Abstract
Background
Diabetic retinopathy, damage to the blood vessels in the retina, is the leading cause of blindness in adults 20–74 years of age. Nearly 300 million people worldwide have diabetes and nearly half of all people with diabetes will develop some degree of diabetic retinopathy during their lifetime. It has been estimated that blindness from diabetic retinopathy is preventable in at least 65% of cases, if detected early. The aim of the project was to develop a flexible, modular, mobile method for screening individuals that could be used effectively in a variety of medical and community settings.
Methods
Our project created software to support a simple, effective retinal screening process for people with diabetes. The system included four separate software components: registration, imaging, grading, and tracking/reporting. The imaging component consisted of customized software running on a computer attached to a camera that drives retinal image acquisition.
Results
Seven hundred and six subjects with diabetes were successfully consented, registered, imaged, and had their eye images graded. The mean time for subjects to be registered, imaged, and have eye images graded was 00:12:53. Seventy-six percent of the sample was instructed to follow-up with their eye doctor in 1 year (had no retinopathy or microaneurysms). Only six patients (0.8 %) were asked to see their eye doctor within 6 weeks (proliferative retinopathy or diabetic maculopathy).
Conclusion
Our project successfully demonstrated that the retinal screening software and workflow process can be used to overcome challenges of providing adequate screening and diagnostic services for people at risk for diabetic retinopathy.
Keywords: diabetic retinopathy, eye images, screening, telemedicine
Introduction
There are 20.8 million children and adults in the United States, or 7% of the population, who have diabetes.1 Nearly one-third or 6.2 million are unaware that they have the disease.1 It is estimated that if the present trend continues, one in three Americans born in 2000 will develop diabetes in their lifetime.2
Complications of diabetes result in 12,000 to 24,000 new cases of blindness each year.1 Diabetic retinopathy, damage to the blood vessels in the retina, is the leading cause of blindness in adults 20–74 years of age.1 Between 40 and 45% of Americans diagnosed with diabetes have some stage of diabetic retinopathy.3 Laser therapy, when applied in a timely manner, can reduce the development of severe vision loss by an estimated 50 to 60%.1 Early detection of diabetic retinopathy is essential.
According to the American Diabetes Association's Standards of Medical Care in Diabetes, eye examinations for patients with type 1 and type 2 diabetes should be conducted annually by an ophthalmologist or optometrist.4 The Center for Disease Control analyzed data from the 1997 to 1999 Behavioral Risk Factor Surveillance System (BRFSS) and found that the levels of preventive-care practices among persons with diabetes are lower than the national objectives for 2010.5 Results differ by state but the proportion of persons who received an annual dilated eye examination ranged from 47.0 to 81.0.5 Objectives for 2010 include increasing that proportion to 75%.5 Again using statistics provided by the BRFSS, the proportion of those receiving dilated eye examinations increased by 12% for the period of 1995 to 2001.6 Failure to comply was associated with being younger, being a member of an ethnic minority, having no diabetes education, not taking insulin, and not engaging in preventative practices requiring physician contact.6 “In 2002, approximately 70% of adults with diabetes reported having received a dilated eye exam within the previous year.7”
The American Telemedicine Association defines telemedicine as the use of medical information exchanged from one site to another via electronic communications.8 In 2007, results of a California Healthcare Foundation pilot project that used telemedicine software developed by the University of California Berkley School of Optometry, expert consultation, digital retinal cameras, and screening during regular office visits proved very favorable. The 2-year pilot screened more than 12,000 patients, half of whom were diagnosed with some kind of retinopathy. Of the 15% that required referrals to an eye doctor, 10% were for sight-threatening retinopathy. The study was so successful that it is now being expanded to include 100 clinics and 100,000 patients across the state.9
In another program, the Veterans Health Administration combined a technology platform and clinical pathway to allow for an effective means to screen patients for sight-threatening diabetic retinopathy. During the first year of the program there were 74,414 unique patients who were imaged at approximately 150 sites. Patients universally liked the fact that the retinal images did not require dilation. Most patients indicated that they would be more likely to return for an annual visit if they only needed to be imaged.10
Background/Methods
The aim of our teleophthalmology project was to develop a flexible, modular, mobile method for screening individuals that could be used effectively in a variety of medical and community settings.
