Abstract
Diabetes is the leading cause of adult vision loss in the United States and other industrialized countries. While the goal of preserving vision in patients with diabetes appears to be attainable, the process of achieving this goal poses a formidable challenge to health care systems. The large increase in the prevalence of diabetes presents practical and logistical challenges to providing quality care to all patients with diabetes. Given this challenge, the Veterans Health Administration (VHA) is increasingly using information technology as a means of improving the efficiency of its clinicians. The VHA has taken advantage of a mature computerized patient medical record system by integrating a program of digital retinal imaging with remote image interpretation (teleretinal imaging) to assist in providing eye care to the nearly 20% of VHA patients with diabetes. We describe this clinical pathway for accessing patients with diabetes in ambulatory care settings, evaluating their retinas for level of diabetic retinopathy with a teleretinal imaging system, and prioritizing their access into an eye and health care program in a timely and appropriate manner.
Keywords: diabetes, diabetic retinopathy, teleretinal imaging, Veterans Health Administration
Introduction
Diabetic retinopathy (DR) is a leading cause of preventable vision loss in the United States and other developed countries.1–4 The value of screening for DR is well established, and a number of preferred clinical practice patterns are in place to guide clinicians in reducing the risk of vision loss from diabetes.5–7 Despite these guidelines, only 60% of persons with diabetes receive timely and appropriate eye examinations.8–11 There are a number of obstacles to being screened for diabetes-related ocular complications. These obstacles include access to care and the misconception by patients that regular eye examinations are unnecessary, especially if visual function is not compromised. Access to eye care is also often limited by geographic, economic, cultural, educational, and other factors.12
Unmet Need in the Veterans Health Administration (VHA)
The VHA is the largest integrated managed health care system in the United States, providing health care services to five million eligible patients. Diabetes within the VHA poses a significant challenge because the estimated prevalence among its enrolled patients is as high as 20%, substantially higher than the general population.13,14 To meet the challenge of offering comprehensive quality care, the VHA has instituted important programs to ensure that all patients with diabetes are evaluated with appropriate periodicity for DR and other related ocular complications.15,16 The VHA also has in place an external peer review program with the objective of creating a nationwide standard to establish policies to modify care processes and to emphasize quality improvement.17 An outcome of this program is to ensure that patients with chronic disease, such as diabetes, and especially those with attendant risk factors, receive regular and timely assessment and treatment of such risk factors and screening for the presence of complications. Recent clinical outcomes show that the VHA has achieved efficiency and quality of care for its patients with diabetes that exceed that in the private sector.3 Table 1 summarizes the processes in place for VHA patients and the number of patients accessed for various evaluative diabetes screening measures for fiscal year 2005.13
Table 1.
Percentage of VHA Patients with Diabetes Achieving Various Evaluative Screening Measures for Fiscal Year 2005
| Indicators | Results (% of patients) |
|---|---|
| HbA1c <9.0% | 85 |
| HbA1c <8.0% | 73 |
| HbA1c <7.0% | 49 |
| Lipid profile | 77 |
| Blood pressure ≤140/90 mm Hg | 75 |
| Retinal examinations (biennial unless risk factors are present) | 79 |
| Annual foot examination | 83 |
Early detection of retinal abnormalities is essential in preventing vision loss from diabetes. Clinical studies have clearly shown that the visual outcome is more favorable if patients are evaluated and treated early.18 In addition to DR, other vision-threatening eye diseases are more common in an aging population and in patients with diabetes. These include glaucoma, cataract, age-related macular degeneration, and systemic-related retinal vascular disease.14 All of these ocular disorders can be identified through regular eye examinations and many can be treated or managed by early identification. Thus, current VHA guidelines recommend eye examinations every 24 months or less for persons with diabetes, depending on findings from a previous eye examination and other identifiable risk factors, such as associated laboratory values [hemoglobin A1c (HbA1c), serum lipid levels, systemic blood pressure, the presence of microalbuminuria] and in those taking insulin19 (Table 2).
Table 2.
