Abstract
Background
Little information is available describing how to implement a disease registry from an electronic patient record system. The aim of this report is to describe the technology, methods, and utility of a diabetes registry populated by the Veterans Health Information Systems Architecture (VistA), which underlies the computerized patient record system of the Veterans Health Administration (VHA) in Veteran Affairs Integrated Service Network 10 (VISN 10).
Methods
VISN 10 data from VistA were mapped to a relational SQL-based data system using KB_SQL software. Operational definitions for diabetes, active clinical management, and responsible providers were used to create views of patient-level data in the diabetes registry. Query Analyzer was used to access the data views directly. Semicustomizable reports were created by linking the diabetes registry to a Web page using Microsoft asp.net2. A retrospective observational study design was used to analyze trends in the process of care and outcomes.
Results
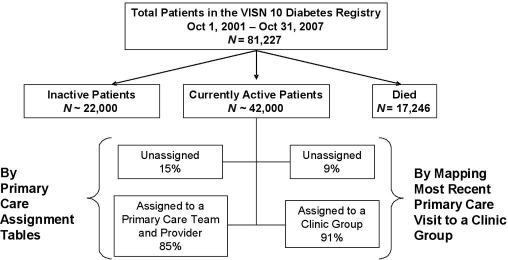
Since October 2001, 81,227 patients with diabetes have enrolled in VISN 10: approximately 42,000 are currently under active management by VISN 10 providers. By tracking primary care visits, we assigned 91% to a clinic group responsible for diabetes care. In the Cleveland Veterans Affairs Medical Center (VAMC), the frequency of mean annual hemoglobin A1c levels ≥9% has declined significantly over 5 years. Almost 4000 patients have been seen in diabetes intervention programs in the Cleveland VAMC over the past 4 years.
Conclusions
A diabetes registry can be populated from the database underlying the VHA electronic patient record database system and linked to Web-based and ad hoc queries useful for quality improvement.
Keywords: quality of health care, diabetes mellitus, computerized medical records systems
Background
In its simplest form, a disease registry is a roster of patients who share a particular disease, plus pertinent clinical information. Examples include the Surveillance Epidemiology and End Results and the United States Renal Data System registries of U.S. patients with cancer or end-stage renal disease, respectively.1,2 These registries are populated by data from standardized forms filled out by clinical providers. They provide information to inform policy decisions and provide data for research. An alternative use for a disease registry is to assist continuous quality improvement in the care of patients with chronic disease.3,4 For this purpose, manual entry of standardized information is cost prohibitive. The most efficient method to populate such a registry is to glean information from the clinical encounters and data captured within an electronic medical record.5 To assist quality improvement, specific information is needed. First, the registry must be able to accurately identify patients who have the disease. Second, the registry must be able to distinguish the provider responsible for management of the patient with the disease of interest, even if the responsible provider changes across time. Third, the registry must be able to distinguish patients who are “active” in the practice from those who no longer receive care from the practice. Fourth, reports from the registry should be easily accessible to the providers most responsible for patient outcomes. It is characteristic of high-performing systems that feedback is closely coupled to actions.6 Fifth, reports from a registry should be useful for implementing action plans to improve patient care, such as organizing group interventions or creating customized patient outreach. Finally, a registry should be able to inform management by tracking trends that affect resource needs.
Despite the potential of chronic disease registries to aid quality improvement, there is little information as to how to implement a disease registry populated from an electronic patient record. The Department of Veterans Affairs (VA) health care system has a comprehensive electronic patient record for inpatient and outpatient care called the Computerized Patient Record System (CPRS). The graphical user interface of CPRS enables users to access individual patient records, one at a time. CPRS supports medical documentation, physician order entry, outpatient pharmacy, imaging, laboratory, and other ancillary test records. It is essentially a paperless medical record that spans the continuum of care, from inpatient to outpatient, within the Veterans Health Administration (VHA) health care system. Underlying CPRS is the Veterans Health Information Systems and Technology Architecture (VistA), a hierarchical database system based on VA FileMan, a database management program used to access and manage VistA data.7 VA FileMan uses Massachusetts General Hospital Utility Multi-Programming System programming language.8 Although VistA, accessed through CPRS, has proved to be remarkably successful in supporting the day-to-day care of the individual patient, it has deficiencies in assembling and reporting aggregate patient data. This article describes our experience using VistA to populate a diabetes registry designed to be useful in improving patient care within the Louis Stokes Cleveland Department of Veterans Affairs Medical Center (VAMC) and its affiliated facilities and clinics.