An exempt institutional review board research study was approved by the University of Pittsburgh Investigational Review Board to assess the capabilities and effectiveness of the technology and workflow process being created to support a teleophthalmology screening program for diabetic retinopathy. Throughout the project, research study observations and feedback contributed to improvements in the technology and workflow. To assess the impact of the teleophthalomology project on individuals with known diabetes, subjects were recruited for a diabetes research study.
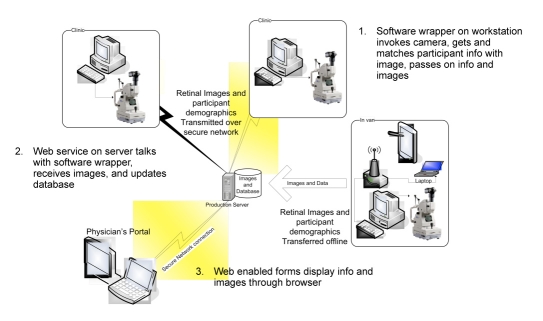
Software components were developed using basic architectural decisions about middleware, security, timing, portability, and the organization of data. Figure 1 illustrates the approaches taken to meet these requirements.
Figure 1.
Software components were developed using basic architectural decisions about middleware, security, timing, portability, and the organization of data.
The teleophthalmology system was designed to gather medical information efficiently, transmit it to the secure database, merge digital images of the retina into the database, and make the merged sets available in a central location from which a specialist could perform a follow-up examination at his/her convenience. The system included four separate software components: registration, imaging, grading, and tracking/reporting.
The software used to accomplish requirements for the registration, grading, and tracking/reporting as Web pages was coded in Microsoft's ASP.Net 2.0 using C#. The database chosen to integrate all data and images was Microsoft's SQL Server 2003. Standard wireless encryption protocols were used within a router, when in the field, and the portable server was protected by physical security at all times, as were all workstations (in locked cabinets).
The registration component, accessible from a common server, allowed efficient registration of new patients, including the collection of demographics and elements of medical history pertinent to diabetes and eye conditions. At health fairs, with groups of patients, multiple registrars used tablets accessing the server over a wireless encrypted connection to meet the demand.
The imaging component consisted of a custom Windows application (primarily in Asp.Net Using C#) wrapping the proprietary software running on a dedicated work-station attached to a nonmydriatic fundus Topcon IMAGEnet 2000 LITE (Topcon, Medical Systems, Inc., Paramus, NJ) camera that drove retinal image acquisition. This application was purposely coded so as to encapsulate the camera instructions, enabling the project to support a change in equipment with minimal reprogramming. Using a Web service to access the database, a worklist was created from registration data of patients who were ready to be imaged. The imager clicked on the patient being imaged and was shown a screen that supported taking photographs of up to three retinal images of each eye, in any order. Comments, additional or unique attributes, and any technical issues that may have been encountered could be added to the patient's record. Once the images were captured, another Web service was used to transfer the retinal images, using secure anonymous file names, to the designated server containing the database. Data captured in the field, at health fairs or local clinics, were then transferred via a secure intranet and merged into a central, secure database server, currently using a semiautomated script.
The patient's entire examination (i.e., retinal images and patient data) was “packaged” together and transferred to a designated, central server. The grading component allowed the specialist to access the server via a secure intranet connection to view a worklist of patients. The grader selected a patient, with either graded or ungraded images, and reviewed patient specific data and images. Both the selection and the grading screens were Web pages. On the grading screen, the specialist could enlarge each retinal image to “full page” for closer examination. Based on analysis of the images, the level of retinopathy, maculopathy, quality of images, and recommendations for follow-up eye care were recorded and saved in the database. A report fitting on 8½ × 11″ paper could be generated in Word for printing, emailing, or storing in a patient's e-record. For graded patients, results of a quality assurance review could also be saved.