VHA Referral Guidelines for Eye Examinations in Patients with Diabetes
| Indicators for referral for eye examination |
|---|
| >1 year since last eye examination or cannot demonstrate recent eye examination by a provider outside of the VHA |
| HbA1c >8.0% after 1 year of treatment |
| Taking insulin |
| Type 1 diabetes >3 years or type 2 diabetes |
| Blood pressure >140/90 mm Hg |
| Impaired renal function, proteinuria (>300 mg/24 h), elevated serum creatinine, on dialysis, or post-transplant |
| History of visual impairment in at least one eye, not necessarily related to hyperglycemia |
| Pregnancy |
| Have additional microvascular or macrovascular complications related to diabetes |
VHA Teleretinal Imaging Program for Patient with Diabetes
Based on the urgent need to develop alternative methods to screen and evaluate an increasing number of patients with diabetes for DR, the VHA developed a program of digital retinal imaging with remote image interpretation (i.e., teleretinal imaging) as a means of improving access to eye care. Digital retinal imaging and fundus photography, when performed using accepted standards and validated pathways, is a potential tool for detecting patients at risk for vision loss from DR and possibly other ocular and related systemic diseases. Digital retinal imaging through undilated pupils has been validated as an alternative to dilated fundus photography in evaluating patients for the presence of DR.20–22 This approach is also more convenient for patients and is more widely accessible. Obviating the need for pupil dilation in most cases allows for more widespread deployment in ambulatory care settings where patients can be accessed as they present for primary care or other non-eye care appointments.
In fiscal year (FY) 2000, the U.S. Congress recognized the importance of preventing blindness from diabetes by recommending that the VHA collaborate with the Department of Defense (DOD) and the Joslin Diabetes Center (Boston, MA) to implement a technology-based platform using nonmydriatic digital retinal imaging and remote image interpretation to assess for the level of DR. That teleretinal imaging system, the Joslin Vision Network™, was an outgrowth of a pilot program developed by the VHA and implemented in FY 1999 in collaboration with the Joslin Diabetes Center, the DOD, and Veterans Integrated Service Networks (VISN) 1 and 20.23 Using a nonmydriatic digital retinal imaging platform, imaging stations were installed at medical centers and community-based outpatient clinics in New England and the Pacific Northwest. Images captured at the remote imaging stations were transmitted to reading centers at the Veterans Affairs (VA) Puget Sound Healthcare System and VA Boston Healthcare System. This pilot program proved to be highly successful in identifying patients in need of further care, while at the same time postponing visits for those with little or no risk factors for the progression of retinopathy.15,16
In 2001, the VHA convened an expert panel to address issues of the clinical application, quality and training, information technology, and health care infrastructure needs for deploying such a teleretinal imaging program. The panel developed recommendations and formulated a plan for a systematic national rollout of VISN-based teleretinal imaging programs.23 The success of this proof of concept and the prospect for sustainability prompted the VHA to expand the model on a nationwide basis.
The Teleretinal Imaging Clinical Pathway
In the VHA and elsewhere, eye care professionals are typically responsible for diagnosing and treating patients for DR. However, patients already accessed into an eye care program are likely receiving appropriate and timely treatment. For patients with chronic disease such as diabetes, the primary care setting is the best site for identifying patients at risk for visual disability.24,25 Thus, teleretinal imaging platforms were deployed primarily in the ambulatory care setting (Figure 1).
Figure 1.
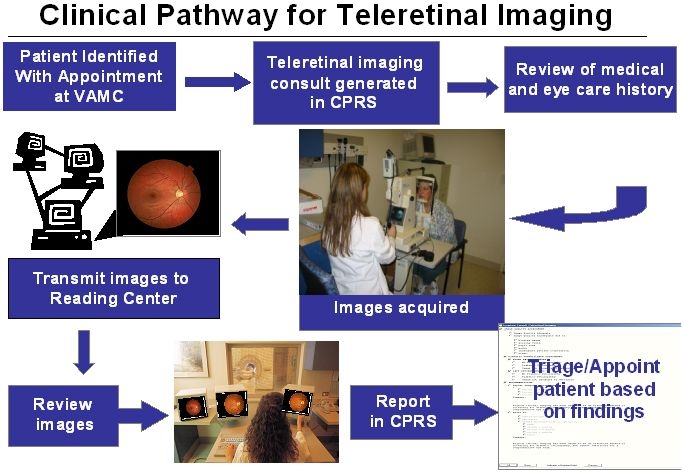
Clinical pathway for teleretinal imaging in the VHA. Potential patients are initially identified as those having an ambulatory care appointment at the VA medical center (VAMC). The imager generates a teleretinal imaging consult, obtains relevant clinical information from the patient, and obtains images. These images are attached to the consult and forwarded to a reading center, where they are reviewed. A report is generated and becomes a part of the patient's medical record. Based on interpretation and referral recommendation of the reader, the imager takes appropriate steps to ensure the patient has necessary eye care follow-up.