Methods
Setting
The Cleveland VAMC currently serves approximately 90,000 individual veterans in northeast Ohio for inpatient and outpatient care. Primary care for the Cleveland VAMC is delivered through 12 community-based and 2 facility-based outpatient clinics. The Cleveland VAMC is contained within VA Integrated Service Network 10 (VISN 10), which covers all VHA services delivered to approximately 200,000 veterans within the state of Ohio. Each patient within the VISN 10 system may be enrolled in one to five sites (Cleveland, Cincinnati, Columbus, Dayton, or Chillicothe). Patients in VISN 10 are assigned to a primary care team/clinic and primary care provider. As an integrated health care system, the VHA pharmacy dispenses outpatient medications prescribed by VHA providers via a computerized order entry system, and outpatient records are stored within VistA. Dates of patients' death are recorded within the VISN 10 VistA database by periodic uploading of the Beneficiary Identification Record Locator Sub-System Death Files maintained by the Department of Veterans Affairs.9
VISN 10 Information Resources Management has mapped most data elements in VistA to an SQL database system, using the commercial software KB_SQL.10 This data transfer takes place on a nightly basis for most data elements. Weekly, the tables of clinical encounters and laboratory test results are completely refreshed for the past 12-month period in the SQL database system. The SQL database system is a relational database, using the unique patient identifier as the primary key, or linking variable.
This report, which includes analyses of patients who were exposed to quality improvement programs (described later) and glycemic outcomes, was approved by the Institutional Review Board of the Cleveland VAMC.
Diabetes Registry
A single base table in the diabetes registry contains the set of unique identifiers for patients in VISN 10 who meet criteria for diabetes, according to operational definitions (Table 1). This table is refreshed on a nightly basis by running a stored procedure of programming code against the SQL database system mapped from VistA. Thus, patients meeting criteria for having diabetes are added on a daily basis. Linked data for each patient in the base table are drawn from the SQL database as “views.” The views exist as virtual tables within the diabetes registry. One advantage of views, as opposed to physical tables, is that the integrity of the SQL database remains secure.
Table 1.
Operational Definitions for the VISN 10 Diabetes Registry
| Step 1: Define patients with diabetes mellitus in VISN 10a | |
| From October 1, 2001 to present, the patient had any combination of ICD-9-CM diagnosis codes (250.xx, 357.2, 362.0, 366.41) on at least three separate dates of clinical encounters | |
| or | |
| From October 1, 2001 to present, the patient had a diabetes-specific medicationb dispensed from a VISN 10 pharmacy on at least two separate dates | |
| Step 2: Define active patients versus not active patients with diabetes | |
| Active patients | Not active patients |
| Date of death = null and at least one of two conditions met: | If conditions for active are not met, then patient is not active |
| 1. The patient had a primary care clinic visit within the past 18 months | |
| or | |
| 2. The patient had a diabetes-specific medicationb dispensed from a VISN 10 pharmacy within the past 18 months | |
| Step 3: Define the clinic group most responsible for diabetes care for each active patient | |
| Active patients | |
| Find the most recent primary care clinic visit within the past 18 months. Based on the location of the visit, assign the patient to: | |
| Site (a mutually exclusive list of five VHA sites in Ohio) | |
| Chillicothe | |
| Cincinnati | |
| Cleveland | |
| Dayton | |
| Columbus | |
| Clinic group (a subset of clinics within each site) | |
| If the patient has no primary care clinic visits within the past 18 months, then classify as unassigned | |
VISN 10 is the VA Integrated Service Network 10.