The tracking/reporting component consisted of another set of Web pages used for recording follow-up communications with the patient and for generating statistical reports for the screened populations. Clinic staff could efficiently track information regarding graded and ungraded image sets. This information contributed to efficient follow-up communications with patients regarding their examination and compliance with recommendations for care. Reports were simple statistics based on date or range selections showing characteristics such as racial and/or geographic diversity and processing (from registration through imaging) time.
Images were taken at two University of Pittsburgh Medical Center (UPMC) clinics and at remote locations throughout southwestern Pennsylvania. UPMC served as a favorable test bed for determining the feasibility and scalability of large-scale implementation of the teleophthalmology systems in a complex health care environment. After prototype testing with approximately 500 patients, registration, imaging, and grading components were upgraded and combined into a true Web application, with log-in verifications. Controls were added to support specific patient searching, as well as maintenance screens to allow quick changes in many drop-down selections on the grading screens. The capability of interfacing directly with a standard Digital Imaging and Communications in Medicine image storage system and attaching reports automatically to the patient e-record exists, but requires further definition and negotiation.
Our study employed “single-field” fundus imaging. The images were centered on the macula. The image sequence was varied between the eyes so that in some patients the right eye was imaged first, whereas in other patients, the left eye was imaged first. This was done in case the flash of the camera, when imaging the first eye, induced significant miosis (small pupil), such that the second eye could not be imaged.
The imagers, all without previous ophthalmic photography experience, were specifically selected in order to demonstrate that a diabetic screening program could be performed without utilizing expert fundus photographers. The imagers were not certified, but the quality of their images was monitored by the reader. The imagers were trained by experienced ophthalmic photographers. The reader was a retina fellowship-trained, board-certified ophthalmologist.
All diabetic retinal lesions were identified and documented. However, there was no attempt to actually classify or impart a specific “level of retinopathy” based on the findings in a single-field study. Although these findings could be loosely associated with a level of retinopathy, there was no attempt to do so. Based on the observed diabetic lesions, a recommendation for referral was made.
Our study had four levels of referral criteria. One year: few retinal hemorrhages or macroaneurysms [(no or mild nonproliferative diabetic retinopathy (NPDR)]. Six months: same as 1 year and cotton wool spots (moderate NPDR and no macular edema). Three months: same as 6 months plus venous beading, intraretinal microvascular anomalies, and more extensive hemorrhages (severe NPDR and no macular edema). As soon as possible (later modified to 6 weeks): retinal/disc neovascularization, preretinal hemorrhages, proliferative diabetic retinopathy and/or hard exudates, cystic changes, extensive hemorrhages, and microaneurysms in the macula (macular edema).
Coincidental ocular conditions, including optic nerve cupping suspicious for glaucoma, macular drusen consistent with age-related macular degeneration, optic nerve swelling consistent with papilledema or pseudotumor cerebri, and one case of lipemia retinalis, were also documented.
Results
An evaluation team from the University of Pittsburgh's Department of Biomedical Informatics was contracted to assess the capabilities and effectiveness of the technology and workflow process being created to support a teleophthalmology screening program for diabetic retinopathy. The study involved behavioral observations, conducting focus groups, and analyzing screening activity reports and participant surveys. By focusing on assembly/disassembly procedures, workflow processes, and workflow environments, the evaluation team identified potential barriers to be removed in order to maximize the success of the project.
Observations occurred in both community and clinical settings. Diabetic retinal screening began in August 2005 in conjunction with the Healthy 4 Life and American Diabetes Association Expo held at the David L. Lawrence Convention Center, Pittsburgh, Pennsylvania. Tele-ophthalmology software, equipment, and staff were used to consent, register, image, and subsequently grade eye images. This was the first of many visits to community sites. Both urban and rural locations within Pittsburgh and surrounding areas were visited to observe workflow and make improvement suggestions. Cameras were also installed at two clinic sites: General Internal Medicine (GIM) Clinic at UPMC Montefiore Hospital in November 2005 and the Center for Diabetes and Endocrinology, Falk Clinic at the University of Pittsburgh Medical Center Presbyterian Hospital in February 2006.
