Abstract
Self-care is essential in chronic disease management; however, adherence to self-care plans is often far from optimal. Advances in technology can facilitate self-management of chronic disease through patient empowerment and timely feedback. The Confidant system is a novel wireless remote patient monitoring and response system, centered around mobile phone technology, that translates scientifically supported knowledge for chronic disease management into action by providing easily followed daily coaching using the patient's own data. Daily provision of interactive, informative messages removes the burdens of recall, record keeping, decision making, scheduling, and data analysis. A pilot-controlled clinical trial evaluated the feasibility and efficacy of the Confidant system in the management of type 2 diabetes in 15 patients utilizing the cell-phone technology and 15 individuals in a control group (standard type 2 diabetes care). The study demonstrated improved levels of glycosylated hemoglobin, positive changes in diabetes management self-efficacy, and diabetes self-care activities among intervention group patients. A larger trial is now in development to demonstrate the clinical benefit of using the Confidant system among type 2 diabetic patients. This article describes the novel technology and applications of the Confidant system.
Keywords: cell-phone technology, chronic disease management, clinical practice, diabetes, self-care
Introduction
Long a disease of great public health importance, type 2 diabetes is now considered epidemic in both children and adults in the United States, due largely to an underlying epidemic of obesity.1,2 In the United States, it affects 18.2 million people or 6.3% of the population.3 From 1996 to 2001, diabetes has climbed from the seventh to the sixth leading cause of death,4 with an increasing number of deaths occurring per year across age and race categories.5–11 Estimated health care expenditures associated with diabetes include $91.8 billion in direct and $39.8 billion in indirect costs as of 2002.12 The cause of such high morbidity, mortality, and costs can be mostly attributed to long-term, chronic diabetes-related complications, such as renal disease, coronary heart disease, blindness, and neuropathy.13
Lifestyle practices and adherence to prescribed interventions have enormous potential to ameliorate the course of chronic diseases. Rich and colleagues14–16 and others17,18 have shown the clinical and financial benefits of a case management system in congestive heart failure. Similar benefits have been seen with case management in other chronic diseases, such as asthma19,20 and diabetes.21,22 The most cost-effective approach to enhanced chronic disease management is improved self-care.23,24 Chronic diseases associated with unhealthy behavior are prevalent, and medical care is becoming more participatory. In addition, new technology expands what people can do for themselves.25 Given the costs of care, self-care is becoming the disease management option of choice; however, empowering patients to engage in high-quality self-management has been a largely elusive goal to date.
The prevention of type 2 diabetes complications is substantially dependent on diabetes control. According to the American Diabetes Association, diabetes self-management is an integral component of diabetes care.26 Improved glycemic control (hemoglobin A1c <7%) has been shown to minimize microvascular complications by decreasing the rates of nephropathy, retinopathy, neuropathy, and cardiovascular disease.27 Blood glucose can often be controlled by following a careful diet and exercise program, losing excess weight, and taking oral medication.26 In addition, self-monitoring of blood glucose is imperative in diabetes self-care; these data allow for adjustment in therapy to meet glycemic goals.27 Maintaining a blood pressure of 130/80 or less can reduce cardiovascular disease by approximately 33 to 50% and can reduce microvascular disease (eye, kidney, and nerve disease) by approximately 33%.26 Lifestyle modification (exercise, diet control, weight loss, smoking cessation) and nutritional counseling, as well as pharmacologic interventions, can lower blood pressure levels as part of a diabetes self-management plan. The same interventions can help manage cholesterol and lipid levels.
Despite the benefits of adhering to a disease management program for diabetes, national compliance to such programs is not optimal. In 2000, the levels of preventive-care practices among diabetes patients were lower than the national objectives for 2010.28 A large-scale study determined that half (51.5%) of diabetes patients “always” self-tested as recommended, and only 11.8% completely adhered to a recommended diet. Because self-efficacy is considered a significant predictor of adherence to management plans,29,30 increasing confidence in self-managing diabetes may be necessary to improve diabetes self-care adherence.
