Abstract
Background
Complicated choledocholithiasis cannot always be managed by standard surgical, radiologic or endoscopic methods. One additional approach is to use percutaneous techniques developed by endourologists to treat renal calculi. In this report, we present our experience over the past 10 years with this novel approach.
Methods
We conducted a retrospective review of all patients who underwent percutaneous, endoscopic treatment of biliary calculi at our institution between January 1997 and August 2007. Primary outcomes of interest were symptom- and stone-free rates, length of stay in hospital and complications.
Results
Nineteen patients underwent 21 percutaneous treatments for biliary calculi. All were dependent on external drainage for symptom control. The primary indications for treatment were cholangitis, retained stone, biliary colic and jaundice. Seventeen patients (89.5%) had failed prior endoscopic retrograde cholangiopancreatography (ERCP) or open attempts at treatment. The 2 remaining patients (10.5%) were deemed unfit for a general anesthetic. Patients had experienced a mean of 1.8 (standard deviation [SD] 1.0) prior failed attempts at stone removal. We used several treatment modalities, including holmium:yttrium-aluminum-garnet laser (61.9%), electrohydraulic lithotripter (19.0%), ultrasound (9.5%), basket extraction (9.5%) and balloon dilatation of the ampulla (19.0%). Overall, treatment led to successful removal of the biliary drainage tube in 94.7% of patients and 76.2% were stone-free. We performed cholangiograms an average of 21.8 (SD 13.7) days after treatment. The average length of stay in hospital was 1.9 (SD 1.1) days. One patient experienced a perioperative acute coronary syndrome and another experienced prolonged biliary drainage. Both had successful endoscopic treatment of their calculi. There were no cases of treatment-related sepsis, and we observed no other complications.
Conclusion
Biliary calculi may be successfully treated using standard endourologic methods with high stone-free rates. This technique is generally well-tolerated even among high-risk patients.
Abstract
Contexte
La cholédocholithiase avec complications ne peut pas toujours être traitée par les méthodes chirurgicales, radiologiques ou endoscopiques habituelles. Une approche supplémentaire consiste à utiliser des techniques percutanées mises au point par des endo-urologues pour traiter les calculs rénaux. Dans ce rapport, nous présentons l’expérience que nous avons acquise en pratiquant depuis 10 ans cette nouvelle technique.
Méthodes
Nous avons procédé à une étude rétrospective portant sur tous les patients qui ont subi un traitement endoscopique percutané contre des calculs biliaires à notre établissement entre janvier 1997 et août 2007. Nous voulions surtout connaître les pourcentages de patients chez qui les symptômes et les calculs avaient disparu, la durée du séjour à l’hôpital et les taux de complications.
Résultats
Dix-neuf patients ont subi 21 traitements percutanés de calculs biliaires. Dans tous les cas, le contrôle des symptômes dépendait du drainage externe. Les indications premières pour le traitement étaient la cholangite, la rétention d’un calcul, la colique biliaire et l’ictère. Chez 17 patients (89,5 %), la cholangiopancréatographie rétrograde endoscopique ou les tentatives ouvertes de traitement avaient échoué. Les 2 autres patients (10,5 %) avaient été jugés incapables de subir une anesthésie générale. Les patients ont été l’objet en moyenne de 1,8 (écart-type [ET] 1,0) tentative antérieure difficile d’extraction des calculs. Nous avons utilisé plusieurs techniques de traitement, y compris le laser holmium:yttrium aluminium-grenat (61,9 %), le lithotriteur électrohydraulique (19,0 %), l’échographie (9,5 %), la manipulation par panier (9,5 %) et la dilatation par ballonnet de l’ampoule (19,0 %). Dans l’ensemble, le traitement a abouti à l’enlèvement réussi du tube de drainage biliaire chez 94,7 % des patients et 76,2 % n’avaient plus de calcul. Nous avons pratiqué des cholangiogrammes en moyenne 21,8 (ET 13,7) jours après le traitement. La durée moyenne du séjour à l’hôpital s’est établie à 1,9 (ET 1,1) jour. Un patient a eu un syndrome coronarien aigu périopératoire et un autre, un drainage biliaire prolongé. Dans ces 2 cas, le traitement endoscopique du calcul a réussi. Il n’y a eu aucun cas de septicémie reliée au traitement et nous n’avons pas observé d’autres complications.