Diabetes-specific medications are any sulfonylurea, biguanide, thiazolidenedione, metiglinide, α-glucosidase inhibitor, insulin, or glucose meter test strips.
The views can be treated as relational database tables for ad hoc queries using the Query Analyzer tool. New views can be added, or revised, by changing the programming defining the view. Programming logic is also used to derive new data fields, or attributes, from the linked data. For example, a view defines and selects the date and value of the “most recent hemoglobin A1c (HbA1c) test” for each patient from the laboratory table in the SQL relational database or defines whether the patient meets criteria for being an “active” patient in the clinical practice (yes/no). Adding such derived variables to a view facilitates rapid reporting for standardized queries. The views also contain the programming logic that helps clean and standardize the data elements mapped from VistA. For example, the HbA1c laboratory test is named by several possible character strings and numeric codes within VISN 10. All possible names or codes must be specified within the stored procedure to ensure complete capture of test results.
In VISN 10, patients are assigned to a primary care provider and clinic: the management of diabetes is considered to be the responsibility of primary care. However, the assignment of patients to a primary care provider requires manual data entry and may lag behind actual clinic care. Therefore, a system to track individual patients by past clinic visits was designed: the algorithm searches for the most recent clinic visit meeting criteria for being a definite, or likely, primary care visit. Based on the location of the clinic encounter, the patient is assigned to the clinic group (Table 1).
Ad Hoc Longitudinal Analyses
We used ad hoc longitudinal analyses to assess the reach and effectiveness of special programs to improve diabetes outcomes. The views contained within the diabetes registry are accessed via the Query Analyzer tool. Query results are downloaded as tab-delimited .txt files and imported into SAS STAT as SAS data sets (SAS Institute, Inc., Cary, NC). Data manipulation and analyses are run using SAS V9.3 for Windows on a micro-PC, protected by the VISN 10 network firewall.
We identified patients in the Cleveland VAMC exposed to one of two special diabetes intervention programs by linking to unique note titles: (1) the Diabetes Care Coordination note and (2) the Diabetes Shared Medical Appointment note. The Diabetes Care Coordination program uses trained clinic nurses, most of whom are certified diabetes educators, to provide individual management for starting and titrating insulin for patients with high HbA1c values. The Diabetes Shared Medical Appointment uses the same approach, but in a group setting based in medical center primary care clinics rather than in community-based clinics. The Diabetes Care Coordination program began in May 2003; the Diabetes Shared Medical Appointment began in 2005. From the diabetes registry, the annual incidence of new patients and their insulin status at the time of first visit to the intervention program was ascertained.
Hemoglobin A1c test results were averaged over each calendar year from 2002 through 2006 for each individual patient tested in the Cleveland VAMC. The yearlong, average HbA1c value was used to avoid seasonal variation in HbA1c values and to give the same weight to each individual, regardless of the frequency of testing.11 For each patient, insulin status was determined by ascertaining the calendar year in which a prescription for insulin was first dispensed by a VISN 10 pharmacy.
Statistical tests were frequency counts and the Cochran–Armitage test for trend using SAS statistical software. Alpha error was set at 0.05, two tailed.
Web-Based Reporting
The data views of the diabetes registry are linked to a Web-based query system supported by Microsoft's asp.net2 program. Semicustomizable queries were programmed in C# language using Visual Basic Design Studio (Figure 4). To facilitate rapid reporting, we set up a view in the diabetes registry that contains only active patients, with fields for the data elements used in the standard queries. For example, the view called the “Active Patient Profile” contains patient-level attributes such as the most recent HbA1c and low-density lipoprotein cholesterol values, the mean value of the most recent three blood pressures, and the date when the next diabetic foot or eye examination is due. Reports can be exported into Excel spreadsheets or tab-delimited .txt files.