Accessing Patients
The VHA Teleretinal Imaging Program is designed to facilitate access to quality diabetes eye care that complies with VHA guidelines for retinal examinations in patients with diabetes and allows prioritization of patients for comprehensive eye evaluations by eye care professionals. Patients are identified by an imager/patient care coordinator through a review of scheduled appointments in primary care or other non-eye care appointments at the respective VA medical centers. Most patients were overdue for their annual diabetic eye examination or were referred by their provider because of prior findings, first-time or new onset symptoms, or complaints deemed by medical providers to warrant referral for eye examination. Patients were typically contacted by the image acquisition specialist to arrange the imaging session on the day of the ambulatory care appointment. Using the VA computerized patient record system (CPRS), the imager identified patients who were overdue for an eye examination. The robust nature and enormous potential of the electronic medical record system within the VA allow the imager to take advantage of CPRS to identify appropriate patients for imaging. Based on the retrospective nature of this report, the number of patients referred to imaging based on patient history, symptoms, or examination findings is undetermined. Patients are only excluded from the teleretinal imaging program if they have a history of previous retinal laser treatment, a history of previous intraocular retinal surgery, if they are one-eyed, or wear an eye prosthesis. All other patients are included, even if they have a history of cataract surgery with intraocular lens implantation, small pupils, media opacities, strabismus, lid or adnexal abnormalities, end stage renal disease, or other preexisting ocular or systemic conditions. Patients are contacted and scheduled for digital retinal imaging via the CPRS consult mechanism.
Imager Training
Imagers are certified through the VA National Teleretinal Training Center in Boston, where each imager participates in a two and one-half day competency-based multidisciplinary program that includes skill transfer in the technique of teleretinal imaging, as well as an intensive overview of diabetes and diabetic eye disease. Imagers are taught to provide an initial triage through recognition of significant lesions of DR and other systemic-related retinal lesions that may require more urgent attention. If the imager identifies an important finding, he/she immediately notifies the reader, who then may perform a more immediate review of the study.
Obtaining Digital Retinal Images
The certified teleretinal imager uses a Topcon TRC-NW6S digital retinal camera to obtain nonmydriatic digital retinal images of three 45° fields and an external image of each eye according to a protocol developed during pilot studies.15,23,26 Images comprising three 45° fields are captured for each eye: nonmydriatic image (NM)-1, centering the macula and including the optic disk; NM-2, encompassing the superior temporal vascular arcade; and NM-3, covering an area of the retina nasal to the optic disk with a slight emphasis toward the inferior quadrant. Additionally, an external image is captured for gross evaluation of the lids, lashes, and periocular region. This imaging protocol allows for a comprehensive evaluation for retinal disease within the vascular arcades, including the optic nerve head and the macula, and, in some cases, as far out as the retinal equator.
After completing the imaging protocol, the imager demonstrates to the patient the basic anatomical structures of the ocular fundus, indicating the optic nerve, the macula, and the retinal blood vessels, and reinforces the importance of optimal blood glucose and blood pressure control. Acting as a care coordinator, the imager also acts on the reader's recommendations and communicates with the patient to establish an appropriate follow-up eye examination schedule.
Image Interpretation
The images and patient data elements are imported into the VHA electronic medical record system Veterans Health Information Systems and Technology Architecture (VistA) via the digital imaging communication standards in medicine pathway and are available for viewing at the local reading center or elsewhere within the VHA system. Independently licensed eye care providers, certified as image review specialists (i.e., readers), review all studies. Readers also undergo a one and one-half day certification program at the VA National Teleretinal Training Center. The reader interprets the study and records results using a reading template that is stored in the CPRS. Reader-generated reports include diagnosis of level of DR and diabetic macular edema, identification of nondiabetic ocular conditions, and recommendation for the next eye examination. These reports and the images are available to the imager, primary care team, and other providers through VistA. In the event of an unexpected urgent or emergent finding, the reader promptly contacts the imager so that appropriate action can be taken.