Tailored Diabetes Disease Management
Several tailored, technologically advanced disease management programs for diabetes have been studied and met with moderate success. Glasgow et al.31 compared an online peer support group and an information-only group (with computer access to relevant articles) to a tailored self-management training (TSM) group that worked with an online “coach” who tailored strategies for each individual to reach dietary goals. Patients could also enter and receive graphical feedback on their blood glucose levels for different times of the day. All groups received Internet-based automated goal setting based on assessment results, identification of barriers and supports, updated diabetes information, and quarterly follow-ups, which produced improvements on behavioral, psychosocial, and biological outcomes from baseline. There was no significant difference between groups, although trends favoring TSM on several outcomes were apparent. Tailoring methods differed somewhat in the German M2DM project, which successfully implemented telemonitoring for physicians; telecare (including message exchange between doctor and patient and physician-supervised care for self-management); remote information access, which allowed providers and patients access to all information in the clinical database; and knowledge management and decision support through tailored alarms and reminders transmitted through cellular phones or email for both providers and patients. Patients participating in the program showed clinical improvement after 6 months of use.32
Tailored reinforcement was also used by Durso et al.,33 who implemented the Personal Diabetes Management Program (PDMP), using cellular phones and the Internet. At predetermined times, the PDMP contacted patients with tailored interactive recorded messages (based on individual needs), which included reminders for performing self-care activities, prompting a call to the provider for medical advice if any symptoms or problems occur, providing health education, and recording personal health data, accomplished by entering the values on a telephone keypad. Data were transferred to a Web site to be reviewed by the provider. A nurse reviewed data provided by the patients and contacted them with feedback and diabetes management changes, if necessary. All participants reported increased awareness of impact of diet, activity, and medication on their diabetes management and some increased daily physical activity levels. Although results were encouraging, several limitations were noted, such as brevity of the study, small number of patients (7), self-reported data, and lack of a control group.
There has been increasing interest in the potential of mobile technologies, such as personal assistants and cell phones, to enhance self-management.34 Gammon and co-workers35 showed that a mobile system used to send child blood glucose monitoring data to parents was integrated into their daily activities and reduced parental anxiety. Mobile technologies are able to fulfill many of the same educational and interactive behavioral goals as desktop computers, but because of their ability to use “push” strategies, their unobtrusive nature, and their potential for integration into individual lifestyles and habits, mobile technologies may show greater appeal, feasibility, and utility for patients compared to desktop programs. While much research is needed on the development and testing of mobile technologies, there is agreement that they have great promise to facilitate self-management behaviors.
Description of Confidant Technology
The Confidant system is a novel wireless remote patient monitoring and response system, centered around mobile phone technology, that translates scientifically supported knowledge for chronic disease management into action by providing easily followed daily coaching using the patient's own data. Daily provision of interactive, informative messages removes the burdens of recall, record keeping, scheduling, and data analysis.
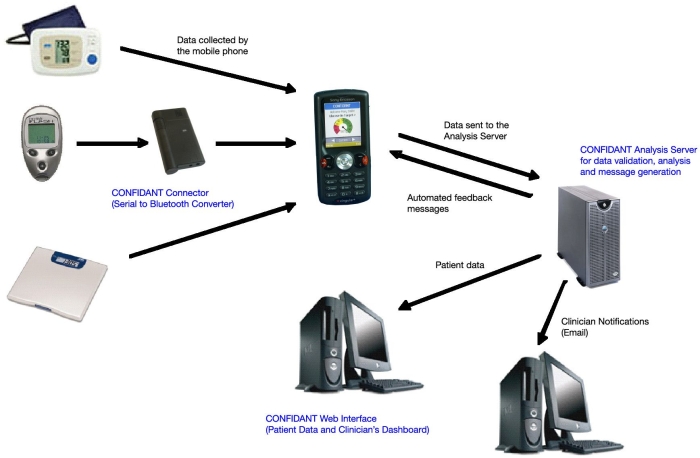
The Confidant system collects data from a range of supported home-monitoring devices. Data are collected from the supported devices and sent to a central database server, using standard wireless technologies. Upon receipt of newly submitted patient data, the Confidant server software will generate and send one or more feedback messages directly to the patient's cell phone. The feedback messages are selected by the system based on the patient's currently submitted and recent historic data.
Confidant currently supports several models of glucose meters, a noninvasive blood pressure cuff, and a weight scale. Additional functions include manual entry of daily step count and display of customized questions and collection of patient responses.
The Confidant system consists of two software modules—the collector and the server—and a single hardware module (the connector), which is used to communicate with monitoring devices through a serial data interface.
The Confidant connector is a proprietary hardware component that connects to a supported measurement device using a serial data cable. Data received from the measuring device are converted to the Bluetooth protocol and transmitted wirelessly to the patient's cell phone.
The collector module is a software program that runs on the patient's cell phone. It receives data from the connector (or directly from Blue Tooth-enabled home-monitoring devices) and transmits it to the server over a cellular data (General Packet Radio Service) network. The collector also provides the user interface for operating the system and viewing graphical and text responses sent from the server.
