Abstract
Objective
To implement a long-term continuing education course for pharmacy practitioners to acquire competency in and accreditation for conducting collaborative comprehensive medication reviews (CMRs).
Design
A 1½- year curriculum for practicing pharmacists that combined distance learning (using e-learning tools) and face-to-face learning was created. The training consisted of 5 modules: (1) Multidisciplinary Collaboration; (2) Clinical Pharmacy and Pharmacotherapy; (3) Rational Pharmacotherapy; (4) CMR Tools; and (5) Optional Studies.
Assessment
The curriculum and participants' learning were evaluated using essays and learning diaries. At the end of the course, students submitted portfolios and completed an Internet-based survey instrument. Almost all respondents (92%) indicated their educational needs had been met by the course and 68% indicated they would conduct CMRs in their practice. The most important factors facilitating learning were working with peers and in small groups. Factors preventing learning were mostly related to time constraints.
Conclusion
Comprehensive medication review competencies were established by a 1½- year continuing education curriculum that combined different teaching methods and experiential learning. Peer support was greatly appreciated as a facilitator of learning by course participants.
Keywords: medication review, continuing education, experiential learning, distance education
INTRODUCTION
Among the elderly population, polypharmacy is increasing1,2; more psychotropic and sedative drugs are being prescribed than is appropriate3,4; and use of medications that are potentially harmful to this age group is common.5-7 Since a significant number of medication-related problems are considered preventable, solutions to reduce them have been actively sought worldwide.8-13 Various medication review procedures based on the philosophy of pharmaceutical care have been implemented in different countries.14-21 In Finland, the Ministry of Social Affairs and Health has recommended regular medication reviews and multiprofessional collaboration as a key solution to promote rational pharmacotherapy and prevent medication-related problems in the elderly.22
Society's increasing expectations of pharmacists' involvement in assuring rational drug therapy and appropriate medication review creates pressure to maintain current and develop new competencies. Finnish community pharmacies have taken actions to promote the safe use of medicines since the early 1990s. The most important effort was the national program in 2000-2003 called TIPPA (in English: Customized Information for the Benefit of the Patient from the Community Pharmacy). In TIPPA all the key pharmacy stakeholders, including government, universities, continuing education centers, and professional organizations, successfully combined their efforts to educate pharmacists to improve patient counseling.23-25 The increased communication as a result of TIPPA drew the attention of pharmacists to various drug-related problems that could not been solved by the pharmacists acting alone. The TIPPA follow-up program in 2004-2007 built on the developments and experiences of the first phase of the program and focused on creating more advanced pharmacy services based on multidisciplinary collaboration and on meeting the needs of the medicine users. The most important service developed under the follow-up program was the comprehensive medication review (CMR) which involves collaboration between pharmacists and physicians.
The clinical and collaborative skills of Finnish pharmacists did not meet the competencies required to conduct CMRs in collaboration with other health care professionals. This was the case even though Finnish community pharmacists have been required to maintain their professional skills and knowledge. For that purpose an organized system of national, local, and in-house training was established in the 1980s.26 Various long-term continuing education trainings have been available for Finnish community pharmacists since the mid-1990s, but no formal accreditation system has been required or established. Our experience and experience in other countries has indicated that changing the working patterns and implementing new professional services would require a long-term training process involving more than 1 pharmacist from the same workplace.23,27 Those participating in training can perform as agents of change in their workplace; thus, independent assignments need to be designed to support this role and collaborative learning with peers. In addition to focusing on factual knowledge, it is important to involve all employees of the organization in the development of new practices.28 This evidence of the importance of sharing new knowledge and applying it to practice collaboratively with peers in the workplace, as well as the content of the training described in this paper, are in line with the Accreditation Council for Pharmacy Education's (ACPE) Accreditation Standards for Continuing Pharmacy Education.29 It states that continuing pharmacy education (CPE) activities should “promote pharmacists' application of learned principles to practice” and that “the teaching and learning methodologies used should foster the continued development of critical thinking and problem-solving skills.” Nevertheless, few actual training programs that comply with the recommendation have been reported in any country, which increases the significance of our curricular effort from the perspective of ACPE competencies.
In this paper we describe the development, learning objectives, syllabus content, and participant receptiveness to a long-term continuing education for pharmacy practitioners to acquire competency and accreditation for conducting comprehensive medication reviews (CMRs) in collaboration with other health care professionals, particularly physicians.