Benefits of the Teleretinal Imaging Eye Care Program
There are several compelling aspects to this teleretinal imaging clinical pathway. The first important feature is that the level of DR is determined reliably. In a series of studies, a significant level of agreement has been shown for the level of DR and for the presence of referable eye diseases between digital retinal imaging and subsequent comprehensive eye examinations performed by eye care professionals.15,21,26 Digital retinal imaging also frequently identifies nondiabetic ocular pathology,15 although there are fewer studies validating this additional feature. A second major benefit of the program occurs during the imaging encounter, when the imager/care coordinator has an opportunity to provide basic education to the patient relating to causes and prevention of diabetes-related eye complications and preservation of vision. An additional unique feature of the program is its link to the comprehensive electronic medical record system of the VHA, which includes a broad array of patient data, clinical reminders, laboratory and diagnostic test results, and expert system feedback to make better decisions regarding diagnosis, treatment, and management. The seamless nature of the imaging technology platform and the VistA/CPRS of the VHA facilitates the comprehensive nature of the diabetes eye care program and provides an integrated patient record system, not only for clinicians but also for managers, quality assurance staff, and researchers.
Patient Satisfaction
Patients' responses to nonmydriatic teleretinal imaging are universally positive. Obtaining retinal images without pupil dilation is efficient and less time sensitive, as the imager does not have to wait for the eye drops to take effect. Indeed, pupil dilation for most patients imposes additional inconveniences and is impractical for a wide-ranging DR screening program.27 Patient acceptance of both the imaging procedure and the educational intervention is important for the successful implementation and sustainability of any such eye care model. We showed previously that the vast majority of patients reported that nonmydriatic digital retinal imaging was comfortable, improved their understanding of eye disease, and was preferred to standard photography or dilated examination by a retinal specialist.21,26 Of equal importance, most patients indicated that they would prefer to return annually for these examinations, thus inferring that nonmydriatic teleretinal imaging may have the potential to enhance adherence to diabetes eye care guidelines.
Economic Benefits
The economic burden of vision loss from diabetes is enormous and has been calculated at $132 billion in direct and indirect costs. These include medical costs, including hospitalizations and the costs of medications, vision rehabilitation, loss of productivity, and the impact on quality of life. The benefits of detecting and treating sight-threatening retinopathy in patients with diabetes have been borne out by many cost-effectiveness and cost-utility studies.28,29 Initially, studies indicated that annual screening for DR in type 2 diabetes showed no economic benefit.29,30 However, later studies showed an important cost benefit.31
Widespread deployment of teleretinal imaging to assess for the level of DR requires that it be a cost-effective strategy. While several studies have shown that fundus photography is more sensitive than a direct ophthalmoscopic examination in screening for DR,32–36 this latter photography requires pupil dilation and is typically carried out by trained personnel using specialized equipment to obtain standard photographic fields.16 This reduces its cost-effectiveness as a screening tool. Using a modeled cost-effectiveness analysis and decision analysis, we compared the cost-effectiveness of teleretinal imaging versus dilated fundus examinations with ophthalmoscopy for their ability to detect vision-threatening proliferative DR and its consequences.
We showed that in the VHA, nonmydriatic teleretinal imaging was both less costly and more effective for detecting proliferative DR and averting cases of severe vision loss.37 Accordingly, nonmydriatic teleretinal imaging may be more time efficient, improves adherence, and offers favorable cost-effectiveness in assessing the level of DR than a standard clinical examination, particularly in low-risk patients. By implication, using teleretinal imaging to evaluate patients may also free up eye care practitioners from screening activities and enable them to utilize their skills more effectively in the care of patients with eye diseases.
Future Direction
In late 2006, 17 of the 21 VISN were awarded funding to incorporate this teleretinal imaging eye care model into their primary care programs. Each of the 17 VISN received funding for six cameras and personnel to support both imaging at remote sites and image review at the VISN level. Later, additional funding was provided for the purchase of cameras at the four additional VISN. Prior to initiating the imaging protocol, both imagers and readers are trained at a 3-day program held at the VA National Teleretinal Training Center in Boston.
During the first year of the national program there were 74,414 unique patients who had teleretinal imaging at approximately 150 imaging sites in 21 VISN. Data on operating characteristics of teleretinal imaging and clinical outcomes from these patients are still being accumulated and will soon be forthcoming. As an example of the clinical diagnoses likely to be observed in the national program, we performed imaging studies on 2724 patients using the clinical pathway described earlier from a rural VA setting (Togus, ME) that has limited eye care services. The average age of these patients was 62 years, 98% were male, their mean duration of diabetes was 7.1 years, and the average HbA1c was 7.2%. Criteria for referral for eye examination included the presence of DR of moderate level or worse or if a study was deemed ungradeable based on an inability to interpret images because of blur, media opacity, missing or poorly composed fields, or other causes. Applying these criteria, 327 patients (12%) were referred for eye examination for evaluation of DR. In addition, a series of nondiabetic conditions were also noted, including cataract (32%), choroidal nevus (8.5%), age-related maculopathy (10%), and suspicion of glaucoma (11%). Another 1.5% of patients had more urgent ocular conditions that required more immediate referral, including evidence of retinal vascular occlusion, retinal embolus, and retinal or preretinal hemorrhage.