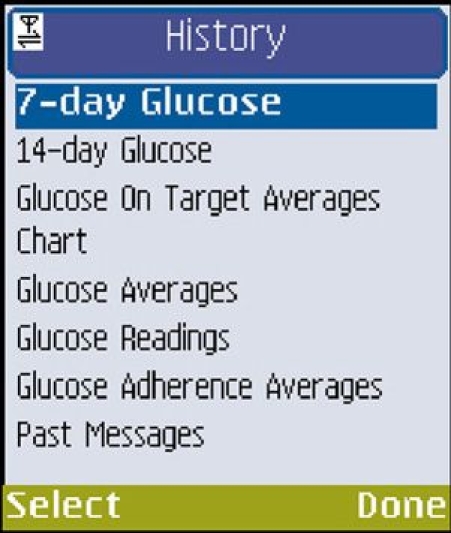
The server module is a software program that runs on standard Web server hardware. The server module receives data sent to it by the collector module and generates customized responses in both graphical and text forms (Figure 1). The Confidant server has an Internet (World Wide Web) user interface. Authorized users with a user name and password may view measurement data collected from the medical devices. The patient also has the ability to review prior messages received from the system. Combining these two elements allows the patient to better understand how well they are self-managing their disease.
Figure 1.
Confidant system.
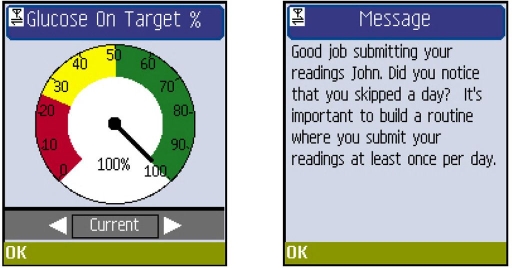
Messages from the Confidant server to the user are normally sent to the mobile phone as a response to data collection so that each time the user sends collected data to the server, s/he receives a message back within seconds based partially on that data. Messages from the Confidant server to the doctor are sent as an email to an address configured for him/her (note that because many mobile phones take email, the email may be delivered to a phone with this feature or to a more traditional email client) (Figures 2 and 3).
Figure 2.
Examples of automated feedback.
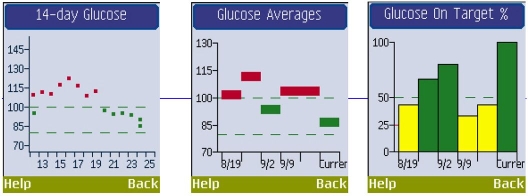
Figure 3.
Examples of summarized patient-specific data.
All data storage and access conform to U.S. Health Insurance Portability and Accountability Act regulations concerning the privacy and protection of data.
The Evaluation
Phase I of the evaluation, called Novel Interactive Cell-phone technology for Health Enhancement, was a controlled clinical trial evaluating the feasibility and efficacy of the Confidant system in the management of type 2 diabetes.36 Phase I evaluated this innovative technology in a community health center setting. As described previously, 30 subjects participated in the study: 15 in the group who used cell-phone technology (intervention) and 15 in the control group utilizing standard care for type 2 diabetes. The intervention phase was 3 months long. Phase I was able to establish levels of compliance using the Confidant system and reasons for any problems; satisfaction with the technology based on clinician and patient feedback; and utility of the Confidant system in enhancing diabetes management based on improved levels of glycosylated hemoglobin, positive changes in diabetes management self-efficacy, and diabetes self-care activities among participating patients. Because phase I was pivotal in establishing feasibility and utility of the Confidant system, all the necessary improvements were done to the system in preparation for a phase II trial.
Improvements to the Confidant System
In response to results of the phase I study and in preparation for a phase II trial, Confidant Inc. has made modifications and additions to the system. Table 1 outlines problems identified in the system through phase I paired with changes that have now been made to the technology and associated procedures.
Table 1.
