Abstract
Purpose
To improve the efficacy and reduce the gastrointestinal toxicity of the cancer prodrug, CPT-11, we have developed immunoconjugates of its active form, SN-38, and an anti-CEACAM5 antibody for targeted chemotherapy.
Experimental Design
SN-38 conjugates of the anti-CEACAM5 mAb, labetuzumab (hMN-14), varying in the nature of the cross-linker attachment at the drug’s 20-hydroxyl position, were evaluated in vitro, in metastatic and/or subcutaneous (sc) human colonic and pancreatic cancer xenografts in nude mice using appropriate controls, and in a CEACAM5-negative tumor model.
Results
A pilot study in a sc LS174T model of human colonic carcinoma established the relative effectiveness of different conjugates. In the lung metastatic model of GW-39 human colonic carcinoma in nude mice, therapy with two specific labetuzumab-SN-38 conjugates, using 0.25 mg SN-38 equivalent/kg, q4d×8, significantly extended median survival time (MST) versus controls (P <0.002). In an expanded evaluation in the sc LS174T xenograft model, specific SN-38 conjugates produced significant tumor growth control and increases in MST versus other controls, including CPT-11 at a 33-fold greater cumulative dose (P <0.01). An improvement was also observed in the therapy of a sc human pancreatic tumor xenograft. In a CEACAM5-negative systemic lymphoma xenograft, one labetuzumab-SN-38 conjugate examined was ineffective, while the conjugate specific for the tumor model produced 100% survival.
Conclusions
The promising labetuzumab-SN-38 conjugates developed showed selective therapeutic efficacy in human tumor models at nontoxic doses that were a fraction of the CPT-11 doses used.
Keywords: CEA, CEACAM5, labetuzumab, SN-38, immunoconjugate therapy
Introduction
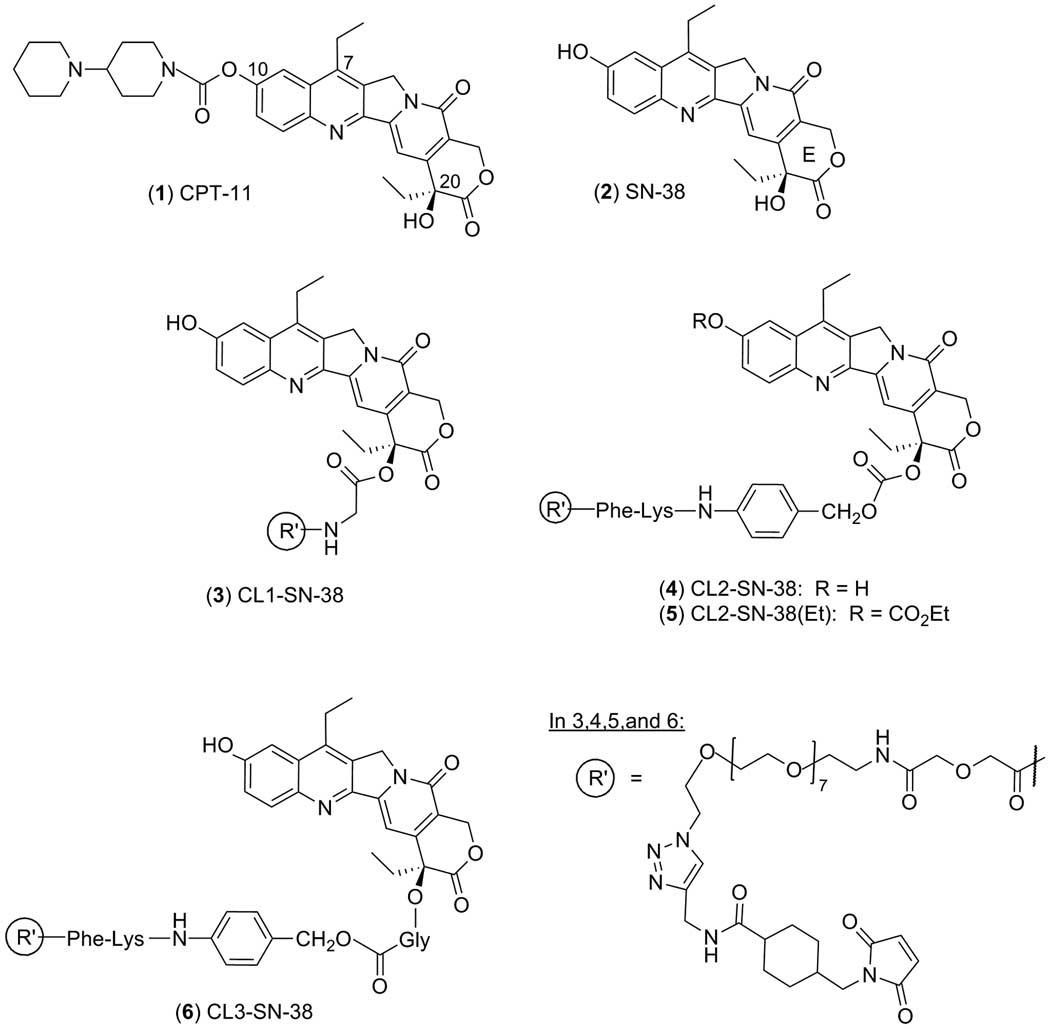
CPT-11 (irinotecan) is a water-soluble prodrug in clinical use for the treatment of metastatic colon cancer, and is also clinically active in lung, cervical, and ovarian cancers (1, 2). It is additionally used in combination therapies with other cancer drugs and biological agents. CPT-11 is converted by human carboxylesterase in vivo to its active form, SN-38, which is more potent by 2–3 orders of magnitude (3). Both CPT-11 and SN-38 belong to the camptothecin (CPT) group of antitumor compounds that inhibit topoisomerase I by stabilizing the DNA-topo I complex (4–6). Structures are shown in Figure 1.
Figure 1.
Structures of CPT-11, SN-38, and bifunctional SN-38 substrates CL1-SN-38, CL2-SN-38, CL2-SN-38(Et) and CL3-SN-38. The numbering is shown in the CPT-11 structure, and the ‘E’ ring is indicated in the SN-38 structure.
The in vivo conversion to the active drug is not efficient (7). Further, SN-38 is converted to its glucuronide, SN-38G, in a detoxification mechanism, and is reconverted back to the active drug by intestinal glucuronidase, thereby causing severe delayed diarrhea (8). In addition, CPT-11 and SN-38 undergo lactone (E-ring)-opening in vivo, with the open carboxylate form further stabilized by complexation with human serum albumin. Since the carboxylate form has only 10% of the drug activity as the intact lactone form, this in vivo lactone opening diminishes drug potency (9, 10). CPT-11 also undergoes oxidative transformations mediated by cytochrome P450, and the metabolites are poorer substrates than CPT-11 itself for carboxylesterase-mediated conversion to SN-38 (11). Many of these processes are also patient-dependent. Pharmacokinetics and complex in vivo metabolism of CPT-11 and SN-38 cause reduced bioavailability of the active drug and also result in unpredictable toxicity. Several approaches have been reported making use of polymers, polymeric micelles, or liposomes as carriers of SN-38 and other camptothecin derivatives for protracted release of the active drug or for passive targeting to tumor sites (12–17).
The goal of this work has been to design a monoclonal antibody (mAb)-SN-38 approach to increase the drug’s efficacy, and reduce its toxicity, in cancer therapy. In this article, we describe the application of this concept to the therapy of metastatic and/or subcutaneous (sc) xenografts of human colonic and pancreatic carcinomas in nude mice. The humanized antibody in these studies, labetuzumab (hMN-14; (18)), targets carcinoembryonic antigen cell adhesion molecule 5, CEACAM5 (CEA, CD66e), which is expressed on a majority of solid tumors. It has been examined in a number of cancer therapy trials (19, 20). The labetuzumab-SN-38 immunoconjugates thus constitute clinically-validated mAb and drug components. The synthesis of relevant bifunctional SN-38 substrates, as well as the procedure for antibody conjugation, has been published recently (21).