Conclusion
Diabetic retinopathy has the potential to severely affect the quality of life for patients with diabetes. Much of this disability and loss of independence can be averted by timely and appropriate screening for the presence of DR. Technological advances such as teleretinal imaging give more patients access to proper screening for DR.
The technology platform and clinical pathway used in the VHA teleretinal imaging program have proved to be effective means to screen patients for sight-threatening DR. Such a clinically relevant, cost-effective program to screen for DR will allow the VHA to expand access to patients with diabetes. Thus, the creative use of validated technology has brought specialty care to patients with diabetes who might not otherwise have ready access. It is anticipated that as this eye care model matures, the pathway will help reduce the incidence of vision-threatening complications of diabetes.
Acknowledgements
Funding for this work was provided in part from a contract sponsored by the Department of the Army by Cooperative Agreement DAMD (17-98-2-8017), grants from VA Health Services Research and Development Service (TEL-02-100 and IIR-04-045), and the National Institutes of Health (K24-DK06321).
Abbreviations
- CPRS
computerized patient record system
- DOD
Department of Defense
- DR
diabetic retinopathy
- FY
fiscal year
- HbA1c
hemoglobin A1c
- NM
nonmydriatic image
- VA
Veterans Affairs
- VHA
Veterans Health Administration
- VISN
Veterans Integrated Service Networks
- VistA
Veterans Health Information Systems and Technology Architecture
References
- 1.American Diabetes Association. Diabetic retinopathy. Diabetes Care. 2000;23(Suppl 1):S73–76. [PubMed] [Google Scholar]
- 2.Aiello LP, Gardner TW, King GL, Blankenship G, Cavallerano JD, Ferris FL, 3rd, Klein R. Diabetic retinopathy. Diabetes Care. 1998;21:143–156. doi: 10.2337/diacare.21.1.143. [DOI] [PubMed] [Google Scholar]
- 3.Kerr EA, Gerzoff RB, Krein SL, Selby JV, Piette JD, Curb JD, Herman WH, Marrero DG, Narayan KM, Safford MM, Thompson T, Mangione CM. Diabetes care quality in the Veterans Affairs Health Care System and commercial managed care: The TRIAD Study. Ann Intern Med. 2004;141:272–281. doi: 10.7326/0003-4819-141-4-200408170-00007. [DOI] [PubMed] [Google Scholar]
- 4.Kempen JH, O'Colmain BJ, Leske MC, Haffner SM, Klein R, Moss SE, Taylor HR, Hamman RF Eye Diseases Prevalence Research Group. The prevalence of diabetic retinopathy among adults in the United States. Arch Ophthalmol. 2004;122:552–563. doi: 10.1001/archopht.122.4.552. [DOI] [PubMed] [Google Scholar]
- 5.VHA/DOD Clinical Practice Guidelines. Eye care for patients with diabetes mellitus. Available from: http://www.oqp.med.va.gov/cpg/DM/DM_base.htm.
- 6.American Optometric Association. 3rd. St. Louis (MO): American Optometric Association; 2002. Care of the patient with diabetes mellitus. [Google Scholar]
- 7.American Academy of Ophthalmology. Preferred practice patterns 2001. Available from: http://www.aao.org/aao/education/library/ppp/index.cfm.
