusions Care of people aged 65 or more with acute medical disorders in acute geriatric units produces a functional benefit compared with conventional hospital care, and increases the likelihood of living at home after discharge.
Introduction
Adequate hospital care for older people (≥65 years) with acute medical disorders requires a comprehensive assessment by multidisciplinary teams to detect early those patients at highest risk of functional decline and institutionalisation.1 2 3 Such care also requires early planning for discharge, and follow-up.1 2 3 The primary aim of this model of care is to reduce functional decline, which is the main determinant of quality of life, cost of care, and vital prognosis.4 Delaying functional decline and increasing the chances of living at home are at least as important as reducing case fatality in frail older people.2
Several interventions have been proposed to improve the effectiveness and efficiency of hospital care for older people with acute medical disorders. Assessment of geriatric patients by a multidisciplinary consultation team has not, however, shown benefits for case fatality, functional decline, or place of residence at discharge.2 5 Hospital at home care for elderly medical patients reduces hospital stay but increases overall length of care, and objective evidence of economic benefit is insufficient.6 Another type of intervention is that provided by multidisciplinary geriatric teams in “acute care for elders units” or acute geriatric units. Previous reviews lumped such units with geriatric evaluation and management units, which normally care for elderly people after stabilisation of an acute condition.2 7 8 9 Other reviews have focused on partial aspects of acute care such as discharge planning or physiotherapy.10 11 To our knowledge only one review has been published on the effectiveness of acute geriatric units, and that provided only descriptive data.12
We systematically reviewed studies on the effect of acute geriatric units compared with conventional hospital care in the treatment of older people with acute medical disorders. We hypothesised that acute geriatric units would reduce functional decline, increase the proportion of patients able to live at home after discharge, reduce case fatality, and result in shorter hospital stays than conventional hospital units.
Methods
Our review included randomised trials, non-randomised trials, and case-control studies that compared outcome of care in acute geriatric units with that in conventional hospital units in patients aged 65 years or more with acute medical disorders. Acute geriatric units were defined as hospital units with their own physical location and structure and run by a specialised multidisciplinary team with direct responsibility for the care of elderly people with acute medical disorders, including acute exacerbations of chronic diseases. This definition is based on seminal research on acute geriatric units1 2 w3 w6 and is consistent with previous definitions in this discipline; for example, two studies stated that an acute geriatric unit is an interdisciplinary model for providing care to older adults during admission to hospital for an acute medical illness.4 13 These studies agreed with those of other authors that the acute geriatric unit is a defined medical unit that uses an interdisciplinary team specialising in geriatric care to provide increased attention to a patient’s level of functioning, specific treatment of diagnoses common to older people, and integrated planning of discharge to maximise clinical outcomes.4 13 w5 w9 w10 Patients are admitted to acute geriatric units for acute problems such as pneumonia, heart failure, sepsis, delirium, urinary tract infections, or chronic obstructive pulmonary disease, which do not require treatment in other specialised units (for example, intensive care unit or coronary unit).
We excluded studies that used secondary data from databases designed for the purposes of healthcare administration, with information not collected directly from the patients by the researchers. We also excluded studies that evaluated interventions aimed at a specific medical disorder (for example, stroke units, psychogeriatric units) or surgical process (for example, orthogeriatric units). To ensure we did not include studies that evaluated care provided out of the acute phase we excluded studies that assessed units with care lasting beyond the acute phase and those with patients admitted to the intervention unit three or more days after hospital admission.
Outcome variables
The primary outcomes were functional decline, living at home, and case fatality at discharge and three months later. We considered functional decline to be loss of independence in one or more basic activities of daily living compared with the situation before admission.4 14 To assess basic activities of daily living we used the Katz index and the Barthel index; each basic activity (transfers, mobility, dressing, eating, bathing) was classified as independent or dependent according to the need for physical assistance to carry out the activity.14 w3 w6 w10 The secondary outcomes were hospital stay during the index admission, the cost of the index admission, and readmission at three months after discharge.
Literature search and data extraction
We searched Medline, Embase, and the Cochrane central register of controlled trials up to 31 August 2008 (see web extra appendix for search strategy) and scanned the reference lists of reviews and relevant articles. We included articles in English and Spanish. To obtain information on unpublished studies or to complete data for published studies on the hospital unit, patients’ characteristics, hospital stay, and costs we contacted the authors.
Two investigators (JJB and FS) evaluated the eligibility and methodological quality of studies obtained from the literature search. In cases of discrepancy a third researcher (JLA) reviewed the studies, and agreement was reached by consensus. JJB and FS independently extracted and compared the data.
Quality assessment
For randomised trials we extracted information on concealment of allocation, the proportion of patients lost to follow-up, the use of intention to treat analysis, and whether the assessment of outcomes was done blinded to intervention group. For non-randomised trials we recorded only losses to follow-up and type of outcome assessment.