We further describe comparative in vivo antitumor effects of the labetuzumab conjugates derived from four bifunctional SN-38 derivatives (CL1-SN-38, CL2-SN-38, CL2-SN-38(Et), and CL3-SN-38), which identified the most promising conjugates. Further, we show that the specific conjugates produce therapeutic efficacies in human colonic and pancreatic carcinoma xenografts in nude mice, at nontoxic doses, which are a fraction of the CPT-11 doses used. Finally, one labetuzumab-SN-38 conjugate is shown to be ineffective in a CEACAM5-negative systemic human lymphoma model in which the targeting mAb-SN-38 conjugate produces cures.
Materials and Methods
Conjugates were prepared as described recently (21). The mean SN-38/mAb molar substitutions were in the 6–7 range. CPT-11 was purchased from Hospira, Inc (Lake Forest, IL) as a sterile solution in saline. Cell lines were obtained from the American Type Culture Collection (Manassas, VA) and maintained in RPMI 1640 media supplemented with FBS (10%) and L-glutamine, MEM non-essential amino acids, and sodium pyruvate. The cells were routinely tested for mycoplasma contamination using the Myco Tect™ Kit (Gibco, Invitrogen Corp., Carlsbad, CA). Seven-week old nude mice and SCID mice were obtained from Taconic Farms (Gemantown, NY), and used after 1 week of quarantine.
In vitro studies
Stabilities, cell-binding assays, and cytotoxicity assays have been described elsewhere (21). Determinations of conjugate stability in mouse serum were performed by the method we reported previously (21).
In vivo studies
General
All animal experiments were performed under approved IACUC protocols. Eight-week-old female athymic nude mice and female CB17 SCID mice were used for in vivo therapy studies. In the subcutaneous (sc) LS174T model, mice were injected with 1×107 LS174T human colonic adenocarcinoma cells as a 0.2 mL suspension in RPMI media. In the lung metastatic model of colon carcinoma, animals were injected intravenously (i.v.) with 30 µL of a 10% (w/v) tumor suspension of the GW-39 human adenocarcinoma (22), and the treatment was started 14 days later. In therapy experiments, conjugates and saline were administered intraperitoneally (i.p.), except that CPT-11 was administered i.v. In the CaPan 1 human pancreatic carcinoma model, 0.2 mL of a 20% w/v tumor suspension in Hank’s balanced salt solution was injected sc in the left or right flanks of nude mice, and the study was started once the tumors reached approximately 0.1–0.2 cm3 in size. Animals were monitored daily for signs of distress (e.g., labored breathing, moribund), weighed weekly, and humanely sacrificed when moribund, body weight loss was ≥20%, tumor volumes reached 2 cm3, or at study termination. Tumor size was monitored by weekly caliper measurements of length and width of the tumor. Tumor volume (TV) was calculated as (L×W2)/2.
Therapy studies
All doses are expressed in terms of drug equivalents. A dose of 0.20–0.23 mg of conjugated SN-38/kg, for a drug/mAb substitution in the range of 6–7, corresponds to the protein dose of 12.5 mg/kg.
A pilot therapy experiment in the LS174T model (n = 5) was conducted to compare the therapeutic efficacies of the labetuzumab conjugates of CL1-SN-38, CL2-SN-38, and CL3-SN-38, and to make an initial selection. The conjugates were given at 0.18–0.23 mg of SN-38 equivalent (eq.)/kg at a schedule of q4d×4.
For therapeutic evaluation in the lung metastatic model of GW-39 human colon carcinoma, groups of animals (n = 7–10) were administered 0.22–0.25 mg SN-38 eq./kg of the specific labetuzumab-CL1-SN-38 and labetuzumab-CL2-SN-38 conjugates, non-targeting immunoconjugates of anti-CD22 mAb, hLL2 (hLL2-CL1-SN-38, hLL2-CL2-SN-38), or equivalent amounts of naked labetuzumab plus free SN-38 as in the specific conjugates, at a dose schedule of q4d×8. Treatments with lower doses of specific conjugates, using 0.045 mg and 0.1 mg of SN-38 eq./kg, q4d×8, were also conducted. There was also a saline control group.
In an expanded therapy experiment in the LS174T model, therapy was started 1 day after tumor cell injection. Groups of mice (n = 8) were treated with the specific conjugates, labetuzumab-CL2-SN-38 or labetuzumab-CL2-SN-38(Et), at either 0.43 mg or 0.09 mg SN-38 eq./kg at a schedule of q4d×8; respective control hLL2 conjugates at 0.43 mg SN-38 eq./kg, qd4×8; mixture of labetuzumab and SN-38 with protein and drug doses corresponding to the higher dose of the specific conjugate, qd4×8; maximum-tolerated-dose (MTD) of CPT-11 at 40 mg/kg (23 mg SN-38 eq./kg), q2d×5; CPT-11 at 30 mg/kg (17.25 mg SN-38 equiv/kg), q4d×8; or saline. Therapy was also evaluated 9 days after tumor cell injection, when tumors reached approximately 0.2 cm3 in size (n = 4–8). In this, specific labetuzumab or control hLL2 conjugates of CL2-SN-38 or CL2-SN-38(Et) or CPT-11 were given at 0.19 mg of SN-38 eq./kg, at two courses of q1d×5, with 2 days of rest between courses. CPT-11 was also administered in one group of animals at the same schedule, but at a 10× higher SN-38 equivalent dose. There was a saline control group.
In the CaPan 1 study, tumor-bearing nude mice were treated with labetuzumab-CL2-SN-38 at 0.375 mg SN-38 equiv/kg, q4d×8. Control groups were administered, at the same dose schedule, saline or a mixture of labetuzumab and SN-38. In the latter, protein and drug doses matched that in the conjugate.
For evaluation in a CEACAM5-negative tumor model, groups of SCID mice (n = 6) were injected i.v. with 5×106 NAMALWA human lymphoma cells, and the therapy was started the following day. The test articles consisted of the specific humanized anti-CD74 mAb, hLL1 (milatuzumab; Immunomedics, Inc.); the conjugate, hLL1-CL2-SN-38; CPT-11; labetuzumab-CL2-SN-38; and saline. The immunoconjugates were adminstered at 0.35–0.44 mg of SN-38 eq./kg, q4d×8, and CPT-11 was given at 6.5 mg/kg (3.76 mg SN-38 eq./kg), q4d×8. Unmodified hLL1 was given at 25 mg/kg, q4d×8, to match the protein dose of the conjugate. The end point was the onset of hind-leg paralysis.
Statistical considerations
Analyses for the tumor growth data were based on area under the curve (AUC) and survival time. Profiles of individual tumor growth were obtained through linear curve modeling. An f-test was employed to determine equality of variance between groups prior to statistical analysis of growth curves. A one-tailed t-test was used to assess statistical significance between any individual treatment group and saline group. Two-tailed t-test analysis was used for comparisons between the treatment groups. As a consequence of incompleteness of the growth curves due to deaths, statistical comparisons of AUC were only performed up to the time at which the first animal within a group was sacrificed. Survival studies were analyzed using Kaplan-Meier plots (log-rank analysis), using Prism® software package (GraphPad Software, Inc., San Diego, CA). The animals were monitored for up to 2–4 times the median survival duration of untreated controls.
Results
Bifunctional SN-38 derivatives
The structures of four different bifunctional SN-38 derivatives, 3–6, with maleimide as the antibody-conjugating group, are shown in Figure 1. Three of these (CL2, CL2(Et) and CL3) share common features, namely: (i) a defined polyethylene glycol (PEG) moiety introduced for water solubility, (ii) the presence of a triazoline group resulting from an azide-acetylene cycloaddition strategy in the design, (iii) the presence of a cathepsin-B-cleavable dipeptide, Phe-Lys, together with a collapsible p-aminobenzyl alcohol (PABOH) moiety, and (iv) the attachment to 20-hydroxyl of SN-38 via a carbonate bond (CL2, CL2(Et)) or a glycinate bond (CL3). CL1 is similar to CL3, except for the absence of the Phe-Lys peptide and the PABOH moiety. The common cleavable bond in these is the carbonate or the ester bond at the 20 position, with additional cleavable peptide incorporated in three of the substrates.