Figure 4.
Layout of VISN 10 intranet Web page to request a report from the diabetes registry. VISN 10 is the VA Integrated Service Network 10 covering the state of Ohio. Users may select one to five criteria simultaneously to narrow the report to a specific group of patients with outlier values.
Results
Identifying Patients with Diabetes
The operational definition used to identify patients who have diabetes from all veterans enrolled in VISN 10 sites is listed in Table 1 (step 1). Either of two criteria may be used for case identification: (1) the presence of an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code or (2) the dispensing of a diabetes-specific medication from a VHA pharmacy. Diabetes-specific medications are defined as sulfonylureas, biguanides, thiazolidenediones, α-glucosidase inhibitors, metiglinides, insulin, and glucose meter test strips. The algorithm using the diagnosis codes searches for any of four ICD-9-CM diagnosis codes specific to diabetes—250.xx, 357.2, 362.0, and 366.4112—for any inpatient or outpatient encounter beginning October 1, 2001. Iterative spot checks initially revealed errors in specificity, prompting a revision of operational definitions. To minimize false-positive case identification, the algorithm was strengthened to require that any of the ICD-9-CM codes be listed on at least three separate dates. Similarly, spot checks revealed that the prescription of a sulfonylurea was incorrectly made on a single occasion and immediately cancelled by the ordering physician. Therefore, the algorithm using medications for case identification was strengthened to require that a diabetes-specific medication be dispensed on at least two separate dates. Using the definition just described, a total of 81,227 unique patients enrolled in VISN 10 since October 1, 2001 currently meet the definition for having diabetes (Figure 1).
Figure 1.
Unique patients in the diabetes registry, by activity status, and method of assignment to the clinic group responsible for diabetes care. VISN 10 is the VA Integrated Service Network 10, which covers the state of Ohio. Patients are retained in the diabetes registry in a cumulative fashion, beginning October 1, 2001. Active patients are defined either by having a primary care clinic visit within the past 18 months or by having diabetes medications dispensed from a VISN 10 pharmacy within the past 18 months. By mapping the location of each patient's most recent primary care visit in the past 18 months to a clinic group, more patients could be assigned to a clinic group responsible for diabetes care than could be assigned by searching the tables that maintain the primary care provider assignments.
Identifying Active Patients
The operational definition for identifying patients actively managed in VISN 10 outpatient clinics is listed in Table 1, step 2. The algorithm searches for either a primary care clinic visit or dispensing of a diabetes-specific medication from a VISN 10 pharmacy within the past 18 months for patients without a date of death. Since October 2001, 17,246 patients with diabetes are known to have died, and approximately 42,000 patients in VISN 10 are currently actively managed for diabetes; however, this number fluctuates frequently (Figure 1).
Identifying the Responsible Provider of Diabetes Care
Using the primary care provider assignment table, 15% of all actively managed patients remain unassigned to either a primary care provider or a clinic in VISN 10. Mapping the most recent primary care clinic encounter to a specific primary care clinic resulted in a reduction in the number of unassigned patients to 9% (Figure 1).
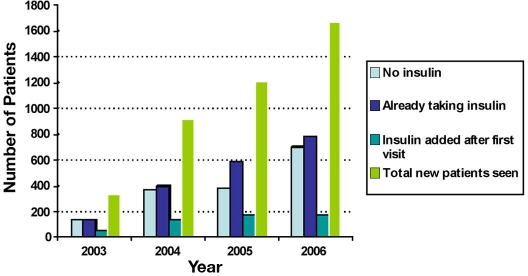
Quality Improvement Programs
In addition to routine quality improvement, two special programs were initiated at the Cleveland VAMC: Diabetes Care Coordination (a nurse case management program) and the Diabetes-Shared Medical Appointment.13 Annual new patients seen by the Diabetes Care Coordination program increased from 346 patients in 2003 to 1505 patients in 2006, while annual new patients seen by the Diabetes-Shared Medical Appointment team increased from 65 patients in 2005 to 169 patients in 2006 (Figure 2). By December 31, 2006, a cumulative total of 3922 patients had been seen by Diabetes Care Coordination nurses and 234 patients had been seen by the Diabetes-Shared Medical Appointment team. The majority of patients were already taking insulin, or insulin was started after the first visit to the program.