We summarised the overall quality of randomised trials with the Jadad scale, excluding blinding of the intervention as this is not possible for acute geriatric units.9 15 Thus the scores ranged from 0 to 3. For all studies we also used the Van Tulder scale, scored from 0 to 19 (highest quality), which has been used in other systematic reviews of interventions in the care of elderly people.16
Data synthesis
For dichotomous outcomes we give the results as combined odds ratios with 95% confidence intervals and for quantitative outcomes as differences in means with standard errors. We used fixed effects methods to combine the outcomes across studies, except when important heterogeneity was observed. Heterogeneity was quantified with the I2 statistic, which measures the percentage of variation among studies due to heterogeneity rather than to chance. For practical purposes we considered heterogeneity to be important when I2 was more than 30%. When it was considered appropriate to combine results in these cases, we used random effects methods.17
When we were unable to retrieve the standard deviation for length of hospital stay and cost of hospital admission, we approximated it from the standard error and 95% confidence intervals.18 When we were unable to estimate the standard deviation, we contacted the authors; this was provided for one study.w6 In three studiesw1 w3 w11 we had to assume that the standard deviation was the same as the mean. Finally, given that we had specific data from each of the two centres that participated in one of the studies,w1 we considered them as independent studies for the analysis of hospital stay and its cost.
Although we created funnel plots to identify possible publication biases, these proved difficult to interpret given the small number of studies. Statistical analyses were carried out using RevMan 4.3 (Cochrane Collaboration).
Results
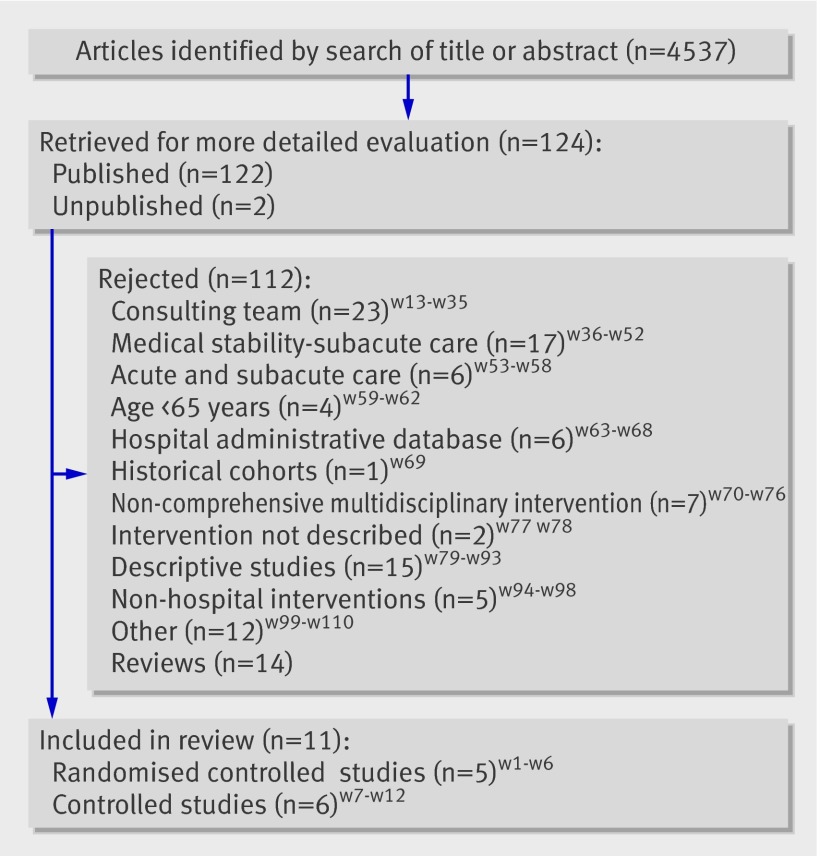
The literature search yielded 4038 articles. After review of the titles and abstracts 119 articles were selected for critical reading. Twelve articles totalling 11 studies met the inclusion criteria (fig 1). Seven of these were done in the United States and the remainder in Australia, Canada, Sweden, and Peru. Authors of five studies were contacted for additional data,w3 w5 w6 w9 w10 but for only onew6 was unpublished data on patients’ living at home after discharge and at three months used.
Fig 1 Flow of papers through study
The table presents the principal characteristics of the included studies. Five were randomised trials,w1-w6 four were non-randomised trials,w7-w10 and two were retrospective case-control studies.w11 w12
Characteristics of studies included in meta-analysis
| Study (setting) | Design (quality) and participants | Comparison groups | Intervention | Usual care | Outcomes | Time of assessment | |
|---|---|---|---|---|---|---|---|
| Acute geriatric unit | Control | ||||||
| Collard 1985w1 (2 community hospitals, USA) | Randomised controlled trial (Jadad 1, Van Tulder 9), medical and surgical patients aged 65 or more admitted from emergency department: 33% acute geriatric unit, 45% control | n=218; mean age 78.5 years, 67% women; 10% residing in nursing home, major diagnostic admission: cardiac 10%, respiratory 26%, fractures 13%, cerebrovascular or neurological 24%, intestinal 16% | n=477; mean age 78 years, 59% women; 8.4% residing in nursing home, major diagnostic admission: cardiac 19%, respiratory 27%, fractures 15%, cerebrovascular or neurological 22%, intestinal 9% | 2 acute geriatric units (10 beds), comprehensive assessment, interdisciplinary conferences twice weekly, early discharge planning. Core team: registered nurse trained for project, social worker, physiotherapist, occupational therapist, physician | Not described | Case fatality, institutionalisation, self related health, length of stay, costs | Hospital admission, and discharge |
| Harris 1991w2 (general hospital, Australia) | Randomised controlled trial (Jadad 2, Van Tulder 9), medical patients aged 70 or more not residing in nursing home, 100% admitted from emergency department | n=97; mean age 79 years, 65% women, major diagnostic admission: circulatory 49.5%, respiratory 10.3%, mental disorders 7.2%, neoplasm 5.2%, gastrointestinal 5.2% | n=170; mean age 78 years, 59% women, major diagnostic admission: circulatory 46.5%, respiratory 17.1%, mental disorders 4.1%, neoplasm 3.5%, gastrointestinal 3.5% | Acute geriatric unit (14 beds), comprehensive assessment. Core team: registered nurse, social worker, physiotherapist, occupational therapist, physician | Similar medical staff but less time devoted by nursing and dedicated physiotherapist, occupational therapist, and social worker. Similar access to undertake discharge planning | Case fatality, institutionalisation, functional and cognitive outcomes, length of stay | Hospital admission, discharge, and 3, 6, 9, and 12 months after discharge |