Conclusion
Il est possible de traiter avec succès les calculs biliaires au moyen des méthodes endo-urologiques habituelles et d’éliminer ainsi les calculs dans un pourcentage élevé de cas. Cette technique est en général bien tolérée, même chez les patients à risque élevé.
Laparoscopic cholecystectomy has become the procedure of choice to treat symptomatic gallstones. However, patients who have clinically important comorbid medical conditions who are not able to undergo a general anesthetic require other forms of treatment such as percutaneous cholecystostomy tube insertion to treat acute cholecystitis. Gallstones may then be extracted in an interval fashion once the tube tract has matured. Unfortunately, not all stones can be cleared this way.
Patients with choledocholithiasis typically have the stones cleared with endoscopic retrograde cholangiopancreaticography (ERCP) and sphincterotomy more than 90% of the time;1 however, ERCP cannot be performed effectively in all patients. Factors such as variability in the anatomy of the ampulla of vater, the presence of duodenal diverticuli or surgical procedures involving the stomach such as Roux-en-Y anastomosis may limit success. Open surgical exploration of the bile duct is not always possible owing to technical reasons or excessive perioperative risk. Unfortunately, options for patients in these circumstances are limited.
In recent years, several groups have begun to explore antegrade choledochoscopy with high-pressure irrigation via a percutaneous transhepatic approach in an attempt to improve stone-free rates.2–8 The initial success of these efforts has led to the collaboration of general surgeons and endourologists at our institution in an effort to relieve biliary obstruction secondary to choledocholithiasis. Our aim was to make patients stone-free and improve outcomes in this patient population. Most of the patients treated so far had complex biliary calculi for which all other surgical treatment options failed. The main reasons for referring patients to our unit were that they were symptomatic despite repeated attempts at stone removal, were at high risk for open surgical procedures, had previous cholecystectomies but had large residual stones (too large for ERCP) and that their anatomies were unfavourable for ERCP.
In this report, we describe a single centre’s experience with percutaneous treatment of complex biliary calculi, using conventional endourologic techniques and instruments.
Methods
We conducted a retrospective review of all patients who underwent percutaneous, endoscopic treatment of biliary calculi from Jan. 1, 1997, to Aug. 31, 2007. We investigated both the endoscopic technique used as well as the type and location of tract as predictors of success. Primary outcomes of interest were symptom- and stone-free rates, length of stay in hospital and complications. The institutional ethics review board (HSREB #13011E) approved our review.
Surgical technique and follow-up
One of 2 endourologists (J.D., H.R.) evaluated all patients preoperatively at St. Joseph’s Health Care, London, Ont. An interventional radiologist had previously secured access to the biliary system via cholecystostomy, transhepatic or T-tube. We allowed percutaneous tracts to mature for a minimum of 3 weeks before we made an attempt at stone manipulation. All patients received antibiotics before the procedure. Tracts were then opacified using 30% radiopaque contrast material to outline the biliary system. Under fluoroscopic guidance, we passed a hydrophilic guidewire through the sphincter of Oddi into the duodenum and then exchanged it for an Amplatz extra-stiff guidewire using a hockey-stick catheter (Cook Medical). Tracts were dilated to either 24-Fr or 30-Fr using Amplatz surgical dilators (Cook Medical) or an Ultraxx balloon (Cook Medical). We used warm normal saline as an irrigant, and we closely monitored the total volume of irrigant. We used standard endoscopic techniques to ensure patients were stone-free at the end of the procedure, if possible.
We used both flexible 14.5-Fr (Pentax Medical Co.) and rigid 26-Fr nephroscopes (Karl Storz GmbH). For biliary stones requiring fragmentation, we routinely used the holmium:yttrium-aluminum-garnet (Ho:YAG) laser. We used both 200-μm and 365-μm laser fibres with an initial setting of 0.8 J/pulse and 8–10 Hz. We used electrohydraulic (Gyrus ACMI), ultrasound-pneumatic (Lithoclast; EMS Medical), Nitinol stone baskets (Cook Medical) and ureteral balloon catheters (Cook Medical) for dilatation of the sphincter of Oddi. We extracted the stones either through the access tract or by flushing them into the duodenum. At the end of the procedure, we ensured drainage through placement of a council catheter (14–22-Fr) or Cope-Loop catheter (10–12-Fr; Cook Urological), which was secured to the skin. We performed cholangiograms routinely in all patients postoperatively (range 1–55 d). The referring surgeon removed the biliary drainage tubes if there was no evidence of residual calculi on the follow-up cholecystogram and no evidence of infection or obstruction. We considered patients to be stone-free if no filling defects were identified on cholangiogram and symptom-free if they did not experience pain, jaundice or cholangitis after removal of the biliary drainage tube.