Conjugates
Conjugates were prepared by first reducing the antibodies to generate thiol groups, followed by coupling to maleimide-appended SN-38 derivatives (21). Data relevant to the conjugates are given in Table 1. In vitro bindings in 2 colon carcinoma cell lines show that the Kd for the conjugates are similar to that of unmodified labetuzumab. The IC50 values for the conjugates, in the LoVo colon cancer cell line, were 2–4-fold higher than for SN-38. The table also details the SE-HPLC retention times. Interestingly, the labetuzumab-CL2-SN-38(Et) conjugate eluted >1 min faster on SE-HPLC, and its retention time suggested that it was possibly a non-covalent dimer. This form of the conjugate also exhibited an enhanced stability in vitro (Table 1).
Table 1.
Size-exclusion HPLC retention times, antigen-bindings, cytotoxicities, and in vitro stabilities of the immunoconjugates.
| Substrate | SE HPLC (ret. time in min) |
Cell-binding: Kd (nM) |
Cytotoxicity (in LoVo) IC50 (nM) |
in vitro stability at 37 °C (half-life) |
|||
|---|---|---|---|---|---|---|---|
| LS174T | LoVo | PBS | Human serum |
Mouse serum |
|||
| labetuzumab | 9.46 | 0.67–2.07* | 0.90–2.07* | n/a | n/a | n/a | n/a |
| labetuzumab -CL1-SN-38 | 9.40 | n/d | 1.40† | 4.1 | 8.6 h | 10.8 h | n/d |
| labetuzumab -CL2-SN-38 | 8.91 | 0.65–2.49* | 0.92–2.17* | 5.3 | 30.1 h | 36.2 h | 25.9 h |
| labetuzumab -CL2-SN 38(Et) | 8.44 | 0.88–3.10* | 1.44–2.95* | 5.2 | 98.4 h | 65.9 h | 41.1 h |
| labetuzumab-CL3-SN-38 | 9.21 | n/d | 1.50† | 9.5 | 48.8 h | n/d | n/d |
| SN-38 | n/a | n/a | n/a | 2.4 –3.2 | n/a | n/a | n/a |
Range in multiple experiments;
single experiment;
Abbreviations: n/a: not applicable; n/d: not determined.
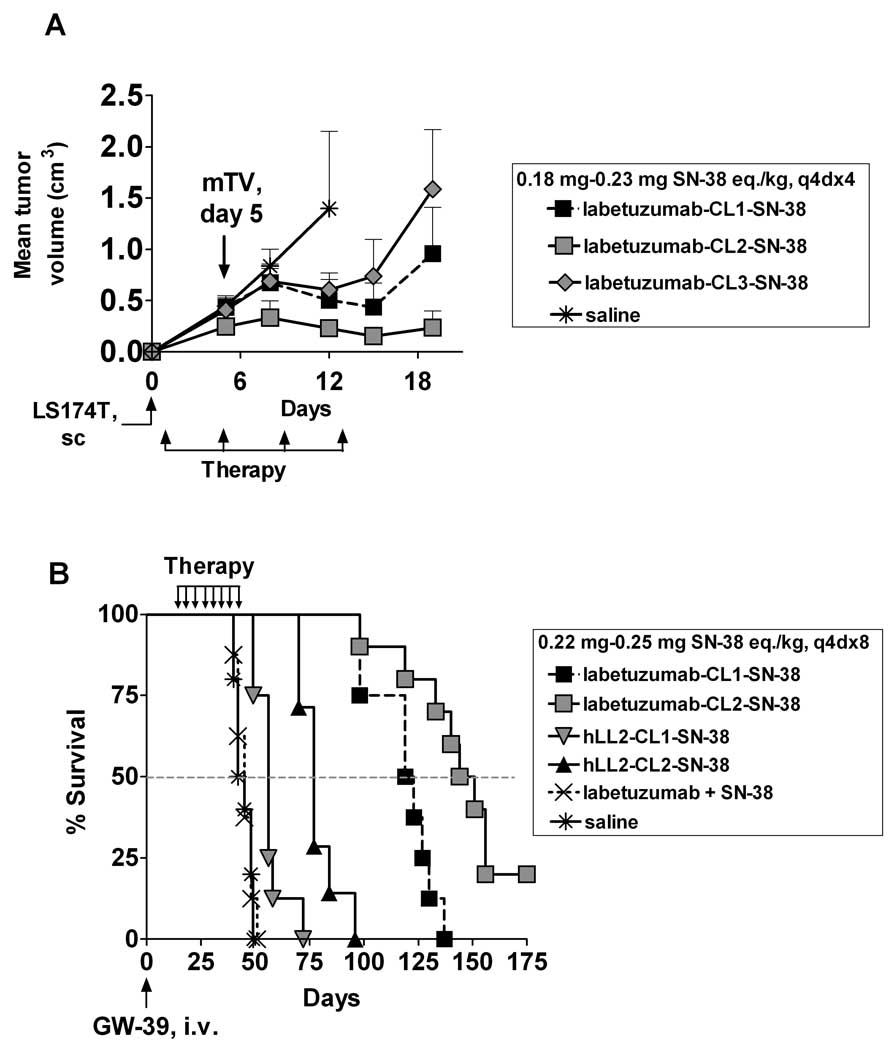
Pilot experiment in sc LS174T model
In an initial exploratory therapy study, labetuzumab conjugates of CL1-SN-38, CL2-SN-38, and CL3-SN-38 were compared in the sc LS174T human tumor xenograft in nude mice (Fig. 2A) to make a preliminary selection. In this aggressive model, all untreated mice succumbed by day 21. On day 19, the mean TV (mTV) of animals receiving labetuzumab-SN-38 conjugates containing CL1, CL2, and CL3 linkers were 200%, 75%, and 400%, respectively, of the corresponding mTV on day 5. Relative efficacies of the conjugates in controlling tumor growth were in the following order: labetuzumab-CL2-SN-38 > labetuzumab-CL1-SN-38 > labetuzumab-CL3-SN-38.
Figure 2.
(A) Pilot therapy in the sc LS174T model of human colon carcinoma in nude mice. One day after sc injection of LS174T cells, groups of animals (n = 5) were administered labetuzumab (hMN-14) conjugates of CL1-SN-38, CL2-SN-38, and CL3-SN-38, i.p., at 0.18–0.23 mg SN-38 eq./kg, q4d×4. Control mice were given saline. The first measurement of tumor volumes was performed on day 5. (B) Evaluation in the lung metastatic model of GW-39 human colon carcinoma in nude mice. Animals were injected intravenously with GW-39 tumor suspension, and the therapy was begun 14 days later (n = 7–10). Labetuzumab conjugates of CL1-SN-38 and CL2-SN-38 and the corresponding non-targeting anti-CD22 mAb, hLL2, conjugates were administered, i.p., at 0.22–0.25 mg SN-38 eq./kg, q4d×8. Controls included saline and a mixture of labetuzumab (12.5 mg/kg) and SN-38 (0.25 mg/kg) administered at the same dose schedule. The figure shows Kaplan-Meier survival plots for the various treatments.
Lung metastatic model of GW-39 human colon carcinoma
Therapeutic efficacies of CL1-linked and CL2-linked conjugates of specific and control mAbs, as well as other controls, were examined in a lung metastatic model of GW-39 human colon carcinoma in nude mice (Fig. 2B). Mean survival time (MST) for various treatments, together with statistical significance of differences in treatment outcomes, is given in Table 2 top panel. Specific labetuzumab conjugates of CL1-SN-38 and CL2-SN-38 at the highest doses showed a significant survival advantage versus equidoses of respective control conjugates of an anti-CD22 mAb, epratuzumab or hLL2 (Immunomedics, Inc.), hLL2-CL1-SN-38 and hLL2-CL2-SN-38, or a mixture of labetuzumab and SN-38, or saline. In addition, the specific conjugates were more efficacious than the conjugates administered at 40% and 20% of the highest doses (not shown). Lastly, labetuzumab-CL2-SN-38 was more potent than labetuzumab-CL1-SN-38.
Table 2.