The educational goals of this curriculum are to: (1) support participant's professional development and acquisition of sufficient clinical skills and knowledge to conduct CMRs; (2) establish collaboration needed for CMR with other health care professionals, particularly with local general practitioners; and (3) create the CMR procedure applicable to local circumstances.
DESIGN
The planning of the training was coordinated by the TIPPA Coordination Group with representatives from universities, professional organizations, national pharmaceutical continuing education centers, and the National Centre for Pharmacotherapy Development.
In the first phase of the curriculum design, examples of similar training programs abroad were systematically sought. Although pharmacists provide medication review services in several countries,16-21 no comprehensive training programs were found. As a result, both the content for and pedagogic design of the curriculum were created by the TIPPA Coordination Group.
Expected Outcomes
The curriculum was designed to increase pharmacy practitioners' theoretical knowledgebase but also to promote higher levels of learning, such as synthesis, application, and evaluation.30 The goal for the curriculum was to create such strong theoretical and practical skills in conducting CMRs that at the end of their studies the participants would be able to provide CMR services independently in a collaborative health care team.
Structure of the Training
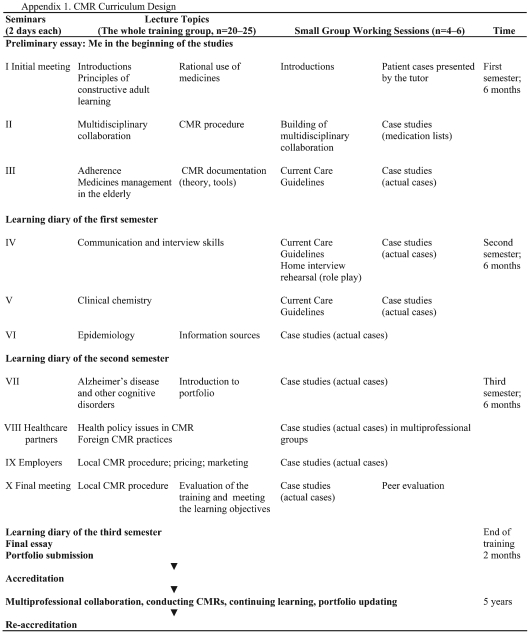
Pilot program.
A pilot program in 2005-2006 was crucial for creating the actual course syllabus and a CMR procedure compatible with the Finnish health care system. A group of 26 pharmacists from different health care settings and geographic regions were chosen because they already had experience in collaborating with other health care professionals. Because hospital and community pharmacists may have complementary knowledge and skills, both were invited to participate in the same training. Participants (5 from hospitals and 21 from community pharmacies) were encouraged to create their own prototype of the comprehensive medication review procedure. They also identified and tested applicable tools and information sources for CMR and developed forms for documentation. The aim of these assignments was to collect as wide a range of information as possible on different types of CMR procedures developed by the participants. The CMR prototypes and documentation forms were analyzed to determine the uniform procedure that would be nationally applied in CMR. The next 2 CMR courses initiated in late 2006 (Appendix 1) were built on the experience gained from the pilot training. The experiences from these 2 training courses involving 42 practitioners (22 in Helsinki and 20 in Oulu) are reported here.
Ongoing structure.
The size of the training group was 20 to 25 pharmacists. To be accepted into the program, the applicants had to have a bachelor of science (BSc) or master of science (MSc) degree in pharmacy. Applicants also had to describe their professional competence, working history, and educational activity after graduation. They needed to have adequate IT-tools in their workplace (eg, a drug-drug interaction database) and an established professional relationship with local health care providers. Also, a preliminary action plan for the local CMR procedure had to be stated in the application. The curriculum lasted for 3 semesters, over a 1½-year time period, and participants earned 35 European Credit Transfer System (ECTS) credits (1 credit corresponds to 26.7 hours of student work). The training was lengthy for 2 reasons. First, persistent multiprofessional collaboration takes time, especially when the aim is to create a permanent CMR service. Second, because the participants worked fulltime, study time for the course was limited.