Results
We identified 19 patients who had undergone 21 percutaneous biliary procedures over the period of interest at our institution. Patient demographic characteristics are presented in Table 1. Prior to referral, patients had already undergone multiple treatments in an attempt to render them stone-free (Table 2), including 10 patients who had previous laparoscopic or open cholecystectomies (52.6%), 13 who had at least one ERCP with or without papillotomy (68.4%) and 10 who had previous open surgical attempts at stone retrieval such as common bile duct exploration or hepatic resection (52.6%). This cohort also included 2 patients (10.5%) previously treated with extra-corporeal shock wave lithotripsy. The mean number of prior treatments for the entire cohort was 1.8 (SD 1.0, range 0–4). All patients were dependent on external biliary drainage for symptom control.
Table 1.
Demographic characteristics of patients who underwent percutaneous, endoscopic treatment of biliary calculi between 1997 and 2007
| Characteristic | No. (%) of patients* |
|---|---|
| Male sex | 5 (26.3) |
| Female sex | 14 (73.7) |
| Indication for treatment | |
| External drainage | 19 (100) |
| Biliary colic | 2 (10.5) |
| Retained stone | 11 (57.9) |
| Cholangitis | 5 (26.3) |
| Jaundice | 1 (5.3) |
| Age, mean (SD) yr | 69.3 (14.1) |
| BMI, mean (SD) | 26.4 (6.9) |
| ASA grade | |
| 1 | 1 (5.3) |
| 2 | 8 (42.1) |
| 3 | 7 (36.8) |
| 4 | 3 (15.8) |
| Anesthetic used (n = 21) | |
| Neurolept | 3 (14.3) |
| General | 18 (85.7) |
ASA = American Society of Anesthesiologists; BMI = body mass index; SD = standard deviation.
Unless otherwise indicated.
Table 2.
Characteristics of biliary calculi in our patient population
| Characteristic | No. (%) of patients* |
|---|---|
| Previous treatment of current stone (n = 21) | 18 (89.5) |
| No. prior treatments, mean (SD) | 1.76 (1.0) |
| Cholecystectomy | 10 (52.6) |
| CBD exploration | 10 (52.6) |
| ERCP | 13 (68.4) |
| PTC | 7 (36.8) |
| SWL | 2 (10.5) |
| Access tract | |
| Cholecystostomy tube | 13 (61.9) |
| Transhepatic tube | 5 (23.8) |
| T-tube | 3 (14.3) |
| Stone location (n = 19) | |
| Gallbladder | 6 (31.6) |
| Common bile duct | 11 (57.9) |
| Cystic duct | 2 (10.5) |
| No. of stones (n = 19) | |
| Single | 7 (36.8) |
| Multiple | 12 (63.2) |
CBD = common bile duct; ERCP = endoscopic retrograde cholangio-pancreatography; PTC = percutaneous trans-hepatic choledochoscopy; SD = standard deviation; SWL = extracorporeal shock wave lithotripsy.
Unless otherwise indicated.
The primary indications for intervention were retained stone requiring external drainage (57.9%), pain (10.5%), infection (26.3%) and jaundice (5.3%). Although general anesthetic was preferred, we performed 3 procedures under neurolept anesthesia owing to the patient being too ill to tolerate a general anesthetic safely (n = 2) or to anesthesiologist preference (n = 1). Ten patients in our cohort were ASA class III or IV (52.6%). The indication to remove only gallstones from patients with a gallbladder still in situ were varied (Table 2). This group included patients who were at extreme perioperative risk (4/6 patients) and 2 patients who had retained fragments in a gallbladder remnant after prior open surgical exploration. We achieved complete stone removal in 5 of 6 patients.
The mean total operating room time was 92.8 (SD 20.9) minutes, whereas mean duration of surgery was 60.4 (SD 19.1) minutes, and mean fluoroscopic time was 6.74 (SD 2.8) minutes. In an attempt to render patients stone-free, we used several endourologic techniques. We performed most procedures exclusively using flexible endoscopes, which facilitated access to the entire biliary system. Use of the Ho:YAG laser was successful in 13 of 21 patients (61.9%). We also used electrohydraulic lithotripsy (19.0%) and ultrasound (9.5%) to fragment large stones. We used stone baskets to extract calculi whenever possible (9.5%), and we employed balloon dilatation of the sphincter of Oddi to facilitate flushing of calculi into the duodenum (19.0%). When we encountered large stones, these were fragmented and extracted through the tract using a rigid endoscope. We placed external drainage tubes in all patients at the end of the procedure.