Mean tumor volume and/or median survival, and statistical data, for two therapy experiments in colon carcinoma models.
| Therapy in the lung metastatic model of GW-39 human colon carcinoma in nude mice | ||||||
|---|---|---|---|---|---|---|
| Conjugates/controls | Median survival (days) |
P value (log-rank) versus | ||||
| Saline | Control hLL2 conj |
mAb+ SN-38 |
labetuzumab- CL1-SN-38 |
|||
| Specific: labetuzumab-CL1-SN-38* | 121 | <0.0001 | <0.0001 | <0.0001 | ||
| Control: hLL2-CL1-SN-38* | 56 | 0.0002 | 0.0003 | |||
| Specific: labetuzumab-CL2-SN-38* | 147.5 | <0.0001 | <0.0001 | <0.0001 | 0.002 | |
| Control: hLL2-CL2-SN-38* | 77 | <0.0001 | 0.0001 | |||
| Control: labetuzumab + SN-38† | 45 | 0.7451 | ||||
| Control: saline | 43.5 | |||||
| sc LS174T model of human colon carcinoma in nude mice: Therapy 1 day after tumor cell injection | ||||||
|
Mean Tumor volume (cm3) |
PAUC | Median Survival | ||||
| days | P value (log-rank) versus | |||||
| Conjugates/controls | Control hLL2 conj |
mAb+ SN-38 |
CPT-11, MTD |
|||
| Specific: labetuzumab -CL2-SN-38‡ | 0.095 ± 0.107, day 28 | Specific vs. control conjugates: PAUC = 0.0078 (on day 28) |
61.5 | 0.1227 | <0.0001 | <0.0001 |
| Control: hLL2-CL2-SN-38‡ | 0.727 ± 0.472, day 28 | 40.5 | 0.1434 | |||
| Specific: labetuzumab CL2-SN-38(Et) ‡ | 0.101 ± 0.147, day 46 | Specific vs. control conjugates: P AUC = 0.0014 (on day 46) |
86 | 0.0102 | <0.0001 | <0.0001 |
| Control: hLL2-CL2-SN-38 (Et) ‡ | 1.497 ± 0.731, day 46 | 51 | <0.0001 | |||
| Positive control: CPT-11, MTD†† | 1.191 ± 0.276, day 32 | Specific conjugates vs. CPT-11: P AUC = 0.0001 (on day 32) |
35 | |||
| Positive control: CPT-11** | 0.823 ± 0.527, day 42 | Specific conjugates vs. CPT-11: P AUC < 0.0493 (on day 42) |
54.5 | |||
| Control: labetuzumab + SN-38‡‡ | 1.390 ± 0.689, day 18 | Specific conjugates vs. this control: P AUC = 0.0005 (on day 18) |
19.5 | |||
| Control: saline | 0.735 ± 0.695, day 14 | Specific conjugates vs. saline control: P AUC < 0.04 (on day 14) |
21 | |||
Doses: 0.22–0.25 mg of SN-38 eq./kg, q4d×8;
0.25 mg SN-38/kg + 12.5 mg labetuzumab/kg, q4d×8;
0.43 mg SN-38 eq./kg, q4d×8;
40 mg CPT-11/kg (23 mg SN-38 eq./kg), q2d×5;
30 mg CPT-11/kg (17.25 mg SN-38 eq./kg), q4d×8;
0.43 mg SN-38/kg + 25 mg labetuzumab/kg, q4d×8.
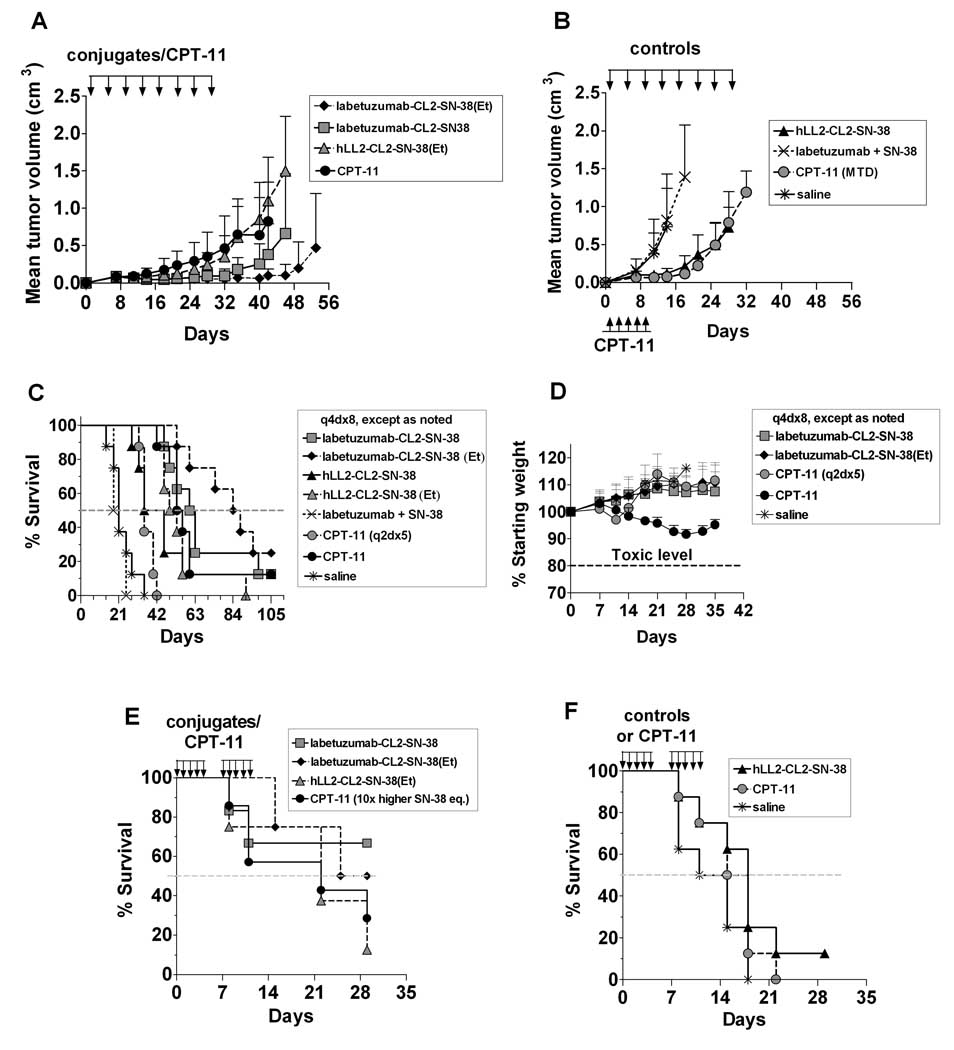
Expanded study in the sc Model of LS174T human colon carcinoma
Having established that labetuzumab-CL2-SN-38 was the best of the CL1-, CL2- and CL3-linked conjugates, it was further evaluated in the sc LS174T model using various controls. At this stage, it was discovered that a variant of CL2-SN-38, namely CL2-SN-38(Et) with an ethyl carbonate group at the 10 position of SN-38, produced a conjugate with an enhanced in vitro stability (Table 1). We therefore evaluated the labetuzumab-CL2-SN-38(Et) conjugate alongside the parental CL2-SN-38 conjugate in the sc LS174T tumor model in nude mice, 1 day after tumor cell injection in nude mice. Tumor growth control data are given in Fig. 3A and 3B, survival data are shown in Fig. 3C, and the differences among various treatments are displayed in Table 2, bottom panel. Specific labetuzumab-SN-38 conjugates were significantly better than the two CPT-11 dose schedules and the respective control hLL2-SN-38 conjugates in tumor growth inhibition. Treatments with specific conjugates were superior, in MST, to the MTD dose of CPT-11, equidoses of labetuzumab and SN-38, and untreated controls. In addition, the ‘Et’ version of the specific conjugate produced a significant survival advantage over a lower dose regimen (not shown) and the control hLL2 conjugate. In this model, there was no significant difference in the two specific conjugates in controlling tumor growth or extending survival. Figure 3D gives the weights for the treatment groups receiving the highest doses of the specific conjugates, CPT-11 administered at two different schedules, and the saline controls. Animals treated with specific conjugates continued to gain weight at a rate similar to the untreated group, while with the MTD dose of CPT-11, there was an initial loss of 3% in body weight by day 11, followed by recovery. In the CPT-11 treatment group receiving the same dose schedule as conjugates, there was a gradual weight loss from day 7 onwards, reaching as much as ~ 9 % by day 28, compared to weight gain of 7–16% in other groups. This suggested that there was some toxicity associated with the CPT-11 treatment, while the immunoconjugate therapy was essentially nontoxic.
Figure 3.