Improvements to the Confidant System
| Problem areas identified by phase I | Improvements in the Confidant system |
|---|---|
|
|
|
|
|
|
|
|
The phase II trial also has the following quality control features built into the design of the intervention. (1) Problem solving of technological issues: patient and clinician guides to using the system, a toll-free number to a technician available at convenient times to patients and clinicians 7 days a week, and a Web site with information for the Confidant system are provided. (2) Clinician–patient interaction: Confidant's server has always had a Web-based interface allowing the clinician to set patient regimens, reminders, and threshold values for caregiver alerts. A new practice management component (the clinician's dashboard) has been added that provides clinicians with a short list of “problem patients.” The dashboard can be customized by the clinician to display patients that are either noncompliant in their self-management or have readings that are consistently outside of preset thresholds. This allows a clinician to quickly discover the few patients that require a more active intervention. By identifying patients that have not been submitting data on a regular basis, the dashboard will also help identify patients that may be experiencing technical problems. (3) Interaction between Confidant and patients: When notified by the clinician, Confidant staff will contact patients who have been identified as possibly having technical problems. (4) Interaction between Confidant staff and clinicians: Confidant staff will be in ongoing communication with participating clinicians regarding problem solving for any problems or concerns that arise with the system. (5) Data quality: Confidant staff will conduct data checks on uploaded data to validate it and make appropriate changes.
In summary, the aim of this technology is to enable the population to benefit from advice tailored specifically to them, without the inconvenience and time constraints involved in personal disease management counseling. Participants utilizing Confidant technology are provided with information about changes that can be made to improve their diabetes management and receive tailored information based on information received from the Confidant system. Participants' ability to modify their health behaviors has the potential to be enhanced significantly by reducing their risk of diabetes-related complications. The impact of the improvements made in the technology will be examined in a phase II clinical trial now in development.
Abbreviations
- PDMP
Personal Diabetes Management Program
- TSM
tailored self-management training
References
- 1.Bonow RO, Gheorghiade M. The diabetes epidemic: a national and global crisis. Am J Med. 2004;116:2S–10S. doi: 10.1016/j.amjmed.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 2.Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin North Am. 2003;32:805–822. doi: 10.1016/s0889-8529(03)00071-9. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2003. Atlanta (GA): U.S: Department of Health and Human Services, Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 4.Arias E, Anderson RN, Kung HC, Murphy SL, Kochanek HD. Deaths: final data for 2001. Natl Vital Stat Rep. 2003;52:1–115. [PubMed] [Google Scholar]
- 5.Harris MI, Flegal KM, Cowie CC, Eberhardt MS, Goldstein DE, Little RR, Wiedmeyer HM, Byrd-Holt DD. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988-1994. Diabetes Care. 1998;21:518–524. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 6.Mokdad AH, Ford ES, Bowman BA, Nelson DE, Engelgau MM, Vinicor F, Marks JS. Diabetes trends in the U.S.: 1990-1998. Diabetes Care. 2000;23:1278–1283. doi: 10.2337/diacare.23.9.1278. [DOI] [PubMed] [Google Scholar]
- 7.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–2000. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 8.Mokdad AH, Ford ES, Bowman BA, Nelson DE, Engelgau MM, Vinicor F, Marks JS. The continuing increase of diabetes in the US. Diabetes Care. 2001;24:412. doi: 10.2337/diacare.24.2.412. [DOI] [PubMed] [Google Scholar]
- 9.CDC. The burden of heart disease, stroke, cancer, and diabetes. United States. 2002 [Google Scholar]
- 10.Engelgau MM, Geiss LS. The burden of diabetes mellitus. In: Leahy JL, Clark NG, Cefalu WT, editors. Medical management of diabetes mellitus. New York: Marcel Dekker; 2000. pp. 1–17. [Google Scholar]
- 11.CDC. Diabetes Public Health Resource [accessed 2007 Sep 28] Available at: http://www.cdc.gov/health/diabetes.htm.