| Landefeld 1995w3 w4 (university hospital, USA) | Randomised controlled trial (Jadad 3, Van Tulder 14.5), medical patients aged 70 or more not admitted to a speciality unit (intensive, cardiology, oncology), 100% admitted from emergency department | n=327; mean age 80.2 years, 68% women, 7% in long term care. Independence basic activities of daily living 62%, major diagnostic admission: neurological 11%, cardiac 18%, infections 18%, pulmonary 19%, gastrointestinal 19% | n=324; mean age 80.1 years, 65% women, 9% residing in long term care, independence basic activities of daily living 62%, major diagnostic admission: neurological 13%, cardiac 15%, infections 20%, pulmonary 14%, gastrointestinal 20% | Acute geriatric unit (14 beds) prepared environment, comprehensive assessment, interdisciplinary conference daily, medical review daily, early discharge planning. Core team: geriatrician, registered nurse, social worker, physiotherapist, nutritionist | Similar hospital supported staffing ratios and access to similar hospital provided support services | Case fatality, institutionalisation, functional and mental outcomes, self related health, length of stay, costs | Hospital admission, discharge, and 3 months after discharge |
| Asplund 2000w5 (university hospital, Sweden) | Randomised controlled trial (Jadad 2, Van Tulder 13.5), medical patients aged 70 or more not admitted to a specialty unit (intensive, cardiology, stroke), 100% admitted from emergency department | n=190; mean age 81 years, 58% women, 16% residing in an institution, baseline independence in basic activities of daily living 52% | n=223; mean age 81 years, 63% women, 16% residing in an institution, baseline independence in basic activities of daily living 44% | Acute geriatric unit (11 beds) organised solely for study, comprehensive assessment, interdisciplinary conference 1 day a week, early rehabilitation and discharge planning. Core team: internist, geriatrician, registered nurse, physiotherapist, occupational therapist, dietician | In unit: no physiotherapist, occupational therapist, or dietician routinely available. Social worker part time. No geriatrician. Frequent relation between staff of both acute geriatric and usual care units) | Case fatality, institutionalisation, functional and cognitive outcomes, psychological wellbeing, length of stay, costs | Hospital admission, discharge, and 3 months after discharge |
| Counsell 2000w6 (community teaching hospital, USA) | Randomised controlled trial (Jadad 3, Van Tulder 14.5), medical patients aged 70 or more not admitted to a specialty unit (intensive, cardiology, oncology) and not residing in a nursing home, 100% admitted from emergency department | n=767; mean age 80 years, 60% women, independence in basic activities of daily living 61%, major diagnostic admission: neurological 19%, cardiac 11%, infections 14%, pulmonary 25%, gastrointestinal 20% | n=764; mean age 79 years, 61% women, independence in basic activities of daily living 63%, major diagnostic admission: neurological 21%, cardiac 12%, infections 14%, pulmonary 23%, gastrointestinal 17% | Acute geriatric unit (34 beds) prepared environment, comprehensive assessment, interdisciplinary conference daily, medical review daily, early discharge planning. Core team: geriatrician, registered nurse, social worker, physiotherapist | Similar attending physician and nursing staff to patient ratio and hospital provided support services | Case fatality, institutionalisation, functional outcomes, and patient, caregiver, and staff satisfaction, length of stay, costs | Hospital admission, discharge, and 1, 3, 6, and 12 months after discharge |
| Meissner 1989w7 (community teaching hospital, USA) | Prospective controlled trial (Van Tulder 7), medical patients aged 70 or more with potential for functional recovery, patients assigned to units based on administrative criteria such as availability of beds and staff | n=103; mean age 81 years, 71% women, 63% admitted from emergency department | n=75; mean age 80 years, 61% women, 61% admitted from emergency department | Acute geriatric unit (20 beds), comprehensive assessment, interdisciplinary conference 1 day a week, physiotherapy, and early discharge planning. Core team: geriatric nurse coordinator; therapists | Not described | Case fatality, institutionalisation, functional outcomes, length of stay, costs | Hospital admission, and discharge |
| Stewart 1999w8 (community teaching hospital, USA) | Prospective controlled trial (Van Tulder 5), medical patients aged 75 or more not fully independent or terminally ill. If aged 75-85, other frailty criteria were necessary. “Convenience sample” approximation | n=34; mean age 86 years, 49% women | n=27; mean age 82 years, 63% women | Acute geriatric unit (14 beds), comprehensive assessment, continuity of care. Core team: geriatrician, registered nurse, social worker | Not described | Length of stay, costs | Hospital admission and discharge |