Expanded study in the sc LS174T model of human colon carcinoma in nude mice with labetuzumab-CL2-SN-38 and its longer-acting version, namely labetuzumab-CL2-SN-38(Et), with appropriate controls. (A–D) Therapy was started 1 day after sc injection of LS174T cells. Groups of animals (n = 8) were treated i.p. with specific labetuzumab or control hLL2 conjugates, each at 0.43 mg SN-38 eq./kg, q4d×8; treated i.v. with CPT-11 using a maximum-tolerated-dose schedule of 40 mg/kg (23 mg SN-38 eq./kg), q2d×5 (shaded circle, in 3B) or a lower dose of 30 mg/kg (17.25 mg SN-38 eq./kg) at the same dose schedule as for other test agents, namely q4d×8 (solid circle, in 3A); treated (i.p.) with a mixture of labetuzumab at 25 mg/kg and SN-38 at 0.43 mg/kg, q4d×8; and saline, q4d×8. Mean tumor volume vs. time plots are shown in two separate panels, A & B, for clarity; Kaplan-Meier survival plots for all the treatments are depicted in panel C; and percent weight gains in treatments with saline, specific conjugates, and CPT-11 are indicated in panel D. Panels E & F pertain to Kaplan-Meier survival plots in a 2nd therapy experiment that was started 9 days after LS174T tumor cell injection. Groups of animals (n = 4–7) were treated at a schedule of (q1d×5)×2, with 2 days of rest between courses, with specific labetuzumab conjugates of CL2-SN-38 and CL2-SN-38(Et), and the corresponding nontargeting conjugates of hLL2 mAb, each administered at 0.19 mg SN-38 eq./kg; CPT-11 given at 0.33 mg/kg (0.19 mg SN-38 eq./kg; shaded circle) or at a 10-fold higher dose of 3.25 mg/kg (1.9 mg SN-38 eq./kg; solid circle); and saline. The plots are given in two separate panels (E & F) for clarity.
Therapy was also examined 9 days after sc tumor cell injection, when the mean tumor volumes reached 0.2 cm3. MST data are given in Fig. 3E and 3F. MST for the untreated control was 13 days. Specific conjugates labetuzumab-CL2-SN-38 and labetuzumab-CL2-SN-38(Et) significantly extended survival versus untreated or equidose CPT-11 treatment (P<0.05). In this established model, tumors grew too rapidly to be contained by any therapeutic intervention.
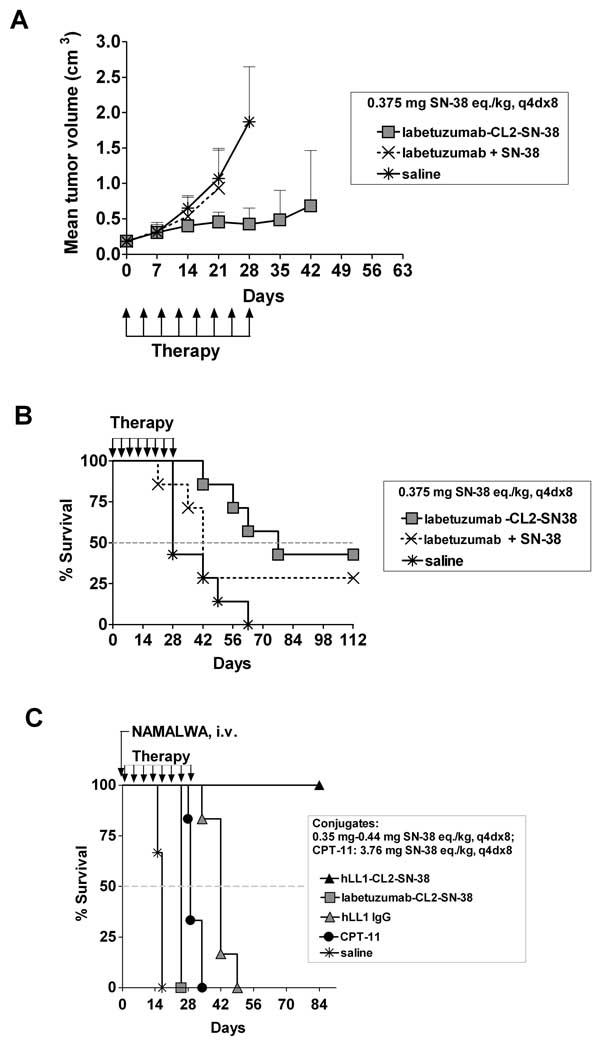
CaPan 1 pancreatic carcinoma model
CaPan 1 pancreatic cancer cell line is positive for CEACAM5. Therefore, the labetuzumab-CL2-SN-38 conjugate was evaluated in the therapy of sc CaPan 1 human tumor xenografts in nude mice. Data are shown in Figure 4A and 4B. On the last days measurable (before any animal was sacrificed), the mTVs of the various groups were as follows: 0.684 ± 0.779 cm3 on day 42 for the group receiving labetuzumab-CL2-SN-38; 0.935 ± 0.559 cm3 on day 21 for the group treated with a mixture of labetuzumab and SN-38 containing the same protein and drug doses as in conjugate; and 1.871 ± 0.777 cm3 on day 28 in the untreated group. MSTs in these treatments were 77, 42, and 28 days, respectively. Conjugated SN-38 was significantly better than untreated controls in extending survival (P = 0.0045).
Figure 4.
Therapy of the sc CaPan 1 human pancreatic adenocarcinoma xenograft in nude mice (A&B) and evaluation in a CEACAM5-negative systemic lymphoma model in SCID mice (C). In the sc CaPan 1 model, groups of mice (n = 7) were administered the specific labetuzumab-CL2-SN-38 conjugate at 0.375 mg SN-38 eq./kg, a noncovalent mixture of labetuzumab (25 mg/kg, same as in the conjugate) and SN-38 (0.375 mg/kg, same as in the conjugate), or saline, each at a dose schedule of q4d×8. (A) Plot of mean tumor volume vs. time, and (B) Kaplan-Meier survival plots. (C) Groups of SCID mice (n = 6) were injected i.v. with NAMALWA lymphoma cells, and the treatment was started one day later with the targeting anti-CD74 mAb, hLL1, the targeting hLL1-CL2-SN-38 conjugate, non-targeting hMN-14-CL2-SN-38 conjugate, CPT-11, or saline. The conjugates were administered at 0.35–0.44 mg SN-38 eq./kg, q4d×8; CPT-11 at 3.76 mg SN-38 eq./kg, q4d×8; hLL1 at the equi-protein dose of 25 mg/kg, q4d×8; and saline, q4d×8. Figure shows the Kaplan-Meier survival plots.
Treatment in a CEACAM5-negative systemic lymphoma model in SCID mice
In SCID mice bearing systemic human lymphoma or multiple myeloma xenografts, a doxorubicin conjugate of an anti-CD74 mAb, hLL1(milatuzumab), had been shown previously to produce excellent cures at low doses of the conjugate (23, 24). Figure 4C shows Kaplan-Meier survival plots generated in the therapy of SCID mice with systemic NAMALWA lymphoma. The specific mAb, hLL1, and its conjugate, hLL1-CL2-SN-38, were superior to saline, hMN-14-CL2-SN-38, and CPT-11 in extending survival (P <0.0024), while the specific hLL1-SN-38 conjugate was more potent, with 100% cure rate, than the equivalent protein dose of naked hLL1 (P = 0.0006).
Discussion
With a view to enhancing the bioavailabilty of the potent topoisomerase I inhibitor, SN-38, in cancer therapy, we have designed and evaluated a number of antibody-SN-38 immunoconjugates for targeting xenograft models of human colonic and pancreatic carcinomas expressing the CEACAM5 antigen. Conjugates containing a carbonate bonding to SN-38, as well as a cathepsin-B-cleavable peptide in the linker, were identified as the best, based on in vivo studies. These products produced significant and selective therapeutic effects in metastatic and sc human colonic carcinoma xenografts in nude mice, compared to non-targeting control conjugates as well as CPT-11 used as a positive control, at doses that were nontoxic and a fraction of the CPT-11 doses. Antitumor effects were also observed in a human pancreatic tumor model.