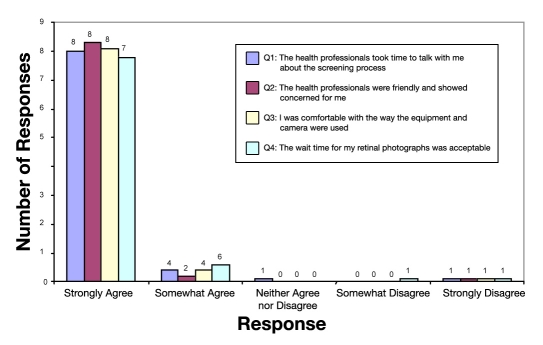
During several of the initial community events in which screening occurred, the evaluation team observed that a variety of problems occurred during the assembly/disassembly process, as well as the workflow. Staff encountered problems in assembling the camera system and making the proper connections to the computer. Software log-in problems also occurred, and software technologists were often not on site to address the issues. As a result, patients became irritable and often left without being imaged. These issues were addressed in three ways. First, a camera/local area network (LAN) assembly manual was created. Second, software personnel were notified of the problems and staff was trained thoroughly. The last intervention was the assembly of mobile carts that allowed the system to be assembled and maintained in a mobile compartment. This greatly reduced on-site set-up time by minimizing connections; staff would only have to plug the system into a power source and connect the camera to the computer via a Universal Serial Bus cord. After addressing these concerns, the evaluation team conducted surveys in order to obtain satisfaction data. Eighty-six study participants volunteered to complete a survey. The results of these surveys can be found in Figure 2.
Figure 2.
Cumulative teleophthalmology patient satisfaction surveys results (n = 86).
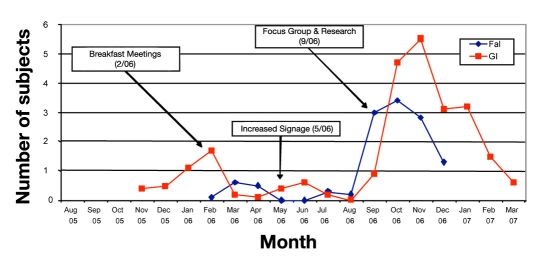
During the clinical observations, four interventions occurred. The first was a series of breakfast meetings held in February 2006. These helped indoctrinate the medical staff to the project. Second, in May 2006, the clinics began to display a poster advertising fast, easy, and no-eye-drops-required eye screenings for patients with diabetes. The third intervention occurred in September 2006 when focus groups were held at each clinic. These were held early in the morning during clinic preparation. Participants attended as their time allowed. Questions for discussion included “Are consent forms readily available?,” “Any comments from patients or doctors?,” “Has everyone met imaging personnel?,” “Are posters available?,” and “What can we do to help?”
Information from the focus group identified multiple recruitment barriers within the clinic. One barrier was that patients were often in a hurry to complete their visit and did not wish to be screened by staff. Another barrier was that clinicians often forgot about the diabetic retinopathy screening project and thus did not ask their patients to participate. From these focus groups, it was deemed appropriate to increase signage regarding the study at both clinics in order to remind physicians to tell their patients about available screening, as well as to increase patient curiosity for the diabetic screening project. The fourth intervention, which also occurred in September 2006, may have had the most impact. In GIM, patients were asked to complete health questions on an electronic tablet. Immediately after they were asked if they had diabetes, they were asked if they would be interested in a diabetic retinal screening study. If the patient chose yes, the tablet sent an electronic page to the project coordinator and consent could be obtained. Patient recruitment increased once this automatic paging protocol was implemented. The Falk Clinic incorporated a similar question on a hard copy medical history form that the patient was routinely asked to complete. Screening rates are available for GIM only. From September 2006 through March 2007, 635 patients with diabetes were given the electronic question and 195 or 31% were imaged. The intervention impact on recruitment is displayed in Figure 3. Participation declined at GIM for several reasons: holiday season, onslaught of winter weather, and the fact that the majority of the patients with diabetes who were interested in the study had already been imaged. Participation at the Falk Clinic declined due to the fact that their offices moved and were not set up again to take images.