| Wong 2006w9 (teaching hospital, Canada) | Prospective controlled trial (Van Tulder 11), medical patients aged 75 or more. Excluded: critical care, palliative care, post-anaesthetic recovery. Patients placed in acute geriatric unit if bed available, usual care wards had six stroke beds | n=324; mean age 83.4 years, 58% women, 22.7% residing in a nursing home, major diagnostic admission: neurological 9.5%, cardiovascular 21.6%, infections 25.3%, pulmonary 8.3%, gastrointestinal 13.3%, malignancy 4.6% | n=221; mean age 82.3 years, 54% women, 16.4% residing in a nursing home, major diagnostic admission: neurological 31%, cardiovascular 9%, infections 13.1%, pulmonary 9.5%, gastrointestinal 13.6%, malignancy 5.4% | Acute geriatric unit (21 beds) prepared environment, comprehensive assessment, interdisciplinary rounds 2 days a week, medical review daily, early rehabilitation and discharge planning. Core team: geriatrician, registered nurse, social worker, physiotherapist, occupational therapist, dietician, and pharmacist | One interdisciplinary round a week, fewer geriatric medicine and psychiatry consultations available, same hospital and family practitioners involved in acute geriatric and usual care units | Case fatality, institutionalisation, length of stay, readmission | Hospital admission and discharge |
| Zelada 2007w10 (military hospital, Peru) | Prospective controlled trial (Van Tulder 10), medical patients aged 65 or more not admitted to intensive unit. Excluded: dependent in all basic activities of daily living, severe dementia, severe aphasia, terminal cancer. Patients admitted to unit according to criteria of emergency department team and to availability of beds | n=68; mean age 79.6 years, 62% women, 79.4% admitted from emergency department, baseline independence in basic activities of daily living 43%, major diagnostic admission: respiratory 26.5%, gastrointestinal 17.6%, cardiovascular 8.8%, renal 14.7%, metabolic 4.4% | n=75; mean age 76 years, 56% women, 74.7% admitted from emergency department. Baseline independence in basic activities of daily living 51%, major diagnostic admission: respiratory 22.7%, gastrointestinal 13.3%, cardiovascular 25.3%, renal 6.7%, metabolic 8% | Acute geriatric unit (10 beds), comprehensive assessment, interdisciplinary rounds 1 day a week, early discharge planning. Core team: geriatrician, registered nurse, social worker, physiotherapist, occupational therapist | Not described | Functional outcomes, length of stay | Hospital admission and discharge |
| Barrick 1999w11 (university hospital, USA) | Retrospective case-control (Van Tulder 8), medical patients aged 65 or more living in nursing home matched by age and functional status | n=384; mean age 84.4 years, 69% women, patients significantly more impaired in basic activities of daily living | Usual care unit in same hospital (n=74, mean age 81.3 years, 61% women) and usual care unit in other hospital (n=309, mean age 83 years, 69% women) | Acute geriatric unit (20 beds), comprehensive assessment, continuity of care. Core team: geriatrician, registered nurse | Not described | Case fatality, length of stay | Hospital admission, discharge, and 6 months after discharge |
| Javadevappa 2006w12) (university hospital, USA) | Retrospective case-control (Van Tulder 9), medical patients aged 65 or more with congestive heart failure, pneumonia, or urinary tract infection, not admitted to specialty units (intensive, cardiology, oncology), matched by sex, age, ethnicity and comorbidity, alive at follow-up | n=680; mean age 79.6 years, 67% women, 43% residing in a nursing home | n=680; mean age 79.2 years, 70% women, 27% residing in a nursing home | Acute geriatric unit (36 beds) prepared environment, comprehensive assessment, interdisciplinary rounds 3 days weekly, medical review daily, early discharge planning. Core team: geriatrician, geriatric nurse, social worker, physiotherapist, occupational therapist, dietician, and pharmacist | Similar staffing and nurse to patient ratio | Utilisation of health resources, length of stay, costs | Hospital admission and discharge |
The methodological quality of the studies was heterogeneous, especially for non-randomised trials (table). Three of the randomised trials used sealed envelopes to allocate patients to groups.w3 w5 w6 Only one of them did an intention to treat analysis at discharge, but this was not done at follow-up.w6 Of the four non-randomised trials, three used informal procedures for allocation based on bed availability.w7 w9 w10
Criteria for patient selection were age plus a medical condition not requiring admission to specialty units. Five studies included patients aged 70 or more,w2 w7 three aged 65 or more,w1 w10 w11 and one aged 75 or more.w9 One study selected patients aged 75 or more with at least one geriatric condition.w8 Finally, one study selected patients aged 65 or more who were admitted for heart failure, pneumonia, or urinary tract infection.w12 Two studies excluded older people (≥70 years) living in a nursing home,w2 w6 whereas anotherw11 included only those who lived in a nursing home.
In four of the five randomised trials all the patients came from emergency services,w2-w6 whereas in three non-randomised studies more than 62% came from emergency services.w7 w9 w10 Three studies did not provide this information.w8 w11 w12
The intervention units functioned in similar ways, generally having four characteristics that distinguished them from conventional units: comprehensive geriatric assessment of patients, use of standardised instruments for measurements, weekly multidisciplinary meetings, and early planning of discharge. The composition of the basic multidisciplinary team typically included at least one geriatrician, nursing staff trained in geriatrics, a social worker, and therapists.
