Abstract
Objectives
To implement team-based learning in the workshop portion of a pathophysiology and therapeutics sequence of courses to promote integration of concepts across the pharmacy curriculum, provide a consistent problem-solving approach to patient care, and determine the impact on student perceptions of professionalism and teamwork.
Design
Team-based learning was incorporated into the workshop portion of 3 of 6 pathophysiology and therapeutics courses. Assignments that promoted team-building and application of key concepts were created.
Assessment
Readiness assurance tests were used to assess individual and team understanding of course materials. Students consistently scored 20% higher on team assessments compared with individual assessments. Mean professionalism and teamwork scores were significantly higher after implementation of team-based learning; however, this improvement was not considered educationally significant. Approximately 91% of students felt team-based learning improved understanding of course materials and 93% of students felt teamwork should continue in workshops.
Conclusion
Team-based learning is an effective teaching method to ensure a consistent approach to problem-solving and curriculum integration in workshop sessions for a pathophysiology and therapeutics course sequence.
Keywords: team-based learning, small groups, workshops, case-based teaching, active learning
INTRODUCTION
Pathophysiology and therapeutics courses delivered as part of doctor of pharmacy (PharmD) curricula in colleges and schools of pharmacy are often team-taught courses to which multiple faculty members contribute. Typically, these courses are delivered in a sequence. Often, large classroom lectures are combined with small classroom discussions (workshops) where students apply knowledge to patient case scenarios. The primary advantage to multiple faculty members teaching across 1 educational sequence is that students are able to learn from specialists or content experts for each topic. However, the team-teaching approach is not without flaws. A large number of faculty members teaching 1 course make it difficult to provide a consistent approach to common course objectives such as teamwork, professionalism, and communication. Additionally, it is difficult for faculty members to integrate content from other areas of the curriculum if they are not familiar with those areas.
Faculty members at The Ohio State University College of Pharmacy involved in teaching the workshop portion of a pathophysiology and therapeutics course sequence were concerned about the level of integration of course materials and common skills from across the curriculum, as well as the degree to which problem-solving was being consistently taught and evaluated. In order to address these issues, a revision of the workshop portion of the pathophysiology and therapeutics courses in the second year of a 4-year PharmD program was undertaken. The pedagogical strategy of team-based learning was introduced into this course sequence to address these challenges.1
Team-based learning is an instructional strategy that builds upon the strengths of individual students by allowing them to work together to achieve a common goal. In order to effectively accomplish this task, 4 principles are essential: (1) teams must be appropriately formed; (2) students must be accountable for both individual and teamwork; (3) assignments must promote learning and team development; and (4) feedback must be frequent and timely.1
Team-based learning is designed to enhance the quality of learning through the use of high-performing learning teams. The principle behind team-based learning is that students working together as a team are capable of achieving a higher level of learning than individual students alone. Since its inception in the 1970s, team-based learning has been used in numerous settings and disciplines of postsecondary education, including the small classroom setting.2 In the past decade, team-based learning has been studied, successfully implemented, and extensively described in medical education.1,3 Letassy and colleagues also described the use of team-based learning in an endocrinology module of a PharmD curriculum.4
The backbone of team-based learning is the use of individual and team assessments throughout the course.1 To determine basic understanding of the assigned topic, students are assessed as an individual and as a team on assigned readings and lectures through a readiness assurance process. Design and implementation of the readiness assurance process is crucial to the success of team-based learning. The first step of the process consists of completing an individual readiness assurance test on the assigned topic. Immediately following the individual test, the exact same questions are given on a team readiness assurance test. The final step of the readiness assurance process is to immediately review the questions following the team readiness assurance test to ensure students receive timely feedback. Students are rewarded for individual preparation of course material via the individual test and are accountable to fellow team members if they are not prepared for the team readiness assurance test. The use of this format facilitates student-to-student teaching and learning and provides students the opportunity to achieve a higher level of content understanding via interactions with their peers. In addition to the readiness assurance process, team-based learning recommends the incorporation of other activities that require application of course content and continued team development.1
Team-based learning provides many benefits to professional education: high level of student learning, communication, professionalism, and consistency.1 In addition to these benefits, team-based learning can also help colleges and schools of pharmacy demonstrate to the Accreditation Council for Pharmacy Education that they are using “proven teaching and learning methodologies, using a variety of teaching and learning techniques, applying and reinforcing curricular content, and introducing and reinforcing innovations to promote optimal learning.”5 In this paper, we will describe the implementation of team-based learning into the workshop portion of 3 courses within a 6-course pathophysiology and therapeutics sequence in order to (1) promote integration of concepts across the pharmacy curriculum, (2) provide a consistent problem-solving approach to patient care, and (3) determine the impact of team-based learning on student perceptions of professionalism and teamwork. We present data from 1 class of students going through the pathophysiology and therapeutics course sequence. This project was approved by The Ohio State University Institutional Review Board.
