Abstract
Background
Diabetes mellitus is one of the chronic diseases exploiting the largest number of telemedicine systems. Our research group has been involved since 1996 in two projects funded by the European Union proposing innovative architectures and services according to the best current medical practices and advances in the information technology area.
Method
We propose an enhanced architecture for telemedicine giving rise to a multitier application. The lower tier is represented by a mobile phone hosting the patient unit able to acquire data and provide first-level advice to the patient. The patient unit also facilitates interaction with the health care center, representing the higher tier, by automatically uploading data and receiving back any therapeutic plan supplied by the physician. On the patient's side the mobile phone exploits Bluetooth technology and therefore acts as a hub for a wireless network, possibly including several devices in addition to the glucometer.
Results
A new system architecture based on mobile technology is being used to implement several prototypes for assessing its functionality. A subsequent effort will be undertaken to exploit the new system within a pilot study for the follow-up of patients cared at a major hospital located in northern Italy.
Conclusion
We expect that the new architecture will enhance the interaction between patient and caring physician, simplifying and improving metabolic control. In addition to sending glycemic data to the caring center, we also plan to automatically download the therapeutic protocols provided by the physician to the insulin pump and collect data from multiple sensors.
Keywords: Bluetooth technology, mobile computing, multi access service, telemedicine
Introduction
Diabetes mellitus (DM) is one of the foremost chronic diseases in Western countries: the highest rate of diabetes prevalence is found in the North American region (9.2%), followed by the European region (8.4%).1 Several studies have shown that the majority of costs for DM management are related to hospitalization as a consequence of diabetes-related micro- and macrovascular complications. It is therefore becoming mandatory to define suitable programs in order to improve the overall disease management process. DM is also the chronic disease scoring the largest number of telecare and telemonitoring systems in the literature,2–4 with the goal of enabling patients to send data collected at home to a health care center (HCC) and letting care managers come up with prompt advice for them, thus improving their metabolic control.
Our research group has been involved since 1996 in two projects funded by the European Union proposing innovative telemedicine architectures and services according to the best current medical practices and advances in the information technology area. After a detailed description and discussion of the main features and drawbacks shown by the telemedicine systems developed in those previous projects, this article proposes a new architecture based on the mobile phone acting as a gateway for data and message exchange with the HCC.
The T-IDDM Project
The first project, named T-IDDM (1996–1999),5 was meant to accomplish the specific aims of allowing cost-effective monitoring of a large number of patients automating home data collection and training them in managing their insulin therapy. As shown in Figure 1, the T-IDDM service proposed in the project relied on an architecture consisting of two modules: the patient unit (PU) and the medical unit (MU). The PU is software installed on a personal computer (PC) located at the patient home, providing support in accomplishing the following tasks:
collecting data, either manually or automatically from the glucometer;
self-monitoring of blood glucose levels (BGL), suggesting insulin dose adjustments when needed; and
delivering monitoring data to the HCC.
Figure 1.
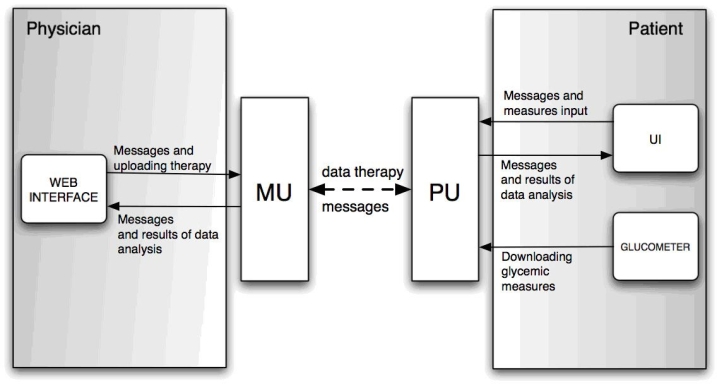
The T-IDDM system architecture.