The follow-up period varied. All the randomised studies except onew1 provided follow-up data at three months, at a minimum. Five studies reported on readmissions, two at three months after dischargew3 w5 and three at one month after discharge.w6 w9 w11
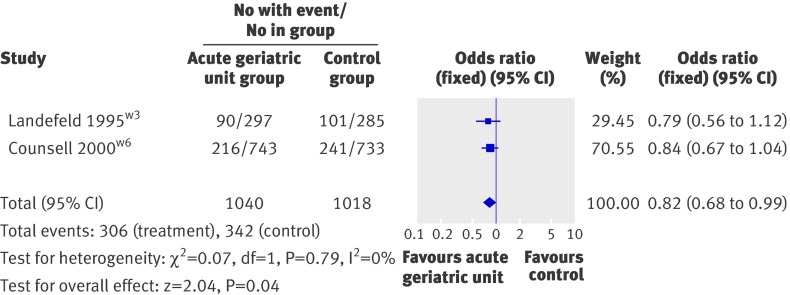
Functional decline
Only three studies presented results on functional decline at discharge, two of which were randomised trials (fig 2). In these two studies, which accounted for more than 65% of patients in the randomised trials, the patients in acute geriatric units showed a lower risk of functional decline than those in conventional units (combined odds ratio 0.82, 95% confidence interval 0.68 to 0.99). After the inclusion of a non-randomised study, results were similar (0.78, 0.65 to 0.94) but showed greater heterogeneity (I2=55.7%) because of the large reduction in functional decline in the acute geriatric unit in that study (0.35, 0.17 to 0.76).w10
Fig 2 Functional decline at discharge from hospital in randomised trials comparing acute geriatric units with conventional hospital care
Only one studyw6 provided data on functional decline at three months after discharge, with no differences in the incidence of functional decline between the groups. Another three randomised studies provided data that could not be analysed but reported an absence of differences in functional decline at three months after discharge.w2 w3 w5
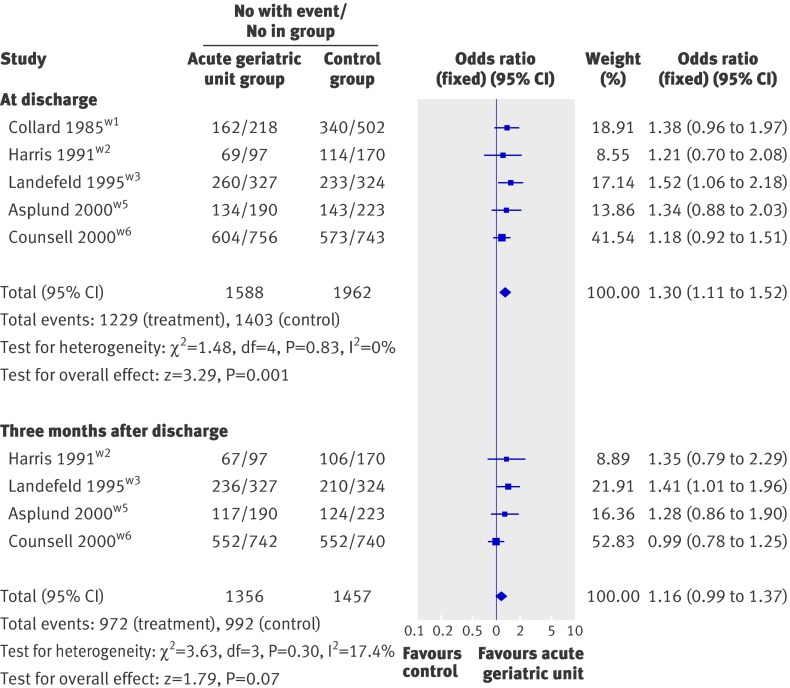
Living at home
In randomised studies, patients cared for in acute geriatric units were more likely to be living at home after discharge (1.30, 1.11 to 1.52), a benefit that was marginally maintained three months after discharge (fig 3). Results at discharge still held when analyses were repeated including non-randomised studies (1.28, 1.12 to 1.47).
Fig 3 Living at home at discharge from hospital and three months after discharge in randomised trials comparing acute geriatric units with conventional hospital care
Acute geriatric units and conventional care units showed no differences in frequency of admission to a nursing home at discharge (0.76, 0.51 to 1.28) or three months after discharge (0.90, 0.74 to 1.14).
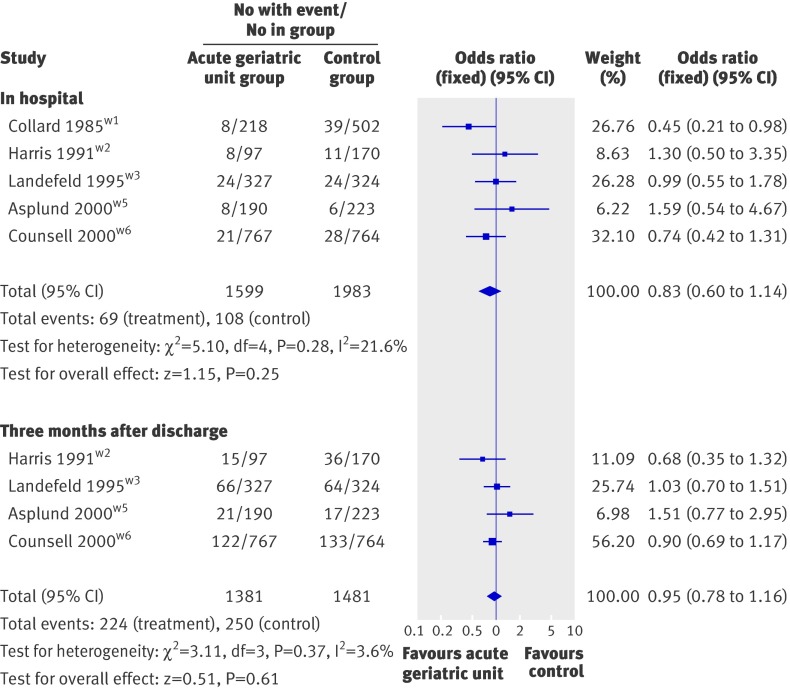
Case fatality
No significant differences were found in case fatality between acute geriatric units and conventional care units either in hospital or three months after discharge (fig 4). The results were similar in the randomised and non-randomised studies, although in the randomised studies case fatality at discharge ranged between 2.5% and 9% whereas in the non-randomised studies it exceeded 10%.