A majority of carcinomas, encompassing gastrointestinal, respiratory, genitourinary, and breast cancers, overexpress the tumor antigen, CEACAM5 (25−29). Therefore, this antigen has been a therapeutic target for radiolabeled and drug- or toxin-conjugated anti-CEACAM5 mAbs. Labetuzumab, or the humanized MN-14 antibody, specifically targets the A3B3 epitope of CEACAM5, which is not shared with other members of the CEACAM family (30). The role of CEACAM5 in tumor biology and tumor metastasis has been described (31). Moreover, the role of the anti-CEACAM5 mAb, labetuzumab, in inhibiting cancer metastases when CEACAM5 expression is upregulated, and its role in augmenting the antitumor effects of chemotherapy in the treatment of human tumor xenograft models, have been described (31, 32). Radioiodinated labetuzumab has been extensively investigated clinically in an adjuvant setting of colorectal cancer post salvage resection of liver metastases, with considerable improvement in survival reported (20). CEACAM5 is traditionally considered non-internalizing, but a number of reports show that slow internalization of CEACAM5 and, with it, the targeted antibody, occurs due to membrane turnover (33−35). Internalization and intracellular processing of labetuzumab on two colonic cancer cell lines in vitro also has been described (36).
We originally examined the conjugates of a bifunctional derivative, designated CL-SN-38, but its continued exploration was hampered by poor yields in synthetic chemistry and poor protein recoveries in conjugate preparations, notwithstanding the therapeutic potential (37). Subsequently, the conjugates were redesigned (21). The therapeutic efficacy of these improved SN-38 conjugates is the subject of this article.
The conjugates maintained cell-binding to specific cell lines, and also exhibited potent cytotoxicities. The somewhat faster elution of labetuzumab-CL2-SN-38(Et) compared to the native mAb appeared to suggest a dimeric form of the conjugate. Perhaps, in the putative non-covalent dimeric form, the carbonate group of the derivatized SN-38 is more shielded from hydrolytic cleavage, and perhaps this accounts for its increased in vitro stability.
In a pilot experiment in the aggressive sc LS174T tumor model, a preliminary selection was made among the labetuzumab conjugates of CL1-SN-38, CL2-SN-38, and CL3-SN-38. The CL3-linked conjugate was ruled out from further consideration. The in vivo efficacy data correlated with the relative cytotoxicities in vitro. Both CL1- and CL3-linked conjugates have the ester attachment to SN-38, but the latter differs in the structural features around the ester region and also exhibits ~ 4-fold increased stability in vitro compared to the CL1-linked conjugate. Yet, the CL3 conjugate appears to be less efficacious than the CL1 conjugate. In the CL3 conjugate, the drug has the opportunity to be released as the glycinate ester intracellularly, if cleavage by cathepsin-B precedes ester cleavage. The glycinate ester, in turn, has the potential to abrogate drug activity by intramolecular lactone ring opening, in view of the favorable 6-membered geometry. Such a situation does not exist with the CL1-linked conjugate.
The therapeutic potential of the CL1- and CL2-linked conjugates was evaluated in the lung metastatic model of human colonic carcinoma. It is particularly relevant to examine experimental therapeutics in metastatic models of human cancer since, clinically, tumors do not generally present themselves as a bulky sc mass. A lung metastatic model GW-39 human colon carcinoma in nude mice has been described (22), involving the formation of multiple tumor nodules throughout the lungs within 2 weeks of iv injection of a suspension of colonic cancer cells. Successful radioimmunotherapy of this metastatic tumor model has been also reported (22, 38). In the present study, specific labetuzumab-CL1-SN-38 and labetuzumab-CL2-SN-38 conjugates were compared with non-targeting conjugates of anti-CD22 mAb, hLL2. An equidose mixture of labetuzumab and SN-38, corresponding to the doses in the specific conjugates, lower doses of specific conjugate, and saline controls were also included in the study. The specific conjugates proved to be significantly better than all controls. Of the two specific conjugates, the CL2-linked conjugate was significantly better than the CL1-linked conjugate in extending survival, consistent with a 3-fold better stability for the CL2 versus CL1 linker in vitro (Table 1). This experiment suggested a clear choice of the conjugate, namely labetuzumab-CL2-SN-38, although the CL1-SN-38 conjugate itself was significantly better than the controls (Table 2, top panel).
In an expanded study in the sc LS174T model of human colon carcinoma, both labetuzumab-CL2-SN-38 and its longer-acting ‘Et’ version, labetuzumab-CL2-SN-38, were examined using appropriate controls including CPT-11. The study was performed in 2 formats: either as a tumor outgrowth control study in which the conjugates and the control materials were administered 1 day after tumor cell administration, or in an established model after tumor volumes reached 0.2 cm3. In the first study, CPT-11 was administered either at a dose and a dose schedule stated to be the MTD (12) or at a 25% lower dose, but with the same dose schedule as for test conjugates. In the MTD schedule of CPT-11, the cumulative SN-38 equivalent dose was 33.4× greater than that in the conjugate. The specific conjugates produced a significantly better tumor growth control versus all control agents and a significantly prolonged median survival versus most controls (Table 2, bottom panel), but there was no significant difference in the efficacy of the two specific conjugates. When the therapy was started 9 days after tumor cell injection, treatment with specific conjugates showed a survival advantage (P <0.05) versus non-treatment or treatment with an equivalent CPT-11 dose.
The advantage of the specific conjugate over the MTD dose of CPT-11 in controlling tumor outgrowth is more significant than the preclinical data suggest. This is because human carboxylesterase is inefficient in the conversion of CPT-11 to its active drug relative to carboxylesterase from animal species (7). Thus, the difference in the efficacies of the sub-MTD dose of the conjugate and the MTD dose of CPT-11 could be expected to be more pronounced in a clinical setting than in the preclinical tumor models. The MTDs of the specific conjugates have not been established yet. However, in one experiment, a bolus i.p. injection of 23.5 mg of conjugated SN-38/kg dose of labetuzumab-CL2-SN-38 in a nude mouse was nontoxic (not shown). This dose was 6.8–13.6-fold higher than the cumulative conjugated SN-38 dose administered in the two therapy experiments described above. Volume limitations precluded a further increase in the bolus dose, but multiple administrations of the conjugate at 10- and 20- fold more cumulative dose than in the therapy experiment will be undertaken to determine toxicity and the therapeutic window.
The labetuzumab-CL2-SN-38 conjugate was also explored in the therapy of sc CaPan 1 human pancreatic adenocarcinoma in nude mice. The rationale for this stems from tumor targeting by the radioiodinated murine anti-CEACAM5 antibody, 131I-MN-14, in the nude mouse model of CaPan 1 human pancreatic adenocarcinoma (39). In that study, radiolabeled MN-14 was shown to deliver a dose to tumor that was 3-fold higher than dose to blood. A much higher dose was delivered to tumor by a radioiodinated anti-mucin mAb, 131I-PAM4 (39), but the comparative study nonetheless provided the impetus to examine targeted therapy with labetuzumab-SN-38 in this tumor model, and the results showed that the labetuzumab-CL2-SN-38 conjugate was significantly better compared to saline controls in extending survival. We have also evaluated the therapeutic potential of SN-38 conjugates of the humanized anti-mucin mAb, hPAM4, and those results will be communicated elsewhere.
Specificity of efficacy was determined in a therapy experiment in the CEACAM5-negative NAMALWA human lymphoma tumor model (Fig. 4C). This systemic model was not sensitive to CPT-11 therapy, because CPT-11 was only modestly effective. Nonetheless, the SN-38 conjugate of the specific anti-CD74 mAb, hLL1 (milatuzumab), produced 100% survival, thereby underscoring the significance of targeted therapy. An equivalent dose of non-targeting labetuzumab-CL2-SN-38 was much less effective, being only slightly better than the saline control.
The non-specific hLL2-SN-38 conjugates described herein were found to be more effective than the saline control or an equidose mixture of specific mAb and SN-38. Similar non-specific antitumor effects have been reported with other antibody-drug conjugates as well. For example, it has been shown that the CD33-targeted calicheamicin conjugate, hP67.6-AcBut-CalichDMH (gemtuzumab ozagamicin), as well as the calicheamicin conjugates of rituximab and the anti-CD22 mAb, G5/44, produced significant growth-inhibition of 10 different CD33-negative tumor xenografts (40). Passive targeting due to an enhanced permeation and retention effect was invoked to explain these results, which also might be operating to some extent in our experiments. It is also possible that low levels of CD22 expression can lead to the observed therapeutic effects, but this needs to be examined.
