Abstract
Introduction
Plexiform schwannoma is one of the least common variants of schwannoma. It is usually found on the trunk, head, neck and upper extremities. Most reported cases are small tumors, less than 2cm in maximum diameter, arising from superficial nerves. Trauma and neurofibromatosis type 2 are well-recognized risk factors for plexiform schwannoma. It is important to differentiate it from plexiform neurofibroma, because the former has neither an association with von Recklinghausen’s disease nor a malignant potential.
Case presentation
We report a case of a large plexiform schwannoma arising from the posterior tibial nerve in proximity with the medial malleolus. The patient had no history of ankle strain, fracture or neurofibromatosis type 2. Magnetic resonance imaging demonstrated a multinodular, inhomogeneous lesion, measuring 6 × 4 × 2.8 cm. Fine needle biopsy was suggestive of a benign lesion, deriving from neural elements. The mass was excised marginally. Permanent section showed that the lesion was multilobular, surrounded by a thin fibrous capsule and consisting of elongated cells, rare typical mitosis, cells with degenerative features and stained positive for S-100 protein. The patient was not evident disease at the latest follow-up 2.3 years later, with an excellent functional result. No sensory or motor deficits were encountered.
Conclusion
There are no reports in the literature for large plexiform schwannomas arising from the tibial nerve. Marginal excision seems to be the recommended therapy for this rare tumor.
Introduction
Plexiform schwannoma is a very rare, benign peripheral nerve sheath tumor, accounting for 5% of all schwannomas [1,2]. Plexiform schwannomas consist exclusively of Schwann cells presenting a plexiform arrangement which is mimicking plexiform neurofibroma, a tumor with a distinct propensity for anaplastic transformation [3]. Plexiform schwannoma was first described in 1978 by Harkin et al [4] and since then approximately one hundred cases have been reported in the literature. The tumor is most often found on the trunk, head, neck or the upper extremities, but it has occasionally been found in the lower extremities [5]. Most plexiform schwannomas reported are small and measure less than 2cm [6].
We report a case of a sizeable plexiform schwannoma of the posterior tibial nerve in proximity with the medial malleolus.
Case presentation
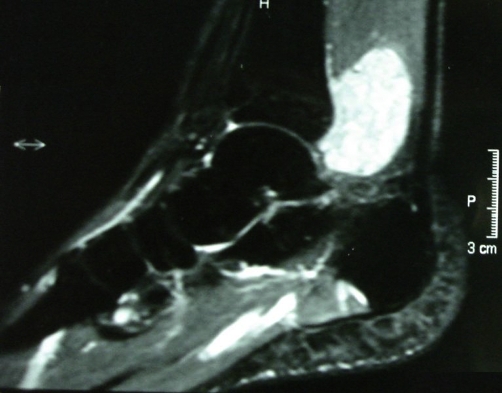
A 29-year-old white Caucasian male presented himself with a slowly growing mass in his right ankle. He was complaining of mild pain and paresthesia of six months duration. On physical examination a firm painless mass was palpable behind the medial malleolus. Magnetic resonance imaging (MRI) demonstrated a multinodular, inhomogeneous lesion, measuring 6 × 4 × 2.8 cm, which was isointense with muscles in T1-weighted images (Figure 1) but of very high intensity in T2-weighted images (Figure 2). No invasion of the surrounding tissues was observed. Diagnosis was oriented towards neurofibromatosis type 2 NF2. The lack of family case-history and the findings of the clinical-imaging examination (brain MRI) that ruled out the possibility of meningiomas, gliomas or schwannomas basically excluded such a diagnosis.
Figure 1.
Preoperative T1-weighted MR image demonstrates a multinodular tumor of the posterior tibial nerve.
Figure 2.
Preoperative T2-weighted MR image demonstrates a high-intensity heterogenous mass in the same place.
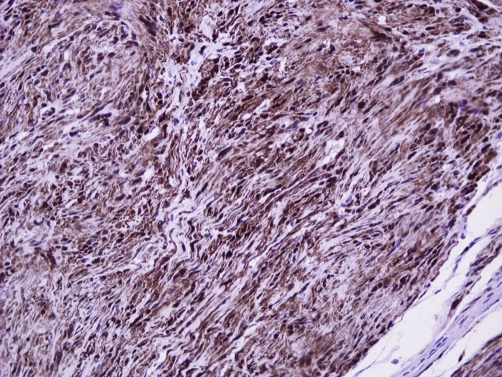
The diagnostic process was completed with fine needle biopsy which was suggestive of a benign lesion, deriving from neural elements. We performed a marginal excision of this mass and monitored the post-operative period which was uneventful. Permanent section showed that the lesion was multilobular, surrounded by a thin fibrous capsule and consisting of elongated cells, rare typical mitosis, cells with degenerative features and stained positive for S-100 protein (Figure 3) but negative for actin and desmin. The lesion was therefore considered to be a benign neurilemoma with plexiform features. The patient was not evident of disease in the latest follow-up, 2.3 years later. No sensory or motor deficits were observed and the patient was very satisfied with the outcome of the treatment.
Figure 3.
S-100 protein immunostain, magnification ×200. A consistent feature of plexiform schwannoma is a diffuse and strong positivity at S-100 protein immunostaining.