The curriculum consisted of 10 two-day seminars and independent distance learning sessions in-between, some of which took place in an e-learning environment (Appendix 1). Before each seminar session, participants needed to complete assignments, including review of specific reading materials. Seminar days included lectures by leading national experts from different fields and small group sessions. Distance learning consisted of the following elements throughout the training: (1) engaging in multidisciplinary networking and development of a local CMR procedure intended to establish permanent collaboration; (2) learning by reviewing actual patient cases selected from the pharmacist's own practice; (3) conducting theoretical studies and researching the literature; and (4) working in an e-learning environment, Moodle (Moodle, Perth, Western Australia). Moodle is an interactive discussion forum where participants can discuss their patient cases, solve problems, and share ideas and knowledge. Secondly, Moodle had templates that covered almost all of the course-related materials including timetables, assignments, CMR forms and tools, reading assignments, and lecturers' PowerPoint presentations. A majority of the completed assignments were posted in the discussion areas on Moodle so that all participants could read and comment on them.
Pedagogic Design
In continuing education, the connection between personal development, work, and education is important. Kolb sees experiential learning as a process that is capable of linking these 3 factors.31 A tight connection between theoretical studies and work was essential to CMR training. The goal of creating a successfully working CMR procedure in the participants' working environment required commitment from both the employer and coworkers.28 Thus, Kolb's theory of experiential learning was chosen as the pedagogic basis for the CMR training. In Kolb's model, learning is a continuous circle, where concrete experience is the basis for observation and reflection. Reflection assists abstract conceptualization, which in turn leads to active experimentation.31
In order to take all of these aspects into account, a variety of teaching methods were applied.32 Experiences of long-term continuing education during the TIPPA program had revealed that various reflective teaching methods involving the entire staff of an organization was required to improve knowledge and skills in patient counseling performance.23 In CMR training teaching students with different learning styles has been taken into account, especially in the structure of the seminar sessions (Appendix 1).31,33
Interactive sessions that emphasize participating in learning activities and practicing skills are more likely to produce positive learning outcomes than traditional lectures.34 Also case-based learning produces better learning outcomes of clinical skills than traditional teaching methods.35 Therefore, actual CMR cases and case discussions were used as the main stimulus to fulfill the educational goals of the CMR training. The training participants, who were all practicing pharmacists, already had basic pharmaceutical knowledge and skills, but their skills needed to be improved for them to attain the competence needed to conduct CMRs. When participants reviewed actual patient cases, they learned to apply their existing knowledge, but also to recognize their deficiencies and identify future educational needs. Knowledge was gained from lectures, literature, and assignments, as well as from multiprofessional discussions with physicians and nurses.
In order to facilitate interaction between students, the 20 to 25 CMR training participants were divided into small groups of 4 to 6 at the beginning of the training. Hospital pharmacists and community pharmacists were placed in separate groups to achieve optimal peer support. Each small group was guided by a tutor who was accredited to conduct CMRs. The small groups had their own discussion forums in the e-learning environment and they met during each seminar session to follow everyone's progress in development of the local application of the general CMR procedure and to discuss the patient cases and various related clinical issues. The groups also had long-term projects, the most remarkable of which was the Current Care Guidelines project, in which each group chose the current care guidelines that they perceived as most relevant to their clinical practice, summarized the guidelines, and applied them to selected patient cases.
The accreditation process has to be renewed every 5 years. In order to accomplish reaccreditation, the pharmacists have to update the portfolio and show that they have kept up their competence by both conducting CMRs and further educating themselves. The first reaccreditations are due in 2013.
Core Contents
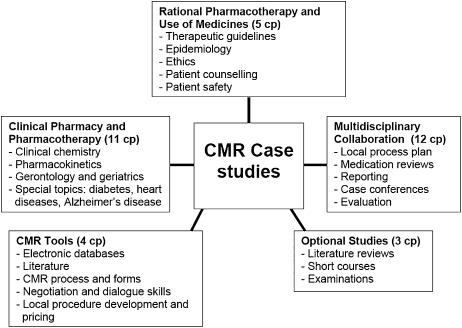
The course consisted of 5 modules continuing throughout the entire training (Figure 1). The case studies integrated the modules by combining different kind of knowledge needed in conducting CMRs.
Figure 1.
Core contents of the CMR training (35 ECTS credits (cp), 1.5 years).
Multidisciplinary Collaboration.
The Multidisciplinary Collaboration module was the most time intensive, with assignments intended to guide the participants in creating a permanent CMR collaboration within their local health care environment. The stages were: (1) contacting health care partners; (2) conducting a case conference based on an anonymous medication profile from an actual working environment; (3) designing a CMR process, eg, defining the inclusion criteria for patients; (4) conducting reviews, writing case reports and having case conferences; (5) evaluating collaboration among staff and local health care providers after implementation of the CMR process and creating a plan for continued collaboration. Health care partners were invited to participate in a 2-day seminar while developing the local collaborative model to share experiences (Appendix 1).