Fig 4 Case fatality in hospital and three months after discharge in randomised trials comparing acute geriatric units with conventional hospital care
Length of hospital stay and cost of admission
All the included studies reported on length of hospital stay, but three did not report dispersion measures.w1 w3 w11 The length of stay in the acute geriatric units was fewer than 12 days, and fewer than nine days in the studies published from 1995. In nine of the 11 studies a trend was observed towards a reduced length of stay, of 6-39%.w1 w3 w5 w6 w8-w12 However, the reduced length of stay was heterogeneous among studies; I2 was 49.4% in the randomised studies and 74.1% in the non-randomised studies. This heterogeneity limits firm conclusions being reached on this outcome.
Data on the cost of hospital stay were reported in four of the five randomised studiesw1 w3-w6 and in three of the six non-randomised studies.w7 w8 w12 The US dollar was used in all studies except for one that used Swedish crowns, with the dollar conversion calculated according to the exchange rate provided by the authors.w5 Although the data are difficult to interpret because they did not allow cost effectiveness ratios to be estimated, a slightly, yet significant, lower cost of hospital care was found in acute geriatric units (combined mean difference −0.31, 95% confidence interval −0.52 to −0.09; I2=0%).
Two randomised studiesw3 w5 provided data on readmissions to hospital at three months after discharge, and another randomised studyw6 and two non-randomised studies reported on readmissions in the month after discharge.w9 w11 Another two studiesw7 w12 provided data in a format that was not useful for analysis. The combined odds ratio for readmission at three months in patients discharged from acute geriatric units compared with conventional units in all studies was 0.93 (95% confidence interval 0.77 to 1.11) and in the randomised studies was 1.11 (0.92 to 1.35).
Sensitivity analysis
Separate analyses for the randomised studies and the other studies provided similar results, except that the reduction in hospital stay was larger in the non-randomised studies. The analysis was repeated after excluding the oldest studies (those published before 1995 and that lacked a geriatrician), and after assuming adverse results in people lost to follow-up or lacking data on outcomes. No substantial changes in the results were found in any of these cases.
Discussion
The results of this meta-analysis suggest that care of older people (≥65 years) with acute medical disorders in acute geriatric units leads to less functional decline at discharge and a higher probability of living at home after discharge. The effect of geriatric assessment has been evaluated in different care settings.8 In the case of patients admitted to hospital for acute medical disorders, only the activity of multidisciplinary consultation teams has been assessed, with no benefits found for case fatality, functional decline, or living at home after discharge.2 Since admission to hospital is a risk factor for case fatality, functional decline, and admission to a nursing home, any intervention that helps reduce this risk is potentially important.19
The 18% reduction in functional decline associated with acute geriatric units is similar to that found in a study of patients aged 65 or more with acute medical disorders who received physiotherapy within multidisciplinary care.11 Furthermore, the benefit of living at home after discharge was comparable to that reported in another study in the combined analysis of acute and subacute hospital care units.2
This improvement in functional outcomes was not accompanied by an increased rate of admissions at three months or increased case fatality. Although the tendency towards a higher probability of living at home was maintained at three months after discharge from an acute geriatric unit, the reduction in functional decline was seen only at discharge; thus future studies should examine whether it persists in the medium term. We did not find a reduction in case fatality either at discharge or at three months follow-up. This is a common finding in studies of very old (frequently aged 80 or more) or frail people. In fact, several authors and older people too feel that improving case fatality at the expense of disability and dependence should not be considered an optimal outcome.2 20
Characteristics of acute geriatric unit
The studies reviewed provide limited information about the characteristics and form of operation of the conventional hospital units. This is important because the effect of acute geriatric units is measured by comparison with these units and could vary locally depending on the characteristics of conventional hospital units. Although the acute geriatric units in this review all included therapists as part of the normal working team (table), in general they did not have more staff than the conventional units, so that the differences between them seem to centre on specialisation and organisation of work. The distinctive feature of acute geriatric units is the comprehensive geriatric assessment and care focusing on patients’ needs, interdisciplinary work carried out by a core team of professionals (geriatrician, nursing staff trained in geriatrics, therapists, and social worker), and early planning of discharge. Other studies have evaluated partial aspects of this specialised care, such as early discharge planning or physiotherapy alone,10 11 without finding conclusive results, indicating that the benefit may derive from a combination of these interventions.2 Specialisation in the care of elderly people and formal interdisciplinary meetings (ranging from once a week in three studies to more than once a week in five studies) may contribute to the benefits of care in acute geriatric units, as has been shown in patients with stroke or hip fracture.21 22 Another aspect of acute geriatric units that might contribute to their effectiveness, compared with the lack of benefits from geriatric consultation teams, is direct responsibility for the patient, which ensures compliance with diagnostic and therapeutic recommendations and the implementation of the care plan.2 w29
In general the working method of the acute geriatric unit is similar to that of the geriatric evaluation and management unit, although more intensive. These two units complement each other in providing care; in some places, such as the United Kingdom, services may even be found where care in the acute hospital phase is complemented by subsequent care in the same unit to promote functional recovery and return home.23 The benefit of care in the subacute phase is better established, however, since geriatric evaluation and management units are the units most often studied in evaluating the impact of comprehensive geriatric assessment in hospital.2 8 Separate analysis of intervention in the acute hospital phase makes it possible to assess the impact of early specialised intervention in older people. The incidence of functional decline is highest in this early phase,14 24 which increases the risk of admission to a nursing home and death.25
Patients and case mix
The operational definition of acute geriatric unit used in this review was inclusive, allowing information to be combined across healthcare systems in different parts of the world. This serves to increase generalisability of results while retaining internal validity, because meta-analytic techniques ensure that the data for each acute geriatric unit are compared only with those of the standard care group in each trial. A potential drawback of combining data across healthcare systems is that our results might not apply to those systems where standards of care had evolved substantially from those prevailing when trials in this review were done.