While it is tenuous to compare the protein or the drug doses used for these preclinical therapeutic studies with those of other drug conjugates used in solid tumor models, in view of the differences in drugs, tumor models, doses, and dose schedules, such comparisons can be nonetheless informative. For example, auristatin E-conjugated antibodies were evaluated in LNCaP and CWR22 prostate models using 5 mg/kg of protein doses of the conjugates at a schedule of q4d×6 or q4d×12 (41). In therapies in COLO 205, LoVo, and HT-29 models, the maytansinoid conjugate of murine C242 mAb, directed against CanAg antigen, was examined at 16 mg/kg of antibody doses at a schedule of q1d×5 or (q1d×5) ×2 (42), and the dose was 59–79 % of the stated MTD. The maytansinoid conjugate of humanized C242 has been examined clinically (43). More recently, the trastuzumab-DM1 conjugate, designed with a more stable thioether linkage in place of a disulfide linkage, was evaluated preclinically in a HER2-positive breast cancer model (44), with lower protein doses administered in view of an increased stability of the conjugate. The SN-38 conjugates reported herein are used at 12.5–25.0 mg/kg protein doses of the conjugates at a schedule of q4d×8. In the preclinical therapy studies using PEG-SN-38 conjugates (12), the drug was used at its MTD to document therapeutic effects. Similarly, in the polymer micelle formulation of SN-38, the drug was used at the MTD dose or at 50% MTD dose to document significant antitumor effect in a VEGF-secreting tumor model (13). The SN-38 equivalent doses used with the present labetuzumab conjugates are 15–25-fold lower than with the polymer-SN-38 conjugates. The MTD has not been established yet for the hMN-14-SN-38 conjugates, but a 7–14 × higher bolus dose than the cumulative dose used in the therapy experiments was seen to be nontoxic based on limited data. These considerations suggest that our labetuzumab-SN-38 immunoconjugates should prove of value in achieving enhanced bioavailability and reduced toxicity in the therapy of CEACAM5-expressing cancers. It is our intention to develop labetuzumab-CL2-SN-38 and labetuzumab-CL2-SN-38(Et) conjugates further for this purpose.
Statement of Translational Relevance
We report that by combining the CEACAM5 (CEA)-targeting humanized antibody, labetuzumab, with the active drug form of the cancer prodrug, CPT-11, therapy of human colonic and pancreatic cancer xenografts can be achieved at essentially nontoxic equivalent doses of the active drug, SN-38. The antibody has been extensively tested clinically, and is potentially useful for targeted drug therapy of a majority of solid cancers that overexpress the target antigen. The clinical pharmacology and metabolism of both CPT-11 and SN-38 are well established. Targeted therapy with the labetuzumab-SN-38 conjugate could enhance the bioavailability as well as the safety profile of the potent topoisomerase I inhibitor, SN-38. Selective therapeutic efficacies of labetuzumab-SN-38 conjugates, observed in subcutaneous and metastatic tumor models, may translate into a useful addition in the clinical management of CEACAM5-expressing cancers.
Acknowledgments
We thank Anju Nair and Ashraf Gomaa (animal studies), Roberto Arrojo (in vitro experiments), and Agatha Sheerin and Fatma Tat (immunoconjugate preparations) for excellent technical support.
References
- 1.Rougier P, Bugat R. CPT-11 in the treatment of colorectal cancer: Clinical efficacy and safety profile. Semin Oncol (suppl. 3) 1996;23:34–41. [PubMed] [Google Scholar]
- 2.Saijo N. Preclinical and clinical trials of topoisomerase inhibitors. Ann NY Acad Sci. 2000;922:92–99. doi: 10.1111/j.1749-6632.2000.tb07028.x. [DOI] [PubMed] [Google Scholar]
- 3.Kawato Y, Aonuma M, Hirota Y, Kuga H, Sato K. Intracellular roles of SN-38, a metabolite of the camptothecin derivative CPT-11, in the antitumor effect of CPT-11. Cancer Res. 1991;51:4187–4191. [PubMed] [Google Scholar]
- 4.Potmesil M. Camptothecins: from bench research to hospital wards. Cancer Res. 1994;54:1431–1439. [PubMed] [Google Scholar]
- 5.Sawada S, Okajima S, Aiyama R, et al. Synthesis and antitumor activity of 20(S)-camptothecin derivatives: carbamate-linked, water-soluble derivatives of 7-ethyl-10-hydroxycamptothecin. Chem Pharm Bull (Tokyo) 1991;39:1446–1450. doi: 10.1248/cpb.39.1446. [DOI] [PubMed] [Google Scholar]
- 6.Rivory LP, Bowles MR, Robert J, Pond SM. Conversion of irinotecan (CPT-11) to its active metabolite, 7-ethyl-10-hydroxycamptothecin (SN-38), by human liver carboxylesterase. Biochem Pharmacol. 1996;52:1103–1111. doi: 10.1016/0006-2952(96)00457-1. [DOI] [PubMed] [Google Scholar]
- 7.Satoh T, Hosokawa M, Atsumi R, Suzuki W, Hakusui H, Nagai E. Metabolic activation of CPT-11, 7-ethyl-10-[4-(1-piperidino)-1- piperidino]carbonyloxycamptothecin, a novel antitumor agent, by carboxylesterase. Biol Pharm Bull. 1994;17:662–664. doi: 10.1248/bpb.17.662. [DOI] [PubMed] [Google Scholar]
- 8.Gupta E, Lestingi TM, Mick R, Ramirez J, Vokes EE, Ratain MJ. Metabolic fate of irinotecan in humans: correlation of glucuronidation with diarrhea. Cancer Res. 1994;54:3723–3725. [PubMed] [Google Scholar]
- 9.Burke TG, Mi Z. The structural basis of camptothecin interactions with human serum albumin: impact on drug stability. J Med Chem. 1994;37:40–46. doi: 10.1021/jm00027a005. [DOI] [PubMed] [Google Scholar]
- 10.Giovanella BC, Harris N, Mendoza J, Cao Z, Liehr J, Stehlin JS. Dependence of anticancer activity of camptothecins on maintaining their lactone function. Ann NY Acad Sci. 2000;922:27–35. doi: 10.1111/j.1749-6632.2000.tb07022.x. [DOI] [PubMed] [Google Scholar]
- 11.Rivory LP, Riou JF, Haaz MC, et al. Identification and properties of a major plasma metabolite of irinotecan (CPT-11) isolated from the plasma of patients. Cancer Res. 1996;56:3689–3694. [PubMed] [Google Scholar]
- 12.Sapra P, Zhao H, Mehlig M, et al. Novel delivery of SN38 markedly inhibits tumor growth in xenografts, including a camptothecin-11-refractory model. Clin Cancer Res. 2008;14:1888–1896. doi: 10.1158/1078-0432.CCR-07-4456. [DOI] [PubMed] [Google Scholar]
- 13.Koizumi F, Kitagawa M, Negishi T, et al. Novel SN-38-incorporating polymeric micelles, NK012, eradicate vascular endothelial growth factor-secreting bulky tumors. Cancer Res. 2006;66:10048–10056. doi: 10.1158/0008-5472.CAN-06-1605. [DOI] [PubMed] [Google Scholar]
- 14.Zhang JA, Xuan T, Parmar M, et al. Development and characterization of a novel liposome-based formulation of SN-38. Int J Pharm. 2004;270:93–107. doi: 10.1016/j.ijpharm.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 15.Okuno S, Harada M, Yano T, et al. Complete regression of xenografted human carcinomas by camptothecin analogue-carboxymethyl dextran conjugate (T-0128) Cancer Res. 2000;60:2988–2995. [PubMed] [Google Scholar]
- 16.Singer JW, De VP, Bhatt R, et al. Conjugation of camptothecins to poly-(L)-glutamic acid. Ann NY Acad Sci. 2000;922:136–150. doi: 10.1111/j.1749-6632.2000.tb07032.x. [DOI] [PubMed] [Google Scholar]