DESIGN
Pedogogy
The optimal delivery of a 6-course pathophysiology and therapeutics sequence in The Ohio State University's entry-level PharmD program had continually evolved since its inception in 1999. The sequence consisted of 3 or 4 hours of lecture plus one 3-hour discussion-based, small classroom experience (workshop) per week, which incorporated active-learning strategies and case-based discussions. Initially, each of the 6 courses had an individual course director responsible for all aspects of the course (eg, securing and scheduling lecturers, developing examinations, overseeing workshops). These courses were designed to enhance student learning on a wide array of therapeutic areas through textbook readings, lecture by content experts, and discussion during workshop sessions.
A review of the pathophysiology and therapeutics sequence was conducted after 4 years of course delivery. A major finding of this review was the substantial amount of time and resources dedicated to the workshop sessions, often at the expense of other aspects of the course. Despite efforts to manage consistency across workshops and progressive development of student skills across the 6 courses, the directors felt curricular integration and skill development could be strengthened further. In order to address these findings, the decision was made to hire a workshop coordinator in 2006 to oversee workshop sessions and ensure that the consistency, integration, and progression that were initially desired would occur. The decision was made by the workshop coordinator to use team-based learning as the backbone for the workshop sessions because of its numerous potential benefits to pharmacy education.
Educational Environment
The pathophysiology and therapeutics sequence was delivered over 6 consecutive courses, beginning in the fall of the second year. Workshops met for 3 hours weekly and were facilitated by workshop faculty members; 25-30 students were assigned to each workshop. Team-based learning was implemented in courses 2, 3, and 4 of the 6-course pathophysiology and therapeutics sequence. Course 1 of the sequence focused on patient history taking and physical examination; it did not incorporate team-based learning into assigned workshop experiences. At the beginning of courses 2, 3, and 4, teams of 5 to 6 students were assigned by the workshop coordinator who ensured students did not have any of the same teammates from previous courses. Students were encouraged to work out any team dynamic issues among themselves to enhance professional development and conflict resolution skills.
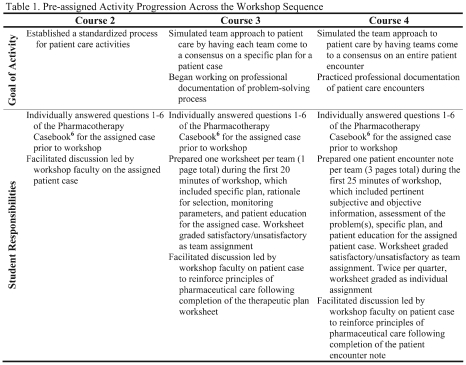
Each workshop was divided into a pre-assigned portion and an in-class portion. For the pre-assigned portion, students were assigned a patient case out of the Pharmacotherapy Casebook6 relating to recent lecture content. Weekly assignments for the pre-assigned case changed from course to course to facilitate development of the problem-solving process and students' ability to handle increasingly complex patient cases (Table 1). Students initially reviewed the basic principles of the pharmaceutical care process7 and then progressively applied the aspects of this process through documentation exercises.
For the in-class portion of the workshop sessions, activities were distributed to the teams for completion following the pre-assigned case discussion. In-class activities were typically mini-case scenarios involving application of the week's primary disease state. Efforts were made to incorporate concepts throughout the pathophysiology and therapeutics sequence and other portions of the curriculum (eg, ethics, law) into the in-class activities. Following the team workup, workshop faculty facilitated classroom discussion of in-class activities.