The operational definition of acute geriatric unit also allowed for variation in the case mix between units, resulting from the existence of other specialised units, mainly intensive care units and coronary units, which attend to patients who would otherwise be cared for in acute geriatric units or transferred to other hospitals. In fact, in three of the randomised trials in this review, the hospitals had specialised units distinct from acute geriatric unitsw3 w5 w6; also certain variation between studies was seen in the diagnostic groups at admission (table). The influence of the case mix on the effectiveness of acute geriatric units should be a priority for future research.
The randomised studies in our review selected patients based on their age (generally ≥70 years). It has been suggested that those patients who will benefit most from acute geriatric units are the frailest elderly, regardless of the condition leading to admission.2 3 Our analysis did not allow us to draw such conclusions, although in most studies evaluated the mean age of the intervention and control groups exceeded 80 years. Four studies reported baseline dependency in at least one basic activity of daily living, which ranged between 40% and 60%.w3 w5 w6 w10 Advanced age and dependence in basic activities of daily living are independently associated with a higher risk of adverse events during hospital stay and of greater functional decline at discharge.19 24 25 However, only two studies evaluated the incidence of functional decline in people older and younger than 80 years, and in those who were independent or with some dependence in basic activities of daily living. In both studies the benefit of the intervention was observed in all patient subgroups.w3 w10
Limitations of the study
This review has some limitations. The number of randomised trials included is small, and the findings of this study might reflect usual clinical practice until 2000 (date of the most recent randomised study in this review). Thus the effect of acute geriatric units compared with conventional hospital units may have changed, as occurred when the results of the first clinical trials of geriatric evaluation and management units were compared with later ones.w38 However, more recent controlled studiesw9 w10 w12 suggest that the differences between acute geriatric units and conventional units may still remain. It could be argued that the lack of randomised controlled trials since 2000 is due to acute geriatric units having become the norm for care, so that there are presently no standard hospital care units with which they can be compared. We do not believe this is the case, however, because acute geriatric units are far from widespread in many settings and countries,13 26 27 28 29 and recent research agendas have explicitly recommended to test the effectiveness of this type of care.30 In our view the theoretical and practical difficulties of doing these trials might justify the paucity of research in this field. Finally, the studies evaluated do not provide data on the components of the intervention responsible for the benefits observed, nor do they permit us to draw firm conclusions on the effect of acute geriatric units on other relevant outcomes in the medium and long term, except for returning home to live.
Conclusion
In conclusion, acute geriatric units reduce functional decline at discharge and increase the probability of living at home at discharge and at three months after discharge without increasing case fatality or the costs of hospital care. Research should focus on the impact of acute geriatric units on functional decline in the medium term and should try to identify the specific activities associated with this effect. The methodological quality of investigations should also be improved by giving priority to randomised studies, and efficiency should be evaluated not just by carrying out cost analysis but also by calculating cost effectiveness ratios. Finally, larger sample sizes may be needed to evaluate the impact of acute geriatric units on case fatality.
What is already known on this topic
The effect of geriatric assessment has been evaluated in hospital and community settings
In older people admitted to hospital with acute disorders, the intervention of consultation teams has not shown clinical or administrative benefits
What this study adds
Care of older people with acute disorders in acute geriatric units reduces the risk of functional decline at discharge and increases the probability of returning home
This benefit is not accompanied by an increase in case fatality, readmissions, or hospital costs
We thank Mercedes Corrales for her help with the literature search.
Contributors: JJB and FRA drafted the manuscript. JJB, FMS, and JLA contributed to the selection of studies and data extraction. All authors contributed to the study design, data analysis, and interpretation of results, and reviewed the manuscript for important intellectual content and approved the final version. JJB is a guarantor.
Funding: This study was partially funded by grant No FIS PI05/90212 and research on fragility and the elderly (RETICEF) grant No RD06/0013, Instituto de Salud Carlos III, Ministry of Health and Consumer Affairs.
Competing interests: None declared.
Ethical approval: Not required.
Cite this as: BMJ 2009;338:b50
References
- 1.Calkins E, Naughton BJ. Care of older people in the hospital. In: Calkins E, Boult C, Wagner EH, Pacala JT, eds. New ways to care for older people. Building systems based on evidence. New York: Springer, 1998:99-111.