The MU was available instead over the HCC intranet and consisted of a Web application integrating several functionalities, helping the physician in
visualizing and analyzing patients' data,
supporting his/her decision and therapy planning requirements, and
exchanging messages and/or therapeutic advices with his/her patients.
Furthermore, the MU was equipped with software accepting incoming point-to-point connections from PUs through standard modems for data, therapies, and messages exchange.
Communication between PU and MU was driven by the patient, who could send monitoring data to the MU periodically, e.g., every 7–10 days. The two units worked asynchronously, as it was not known a priori when data transfers took place. Although such architecture represented an interesting and advanced effort for improving glucose metabolic control by boosting more frequent contacts between physicians and patients, it also revealed some shortcomings, essentially because of limitations of the technologies available in those years. First, the patient needed a PC for performing self-monitoring (downloading data from the glucometer and consulting the local copy of his therapy protocol), as well as for any interaction with the HCC (uploading data to the MU, receiving therapy protocol updates, or exchanging messages). Second, because the PU application was running at a patient's home PC, keeping up with software updates was inherently difficult and time-consuming.
The M2DM Project
Some of the aforementioned drawbacks were overcome by the subsequent project, M2DM (2001–2003),6 centralizing in a Web service most of the functionalities spread previously between PU and MU. Data exchanged between physicians and patients remain almost the same (BGL measurements, therapies, and messages), but the new system makes additional communication facilities available to users, also integrating a customizable service for automatically notifying relevant events with text messaging, such as email or mobile phone short message service (SMS). The M2DM system has been developed on top of a multiaccess architecture integrating several communication technologies and devices such as the Web, client–server applications on PCs, specialized devices for data collection and transmission, and an interactive voice responder (IVR), as shown in Figure 2.
Figure 2.
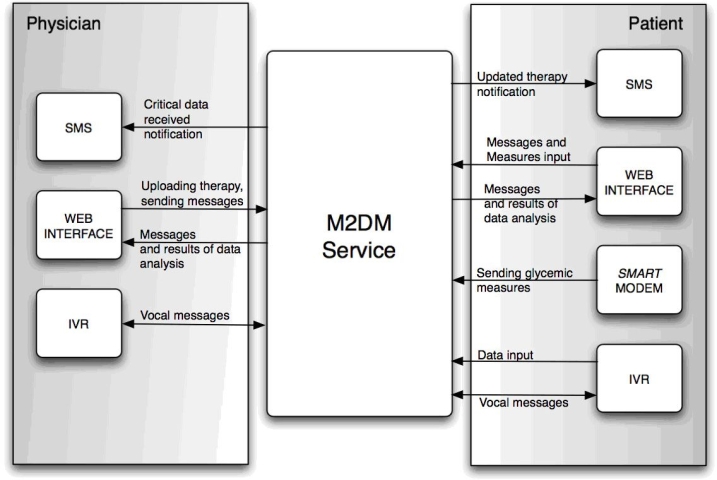
The M2DM system architecture.
From a technological viewpoint, each user or service access is mediated by a specialized software agent, and coordination of the agents' activities is planned by highly configurable middle-layer software. This middle layer may implement some of the overall application logic, for example the capability of scheduling automatic activities such as mail/SMS notifications or data analysis services, according to user profiles and service configuration. A typical scenario involves the patient using a smart modem periodically to send through a public switched telephone network (PSTN) line his BGL measurements taken through a glucometer at home. Data are received and stored in a central data base so that they can be analyzed in order to detect metabolic alterations and automatically generate alarms. The physician is notified of data reception and analysis results so that he/she may exploit the visualization and decision support tools integrated into the M2DM service for reviewing the patient's metabolic condition. The physician may also modify the therapy of a patient, who will be notified automatically about any change. Any alert (data reception, alarm generation, therapy modification, reading of a message, etc.) can be signaled to the recipient (patient or physician) as an SMS or as a text message saved into his/her own system mailbox where other messages from regular users are also delivered. Furthermore, in compliance with the multiaccess approach, messages can be read either through the Web or through the IVR system. The multiaccess approach showed some interesting advantages with respect to the previous architecture:
uploading data no longer requires a PC, as it may be accomplished with a phone line and a smart modem only;
users' interaction and communication become timelier by means of automatic reminders and notifications; and
access to some functionalities (data and messages exchange) may exploit different devices and technologies (Web, smart modems, and phones).