The introduction of team-based learning into the workshops required a shift in teaching responsibilities. Previously, the majority of workshop preparation time consisted of development of patient cases and rubrics by the content expert and subsequent grading of individual patient documentation exercises by workshop faculty members. The change to team-based learning eased the grading burden and shifted the faculty time required from post-workshop grading to pre-workshop planning and development; however, no substantial decrease in time required to teach was noted among workshop faculty members. Workshop faculty members worked with content experts and the workshop coordinator to develop team activities and readiness assurance process assessments. The process of grading was streamlined by making all readiness assurance test questions multiple-choice items and using a grading system of satisfactory or unsatisfactory for work submitted by teams.
Time involved in the workshop portion of the pathophysiology and therapeutics sequence consisted of 4 sections lasting for 3 hours, plus a 2-hour weekly meeting among workshop faculty members, the workshop coordinator, the course director, and content experts. Additionally, workshop faculty members graded written documentation and drug information assignments. The workshop coordinator was responsible for supervising the workshop instructors, managing and editing workshop activities and the readiness assurance process, directing weekly workshop meetings, and handling all student questions and final grading for the workshops. Overall time spent outside of scheduled classroom sessions and content meetings was approximately 5 to 10 hours per section per week for each workshop faculty member, and 10 to 15 hours per week for the workshop coordinator.
EVALUATION AND ASSESSMENT
One hundred sixteen students from the Class of 2009 completed the pathophysiology and therapeutics sequence. Courses 2, 3, and 4 of the sequence were assessed as follows. Three multiple-choice examinations constituted 75% of the final grade. Examination questions were developed by content experts in relation to assigned readings, lecture material, and to a lesser extent, workshop content. The remaining 25% of the course grade was designated to the workshop sessions. Workshop grades were made up of the following components: 5 individual readiness assurance tests (20%-30% of workshop grade), 5 team readiness assurance tests (30%-40%), peer evaluation (10%), drug information assignment (10%), and written documentation of patient cases (20%-30%).
Five times throughout each course, students completed individual readiness assurance tests and team readiness assurance tests. Each assessment consisted of 5 multiple-choice case-based questions that were developed by workshop faculty members with oversight from the workshop coordinator and content expert. The current literature on team-based learning suggests preparing the readiness assurance process to assess student knowledge and comprehension of the readings and lecture content1; however, since the course examinations already included some content questions at the recall level, the readiness assurance process assessments for the pathophysiology and therapeutics workshops were written at the application and analysis level of Bloom's taxonomy.8 In order to test application of challenging therapeutic concepts and fulfill the objective of integrating content across the curriculum, questions incorporated readings, lectures, and workshop activities. To simulate clinical practice situations, questions contained more than 1 possible answer; however, only 1 best answer was accepted as correct for each question. Students could individually submit a written challenge to individual readiness assurance test questions within 24 hours of the assessment. Students were given 15 minutes to complete the individual readiness assurance test and 20 minutes to complete the team test. Each assessment was immediately reviewed to stimulate discussion and provide immediate feedback to students.
At the end of each of the 3 courses, students completed a peer evaluation of each of their teammates. For this evaluation, students could not assign the same grade to each team member and had to explain why the highest and lowest grades were awarded. The average peer evaluation score accounted for 10% of the student's workshop grade for the course.
The effectiveness of team-based learning for workshop activities was assessed in 3 ways. First, student performance on graded readiness assurance process assessments was monitored across 3 of the 6 pathophysiology and therapeutics courses to determine the impact of team-based learning on problem-solving skills. Second, students were asked to self-assess teamwork and professionalism at the beginning and end of the 3 courses. Finally, at the end of course 4, students were asked their perceptions and satisfaction on the principles of team-based learning and whether it should be continued in the curriculum.
To assess student professionalism and teamwork, a survey instrument was developed using questions previously studied in team-based learning for teamwork and questions from a pharmacy professionalism survey instrument.9,10 Students were asked to complete the survey instrument at the beginning and end of each of the 3 academic courses and incentive points were given for survey completion. For both the teamwork and professionalism instruments, the items were summed in order to produce a “score” for each student at the beginning and end of each course. A paired t test was used to compare pre- and post-course teamwork and professionalism scores.