Figure 2.
Annual increase in new patients seen by two ambulatory quality improvement programs in the Louis Stokes Cleveland Department of Veterans Affairs Medical Center by insulin status. The Diabetes Care Coordination Program (a nurse case manager program) began in 2003 to offer insulin initiation and intensification to patients with high HbA1c values in the community-based outpatient clinics affiliated with the Cleveland VAMC. The Diabetes-Shared Medical Appointment (a multidisciplinary team program) began in 2005 to offer insulin initiation and intensification to patients with high HbA1c values in the Cleveland VAMC primary care clinics located in the medical center facility.
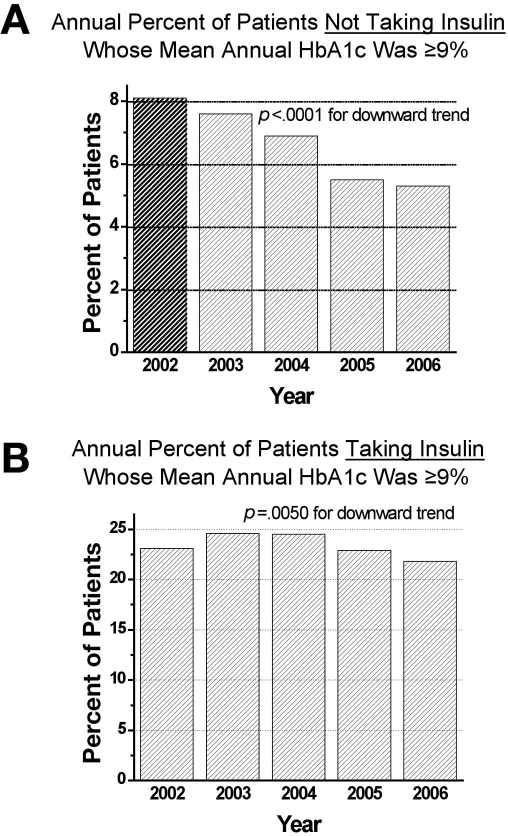
Trends in Glycemic Outcomes
A 5-year trend in glycemic outcomes was determined for patients in the Cleveland VAMC. The denominator was all patients with diabetes receiving any HbA1c tests in the Cleveland VAMC from 2002 through 2006. All test results for each individual were averaged over each calendar year, yielding a single mean HbA1c value per patient per year. For patients not taking insulin during the calendar year, the percent with mean annual HbA1c values ≥9% trended downward from 8.1% in 2002 to 5.3% in 2006 (p < 0.0001) (Figure 3). For patients taking insulin, the annual percent with mean annual HbA1c values ≥9% trended downward from 24.6% in 2003 to 21.8% in 2006 (p = 0.0005). Overall, 26% of patients were taking insulin.
Figure 3.
Time trends in percent of patients with high HbA1c values in the Louis Stokes Cleveland Department of Veterans Affairs Medical Center by insulin status. For each patient, HbA1c values within the calendar year were averaged to yield a mean annual HbA1c value (a single value per patient). Insulin status was determined for each patient by year in which an insulin prescription was first dispensed from a VISN 10 pharmacy. Once started, the patient was assumed to remain on insulin for subsequent years.