Need for an Enhanced Messaging System
Following a year of service, a survey has been conducted in order to assess the use patterns along with the level of acceptance and satisfaction perceived by users. As better described in a following section, the experiment was definitely seen as successful toward the establishment of tighter communication links among patients, their families, and doctors at the HCC, with the goal of improving the process of glycemic monitoring and regulation. This was witnessed by the many patients who asked us to continue upkeeping the service even after the official project was over. However, the most striking evidence arises from seeing that, on average, patients connected only three times per week, sending a total of 20,000 glucose readings with as few as 2000 insulin dosages, all input through the Web interface. This is probably because of the fact that despite the multimodal access provided by the system, the only ways it offered the uploading of glycemic readings acquired by means of a glucometer to the HCC relied on one of the following procedures:
downloading readings onto the patient's PC configured with Internet access, which relayed those data to the HCC over the Internet automatically;
coupling the glucometer directly with a dedicated modem able to send data through the HCC using a standard PSTN link; or
manual transcription of glycemic data through the system Web interface.
All three options were inherently inspired by a batch-style data processing model with the patient entering data into the system usually once per week,7 which turned out to be a limitation. Although all the devices on the market were equipped with an internal diary able to store several days of data samples, that way of interacting with the system spoiled the monitoring process either by increasing the possibility of losing data altogether or by sending obsolete data to the HCC well after the time they were acquired. This is bound to become a serious drawback, especially when a patient leaves his home setting for a vacation or a work trip, changing his food/exercise habits and needing a stricter supervision by the HCC, with the basic requirement of having a PC with an Internet connection or a PSTN not fulfilled.
Finally, even though the M2DM system was able to track the therapy assigned to the patient along with the control law for keeping glycemic levels within the desired range, this knowledge was provided as an informational support only and could not be applied to provide real-time advice to the patient.
A Mobile Architecture for Diabetes Managament
As mobile technology evolves, more and more devices appear on the market, exhibiting ever-increasing computational capabilities and offering the possibility of being customized by installing user-provided applications. Among mobile devices, cellular phones are rather ubiquitous, easy to use, and account for an inexpensive communication link able to exchange text and binary data from almost any part of a territory. Furthermore, the majority of cellular phones also provide support for applications complying with the J2ME™ platform. This is perhaps the most widespread standard available for writing and packaging mobile applications, also accounting for an easy integration with existing software libraries implemented in Java™. Thus, with the goal of overcoming all the aforementioned limitations and improving the interaction between patient and HCC, we decided to undertake a major effort in reshaping the whole system architecture by adding a mobility module that provides a new and more effective communication channel.
In fact, several ongoing projects already address the use of mobile devices with the goal of improving the treatment of patients affected by DM. Some of those projects are more focused toward coupling the mobile appliance with a glucometer, which may eventually become embedded within the same device.8 Other projects address instead the problem of improving patient awareness by focusing on data analysis and providing the patient with more comprehensive suggestions concerning therapy.9 Figure 3 illustrates the architecture we propose, which tries to complement both approaches and to be as broad as possible by pushing the message exchange capabilities available within the M2DM framework toward a mobile perspective. As shown in Figure 3, in addition to being used for uploading data to the HCC, receiving therapeutic plans, and exchanging warning and alert messages, the mobile phone also acts as a hub for a wireless network whose spokes are the data acquisition devices.
Figure 3.

New mobile architecture enhancements for M2DM.