In order to assess perceptions on the principles of team-based learning in a workshop, students were asked to complete an electronic survey instrument at the end of course 4 and given an incentive for survey completion.
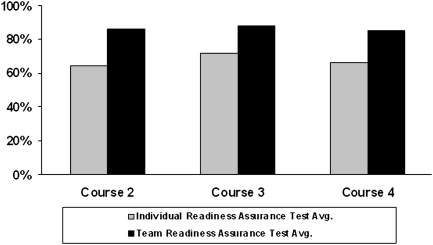
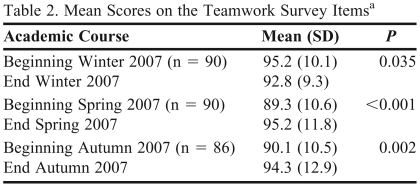
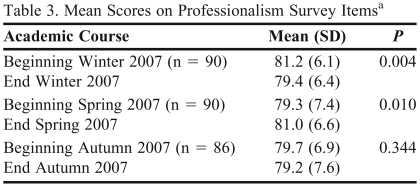
Student performance on readiness assurance process assessments for 3 consecutive courses is displayed in Figure 1. Student scores on individual readiness assurance tests and team readiness assurance tests were relatively consistent. For all 3 courses, average scores on the team readiness assurance test were nearly 20 percentage points higher than scores on the individual readiness assurance test. Table 2 provides the mean scores for the teamwork instrument at both the beginning and end of the 3 consecutive courses. The students began with positive impressions of teamwork, and these impressions continued throughout the courses in which team-based learning was implemented. Similarly, students started with a high sense of professionalism and this remained over the 3 courses (Table 3).
Figure 1.
Average student scores on the Readiness Assurance Process assessments.
Table 2.
Mean Scores on the Teamwork Survey Itemsa
The score was out of a possible 110. Higher scores indicate more teamwork.
Table 3.
Mean Scores on Professionalism Survey Itemsa
The score was out of a possible 90. Higher scores indicate a higher degree of professionalism.
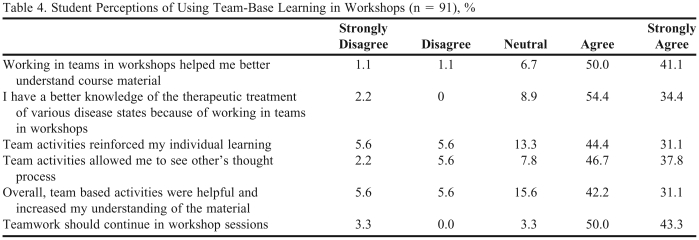
Following the 3 courses that included team-based learning, students were asked to complete a survey on perceptions of team-based learning in the workshop sessions. Seventy-eight percent (91/116) of students completed the survey instrument (Table 4). Overall, student evaluations of team-based learning were extremely positive. On all questions posed in the evaluation, at least 75% of students agreed or strongly agreed with statements regarding the topic of working in teams. More than 90% of students felt that working in teams in workshops helped them better understand the course material, 88% felt it gave them a better knowledge of therapeutic treatments of disease, and 75% felt it reinforced individual learning. The vast majority of students (83%) felt that team-based learning should continue. Additionally, when asked what they liked best about workshop sessions, 59.4% of students responded that it was working in teams, and when asked what they liked least, only 5.5% of students stated that working in teams was their least favorite aspect of the workshop.
Table 4.
Student Perceptions of Using Team-Base Learning in Workshops (n = 91), %
DISCUSSION
While the use of team-based learning in an individual course of a PharmD curriculum has been discussed,4 this is the first paper to discuss the use of team-based learning in small group workshops that were part of a lecture course and delivered across a sequence of pathophysiology and therapeutics pharmacy courses. The decision to incorporate team-based learning was based on faculty members' desire to strengthen workshop sessions over previous course designs. The use of team-based learning provided additional benefits to a professional program, including a structured, consistent process for approaching patient care, integration of content throughout the pharmacy curriculum, and enhancement of student professionalism, teamwork, and communication.
