Lymphangiomas (also called cystic hygroma, lymphactic or chylous cysts) are cystic abnormalities of the lymph vessels that are predominantly congenital, though acquired causes have been suggested. They typically present at birth or within the first 2 years of life. Most occur in the head and neck, occasionally the axilla or groin, and very rarely in the mediastinum. We report the case of a patient with a mediastinal cystic lymphangioma that was successfully excised using a minimally invasive technique.
Case report
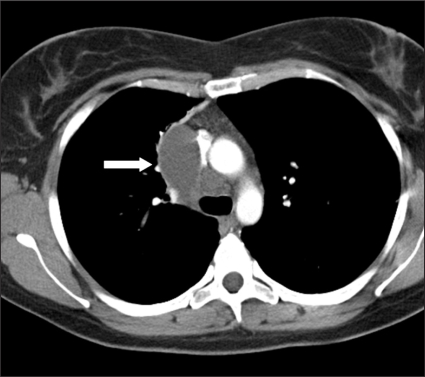
We noted a right superior paratracheal mass on a pre-emigration chest radiograph of a 43-year-old woman. Apart from mild asthma that had developed in adulthood, she was fit and well. She had no other symptoms, nor any history of trauma or previous surgery. A computed tomography (CT) scan of her chest showed a right paratracheal cystic mass (Fig. 1). Considering the uncertainty of the diagnosis and the desire of the patient to emigrate, we offered thorascopic exploration and excision.
Fig. 1.
Chest computed tomography (CT) scan shows a right paratracheal cystic mass with CT attenuation of 0 Hounsfield units (consistent with water; white arrow). The mass was laterally associated with atelectatic lung. We identified no evidence of contrast-enhancement of the wall of the cyst.
Results of an on-table bronchoscopic assessment of the airway were normal. After administering standard general anesthesia and single-lung ventilation, we conducted a 4-port video-assisted thorascopic (VATS) excision of the cyst. We aspirated straw-coloured fluid and excised a “pseudocapsule” of mediastinal pleura, revealing a multi-loculated cyst adjacent to the azygous lymph node at the confluence of azygous vein and superior vena cava. There were no adherent lung or mediastinal structures.
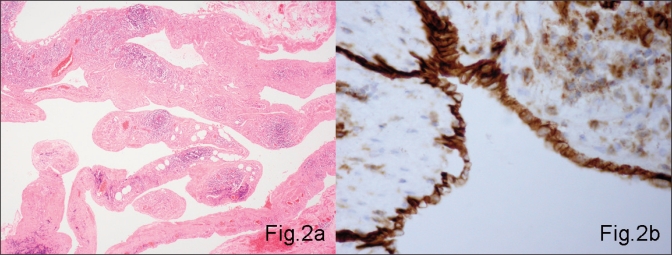
The patient went on to recover uneventfully; at her 3-month follow-up, she was fully recovered. Her asthma symptoms remained unchanged. Histology of the completely excised cystic mass confirmed a multilocular CD31-positive lymphangioma (Fig. 2). We found no features that indicated foregut or teratomatous derivation.
Fig. 2.
Histology of the cyst shows (A) lymphoid tissue and smooth muscle in its wall (hematoxylin and eosin stain, original magnification ×100), with (B) cuboid of flattened cells lining the cavity. Immunostaining with CD31 confirms their endothelial origin and hence the diagnosis of cystic lymphangioma (original magnification ×200).
Discussion
Lymphangiomas are generally considered to be congenital malformations arising because of failure of lymph vessels to connect to the venous system, abnormal budding and/or sequestrations of primitive embryonic lymphatic tissue.1 They are typically thin-walled structures and can be unilocular or, as in our patient’s case, multilocular. They usually contain serous or chylous fluid. They are often classified based on the gross appearance of the abnormal lymphactic tissue as capillary, cavernous or cystic.1,2
Mediastinal cystic lymphangiomas are rare but have been previously reported.1–3 In 279 benign mediastinal cysts excised at the Mayo Clinic over a 40-year period, only 5 (1.8%) were cystic lymphangiomas.4 Most adults are asymptomatic, though airway compression and wheezing are reported.3 Typically, mediastinal cystic lymphangiomas are found in the superior mediastinum, more often on the right side. As such, the differential diagnosis includes the more commonly encountered bronchiogenic cysts, thymic cysts or thymomas. Chest CT scans usually reveal a well-circumscribed and localized homogeneous soft-tissue mass consistent with a cyst (Fig. 1), but a more heterogeneous picture can be seen. Calcification is rare. Histological appearance along with immunocytochemical staining for CD31 confirms the diagnosis. Malignant transformation has not been reported, but complete surgical excision is generally recommended. Traditionally, this was performed via thoracotomy, but several reports advocate thorascopic excision, as in our patient’s case.5
Our report illustrates the typical presentation, radiological appearance and histological diagnosis of lymphangioma. We advocate thorascopic excision if possible when a mediastinal cystic lymphangioma is suspected.
Footnotes
Competing interests: None declared.
References
- 1.Brown LR, Reiman HM, Rosenow EC, III, et al. Intrathoracic lymphangioma. Mayo Clin Proc. 1986;61:882–92. doi: 10.1016/s0025-6196(12)62609-3. [DOI] [PubMed] [Google Scholar]
- 2.Limmer S, Krokowski M, Kujath P. Pulmonary lymphangioma. Ann Thorac Surg. 2008;85:336–9. doi: 10.1016/j.athoracsur.2007.07.033. [DOI] [PubMed] [Google Scholar]
- 3.Misthos P, Sepsas E, Kokotsakis I, et al. Asymptomatic solitary mediastinal cystic lymphangioma: a rare entity. Asian Cardiovasc Thorac Ann. 2006;14:476–8. doi: 10.1177/021849230601400607. [DOI] [PubMed] [Google Scholar]
- 4.Wychulis AR, Payne WS, Clagget OT, et al. Surgical treatment of mediastinal tumors: a 40 year experience. J Thorac Cardiovasc Surg. 1971;62:379–92. [PubMed] [Google Scholar]
- 5.Kitami A, Suzuki T, Usuda R, et al. Diagnostic and therapeutic thoracoscopy for mediastinal disease. Ann Thorac Cardiovasc Surg. 2004;10:14–8. [PubMed] [Google Scholar]