According to our view, instead of being coupled physically, the mobile phone and the glucometer are kept as separate devices and communicate through a link based on the Bluetooth technology standard. Almost all glucometers available today on the market include a serial port through which data can be downloaded to a PC. However, instead of hardwiring the glucometer to the mobile phone, the former has been equipped with a custom-tailored Bluetooth board, thus enabling it to communicate with the latter.
While we were just planning to keep the glucometer as the only monitoring device during the first phase of the project, the adopted architecture has already opened up new scenarios where the mobile phone acts as a gateway, providing access to the Internet for a host of monitoring devices, building up a piconet centered around the patient. These devices may act as discrete data sources, such as the glucometer, the insulin pump, or a scale for measuring the patient weight at some predefined time intervals, as well as streaming data sources such as an electrocardiograph or a pulse oxymeter.
The Bluetooth interconnecting board is provided by STMicroelectronics and features a radio frequency module and an ARM7 processor. It is very compact and its size accounts for placing it on the bottom of the devices to be interconnected. Furthermore, in addition to implementing the algorithms needed for replicating data on the serial port of the device and exposing a Bluetooth serial port profile, the processor can be endowed with any custom logic. This may be useful for implementing security solutions controlling hand shaking and data exchange among devices, or for filtering algorithms which are especially useful for real-time streaming data sources.
Figure 4 illustrates in deeper detail the architecture of the system, emphasizing the communication paths between patient and HCC and pointing out the two main loops through which advice is conveyed. The mobile phone, which is supposed to stay always within a patient's reach, acts as the patient unit and hosts the front end application, providing access to the whole system. Each time the patient uses the glucometer, this application automatically acquires new glycemia readings using Bluetooth technology, stores data on the local diary, and performs a simple analysis, suggesting in real time the therapeutic actions according to the plan provided by the HCC. This interaction matches the small loop on the left side of Figure 4. The patient is then asked to revise those actions and acknowledge them so that they can be forwarded along with the readings to the HCC where more comprehensive checks are performed and the caring physician may eventually review the whole case. Whenever an exceptional event is noticed by the local unit, an SMS is sent automatically to the mobile phone of the caring physician so that he/she may be informed immediately. Finally, whenever the physician recognizes the need for a therapy change, he/she enters the new plan on the medical unit, which is later forwarded automatically to the patient's unit, along with any informational message he/she may have enclosed, as illustrated by the bigger loop shown in the bottom part of Figure 4, Figure 5 shows some sample screens collected on a mobile phone running the application.
Figure 4.
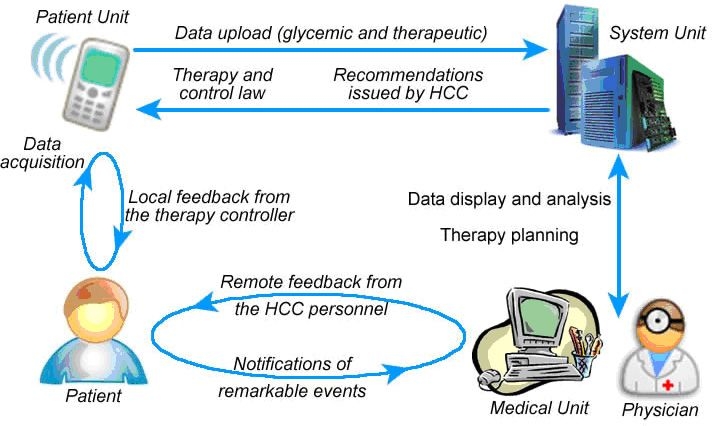
Communication paths between patient and HCC.
Figure 5.
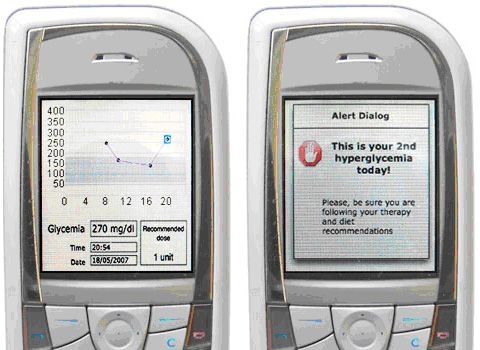
Screen shots of a mobile phone running a patient unit.