Clinical Pharmacy and Pharmacotherapy.
The objective for the Clinical Pharmacy and Pharmacotherapy module was to teach participants to integrate data from different information sources. It included elements of pharmacotherapy, pharmacokinetics, geriatrics, ethiology and pathology, psychology, nursing science, and ethics. Clinical chemistry, ie, the interpretation of laboratory results, was also included in the module. All thematic topics were approached from the point of view of medication review. Thus, evidence-based treatment of common diseases and the effects that, for example, aging, renal failure, and polypharmacy have on pharmacotherapy were essential topics in this module. The participants had an opportunity to choose the topic for a few lectures based on their educational needs. Possible topics included Alzheimer's disease, diabetes, heart diseases, and psychiatric disorders. The theoretical knowledge obtained from the lectures and assignments was used in practice when participants reviewed actual patient cases. Each participant had to complete 5 to 10 reviews during the training. Cases were presented and discussed in small groups at every seminar session. Cases were also brought to the e-learning environment, where there was a separate discussion area for peer group support, feedback, and advice concerning the review.
Rational Pharmacotherapy.
The goals of the Rational Pharmacotherapy module were to make participants notice irrational medication use patterns, understand the importance of patient counseling, and learn to interpret the strength of evidence from the medical literature. The module covered the following subjects: concepts and importance of rational use of medicines and patient safety, drug related problems (DRPs),15,36 adherence, factors that influence medication use and selection, and trends in pharmacotherapy and ethics. Evidence-based Finnish Current Care Guidelines were studied and the knowledge gained was used in conducting CMR.
CMR Tools.
The Tools module was intended to acquaint the participants with different databases and reliable information sources that could be used during the CMR process. Different forms used in the CMRs (eg, patient interview form and case report form) were also introduced to the participants. Development, marketing, and pricing of CMR services were crucial assignments in the Tools module. Participants studied written material on communication skills and interview techniques and then worked in small groups with a communications professional to practice and improve their skills and techniques.
Based on the self-assessment mentioned earlier, the participants were expected to analyze their learning needs and compare them to the contents of the training. Optional studies (3 ECTS credits) could be chosen to complete knowledge on relevant topics. Optional studies could be performed either through literature reviews, conventional examinations, or short additional training courses, or through a combination of these. All optional studies had to be related to CMR and include a reflective component (eg, a written report to reflect what they had learned and how they could apply the knowledge to CMR).
EVALUATION AND ASSESSMENT
Reflection and self-assessment were strongly supported throughout the training. Participants' learning was evaluated continuously by the principal training coordinator through learning diaries; written assignments, especially in the e-learning environment; and the portfolio. Since all writing assignments were mandatory, the training coordinator got a clear impression of the development of the participants' knowledge and skills. Most students used the discussion areas in the e-learning environment voluntarily to discuss assignments and patient cases and to share ideas and tips, eg, concerning useful literature.
Before the first seminar days, participants were to write a preliminary essay on the topic “Me in the Beginning.” In this essay, the participants evaluated their current knowledge; described their educational needs, goals, and expectations; and how they hoped to contribute to the learning of other participants. After every seminar session the participants were asked to write in a learning diary about their progress and what they had learned. Learning diaries were returned to the principal coordinator of the CMR training after each semester. The principal coordinator evaluated participants' progress throughout the training and provided them with written feedback. After the final seminar, the participants had to write a final essay that compared their actual learning over the course with the expectations and knowledge described in their preliminary essay. The deepest form of reflection occured when the participants prepared the required portfolio for the TIPPA Coordination Group in order to achieve accreditation from the professional organizations. The portfolio needed to reflect the students' professional and personal growth from the start of the training to its completion and address the participants' plans for the future. The portfolio had to cover 3 main themes: (1) personal development, (2) multidisciplinary collaboration, and (3) development of the local CMR procedure. At least 3 case study reports of completed CMRs had to be included in the portfolio.