Horizontal and vertical integration of curricular content is desired to reinforce key concepts of pharmacy education. However, the large number of topics covered and the multiple faculty members necessary to deliver a PharmD curriculum make this integration difficult to achieve. Team-based learning provides a consistent approach to a workshop series for students and faculty members. The use of team-based learning in our pathophysiology and therapeutics sequence exposed multiple faculty members to its framework. This structural exposure let faculty members integrate concepts from their areas of expertise into other parts of the curriculum within the familiar context of team-based learning. Our use of a workshop coordinator for the sequence provided faculty members with a point person with whom to share any ideas for content integration into the curriculum. Additionally, student familiarity with team-based learning format and expectations makes integration of curricular content easier to achieve by encouraging students to focus on the content instead of assignment instructions and assessments. Finally, team-based learning allowed students to share knowledge and ideas with peers when revisiting concepts from earlier in the curriculum, thereby facilitating student-to-student reinforcement in place of individual student recall.
The use of team-based learning provided a consistent framework for pathophysiology and therapeutics workshops to operate. Workshop activities used a case textbook6 and mini-case patient scenarios to reinforce the problem-solving approach to pharmaceutical care.7 For the workshop sequence, individual readiness assurance tests and team readiness assurance tests were developed to evaluate student ability to apply the pharmaceutical care process to course materials. The framework of team-based learning used the readiness assurance process to encourage student-to-student learning. Throughout the sequence, team readiness assurance test scores were consistently 20% higher than individual readiness assurance test scores, indicating that student-to-student teaching and learning was taking place in workshop sessions and reinforcing the value of team-based learning. The results of our experience were consistent with other team-based learning research and indicated that high-level learning occurred within student teams.1 The concept of using an established framework to facilitate repetition of concepts, and ultimately progression of problem-solving skills throughout a sequence of courses, is viewed as one of the strongest benefits of using team-based learning in the manner described.
Professionalism and teamwork are concepts important to pharmacy students' development; however, they are difficult to incorporate and assess in most curricula. The use of team-based learning in weekly workshop sessions encouraged students to develop these necessary skills. Through weekly interactions with peers, students learned how to approach patient case scenarios as part of a team and come to a consensus on how to proceed. Assignment of teams by the workshop coordinator for each course was viewed as an important component to provide student exposure to multiple peers for team-building activities. Throughout the weekly workshop sessions, professional communication and behavior were necessary to complete assignments and achieve a satisfactory score. The inclusion of peer evaluation as a portion of the workshop grade further encouraged students to consistently contribute to workshop assignments.
To measure the impact of team-based learning on student perception of teamwork and professionalism, students were asked to complete a survey instrument at the beginning and end of each of the 3 pathophysiology and therapeutics courses. The teamwork portion of the survey incorporated concepts proposed by Birmingham and McCord9 on student perception of teammate trust, willingness to assist, and motivation. A validated instrument to measure professionalism in pharmacy students was used.10 Initial scores from this survey indicated students perceived teamwork and professionalism skills as very strong prior to the introduction of team-based learning. While a significant improvement in student perceptions occurred for both teamwork and professionalism across the sequence, the unanticipated high initial scores made this change difficult to assess. The authors do not feel the positive change in scores indicate a significant educational change due to high initial scores; however, results indicated that team-based learning did not negatively impact pharmacy students' perception of teamwork or professionalism.
At the end of the 3-course sequence, students completed a survey instrument on the use of team-based learning for the workshop sequence. Students felt positive about the team-based learning format. Only 5% of students felt the worst part of workshops was the teamwork aspect. In contrast, the vast majority of students felt working within a team helped reinforce learning and understanding of course material. Nearly 95% of students encouraged the continued use of teamwork in workshop sessions.
Another benefit of the change to team-based learning involved a shift in the type of work performed by workshop faculty members. Previously, workshop faculty members' time and energy were largely spent on grading students' individual case write-ups. Introducing team-based learning removed the grading burden, allowing workshop faculty members to focus on other key course aspects, including design of workshop activities, better preparation for each workshop, and enhanced facilitation of the actual workshop.
Limitations
Logistical challenges and concerns with using team-based learning for workshop sessions included the amount of time necessary to ensure consistency, progression, and integration across the pathophysiology and therapeutics sequence. In addition to time spent in each course, development of activities that integrated content across the curriculum required workshop faculty members and the workshop coordinator meeting and coordinating with multiple faculty members.