Results
During the last year of project funding an extensive evaluation of the service was performed in order to verify the effectiveness of the multiaccess approach. In Italy the evaluation involved 38 active and 30 control patients from two caring sites participating in the project: Policlinico San Matteo (PSM) caring for pediatric patients (16 active and 12 control) and Fondazione S. Maugeri (FSM) managing adult ones (22 active and 18 control). According to the project plan, each caring site appointed a single physician in charge of managing the patients involved in the evaluation. Dropout only occurred at the very beginning of the study and included 8 patients in the active group and 4 in the control one. The study considered outcomes related to six sections: organizational, economic, technical, usability, clinical, and quality of life. From organizational and economical points of view, the service proved to be very effective in optimizing the schedule, duration, and number of patient visits, thus helping in saving costs due to hospitalization and decreasing the number of working days lost.7 As a result, the clinical staff was able to concentrate most of their efforts on critical cases and still supervise the simplest ones remotely.
Technical evaluation of the service has been performed analyzing the service logs to extract data concerning the number and frequency of users' accesses and the total/average number of BGL measurements and insulin doses sent by patients to the HCC per week. The average access to the Web service was about 1.3 times per week per patient and 6.7 times per week per physician. Patients transferred about 20,000 BGL readings and 2000 insulin dosages. Detailed results of using the system in Italy are considered fully satisfactory after the exploitation phase. Table 1 reports the number of interactions to the service for physicians and patients either as Web visits or through all the access modes provided (i.e., modem, IVR, Web), whereas Table 2 shows BGL readings and insulin intakes recorded by patients using any access mode.
Table 1.
System Usage Evaluation Results
| Average number of web visits per week | Average number of interactions per week | |||
|---|---|---|---|---|
| FSM | PSM | FSM | PSM | |
| Patients | 1.40 (N = 16) | 1.21 (N = 14) | 3.79 (N = 16) | 2.77 (N = 14) |
| Physicians | 6.11 (N = 1) | 7.29 (N = 1) | 19.1 (N = 1) | 17.7 (N = 1) |
Table 2.
Number of Data Sent by Patients to Clinical Center Using a Smart Modem
| # BGL | # Insulin | |
|---|---|---|
| PSM | 6602 14 patients, 13 months | 454 14 patients, 13 months |
| 507.85 (42.15) average per month (SE) | ||
| FSM | 13995 16 patients, 13 months | 1653 16 patients, 13 months |
| 1090.31 (56.35) average per month (SE) |
The overall service usability perception was also very high. The highest level of acceptance was scored by the smart modem for data transmission, but results for the Web service were also very good, given that patients with different ages and cultural backgrounds were involved in the study.
Clinical evaluation was based on a comparison of the HbA1c course among active and control patients; results are shown in Table 3. Both active and control patients improved their metabolic control during the survey, but the improvement was far more statistically significant in active ones. The decrease of HbA1c was even more evident in patients showing values higher than 8% at the beginning of the study. Another interesting result is given by the number of hypo- and hyperglycemias measured at the beginning and at the end of the study. As reported in Table 4, in the last 4 months there was an increase in the percentage of normal values and a strong reduction in the number of hyperglycemias as compared to the first 4 months during the evaluation year.
Table 3.