Survey
Within a month after the final seminar days, the participants assessed their training via an Internet-based survey routinely used by the University of Kuopio, Centre for Training and Development. The survey instrument consisted of 3 sections. Five statements with a 5-point nominal rating scale (1 = poor to 5 = outstanding) were used to assess participants' perceptions about their learning; curriculum design; teaching methods; learning materials; and content validity of the assignments/group projects/and examinations. The next section had 2 questions with responses of yes, possibly, and no: (1) Did the training meet your educational expectations and needs? (2) Would you recommend this training for your peers? The third section of the survey instrument had 4 open-ended questions: (1) What factors facilitated your learning in this training?; (2) What factors prevented or hampered your learning in this training?; (3) What did you learn and how can you apply it to practice?; (4) What ideas, comments and suggestions do you have for the improvement of the training.
The participants also were asked to estimate whether they were going to conduct CMRs in the future. The alternative responses given were: I will (the plans for the future already exist); I intend to continue the practice; I'm still uncertain; and I will not conduct CMRs in my practice in the future.
Of the 42 participants who attended the training, 90% (n=38) responded to the Internet survey. The mean score for the 5 statements in the first section was 4.5 ± 0.7. The highest ratings were given to learning (4.6 ± 0.7) and curriculum design (4.6 ± 0.5). Teaching methods and learning materials got a mean score of 4.4 ± 0.7 and 4.4 ± 0.6, respectively. The mean score for content validity of assignments/group works/examinations was 4.3 ± 0.7.
A majority (92%, n=35) of the respondents responded that the course met their educational needs. The remaining 3 respondents answered that the course “possibly” met their educational needs. Even more (95%; n=36) of the respondents answered that they would recommend the training for their peers.
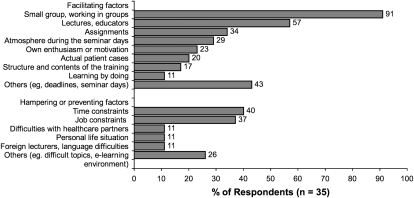
Thirty-five participants (83%) responded to the open-ended questions about factors which facilitated, prevented, or hampered their learning (Figure 2). Almost all of them (91%, n=32) mentioned that the small group format (43%, n=15), working in groups (29%, n=10), or the knowledge, enthusiasm or activity of other participants (20%, n=7) had improved their learning. The most commonly mentioned preventive or hampering factors were “lack of time” and “busyness” (40%, n=14) and job constraints (37%, n=13) such as busyness or lack of support at the workplace.
Figure 2.
Opinions of CMR training participants on factors facilitating or preventing learning (open-ended question, % of the respondents, n=35).
There were miscellaneous responses (86%, n=36) to the question “What did you learn and how can you apply it to practice?” The most commonly mentioned phrase was “I learned a lot” (36%, n=13). Ten respondents (28%) mentioned issues related to pharmacology or pharmacotherapy. Both multidisciplinary collaboration and development of CMR procedure were mentioned by 8 participants (22%), geriatric pharmacotherapy by 6 (17%), and interpretation of laboratory test values by 5 (14%). Several participants mentioned “broader perspective” or “seeing things as a whole” (17%, n=6) or application of existing knowledge (11%, n=4). Half of the respondents (n=18) mentioned the learning was useful in everyday work, regardless of whether it involved conducting CMRs.
Twenty-nine participants (69%) presented ideas to improve the training. Even though working in small groups was seen to be a useful way of learning, some of the respondents wished for more communication among all participants (14%, n=4) or occasional mixing of tutor groups for wider perspective (10%, n=3). Six respondents (21%) wished for additional annual training days. The development of CMR services was seen as difficult and time consuming, so a few students (10%, n=3) wanted that to be started in an earlier phase of the training, and an additional 3 (10%) wanted a lecture on an operational local CMR practice.
Most of the respondents (68%, n=26) planned to conduct CMRs in the future. Five (13%) answered “I will (the plans for the future already exist)” and 21 (55%) “I intend to continue the practice.” Eleven respondents (29%) were still uncertain. Only 1 respondent answered “I will not conduct CMRs in the future.” She indicated that she had discontinued her studies. The respondents mentioned the following barriers to conducting CMRs in the future: financing (13%, n=5); still unclear if the employer wants CMR services to be produced (8%, n=3); and development of the local CMR procedure still unfinished (5%, n=2). The results suggest that the time between course completion and survey administration may not have been long enough for the participants to build the infrastructure required to provide CMR services. None of the barriers mentioned were related to lack of the respondents' skills, enthusiasm, or will to conduct CMRs.