- 8.Brechner RJ, Cowie CC, Howie LJ, Herman WH, Will JC, Harris MI. Ophthalmic examination among adults with diagnosed diabetes mellitus. JAMA. 1993;270:1714–1718. [PubMed] [Google Scholar]
- 9.Orr P, Barron Y, Schein OD, Rubin GS, West SK. Eye care utilization by older Americans: the SEE Project. Salisbury Eye Evaluation. Ophthalmology. 1999;106:904–909. doi: 10.1016/s0161-6420(99)00508-4. [DOI] [PubMed] [Google Scholar]
- 10.Moss SE, Klein R, Klein BE. Factors associated with having eye examinations in persons with diabetes. Arch Fam Med. 1995;4:529–534. doi: 10.1001/archfami.4.6.529. [DOI] [PubMed] [Google Scholar]
- 11.Schoenfeld ER, Greene JM, Wu SY, Leske MC. Patterns of adherence to diabetes vision care guidelines: baseline findings from the Diabetic Retinopathy Awareness Program. Ophthalmology. 2001;108:563–571. doi: 10.1016/s0161-6420(00)00600-x. [DOI] [PubMed] [Google Scholar]
- 12.Hartnett ME, Key IJ, Loyacano NM, Horswell RL, DeSalvo KB. Perceived barriers to diabetic eye care. Arch Ophthalmol. 2005;123:387–391. doi: 10.1001/archopht.123.3.387. [DOI] [PubMed] [Google Scholar]
- 13. Feb 2006 Fact Sheet [cited 2006 Dec]. February 2006 www.va.gov.
- 14.Orcutt J, Avakian A, Koepsell TD, Maynard C. Eye disease in veterans with diabetes. Diabetes Care. 2004;27:B50–3. doi: 10.2337/diacare.27.suppl_2.b50. [DOI] [PubMed] [Google Scholar]
- 15.Cavallerano AA, Cavallerano J, Katalinic P, Blake B, Rynne M, Conlin PR, Hock K, Tolson AM, Aiello LP Joslin Vision Network Clinical Team. A telemedicine program for diabetic retinopathy in a Veterans Affairs Medical Center–the Joslin Vision Network Eye Health Care Model. Am J Ophthalmol. 2005;139:597–604. doi: 10.1016/j.ajo.2004.10.064. [DOI] [PubMed] [Google Scholar]
- 16.Conlin PR, Fisch BM, Cavallerano AA, Cavallerano JD, Bursell SE, Aiello LM. Nonmydriatic teleretinal imaging improves adherence with annual eye examinations in patients with diabetes. J Rehabil Res Dev. 2006;43:733–740. doi: 10.1682/jrrd.2005.07.0117. [DOI] [PubMed] [Google Scholar]
- 17.EPRP Diagnostic Coding Reviews Health for Operations and Management Monitors FY 2007 Website for Tech Manual. Available from: http://vaww.oqp.med.va.gov.
- 18.Bailey CC, Sparrow JM, Grey RH, Cheng H. The National Diabetic Retinopathy Laser Treatment Audit. III. Clinical outcomes. Eye. 1999;13:151–159. doi: 10.1038/eye.1999.42. [DOI] [PubMed] [Google Scholar]
- 19.VHA/DOD Clinical Practice Guidelines. Eye care for patients with diabetes mellitus [cited 2006 Dec] Available from: http://www.oqp.med.va.gov/cpg/DM/DM_base.htm.
- 20.Bursell SE, Cavallerano JD, Cavallerano AA, Clermont AC, Birkmire-Peters D, Aiello LP, Aiello LM, Joslin Vision Network Research Team Stereo nonmydriatic digital-video color retinal imaging compared with Early Treatment Diabetic Retinopathy Study seven standard field 35-mm stereo color photos for determining level of diabetic retinopathy. Ophthalmology. 2001;108:572–585. doi: 10.1016/s0161-6420(00)00604-7. [DOI] [PubMed] [Google Scholar]
- 21.Cavallerano AA, Cavallerano JD, Katalinic P, Tolson AM, Aiello LP, Aiello LM. Use of Joslin Vision Network digital-video nonmydriatic retinal imaging to assess diabetic retinopathy in a clinical program. Retina. 2003;23:215–223. doi: 10.1097/00006982-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Aiello LM, Cavallerano J, Cavallerano A, Bursell S. The Joslin Vision Network (JVN): innovative telemedicine care for diabetes. Ophthalmol Clin North Am. 2000;13:213–224. [Google Scholar]
- 23.Conlin PR, Fisch BM, Orcutt JC, Hetrick BJ, Darkins AW. Framework for a national teleretinal imaging program to screen for diabetic retinopathy in Veterans Health Administration patients. J Rehabil Res Dev. 2006;43:741–748. doi: 10.1682/jrrd.2005.08.0146. [DOI] [PubMed] [Google Scholar]