Biliary tract imaging with cholangiograms occurred an average of 21.8 (SD 13.7) days after treatment. Overall, treatment led to symptom relief in 85.7% of patients and 76.2% were stone-free on postoperative imaging. The referring surgeon was ultimately able to remove the biliary drainage tube in all but 1 patient (4.8%). This patient experienced prolonged biliary drainage, and clamping of the cholecystostomy tube was not tolerated. The average length of stay in hospital was 1.9 (SD 1.1, range 0.5–4.2) days. Two patients in our series required a secondary attempt at percutaneous stone removal. One patient had substantial scarring, and the initial attempt at dilatation of the tract was unsuccessful. A second patient had retained stone fragments and it was not possible to remove the cholecystostomy tube. Secondary procedures were successful in both patients.
There were no intraoperative complications and no patients required blood transfusions. Postoperatively, 1 patient experienced acute coronary syndrome (ACS) and another prolonged biliary drainage. Both had successful endoscopic treatment of their calculi. There were no cases of treatment-related sepsis, and we observed no other complications (Table 3).
Table 3.
Surgical outcomes of patients who underwent percutaneous, endoscopic treatment of biliary calculi at our institution
| Outcomes (n = 21) | No. (%) of patients* |
|---|---|
| Length of stay, mean (SD) d | 1.9 (1.1) |
| Follow-up cholangiogram, mean (SD) d | 21.8 (13.7) |
| Stone-free | 16.0 (76.2) |
| Symptom-free | 18.0 (85.7) |
| Overall tube-free (n = 19) | 18.0 (94.7) |
| Complications | |
| Prolonged biliary drainage | 1.0 (4.8) |
| Acute coronary syndrome | 1.0 (4.8) |
| Treatment-related sepsis | — |
| Blood transfusion | — |
SD = standard deviation.
Unless otherwise indicated.
Discussion
In patients with biliary calculi for which both standard endoscopic and open attempts at stone removal have failed, treatment options are limited. These patients often require indefinite biliary drainage; however, such management is uncomfortable for the patient, requires regular tube changes and nursing support and can be complicated by episodes of obstruction and sepsis.9 Shock-wave lithotripsy has also been used, but may require multiple treatments, and success is limited unless accompanied by ERCP or percutaneous removal.10,11 In particular, clearance rates are low in patients wih very large stones or complex biliary anatomies.12,13 Our study constitutes a highly successful case series of the management of complex biliary calculi using endourologic techniques employed in percutaneous renal surgery.
In our series, patients had exhausted all other treatment options before referral and were dependent on external drainage. More than 52% of the cohort had undergone prior cholecystectomies and a similar number had undergone previous open common bile duct explorations or hepatic resections. In this setting, percutaneous, endoscopic surgery is a seldom-used but complementary modality for treating biliary calculi.2–8 Most series are either case reports or small series, and few can claim expertise in the technique. Despite these limitations, we were able to achieve a stone-free rate of 76.2% over a short follow-up period. Stone-free status was not a requirement for removal of the cholecystostomy tube; tubes were removed at the discretion of the referring general surgeon if residual calculi were small and nonobstructive. We used cholangiograms exclusively to determine the residual stone burden and assess biliary drainage. Imaging occurred about 21–28 days after the procedure; however, optimal timing of this assessment remains to be determined. Under this protocol, we removed external drainage tubes in all but 1 patient, an overall success rate of 94.7%, and 85.7% of patients were completely free of symptoms following treatment. As this was a retrospective case series, we are unable to comment on long-term stone-and symptom-free rates. Optimal treatment requires clearance of stones, elimination of strictures, adequate drainage of the biliary system and preservation of the hepatic parenchyma.7 On review, there were no predictors for failure that could be identified before intervention.