Results from the Internet survey and portfolios showed that the learning objectives were met in personal development, conducting CMRs, and cooperating with health care providers. The biggest challenges involved creating competencies needed to develop and implement the local CMR procedure.
DISCUSSION
The objective of the CMR training course was to provide the participating pharmacists with sufficient theoretical and practical skills to be able to provide CMR services in collaboration with other health care professionals. A majority of the course participants believed they would continue to conduct CMRs after the training, suggesting that the goal of the training was achieved. The responses by the participants showed that the content of the CMR training met their educational needs and they were satisfied with the learning and the teaching methods used. Several participants found that attending the CMR training improved their performance at work. Working in small groups and with other participants were deemed to be the most important facilitators of learning. This is consistent with earlier findings that communication with ones' peers is the most important way for pharmacists to learn.37 The greatest factors hampering learning during CMR training, lack of time and job constraints, were clearly associated with trainees working full time while taking the course. Earlier studies show similar barriers toward pharmacists' life-long learning and participation in continuing education.26,38,39
Student essays, learning diaries and portfolios were crucial to the assessment of the quality and content of the CMR training. The principal coordinator used this feedback during the training to develop a comprehensive understanding of how to better focus the ongoing training, but also to improve the curriculum for future CMR training courses. Since the 2 training courses described in this paper, the curriculum has been carried out twice every year. The content of subsequent training courses are still based on the feedback from the previous ones. The student satisfaction with the training has continued to be high and so far only slight modifications in the content of the training have been applied.
Just after the training, about a third of the participants were still uncertain whether they would conduct CMRs in the future, although keeping up competencies on both a practical and theoretical level is required for reaccreditation. The participants were expected to conduct 5 to 10 CMRs during their studies. This amount is arguably too small to establish a routine for conducting CMRs on an ongoing basis. However, several patient cases were discussed during small-group sessions as well as in the e-learning environment. In addition, none of the participants mentioned lack of skills as a barrier for future CMRs. Finnish pharmacists have not traditionally been expected to develop the skills to produce and actively sell pharmaceutical services. Some participants commented on the difficulty and time-consuming nature of the development of a local CMR service, and wished for this assignment to begin earlier in the course. This change has already been made in more recent CMR training courses. It would be valuable to conduct online interviews of participants to see how CMR practice is evolving in Finland and how many of those accredited stay active in conducting CMRs.
The greatest future challenge may be that there are no systems in place for integrating CMRs in other health services or no Finnish guidelines for reimbursement of CMR services. This is probably the main reason why some participants were still uncertain about continuing to do CMRs. Studies to evaluate the benefits of CMRs are underway and the results may greatly affect policymaking and demand for CMR services in Finland. Until then, pharmacists must take the initiative in developing and maintaining local CMR procedures. Both Finnish CMR procedure and training remain dynamic and developing processes. The experiences of CMR training participants are continually used to improve the training. It is important to be prepared for greater demand for CMR services and guarantee competencies for graduating and practicing pharmacists by increasing training in clinical pharmacy.
SUMMARY
Comprehensive medication review competencies were established by a 1½- year continuing education curriculum that combined different teaching methods and experiential learning. Peer support was greatly appreciated as a facilitator of learning by course participants.
ACKNOWLEDGEMENTS
The contributions of Dr. Timothy Chen, University of Sydney, Australia; Prof. Alan Lyles, University of Baltimore, United States; and Thomas R. Fulda, BA, MA, United States are acknowledged in curriculum development (TC) and preparing the manuscript (AL, TRF).