Discussion
Plexiform schwannoma is a rare variant of schwannoma with a plexiform or multinodular growth pattern [2,3]. This benign peripheral nerve sheath tumor appears as an asymptomatic, slowly growing lesion; it is usually found on the trunk, head, neck or upper extremities but it has exceptionally been mentioned in the lower extremities [5,7]. Most reported cases are small tumors, originating from superficial nerves. It is generally accepted that there is a strong relationship with NF2 [3,8,9] and that trauma may play a role in the formation of this tumor [3]. The main differential diagnosis includes plexiform neurofibroma as well as malignant peripheral nerve sheath tumor (MPNST) [3,10]. Differential diagnosis from plexiform neurofibroma is of paramount importance due to the fact that it has a propensity for malignant transformation, which has not been reported to occur in plexiform schwannoma [11,12]. It is also crucial to differentiate it from MPNST, which requires wide excision. In the ankle area it is frequently impossible to salvage the limb, especially if there is involvement of a major nerve/vessel, and amputation may be necessary in order to obtain wide margins [13].
Conclusion
In summary we present a rare case of a large plexiform schwannoma of the medial malleolus arising from the main bundle of the posterior tibial nerve. The patient had no history of trauma or NF-2 which are both well-known risk factors; marginal excision yielded an excellent oncological and functional outcome.
Acknowledgments
The authors would like to thank Christina Panou for text editing.
Abbreviations
- MPNST
malignant peripheral nerve sheath tumor
- MRI
magnetic resonance imaging
- NF2
neurofibromatosis type 2
Consent
Written consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MI drafted the manuscript and carried out the design of the study. II carried out the immunohistochemical studies. IP, SK and ND participated in the design and coordination of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
This article is available from: http://casesjournal.com/casesjournal/article/view/8392
Contributor Information
Markos Ioannou, Email: markosioannou@yahoo.gr.
Ioannis Papanastassiou, Email: jpapa73@yahoo.gr.
Ioanna Iakowidou, Email: voulamita@yahoo.gr.
Stamatios Kottakis, Email: nomiki15@hotmail.com.
Nikolaos Demertzis, Email: ndemertzis@gmail.com.
References
- Rongioletti F, Drago F, Rebora A. Multiple cutaneous plexiform schwannomas with tumors of the central nervous system. Arch Dermatol. 1989;125(3):431–432. doi: 10.1001/archderm.125.3.431. [DOI] [PubMed] [Google Scholar]
- Weiss SW, Goldblum JR. Malignant tumors of the peripheral nerves. In: Strauss M, Grey L, editors. Enzinger and Weiss’s Soft Tissue Tumors. 4. St. Louis: Mosby, Inc; 2001. p. 1166. [Google Scholar]
- Woodruff JM, Marshall ML, Godwin TA, Funkhouser JW, Thompson NJ, Erlandson RA. Plexiform (multinodular) schwannoma. A tumor simulating the plexiform neurofibroma. Am J Surg Pathol. 1983;7(7):691–697. doi: 10.1097/00000478-198310000-00009. [DOI] [PubMed] [Google Scholar]
- Harkin J, Arrington J, Reed R. Benign plexiform schwannoma: a lesion distinct from plexiform neurofibroma [abstract] J Neuropathol Exp Neurol. 1978;37:622. doi: 10.1097/00005072-197809000-00165. [DOI] [Google Scholar]
- Iwashita T, Enjoji M. Plexiform neurilemmoma: a clinicopathological and immunohistochemical analysis of 23 tumours from 20 patients. Virchows Arch A Pathol Anat Histopathol. 1987;411(4):305–309. doi: 10.1007/BF00713373. [DOI] [PubMed] [Google Scholar]
- Katsumi K, Ogose A, Hotta T, Hatano H, Kawashima H, Umezu H, Endo N. Plexiform schwannoma of the forearm. Skeletal Radiol. 2003;32(12):719–723. doi: 10.1007/s00256-003-0701-6. [DOI] [PubMed] [Google Scholar]
- Ikushima K, Ueda T, Kudawara I, Nakanishi K, Yoshikawa H. Plexiform schwannoma of the foot. Eur Radiol. 1999;9:1653–1655. doi: 10.1007/s003300050904. [DOI] [PubMed] [Google Scholar]
- Val-Bernal JF, Figols J, Vázquez-Barquero A. Cutaneous plexiform schwannoma associated with neurofibromatosis type 2. Cancer. 1995;76(7):1181–1186. doi: 10.1002/1097-0142(19951001)76:7<1181::AID-CNCR2820760713>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Ishida T, Kuroda M, Motoi T, Oka T, Imamura T, Machinami R. Phenotypic diversity of neurofibromatosis 2: association with plexiform schwannoma. Histopathology. 1998;32:264–270. doi: 10.1046/j.1365-2559.1998.00336.x. [DOI] [PubMed] [Google Scholar]
- Kleinmann GM, Sanders FJ, Gagliardi JM. Plexiform schwannoma. Clin Neuropathol. 1985;4:265–266. [PubMed] [Google Scholar]
- Fletcher CD. Peripheral nerve sheath tumors. A clinicopathologic update. Pathol Annu. 1990;25(Pt 1):53–74. [PubMed] [Google Scholar]
- Megahed M. Plexiform schwannoma. Am J Dermatopathol. 1994;16(3):288–293. doi: 10.1097/00000372-199406000-00011. [DOI] [PubMed] [Google Scholar]
- Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986;57(10):2006–2021. doi: 10.1002/1097-0142(19860515)57:10<2006::aid-cncr2820571022>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]