- 12.Hogan P, Dall T, Nikolov P. American Diabetes Association. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26:917–932. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 13.Shea S, Starren J, Weinstock RS, Knudson PE, Teresi J, Holmes D, Palmas W, Field L, Goland R, Tuck C, Hripcsak G, Capps L, Liss D. Columbia University's Informatics for Diabetes Education and Telemedicine (IDEATel) Project: rationale and design. Am Med Inform Assoc. 2002;9:49–62. doi: 10.1136/jamia.2002.0090049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rich MW. Management of heart failure in the elderly. Heart Fail Rev. 2002;7:89–97. doi: 10.1023/a:1013706023974. [DOI] [PubMed] [Google Scholar]
- 15.Rich MW, Beckham V, Wittenberg C, Leven CL, Freedland KE, Carney RM. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med. 1995;333:1190–1195. doi: 10.1056/NEJM199511023331806. [DOI] [PubMed] [Google Scholar]
- 16.Rich M, Nease R. Cost-effectiveness analysis in clinical practice: the case of heart failure. Arch Intern Med. 1999;159:1690–1700. doi: 10.1001/archinte.159.15.1690. [DOI] [PubMed] [Google Scholar]
- 17.Eliaszadeh P, Yarmohammadi H, Nawaz H, Boukhalil J, Katz D. Congestive heart failure case management: a fiscal analysis. Dis Manage. 2001;4:25–32. [Google Scholar]
- 18.Balinsky W, Muennig P. The costs and outcomes of multifaceted interventions designed to improve the care of congestive heart failure in the inpatient setting: a review of the literature. Med Care Res Rev. 2003;60:275–293. doi: 10.1177/1077558703254697. [DOI] [PubMed] [Google Scholar]
- 19.Schermer TR, Thoonen BP, van den Boom G, Akkermans RP, Grol RP, Folgering HT, van Weel C, van Schayck CP. Randomized controlled economic evaluation of asthma self-management in primary health care. Am J Respir Crit Care Med. 2002;166:1062–1072. doi: 10.1164/rccm.2105116. [DOI] [PubMed] [Google Scholar]
- 20.Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, Bauman A, Hensley MJ, Walters EH. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev. 2003:1. doi: 10.1002/14651858.CD001117. [DOI] [PubMed] [Google Scholar]
- 21.Banister NA, Jastrow ST, Hodges V, Loop R, Gillham MB. Diabetes self-management training program in a community clinic improves patient outcomes at modest cost. J Am Diet Assoc. 2004;104:807–810. doi: 10.1016/j.jada.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 22.Cranor CW, Bunting BA, Christensen DB. The Asheville Project: long-term clinical and economic outcomes of a community pharmacy diabetes care program. J Am Pharm Assoc (Wash) 2003;43:173–184. doi: 10.1331/108658003321480713. [DOI] [PubMed] [Google Scholar]
- 23.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288:2469–2475. doi: 10.1001/jama.288.19.2469. [DOI] [PubMed] [Google Scholar]
- 24.Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, Gonzalez VM, Laurent DD, Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care. 2001;39:1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Shore MF. Empowering individuals as carers of their own health. World Hosp Health Serv. 2001;37:12–16. 33, 35. [PubMed] [Google Scholar]
- 26.American Diabetes Association. National diabetes fact sheet [accessed 2007 Sep 28] Available from: http://www.diabetes.org/diabetes-statistics/national-diabetes-fact-sheet.jsp.
- 27.American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003;26:S33–S50. doi: 10.2337/diacare.26.2007.s33. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Disease Control Prevention (CDC) Levels of diabetes-related preventive care practices–United States, 1997-1999. MMWR Morb Mortal Wkly Rep. 2000;49:954–958. [PubMed] [Google Scholar]
- 29.Kavanagh DJ, Gooley S, Wilson PH. Prediction of adherence and control in diabetes. J Behav Med. 1993;16:509–522. doi: 10.1007/BF00844820. [DOI] [PubMed] [Google Scholar]
- 30.McCaul KD, Glasgow RE, Schafer LC. Diabetes regimen behaviors. Predicting adherence. Med Care. 1987;25:868–881. [PubMed] [Google Scholar]
- 31.Glasgow RE, Boles SM, McKay HG, Feli EG, Barrera M., Jr The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med. 2003;36:410–419. doi: 10.1016/s0091-7435(02)00056-7. [DOI] [PubMed] [Google Scholar]
- 32.Bellazzi R, Arcelloni M, Bensa G, Blankenfeld H, Bruges E, Carson W. Design, methods, and evaluation directions of a multi-access service for the management of diabetes mellitus patients. Diabetes Technol Ther. 2003;5:621–629. doi: 10.1089/152091503322250640. [DOI] [PubMed] [Google Scholar]
- 33.Durso SC, Wendel I, Letzt AM, Lefkowitz J, Kaseman DF, Seifert RF. Older adults using cellular telephones for diabetes management: a pilot study. Medsurg Nurs. 2003;12:313–317. [PubMed] [Google Scholar]
- 34.Tufano JT, Karras BT. Mobile eHealth interventions for obesity: a timely opportunity to leverage convergence trends. J Med Internet Res. 2005;7:e58. doi: 10.2196/jmir.7.5.e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gammon D, Arsand E, Walseth OA, Andersson N, Jenssen M, Taylor T. Parent-child interaction using a mobile and wireless system for blood glucose monitoring. J Med Internet Res. 2005;7:e57. doi: 10.2196/jmir.7.5.e57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self-management: the NICHE pilot study. J Eval Clin Prac. 2007 doi: 10.1111/j.1365-2753.2007.00881.x. In press. [DOI] [PubMed] [Google Scholar]