- 17.Zamai M, VandeVen M, Farao M, et al. Camptothecin poly[n-(2-hydroxypropyl)methacrylamide] copolymers in antitopoisomerase-I tumor therapy: intratumoral release and antitumor efficacy. Mol Cancer Ther. 2003;2:29–40. [PubMed] [Google Scholar]
- 18.Sharkey RM, Juweid M, Shevitz J, et al. Evaluation of a complementarity-determining region-grafted (humanized) anti-carcinoembryonic antigen monoclonal antibodyin preclinical and clinical studies. Cancer Res. 1995;55:5935s–5945s. [PubMed] [Google Scholar]
- 19.Behr TM, Liersch T, Greiner-Bechert L, et al. Radioimmunotherapy of small volume disease of metastatic colorectal cancer. Cancer. 2002;94:1373–1381. doi: 10.1002/cncr.10308. [DOI] [PubMed] [Google Scholar]
- 20.Liersch T, Meller J, Bittrich M, Kulle B, Becker H, Goldenberg DM. Update of carcinoembryonic antigen radioimmunotherapy with (131)I-labetuzumab after salvage resection of colorectal liver metastases: comparison of outcome to a contemporaneous control group. Ann Surg Oncol. 2007;14:2577–2590. doi: 10.1245/s10434-006-9328-x. [DOI] [PubMed] [Google Scholar]
- 21.Moon SJ, Govindan SV, Cardillo TM, D’Souza CA, Hansen HJ, Goldenberg DM. Antibody conjugates of 7-ethyl-10-hydroxycamptothecin (SN-38) for targeted cancer chemotherapy. J Med Chem. 2008;51:6916–6926. doi: 10.1021/jm800719t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharkey RM, Weadock KS, Natale A, et al. Successful radioimmunotherapy for lung metastasis of human colonic cancer in nude mice. J Natl Cancer Inst. 1991;83:627–632. doi: 10.1093/jnci/83.9.627. [DOI] [PubMed] [Google Scholar]
- 23.Griffiths GL, Mattes MJ, Stein R, et al. Cure of SCID mice bearing human B-lymphoma xenografts by an anti-CD74 antibody-anthracycline drug conjugate. Clin Cancer Res. 2003;9:6567–6571. [PubMed] [Google Scholar]
- 24.Sapra P, Stein R, Pickett J, et al. Anti-CD74 antibody-doxorubicin conjugate, IMMU-110, in a human multiple myeloma xenograft and in monkeys. Clin Cancer Res. 2005;11:5257–5264. doi: 10.1158/1078-0432.CCR-05-0204. [DOI] [PubMed] [Google Scholar]
- 25.Gold P, Goldenberg NA. The carcinoembryonic antigen (CEACAM5): past, present, and future. McGill J Med. 1997;3:46–66. [Google Scholar]
- 26.Goldenberg DM, Sharkey RM, Primus F. Carcinoembryonic antigen in histopathology: immunoperoxidase staining of conventional tissue sections. J Natl Cancer Inst. 1976;57:11–22. doi: 10.1093/jnci/57.1.11. [DOI] [PubMed] [Google Scholar]
- 27.Shiveley JE, Beatty JD. CEACAM5-related antigens: molecular biology and clinical significance. Crit Rev Oncol Hematol. 1985;2:355–399. doi: 10.1016/s1040-8428(85)80008-1. [DOI] [PubMed] [Google Scholar]
- 28.Hammarstrom S. The carcinoembryonic antigen (CEA) family: structures, suggested functions and expression in normal and malignant tissues. Semin Cancer Biol. 1999;9:67–81. doi: 10.1006/scbi.1998.0119. [DOI] [PubMed] [Google Scholar]
- 29.Thompson JA, Grunert F, Zimmermann W. Carcinoembryonic antigen gene family: molecular biology and clinical perspectives. J Clin Lab Anal. 1991;5:344–366. doi: 10.1002/jcla.1860050510. [DOI] [PubMed] [Google Scholar]
- 30.Beauchemin N, Draber P, Dveksler G, et al. Redefined nomenclature for members of the carcinoembryonic antigen family. Exp Cell Res. 1999;252:243–249. doi: 10.1006/excr.1999.4610. [DOI] [PubMed] [Google Scholar]
- 31.Blumenthal RD, Osorio L, Hayes MK, Horak ID, Hansen HJ, Goldenberg DM. Carcinoembryonic antigen antibody inhibits lung metastasis and augments chemotherapy in a human colonic carcinoma xenograft. Cancer Immunol Immunother. 2005;54:315–327. doi: 10.1007/s00262-004-0597-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stein R, Goldenberg DM. A humanized monoclonal antibody to carcinoembryonic antigen, labetuzumab, inhibits tumor growth and sensitizes human medullary thyroid cancer xenografts to decarbazine chemotherapy. Mol Cancer Ther. 2004;3:1559–1564. [PubMed] [Google Scholar]
- 33.Tsaltas G, Ford CH, Gallant M. Demonstration of monoclonal anti-carcinoembryonic antigen (CEA) antibody internalization by electron microscopy, Western blotting and radioimmunoassay. Anticancer Res. 1992;12:2133–2142. [PubMed] [Google Scholar]
- 34.Ford CH, Tsaltas GC, Osborne PA, Addeitia K. Novel flow cytometric analysis of the progress and route of internalization of a monoclonal anti-carcinoembryonic antigen (CEA) antibody. Cytometry. 1996;23:228–240. doi: 10.1002/(SICI)1097-0320(19960301)23:3<228::AID-CYTO6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 35.Shih LB, Goldenberg DM, Xuan H, Lu HW, Mattes MJ, Hall TC. Internalization of an intact doxorubicin immunoconjugate. Cancer Immunol Immunother. 1994;38:92–98. doi: 10.1007/BF01526203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stein R, Govindan SV, Hayes M, et al. Advantage of a residualizing iodine radiolabel in the therapy of a colon cancer xenograft targeted with an anticarcinoembryonic antigen monoclonal antibody. Clin Cancer Res. 2005;11:2727–2734. doi: 10.1158/1078-0432.CCR-04-2100. [DOI] [PubMed] [Google Scholar]
- 37.Govindan SV, Cardillo TM, D’Souza CA, et al. Therapy of human colonic and lung cancer xenograftswith SN-38 conjugates of anti-CEACAM5 and anti-EGP-1 humanized monoclonal antibodies. Proc 2007 AACR-NCI-EORTC International Conference on Molecular Targets and Cancer Therapeutics; October 22–26; San Francisco, CA. 2007. (abstract C287). [Google Scholar]
- 38.Blumenthal RD, Sharkey RM, Haywood L, et al. Targeted therapy of athymic mice bearing GW-39 human colonic cancer micrometastases with (131)I-labeled monoclonal antibodies. Cancer Res. 1992;52:6036–6044. [PubMed] [Google Scholar]
- 39.Gold DV, Alisauskas R, Sharkey RM. Targeting of xenografted pancreatic cancer with a new monoclonal antibody, PAM4. Cancer Res. 1995;55:1105–1110. [PubMed] [Google Scholar]
- 40.Boghaert ER, Khandke K, Sridharan L, et al. Tumoricidal effect of calicheamicin immunoconjugates using a passive targeting strategy. Int J Oncol. 2006;28:675–684. [PubMed] [Google Scholar]
- 41.Afar Deh, Bhaskar V, Ibsen E, et al. Preclinical validation of anti-TMEFF2-auristatin E-conjugated antibodies in the treatment of prostate cancer. Mol Cancer Ther. 2004;3:921–932. [PubMed] [Google Scholar]
- 42.Liu C, Tadayoni BM, Bourret LA, et al. Eradication of large colon tumor xenografts by targeted delivery of maytansinoids. Proc Natl Acad Sci USA. 1996;93:8618–8623. doi: 10.1073/pnas.93.16.8618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tolcher AW, Ochoa L, Hammond LA, et al. Cantuzumab mertansine, a maytansinoid immunoconjugate directed to the CanAg antigen: A Phase I, pharmacokinetic, and biologic correlative study. J Clin Oncol. 2003;21:211–222. doi: 10.1200/JCO.2003.05.137. [DOI] [PubMed] [Google Scholar]
- 44.Lewis Phillips GD, Li G, Dugger DL, et al. Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate. Cancer Res. 2008;68:9280–9290. doi: 10.1158/0008-5472.CAN-08-1776. [DOI] [PubMed] [Google Scholar]