As in other studies,5,7 transhepatic access was necessary in several patients (Table 2). We allowed tracts to mature for a minimum of 3 weeks before dilatation. Despite the relatively large size of the working sheath (up to 30-Fr), no substantial bleeding occurred and no patients required transfusion. Stone clearance can thus be optimized without concern for tract location. However, as biliary anatomy may be complex, preoperative imaging is necessary and collaboration between endourologists, general surgeons and/or interventional radiologists can improve safety and optimize the chance of success. Particular attention must also be paid to management of electrolytes and judicious use of saline irrigation. In contrast to the urinary tract, irrigation fluid directly enters the gastrointestinal tract and can lead to abdominal distension and hypervolemia. Our practice does not include the routine use of a nasogastric tube; however, this may be appropriate in some patients.
Biliary obstruction in North America and Europe differs greatly from Asian disease. In Asian patients, disease is often of infectious etiology and can be complicated by hepatic and common bile duct strictures that impair biliary drainage even after stones are cleared.14,15 Our series comprised predominantly patients of Western descent; however, 1 patient was a Chinese immigrant. We noted no differences in the treatment of this patient compared with the remainder of the cohort. We believe that this technique could also be adapted to treat complex intrahepatic stone disease in Asian patients with cholangitis.
We found that use of the Ho:YAG laser was both safe and effective in the treatment of choledocholithiasis. All patients but 1 were stone-free when the laser was used (92.3%). This laser has a tissue penetration of 0.4 mm and can be used to fragment stones and incise strictures within the ductal system.7 Access is easily accomplished through a small-caliber endoscope with minimal change in deflection (Fig. 1). This allows visualization of intrahepatic and extra-hepatic bile ducts, thereby optimizing stone clearance. Electrohydraulic lithotripsy is a useful adjunct in the endoscopic treatment of calculi. The electrohydraulic lithotripsy probe is small (1.2-Fr) and only minimally decreases endoscope deflection. However, in the biliary system and common bile duct in particular, this modality carries a theoretical risk of causing pancreatitis, although this complication was not seen in our series. The use of ultrasound and pneumatic lithoclasts is limited primarily by the requirement for a rigid endoscope and the inability to access small ducts.
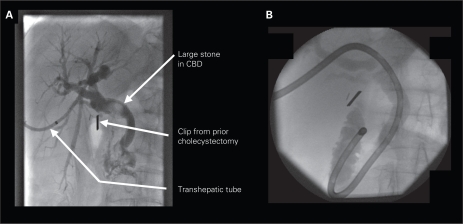
Fig. 1.
(A) Large biliary calculus located within the common bile duct. (B) The patient was successfully treated percutaneously through a dilated transhepatic tract. A 14.5-Fr flexible nephroscope was able to navigate virtually the entire biliary tree, including the duodenum. CBD = common bile duct.
We observed 2 complications in our series. One patient experienced prolonged drainage requiring long-term placement of a biliary drain. As the cholangiogram demonstrated excellent passage of contrast into the duodenum, we felt that this was unlikely to be related to endourologic manipulation. A second patient experienced an acute coronary syndrome postoperatively. This patient was discharged from hospital uneventfully on postoperative day 4. Importantly, no patients experienced postoperative sepsis and no patients died. One contemporary series of percutaneous treatment has reported similar rates of complications, including sub-capsular hematoma, infected hepatic cyst, supraventricular tachycardia and postprocedure pneumonia.7 Others have reported slightly lower complication rates, but tended to contain less surgically complex patients or patients who were healthier and posed less operative risk.2,5 In general, percutaneous treatment compares favourably with ERCP, which had a 30-day morbidity of almost 16% and a mortality of 1% in 1 large prospective study.16 Although length of stay in hospital was short (less than 24 h in 3 patients), most patients had important comorbidities, therefore we recommend overnight observation.
Percutaneous, endourologic surgical techniques can be successfully employed in the management of biliary calculi in selected patients when previous attempts at endoscopic and open stone removal fail. In the setting of failed fluoroscopic manipulation, the main benefit of this approach is direct visualization of stones for either fragmentation or removal. In addition, the use of flexible endourological instruments increases surgical success rates appreciably. Success requires the use of multiple endoscopic techniques and equipment, therefore planning is essential. A multidisciplinary approach using the unique skill sets of endourologists, general surgeons and interventional radiologists is a key element to ensure high stone clearance rates with low morbidity. Despite these limitations, high stone-free and treatment success rates are possible and treatment complications are rare. The precise role for this minimally invasive technique in the treatment of biliary calculi remains to be fully established.
Footnotes
Competing interests: None declared.
Contributors: All authors designed the study. Dr. Ray acquired and analyzed the data and wrote the article, which all other authors reviewed. All authors approved the final version for publication.