REFERENCES
- 1.Linjakumpu T, Hartikainen S, Klaukka T, Veijola J, Kivelä S-L, Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002;55(8):809–17. doi: 10.1016/s0895-4356(02)00411-0. [DOI] [PubMed] [Google Scholar]
- 2.Jyrkkä J, Vartiainen L, Hartikainen S, Sulkava R, Enlund H. Increasing use of medicines in elderly persons: a five-year follow-up of the Kuopio 75+ Study. Eur J Clin Pharmacol. 2006;62(2):151–8. doi: 10.1007/s00228-005-0079-6. [DOI] [PubMed] [Google Scholar]
- 3.Hartikainen S, Klaukka T. Use of psychotropics is high among very old people. Eur J Clin Pharmacol. 2004;59(11):849–50. doi: 10.1007/s00228-003-0702-3. [DOI] [PubMed] [Google Scholar]
- 4.Linjakumpu TA, Hartikainen SA, Klaukka TJ, et al. Sedative drug use in the home-dwelling elderly. Ann Pharmacother. 2004;38(12):2017–22. doi: 10.1345/aph.1E067. [DOI] [PubMed] [Google Scholar]
- 5.Pitkälä KK, Strandberg TE, Tilvis RS. Inappropriate drug prescribing in home-dwelling, elderly patients. A population-based survey. Arch Intern Med. 2002;162(15):1707–12. doi: 10.1001/archinte.162.15.1707. [DOI] [PubMed] [Google Scholar]
- 6.Fialová D, Topinková E, Gambassi G, et al. Potentially inappropriate medication use among elderly home care patients in Europe. JAMA. 2005;293(11):1348–58. doi: 10.1001/jama.293.11.1348. [DOI] [PubMed] [Google Scholar]
- 7.Raivio MM, Laurila JV, Strandberg TE, Tilvis R, Pitkälä K. Use of inappropriate medications and their prognostic significance among in-hospital and nursing home patients with and without dementia in Finland. Drugs Aging. 2006;23(4):333–43. doi: 10.2165/00002512-200623040-00006. [DOI] [PubMed] [Google Scholar]
- 8.Beijer HJM, de Blaey CJ. Hospitalisations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm World Sci. 2002;24(2):46–54. doi: 10.1023/a:1015570104121. [DOI] [PubMed] [Google Scholar]
- 9.Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348(16):1556–64. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 10.Gurwitz J, Field T, Harrold L, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289(9):1107–16. doi: 10.1001/jama.289.9.1107. [DOI] [PubMed] [Google Scholar]
- 11.Aspden P, Wolcott JA, Bootman JL, Cronenwett LR, editors. Washington DC: the National Academy Press; 2006. Preventing Medication Errors: Quality Chasm Series. [Google Scholar]
- 12. Council of Europe, Expert Group on Safe Medication Practices (P-SP-PH/SAFE). Creation of a better medication safety culture in Europe: Building up safe medication practices; 2006. Available at: http://www.coe.int/t/e/social_cohesion/soc-sp/Medication%20safety%20culture%20report%20E.pdf. Accessed on May 8, 2009.
- 13.van der Hooft CS, Dieleman JP, Siemes C, et al. Adverse drug reaction-related hospitalisations: a population-based cohort study. Pharmacoepidemiol Drug Saf. 2008;17(4):365–71. doi: 10.1002/pds.1565. [DOI] [PubMed] [Google Scholar]
- 14.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–43. [PubMed] [Google Scholar]
- 15.Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Clinician's Guide. 2nd ed. New York: The McGraw-Hill Companies; 2004. [Google Scholar]
- 16.Harjivan C, Lyles A. Improved medication use in long-term care: building on the consultant pharmacist's drug regimen review. Am J Managed Care. 2002;8(4):318–26. [PubMed] [Google Scholar]
- 17.Fulda TM, Lyles A, Pugh MC, Christensen D. Current status of prospective drug utilization review. J Manage Care Pharm. 2004;10(5):433–41. doi: 10.18553/jmcp.2004.10.5.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sorensen L, Stokes JA, Purdie DM, Woodward M, Elliott R, Roberts MS. Medication reviews in the community: results of a randomized, controlled effectiveness trial. Br J Clin Pharmacol. 2004;58(6):648–64. doi: 10.1111/j.1365-2125.2004.02220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Pharmacists Association and the National Association of Chain Drug Stores Foundation. Medication therapy management in pharmacy practice: Core elements of an MTM service model (version 2.0) J Am Pharm Assoc. 2008;48:341–53. doi: 10.1331/JAPhA.2008.08514. [DOI] [PubMed] [Google Scholar]
- 20. Department of Health. National Health Service Act 1977: The Pharmaceutical Services (Advanced and Enhanced Services) (England) Directions 2005; 2005. Available at: http://www.dh.gov.uk/assetRoot/04/10/75/97/04107597.pdf. Accessed on June 26, 2008.
- 21. Australian Government, Department of Health and Ageing. Medication management reviews: Residential medication management review (RMMR). Available at: http://www.health.gov.au/internet/main/publishing.nsf/Content/health-epc-dmmrqa.htm. Accessed on May 8, 2009.