Providing Reports
Figure 4 shows a screen print of the VISN 10 intranet Web page for the diabetes registry. The user is given a choice of one to five VHA performance indicators for the quality of care of patients with diabetes, joined by the Boolean ‘and’. Therefore, choosing more indicators results in a smaller group of patients. Although not shown in this screen print, the query is narrowed further by limiting the patient group to a clinic group, a primary care team, a primary care provider, or a specific note title indicating a special intervention program. The provision of reports to diabetes registry users is a work in progress, but represents the end goal of the diabetes registry for continuous quality improvement. The reports can be exported to spreadsheets for filtering, sorting, and mail merging to templated patient letters.
Discussion
In this report, we have described the methods and demonstrated the feasibility of creating an electronic diabetes registry populated from the database underlying the computerized patient record system of the VHA. The necessary tasks included (1) mapping the legacy database system (VistA) into a relational database system (Microsoft SQL server) that supports a high-level query language, (2) operationalizing definitions for case identification of patients with diabetes, (3) operationalizing definitions for an actively managed patient, (4) creating an algorithm to identify the clinic group responsible for primary care for each patient, and (5) using unique clinic note titles to identify patients exposed to special interventions. To protect the integrity of the SQL database system and to minimize data storage requirements, we created views of data linked to each patient in the registry rather than physical data tables. To facilitate rapid Web-based reporting, we added derived variables, such as the most recent HbA1c value, within the Active Patient Profile view. Thus, the Web-linked query needs to search only a single view, or virtual table. Web-linked reports are limited to spreadsheets at this time. We judged that a spreadsheet format (e.g., the ability to sort, filter, and mail merge) would have the best utility for quality improvement activities.
We tailored the data elements of the standard queries available through the Web site to coincide with the diabetes-related performance indicators used by the VHA: glycemic control, cholesterol control, blood pressure control, annual foot examinations, and annual eye examinations.14 These indicators are based on clinical evidence that improvements in the indicators will improve the health status of patients. The VHA monitors these indicators on a quarterly basis and provides feedback to providers at the site and facility levels. The added value of the diabetes registry, as opposed to the performance feedback provided by the VHA Office of Quality and Performance, is that measurement and feedback can occur at the clinic or provider level, where changes to affect clinical performance are made. The diabetes registry reports not only inform providers about performance, but also identify which patients are falling behind in clinical outcomes. This functionality gives the providers a chance to reach out to specific patients in a proactive way. Moreover, the feedback is user driven and can occur at short time intervals. Rapid, repeated feedback at the provider level is considered to be essential to continuous quality improvement.15,16
Ad hoc analysis of data from the diabetes registry demonstrates that glycemic outcomes of patients in the Cleveland VAMC are improving across the past 5 years, regardless of insulin status. However, there is still room for improvement. For example, 75% of all diabetes registry patients are not taking insulin, yet 5% of these patients have HbA1c values of 9% or higher. More than 20% of patients taking insulin currently have high HbA1c values. Therefore, based on the current denominator of approximately 20,000 active patients with diabetes in the Cleveland VAMC (data not shown), approximately 1800 patients need to start or intensify insulin therapy. These patients are candidates for the Diabetes Care Coordination or the Diabetes-Shared Medical Appointment programs, which combine insulin titration with glucose pattern management and carbohydrate counting. Of 1600 new patients seen by these programs in 2006, slightly more than half were either already taking insulin or initiated insulin after the first visit to the intervention program. To meet the needs of the 1800 patients with poor glycemic control in the coming year, one conclusion might be that the programs should focus more exclusively on patients needing to start or advance insulin therapy.
Conclusion
A diabetes registry designed for quality improvement of diabetes care and outcomes can be populated in a continuous manner from the database underlying the VHA electronic patient record database system. The registry may be linked to Web-based queries for repeated surveillance of patients with poor clinical outcomes and ad hoc analyses for longitudinal tracking of special interventions, including the potential workload for quality improvement programs.