- 24.Goldzweig CL, Rowe S, Wenger NS, MacLean CH, Shekelle PG. Preventing and managing visual disability in primary care. JAMA. 2004;291:1497–1502. doi: 10.1001/jama.291.12.1497. [DOI] [PubMed] [Google Scholar]
- 25.Hutchinson A, McIntosh A, Peters J, O'Keeffe C, Khunti K, Baker R, Booth A. Effectiveness of screening and monitoring tests for diabetic retinopathy–a systematic review. Diabet Med. 2000;17:495–506. doi: 10.1046/j.1464-5491.2000.00250.x. [DOI] [PubMed] [Google Scholar]
- 26.Cavallerano JD, Aiello LP, Cavallerano AA, Katalinic P, Hock K, Kirby R, Aiello LM Joslin Vision Network Clinical Team. Nonmydriatic digital imaging alternative for annual retinal exam in persons with previously documented no or mild diabetic retinopathy. Am J Ophthalmol. 2005;140:667–673. doi: 10.1016/j.ajo.2005.03.075. [DOI] [PubMed] [Google Scholar]
- 27.Singer DE, Nathan DM, Fogel HA, Schachat AP. Screening for diabetic retinopathy. Ann Intern Med. 1992;116:660–671. doi: 10.7326/0003-4819-116-8-660. [DOI] [PubMed] [Google Scholar]
- 28.Javitt JC, Aiello LP, Bassi LJ, Chiang YP, Canner JK. Detecting and treating retinopathy in patients with type 1 diabetes mellitus. Savings associated with improved implementation of current guidelines. Ophthalmology. 1991;98:1565–1573. [PubMed] [Google Scholar]
- 29.Dasbach EJ, Fryback DG, Newcomb PA, Klein R, Klein BE. Cost-effectiveness of strategies for detecting diabetic retinopathy. Med Care. 1991;29:20–39. doi: 10.1097/00005650-199101000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Lairson DR, Pugh JA, Kapadia AS, Lorimor RJ, Jacobson J, Velez R. Cost-effectiveness of alternative methods of screening for diabetic retinopathy. Diabetes Care. 1992;15:1369–1377. doi: 10.2337/diacare.15.10.1369. [DOI] [PubMed] [Google Scholar]
- 31.Javitt JC, Aiello LP. Cost-effectiveness of detecting and treating diabetic retinopathy. Ann Intern Med. 1996;124:164–169. doi: 10.7326/0003-4819-124-1_part_2-199601011-00017. [DOI] [PubMed] [Google Scholar]
- 32.Lin DY, Blumenkranz MS, Brothers RJ, Grosvenor DM. The sensitivity and specificity of single-field nonmydriatic monochromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol. 2002;134:204–213. doi: 10.1016/s0002-9394(02)01522-2. [DOI] [PubMed] [Google Scholar]
- 33.Griffith SP, Freeman WL, Shaw CJ, Mitchell WH, Olden CR, Figgs LD, Kinyoun JL, Underwood DL, Will JC. Screening for diabetic retinopathy in a clinical setting: a comparison of direct ophthalmoscopy by primary care physicians with fundus photography. J Fam Pract. 1993;37:49–56. [PubMed] [Google Scholar]
- 34.Harding SP, Broadbent DM, Neoh C, White MC, Vora J. Sensitivity and specificity of photography and direct ophthalmoscopy in screening for sight threatening eye disease: the Liverpool Diabetic Eye Study. BMJ. 1995;311:1131–1135. doi: 10.1136/bmj.311.7013.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kinyoun JL, Martin DC, Fujimoto WY, Leonetti DL. Ophthalmoscopy versus fundus photographs for detection and grading diabetic retinopathy. Invest Ophthalmol Vis Sci. 1992;33:1888–1893. [PubMed] [Google Scholar]
- 36.Moss SE, Klein R, Kessler SD, Richie KA. Comparison between ophthalmoscopy and fundus photography in determining severity of retinopathy. Ophthalmology. 1985;92:62–67. doi: 10.1016/s0161-6420(85)34082-4. [DOI] [PubMed] [Google Scholar]
- 37.Whited JD, Datta SK, Aiello LM, Aiello LP, Cavallerano JD, Conlin PR, Horton MB, Vigersky RA, Poropatich RK, Challa P, Darkins AW, Bursell SE. A modeled economic analysis of a digital tele-ophthalmology system as used by three federal healthcare agencies for detecting proliferative diabetic retinopathy. Telemed J E Health. 2005;11:641–651. doi: 10.1089/tmj.2005.11.641. [DOI] [PubMed] [Google Scholar]