- 22. The Ministry of Social Affairs and Health, Finland. Development of geriatric care and elderly care. Report by Rapporteur ad int. Sosiaali- ja terveysministeriön selvityksiä 2006:30. (in Finnish, summary in English) Available at: http://www.stm.fi/Resource.phx/publishing/documents/7477/index.htx. Accessed on May 8, 2009.
- 23.Kansanaho H, Pietilä K, Airaksinen M. Can a long-term continuing education in patient counselling promote a change in the practice of Finnish community pharmacists? Int J Pharm Pract. 2003;11:153–60. [Google Scholar]
- 24.Kansanaho H, Puumalainen I, Varunki M, Ahonen R, Airaksinen M. Implementation of a professional program in Finnish community pharmacists in 2000–2002. Patient Educ Couns. 2005;57:272–9. doi: 10.1016/j.pec.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 25. Puumalainen I. Development of Instruments to Measure the Quality of Patient Counselling. [dissertation]. Kuopio, Finland: University of Kuopio, 2005. Available at: http://www.uku.fi/vaitokset/2005/isbn951-27-0401-3.pdf Accessed on May 8, 2009.
- 26.Savela E. Kuopio, Finland: University of Kuopio; 2003. Professional Competence in Community Pharmacies – Continuing Education among Finnish Pharmacists Applying the Norm Theory as a Theoretical Framework [dissertation] (English summary) [Google Scholar]
- 27.De Almeida Neto AC, Benrimoj SI, Kavanagh DJ, Boakes RA. Novel educational training program for community pharmacists. Am J Pharm Educ. 2000;64(3):302–7. [Google Scholar]
- 28.Robinson DG, Robinson JC. Training for impact. How to link training needs to business and measure the results. San Francisco, CA: Jossey-Bass, Inc., Publishers; 1989. [Google Scholar]
- 29. Accreditation Council for Pharmacy Education. Accreditation standards for continuing pharmacy education. The Accreditation Council for Pharmacy Education Inc., 2007. Available at: http://www.acpe-accredit.org/pdf/CPE_Standards_Final.pdf. Accessed on September 10, 2009.
- 30.Bloom BS, editor. New York, NY: McKay; 1956. Taxonomy of Educational Objectives. The Classification of Educational Goals. Handbook I: Cognitive Domain. [Google Scholar]
- 31.Kolb DA. Englewood Cliffs, New Jersey: Prentice Hall P T R; 1984. Experiential Learning. Experience as the source of learning and development. [Google Scholar]
- 32.Svinicki MD, Dixon NM. The Kolb model modified for classroom activities. College Teaching. 1987;35(4):141–6. [Google Scholar]
- 33.Vaughn L, Baker R. Teaching in the medical setting: balancing teaching styles, learning styles and teaching methods. Med Teach. 2001;23(6):610–2. doi: 10.1080/01421590120091000. [DOI] [PubMed] [Google Scholar]
- 34.Davis D, O'Brien MAT, Freemantle N, Wolf FM, Mazmanian P, Taylor-Vaisey A. Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA. 1999;282:867–74. doi: 10.1001/jama.282.9.867. [DOI] [PubMed] [Google Scholar]
- 35.Depuis RE, Persky AM. Use of case-based learning in a clinical pharmacokinetics course. Am J Pharm Educ. 2008;72(2) doi: 10.5688/aj720229. Article 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Westerlund LOT, Marklund BRG, Handl WHA, Thunberg ME, Allebeck P. Nonprescription drug-related problems and pharmacy interventions. Ann Pharmacother. 2001;35(11):1343–9. doi: 10.1345/aph.1A065. [DOI] [PubMed] [Google Scholar]
- 37.Hanson AL, DeMuth JE. Facilitators and barriers to pharmacists' participation in lifelong learning. Am J Pharm Educ. 1991;55(1):20–9. doi: 10.5688/aj710467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hanson AL, Bruskiewitz RH, DeMuth JE. Pharmacists' perceptions of facilitators and barriers to lifelong learning. Am J Pharm Educ. 2007;71(4) doi: 10.5688/aj710467. Article 67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Driesen A, Leemans L, Baert H, Laekeman G. Flemish community pharmacists' motivation and views related to continuing education. Pharm World Sci. 2005;27(6):447–52. doi: 10.1007/s11096-005-0950-7. [DOI] [PubMed] [Google Scholar]