Initial student perceptions of professionalism and teamwork were higher than anticipated. The elevated initial impressions made it nearly impossible to detect a meaningful change in these parameters. This was the first use of this survey instrument for professionalism in our students, so it is unknown whether these perceptions occurred from matriculation through our program or if the students had these impressions prior to enrollment in our graduate professional program.
Workshop faculty members were encouraged to facilitate discussion among students and not provide answers. This required workshop faculty members to deflect questions back to the class and have students use available resources to determine the answers. While this led to more discussion and ultimately better student preparation and skill development, it was often viewed as frustrating by students desiring a “correct” answer. Additionally, students viewed the 3-hour workshops as a long time to sit and work on activities for a small portion of the final pathophysiology and therapeutics course grade.
Despite the time required by the workshop coordinator to develop activities, oversee the workshops, and ensure consistency, progression, and integration, the time was spent mostly behind the scenes and not directly in front of the students. Depending on the process of teaching evaluation used by a college or school of pharmacy for career advancement, these teaching responsibilities may not align with traditional teaching expectations, thereby inadvertently penalizing faculty members. In other words, if faculty reward structures for teaching responsibilities are centered around the process of obtaining direct student input on teaching, this approach will not produce the required evidence. Additionally, use of standardized faculty evaluation forms may not include questions designed for facilitation of student-led discussion, making student evaluations difficult to obtain and interpret for both workshop faculty members and the workshop coordinator.
SUMMARY
The use of team-based learning in workshop sessions provided pharmacy students with a consistent approach that reinforced and enhanced their understanding of the problem-solving process and required them to exercise professionalism and the communication skills necessary to become competent pharmacists. The use of a workshop coordinator was extremely valuable to oversee the incorporation of team-based learning into the course sequence and facilitate integration of concepts from across the pharmacy curriculum into workshop activities.
REFERENCES
- 1.Michealsen LK, Parmelee DX, McMahon KK, Levine RE, editors. Team-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving Learning. Sterling. VA: Stylus Publishing; 2008. [Google Scholar]
- 2.Hernandez SA. Team learning in a marketing principles course: cooperative structure that facilitate active learning and higher level thinking. J Marketing Educ. 2002;24(1):73–85. [Google Scholar]
- 3.Thompson BM, Schneider VF, Haidet P, Levine RE, McMahon KK, Perkowski LC, Richards BF. Team-based learning at ten medical schools: two years later. Med Educ. 2007;41(3):250–7. doi: 10.1111/j.1365-2929.2006.02684.x. [DOI] [PubMed] [Google Scholar]
- 4.Letassy NA, Fugate SE, Medina MS, Stroup JS, Britton ML. Using team-based learning in an endocrine module taught across two campuses. Am J Pharm Educ. 2008;72(5) doi: 10.5688/aj7205103. Article 103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Accreditation Council for Pharmacy Education. Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. The Accreditation Council for Pharmacy Education Inc. Available at: http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed on May 6, 2009.
- 6.Schwinghammer TL, editor. Pharmacotherapy Casebook: A Patient-Focused Approach. 6th ed. New York, NY: McGraw-Hill; 2005. [Google Scholar]
- 7.Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: the Clinician's Guide. 2nd ed. New York, NY: McGraw-Hill; 2004. pp. 9–17. [Google Scholar]
- 8.Bloom VS, editor. New York, NY: McKay; 1956. Taxonomy of Education Objectives. The Classification of Educational Goals. Handbook I: Cognitive Domain. [Google Scholar]
- 9.Birmingham C, McCord M. Group Process Research: Implications for Using Learning Groups. In: Michaelsen LK, Knight AB, Fink LD, editors. Team-based Learning: A Transformative Use of Small Groups. Westport, CT: Praeger; 2002. pp. 73–93. [Google Scholar]
- 10.Chisholm MA, Cobb H, Duke L, McDuffie C, Kennedy WK. Development of an instrument to measure professionalism. Am J Pharm Educ. 2006;70(4) doi: 10.5688/aj700485. Article 85. [DOI] [PMC free article] [PubMed] [Google Scholar]