Acknowledgements
This paper was presented, in part, at the Sixth Annual Diabetes Technology Meeting in Atlanta, Georgia, November 2, 2006. Dr. Kern was supported as a fellow by the VA National Quality Scholars program for a portion of the work. This work was supported by the HSR&D service of the Department of Veterans Affairs and the Quality Enhancement Research Initiative of VA HSR&D. The authors gratefully acknowledge the support of Susan Fuehrer, associate director, and William Montague, medical center director, of the Louis Stokes Cleveland Department of Veterans Affairs Medical Center and Dr. Scott Ober, medical director of the community-based outpatient clinics of the Louis Stokes Cleveland Department of Veterans Affairs Medical Center.
Abbreviations
- CPRS
Computerized Patient Record System
- HbA1c
hemoglobin A1c
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- VA
Veterans Affairs
- VHA
Veterans Health Administration
- VAMC
Veterans Affairs Medical Center
- VISN 10
VA Integrated Service Network 10
- VistA
Veterans Health Information Systems and Technology Architecture
References
- 1. Surveillance Epidemiology and End Results. 2007 [cited 2007 Nov 4]. Available from: http://seer.cancer.gov.
- 2. United States Renal Data System. 2007 [cited 2007 Nov 4]. Available from: http:/www.usrds.org.
- 3.McCulloch DK, Price MJ, Hindmarsh M, Wagner EH. A population-based approach to diabetes management in a primary care setting: early results and lessons learned. Eff Clin Pract. 1998;1(1):12–22. [PubMed] [Google Scholar]
- 4.Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998;1(1):2–4. [PubMed] [Google Scholar]
- 5.Friedman DJ. Assessing the potential of national strategies for electronic health records for population health monitoring and research. Vital Health Stat 2. 2006;(143):1–83. [PubMed] [Google Scholar]
- 6.Senge PM. The fifth discipline: the art and practice of the learning organization. 1st. New York: Doubleday; 1990. 423 pp. [Google Scholar]
- 7. VISTA [U.S. government Web site]. June 12, 2007 [cited 2007 Nov 12]. Available from: http://www.virec.research.va.gov/DataSourcesName/VISTA/VISTA.htm.
- 8. VA Fileman SQL Interface (SQLI) Site Manual. 1997 [cited Nov 2007]. Available from: www.vista.med.va.gov/softserv.
- 9. Beneficiary Identification Records Locator Sub-System (BIRLS) Death File. 2007 [cited 2007 Nov 7]. Available from: http://www.virec.research.va.gov/DataSourcesName/BIRLS/BIRLS.htm.
- 10. Knowledge Based Systems: Making Data Meaningful to You [company Web site]. 2007 [cited 2007 Nov 11]. Available from: http://www.kbsystems.com.
- 11.Tseng CL, Brimacombe M, Xie M, Rajan M, Wang H, Kolassa J, Crystal S, Chen TC, Pogach L, Safford M. Seasonal patterns in monthly hemoglobin A1c values. Am J Epidemiol. 2005;161(6):565–574. doi: 10.1093/aje/kwi071. [DOI] [PubMed] [Google Scholar]
- 12.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(Suppl 2):B10–21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- 13.Kirsh S, Watts S, Pascuzzi K, O'Day ME, Davidson D, Strauss G, Kern EO, Aron DC. Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 2007;16(5):349–353. doi: 10.1136/qshc.2006.019158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. VA-DoD Clinical Practice Guidelines. 2007 [cited 2007 Nov 4]. Available from: http://www.oqp.med.va.gov/cpg/cpg.htm.
- 15.Friedman NM, Gleeson JM, Kent MJ, Foris M, Rodriguez DJ, Cypress M. Management of diabetes mellitus in the Lovelace Health Systems' EPISODES OF CARE program. Eff Clin Pract. 1998;1(1):5–11. [PubMed] [Google Scholar]
- 16.Joshi MS, Bernard DB. Clinical performance improvement series. Classic CQI integrated with comprehensive disease management as a model for performance improvement. Jt Comm J Qual Improv. 1999;25(8):383–395. doi: 10.1016/s1070-3241(16)30453-9. [DOI] [PubMed] [Google Scholar]