HbA1c Measurements (% ± STD) at Regular Visits: V1 (First Visit at 0 Months), V3 (after 6 Months), and V5 (after 12 Months)
| Group | V1 | V3 | V5 | |
|---|---|---|---|---|
| FSM | Active (N = 15) | 8.40 ± 2.53 | 7.85 ± 1.51 | 7.75 ± 1.16a |
| Controls (N = 14) | 10.15 ± 3.25 | 9.35 ± 2.19 | 9.28 ± 2.34 | |
| PSM | Active (N = 13) | 8.52 ± 1.08 | 8.06 ± 0.64 | 8.30 ± 0.81 |
| Controls (N = 12) | 8.97 ± 1.54 | 8.47 ± 1.42 | 8.82 ± 1.10 |
The difference of means between V1 and V5 is statistically significant (p < 0.049, Wilcoxon signed-rank test).
Table 4.
Blood Glucose Distributions in Adults and Pediatric Patients at the Beginning and End of Study
| BGL<50 mg/dl | 50<BGL<300 mg/dl | BGL>300 mg/dl | |
|---|---|---|---|
| First 4 months | 1.49% | 68.36% | 30.14% |
| Last 4 months | 0.96% | 77.19% | 21.85% |
Discussion
This article described a service developed within two major projects for helping patients affected by DM in managing their disease and our undergoing efforts for improving the architecure. Although the evaluation of the former system provided suitable results, except for SMS notifications, any other communication could take place only through the Web or the IVR service, thus posing a serious limitation on its widespread availability. Mobile technologies available nowadays seem to be a promising solution to the problems that emerged during the two projects. Thus, in addition to discussing the success factors and drawbacks that emerged during the evaluation study, this article also illustrated a mobile architecture whose functionality is expected to be assessed through a forthcoming pilot study following up patients cared for at a major hospital located in northern Italy.
The new mobile architecture is aimed at supporting a true telemedicine system modeled after a multitier paradigm. Providing the patient with the most appropriate advice is fulfilled by an application implemented on a mobile phone without hindering continuous monitoring by the caring physician. We strongly believe that this approach is broader in perspective than many others,3,8–10 as it defines a generic architecture that supports a patient in managing diabetes autonomously while health care personnel still play key monitoring and control roles in the whole process. This is in line with the first and foremost goal we set forward to pursue, that is, to tighten the bidirectional link between the patient and the HCC, which sees the former sending glycemic data and the latter analyzing and reviewing those data, possibly providing adaptations for base therapy and control law. The need for improving the process of glycemic data collection in sight of better monitoring by the HCC is also witnessed by a survey11 disclosing that more than 60% of patients in Italy still rely entirely on paper for keeping track of their measurements and never attempt to download data from the acquisition device for any kind of processing.
Placing the control logic on a mobile device not only accounts for a more timely data transmission to the HCC, but also facilitates acquiring data from multiple sources, which may be extremely valuable in following up patients affected by chronic diseases, as well as improving a patient's context awareness. Research efforts12 already suggest the possibility of detecting hypoglycemic episodes during sleep by combining several physiological parameters and claim that similar approaches could also be adopted for detecting sudden infant death syndrome. Because of the latest Bluetooth standards, which are being updated to include a medical device profile that defines the requirements for interconnecting medical and health and fitness devices, we expect that more and more devices in this area will be able to exchange data with a mobile phone in the short term. During the first revision of the project based on mobile technology, we had planned to interact with a glucometer only. However, our midterm vision already sees an insulin pump as a candidate device so that any change in a therapy plan made by a physician, upon patient's acknowledgment, may instantly become operational on the pump, with even more complex scenarios such as the aforementioned ones to follow.
Abbreviations
- BGL
blood glucose levels
- DM
diabetes mellitus
- FSM
Fondazione S. Maugeri
- HCC
health care center
- IVR
interactive voice responder
- MU
medical unit
- PC
personal computer
- PSM
Policlinico San Matteo
- PSTN
public switched telephone network
- PU
patient unit
- SMS
short message service
References
- 1.Diabetes prevalence. International Diabetes Federation [accessed 2007 May 28]. Available from: http://www.idf.org/home/index.cfm?node=264.