This work was presented as a podium presentation at the 59th Annual Meeting of the Northeast Section of the American Urological Association, Rochester, NY, Sept. 5–9, 2007 (third prize winner in the resident essay competition) and as a poster at the 62nd Annual Meeting of the Canadian Urological Association, Québec, Que., Jun. 24–7,2007
References
- 1.Neuhaus H. Endoscopic and percutaneous treatment of difficult bile duct stones. Endoscopy. 2003;35:S31–4. doi: 10.1055/s-2003-41534. [DOI] [PubMed] [Google Scholar]
- 2.Gamal EM, Szabo A, Szule E, et al. Percutaneous video choledochoscopic treatment of retained biliary stones via dilated T-tube tract. Surg Endosc. 2001;15:473–6. doi: 10.1007/s004640000274. [DOI] [PubMed] [Google Scholar]
- 3.Hazey JW, McCreary M, Guy G, et al. Efficacy of percutaneous treatment of biliary tract calculi using the holmium:YAG laser. Surg Endosc. 2007;21:1180–3. doi: 10.1007/s00464-006-9168-6. [DOI] [PubMed] [Google Scholar]
- 4.Monga M, Gabal-Shehab LL, Kamarei M, et al. Holmium laser lithotripsy of a complicated biliary calculus. J Endourol. 1999;13:505–6. doi: 10.1089/end.1999.13.505. [DOI] [PubMed] [Google Scholar]
- 5.Ogawa K, Ohkubo H, Abe W, et al. Percutaneous transhepatic small-caliber choledochoscopic lithotomy: a safe and effective technique for percutaneous transhepatic common bile duct exploration in high-risk elderly patients. J Hepatobiliary Pancreat Surg. 2002;9:213–7. doi: 10.1007/s005340200021. [DOI] [PubMed] [Google Scholar]
- 6.Orii K, Nakahara A, Takase Y, et al. Choledocholithotomy by Yag laser with a choledochofiberscope: case reports of two patients. Surgery. 1981;90:120–2. [PubMed] [Google Scholar]
- 7.Shamamian P, Grasso M. Management of complex biliary tract calculi with a holmium laser. J Gastrointest Surg. 2004;8:191–9. doi: 10.1016/j.gassur.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Teichman JM, Schwesinger WH, Lackner J, et al. Holmium: YAG laser lithotripsy for gallstones. A preliminary report. Surg Endosc. 2001;15:1034–7. doi: 10.1007/s004640080149. [DOI] [PubMed] [Google Scholar]
- 9.Granlund A, Karlson BM, Elvin A, et al. Ultrasound-guided percutaneous cholecystostomy in high-risk surgical patients. Langenbecks Arch Surg. 2001;386:212–7. doi: 10.1007/s004230100211. [DOI] [PubMed] [Google Scholar]
- 10.Amplatz S, Piazzi L, Felder M, et al. Extracorporeal shock wave lithotripsy for clearance of refractory bile duct stones. Dig Liver Dis. 2007;39:267–72. doi: 10.1016/j.dld.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Shim CS, Moon JH, Cho YD, et al. The role of extracorporeal shock wave lithotripsy combined with endoscopic management of impacted cystic duct stones in patients with high surgical risk. Hepatogastroenterology. 2005;52:1026–9. [PubMed] [Google Scholar]
- 12.Gilchrist AM, Ross B, Thomas WE. Extracorporeal shockwave lithotripsy for common bile duct stones. Br J Surg. 1997;84:29–32. [PubMed] [Google Scholar]
- 13.Rabenstein T, Radespiel-Troger M, Hopfner L, et al. Ten years experience with piezoelectric extracorporeal shockwave lithotripsy of gallbladder stones. Eur J Gastroenterol Hepatol. 2005;17:629–39. doi: 10.1097/00042737-200506000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Hanau LH, Steigbigel NH. Cholangitis: pathogenesis, diagnosis, and treatment. Curr Clin Top Infect Dis. 1995;15:153–78. [PubMed] [Google Scholar]
- 15.Rana SS, Bhasin DK, Nanda M, et al. Parasitic infestations of the biliary tract. Curr Gastroenterol Rep. 2007;9:156–64. doi: 10.1007/s11894-007-0011-6. [DOI] [PubMed] [Google Scholar]
- 16.Christensen M, Matzen P, Schulze S, et al. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721–31. doi: 10.1016/s0016-5107(04)02169-8. [DOI] [PubMed] [Google Scholar]