- 2.Ellis G, Langhorne P. Comprehensive geriatric assessment for older hospital patients. Br Med Bull 2005;71:45-9. [DOI] [PubMed] [Google Scholar]
- 3.Parker SG, Fadayevatan R, Lee SD. Acute hospital care for frail older people. Age Ageing 2006;35:551-2. [DOI] [PubMed] [Google Scholar]
- 4.Palmer RM, Counsell SR, Landefeld SC. Acute care for elders units. Practical considerations for optimizing health outcomes. Dis Manage Health Outcomes 2003;11:507-17. [Google Scholar]
- 5.Gray L. Geriatric consultation: is there a future? Age Ageing 2007;36:1-2. [DOI] [PubMed] [Google Scholar]
- 6.Shepperd S, Iliffe S. Hospital at home versus in-patient hospital care. Cochrane Database Syst Rev 2005;(3):CD000356. [DOI] [PubMed] [Google Scholar]
- 7.Stuck AE, Siu AL, Wielad GD, Adams J, Rubenstein L. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet 1993;342:1032-6. [DOI] [PubMed] [Google Scholar]
- 8.Parker G, Bhakta P, Katbamna S, Lovett C, Paisley S, Parker S, et al. Best place of care for older people after acute and during subacute illness: a systematic review. J Health Serv Res Policy 2000;5:176-89. [DOI] [PubMed] [Google Scholar]
- 9.Day P, Rasmussen P. What is the evidence for the effectiveness of specialist geriatric services in acute, post-acute and sub-acute settings? A critical appraisal of the literature. NZHTA Report 2004;7(3).
- 10.Shepperd S, Parkes J, McClaren J, Philips C. Discharge planning from hospital to home. Cochrane Database Syst Rev 2004;(1):CD000313. [DOI] [PubMed] [Google Scholar]
- 11.De Morton NA, Keating JL, Jeffs K. Exercise for acutely hospitalised older medical patients. Cochrane Database Syst Rev 2007;(1):CD005955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.González-Montalvo JI, Baztán Cortés JJ, Alarcón Alarcón T, Bárcena Alvarez A. Rentabilidad de las unidades geriátricas de agudos. Revisión sistemática. Rev Esp Geriatr Gerontol 2007;42:240-50. [Google Scholar]
- 13.Jayadevappa R, Bloom BS, Raziano DB, Lavizzo-Mourey R. Dissemination and characteristics of acute care for elders (ACE) units in the United States. Int J Technol Assess Health Care 2003;19:220-7. [DOI] [PubMed] [Google Scholar]
- 14.Sager MA, Franke T, Inouye SK, Landefeld S, Morgan TM, Rudberg MA, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med 1996;156:645-52. [PubMed] [Google Scholar]
- 15.Jadad A, Moore RA, Carroll D, Jenkinson C, Reynolds JM, Gavaghan DJ, et al. Assessing the quality of reports on randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [DOI] [PubMed] [Google Scholar]
- 16.Van Haastregt JCM, Diederiks JPM, van Rossum E, de Witte LP, Crebolder HFJM. Effects of preventive home visits to elderly people living in the community: systematic review. BMJ 2000;320:754-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altman DG. Confidence intervals. In: Sackett DL, Straus SE, Richardson WS, Rosenberg W, Haynes RB, eds. Evidence-based medicine, 2nd ed. Toronto: Harcourt, 2000:211-20.
- 19.Reuben DB. Making hospitals better places for sick older persons. J Am Geriatr Soc 200;48:1728-9. [DOI] [PubMed]
- 20.Salkeld G, Cameron ID, Cumming RG, Easter S, Seymour J, Kurrle SE, et al. Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ 2000;320:241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stroke Unit Trialist’ Collaboration. Collaborative systematic review of the randomised of organised inpatients (stroke unit) care after stroke. BMJ 1997;314:1151-9. [PMC free article] [PubMed] [Google Scholar]
- 22.Cameron I, Crotty M, Currie C, Finnegan T, Gillespie L, Handoll H, et al. Geriatric rehabilitation following fractures in older people: a systematic review. Health Technol Assess 2000;4(2):1-83. [PubMed] [Google Scholar]
- 23.Grimley Evans J. Geriatric medicine: a brief history. BMJ 1997;315:556-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 2003;51:451-8. [DOI] [PubMed] [Google Scholar]
- 25.Covinsky KE, Justice AC, Rosenthal GE, Palmer RM, Landefeld CS. Measuring prognosis and case mix in hospitalized elders. The importance of functional status. J Gen Intern Med 1997;12:203-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernabei R, Landi F, Zuccala G. Health care for older persons in Italy. Aging Clin Exp Res 2002;14:247-51. [DOI] [PubMed] [Google Scholar]
- 27.Gómez-Pavón J, Ruipérez-Cantera I, Rodríguez-Valcarce A, Rodríguez-Solis J, González-Guerrero JL, Maturana Navarrete N. Level of appropriateness of geriatric resources in general hospitals in Spain: period 2003 to 2005. Rev Esp Geriatr Gerontol 2006;41:77-80. [Google Scholar]
- 28.Rockwood K. Commentary: what does an ACE unit trump. Can J Geriatr 2006;9:102. [Google Scholar]
- 29.Marin PP. Health policies for older adults: thoughts for action. Rev Med Chil 2007;135:392-8. [DOI] [PubMed] [Google Scholar]
- 30.Norris SL, High K, Gill TM, Hennessy S, Kutner JS, Reuben DR, et al. Health care for older Americans with multiple chronic conditions: a research agenda. J Am Geriatr Soc 2008;56:149-59. [DOI] [PubMed] [Google Scholar]