- 2.Ahring KK, Ahring JP, Joyce C, Farid NR. Telephone modem access improves diabetes control in those with insulin-requiring diabetes. Diabetes Care. 1992;15(8):971–975. doi: 10.2337/diacare.15.8.971. [DOI] [PubMed] [Google Scholar]
- 3.Shea S, Starren J, Weinstock RS, Knudson PE, Teresi J, Holmes D, Palmas W, Field L, Goland R, Tuck C, Hripcsak G, Capps L, Liss D. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) Project: rationale and design. J Am Med Inform Assoc. 2002 Jan–Feb;9(1):49–62. doi: 10.1136/jamia.2002.0090049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomez EJ, Hernando ME, Garcia A, Del Pozo F, Cermeno J, Corcoy R, Brugues E, De Leiva A. Telemedicine as a tool for intensive management of diabetes: the DIABTel experience. Comput Methods Programs Biomed. 2002 Aug;69(2):163–177. doi: 10.1016/s0169-2607(02)00039-1. [DOI] [PubMed] [Google Scholar]
- 5.Bellazzi R, Larizza C, Montani S, Riva A, Stefanelli M, d'Annunzio G, Lorini R, Gomez EJ, Hernando E, Brugues E, Cermeno J, Corcoy R, de Leiva A, Cobelli C, Nucci G, Del Prato S, Maran A, Kilkki E, Tuominen J. A telemedicine support for diabetes management: the T-IDDM project. Comput Methods Programs Biomed. 2002 Aug;69(2):147–161. doi: 10.1016/s0169-2607(02)00038-x. [DOI] [PubMed] [Google Scholar]
- 6.Bellazzi R, Arcelloni M, Bensa G, Blankenfeld H, Brugués E, Carson E, Cobelli C, Cramp D, D'Annunzio G, De Cata P, De Leiva A, Deutsch T, Fratino P, Gazzaruso C, Garcìa A, Gergely T, Gómez E, Harvey F, Ferrari P, Hernando E, Boulos MK, Larizza C, Ludekke H, Maran A, Nucci G, Pennati C, Ramat S, Roudsari A, Rigla M, Stefanelli M. Design, methods and evaluation directions of a multi-access service for the management of diabetes mellitus patients. Diabetes Technol. Ther. 2003;5(4):621–629. doi: 10.1089/152091503322250640. [DOI] [PubMed] [Google Scholar]
- 7.Larizza C, Bellazzi R, Stefanelli M, Ferrari P, De Cata P, Gazzaruso C, Fratino P, D'Annunzio G, Hernando E, Gomez EJ. The M2DM Project–the experience of two Italian clinical sites with clinical evaluation of a multi-access service for the management of diabetes mellitus patients. Methods Inf Med. 2006;45(1):79–84. [PubMed] [Google Scholar]
- 8.Carroll AE, Marrero DG, Downs SM. The HealthPia GlucoPack Diabetes phone: a usability study. Diabetes Technol Ther. 2007 Apr;9(2):158–164. doi: 10.1089/dia.2006.0002. [DOI] [PubMed] [Google Scholar]
- 9. Roche Accu-Check Pocket Compass [accessed 2007 May 28]. Available from: http://www.accuchek.it/it/rewrite/content/it_IT/40.60.30:30/article/ACCM_general_article_3755.htm.
- 10.Lee RG, Hsiao CC, Chen KC, Liu MH. An intelligent diabetes mobile care system with alert mechanism. Biomed Eng Appl Basis Commun. 2005;17(4):186–192. [Google Scholar]
- 11. Progetto Diabete [accessed 2007 May 28]. Available from: http://www.progettodiabete.org/indice_ie1000.html?sondaggi/2006/polling159.html.
- 12.Nguyen HT, Ghevondian N, Jones T. Neural-network detection of hypoglycemic episodes in children with type 1 diabetes using physiological parameters. 28th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; Aug 31–Sep 3; New York. 2006. pp. 6053–6056. [DOI] [PubMed] [Google Scholar]