Figure 3.
Clinic recruitment by month highlighting four interventions and subsequent effects.
The diabetes research study enrolled 706 patients with diabetes. Eighty-five percent or 599 examinations were able to be graded. Six patients (less than 1%) were recommended to see their eye doctor within 6 weeks. The average time to process a patient was just 12.88 minutes. Demographics and select outcomes are presented in Tables 1 and 2, respectively.
Table 1.
Demographics
| Demographics | Falk Clinic (n = 122) | General Internal Medicine (n = 247) | Community (n = 337) |
|---|---|---|---|
| Gender | |||
|
60 (51%) | 122 (49%) | 132 (39%) |
|
62 (49%) | 125 (51%) | 205 (61%) |
| Mean age in years | 51 | 57 | 61 |
| Race | |||
|
89 (73%) | 132 (53%) | 265 (78%) |
|
28 (23%) | 102 (41%) | 64 (19%) |
|
1 (1%) | 2 (1%) | 3 (1%) |
|
3 (2%) | — | 3 (1%) |
|
1 (1%) | 1 (1%) | — |
|
— | 10 (4%) | 2 (1%) |
| Diabetes | |||
|
44 (36%) | 18 (7%) | 21 (6%) |
|
78 (64%) | 229 (93%) | 316 (94% |
| Mean duration in years | 13 | 10 | 8 |
| Mean hemoglobin percentage A1c | 7.4 | 7.3 | 7.2 |
| Mean time in minutes | 18.1 | 11.4 | 12.0 |
| Last eye examination | |||
|
3 (2%) | 4 (2%) | 15 (5%) |
|
5 (4%) | 24 (10%) | 25 (7%) |
|
19 (16%) | 28 (11%) | 32 (10%) |
|
41 (34%) | 73 (29%) | 71 (21%) |
|
51 (42%) | 111 (45%) | 173 (51%) |
|
3 (2%) | 4 (2%) | 18 (5%) |
|
— | 3 (1%) | 3 (1%) |
Table 2.
Select Outcomes
| Follow-up and compliance results | Falk Clinic (n = 111) | General Internal Medicine (n = 199) | Community (n = 289) |
|---|---|---|---|
| Follow-up recommendations | |||
|
2 (2%) | 2 (1%) | 2 (1%) |
|
10 (9%) | 6 (3%) | 11 (4%) |
|
5 (4%) | 10 (5%) | 13 (5%) |
|
94 (85%) | 181 (91%) | 263 (91%) |
| Compliance with follow-up recommendations | |||
|
45 (41%) | 70 (35%) | 114 (39%) |
|
27 (24%) | 47 (24%) | 58 (20%) |
|
19 (17%) | 30 (15%) | 52 (18%) |
|
20 (18%) | 52 (26%) | 65 (23%) |
Discussion
System software continues to be used by the diabetes research study in UPMC clinics and at health fairs throughout the greater Pittsburgh area, with images and metadata transfers to the designated server. The system design can easily enable the transfer of data packages to a corporate digital image archive system or alternative servers in the future. Full corporate application is, however, a complex undertaking, requiring the integration of information systems, image systems, image archives, and specialized image viewing software.
Because of the success of recruitment using the electronic tablet in clinical settings, it may be useful to have automatic alerts go off in the electronic health record that prompt clinicians to schedule eye examinations yearly for their patients. This may increase patient treatment compliance greatly.
Once problems in assembly and workflow were addressed, the mobile unit proved to be a useful tool for screening diabetic patients for retinopathy. The community portion accounted for 47.7% of our study population. Staff trained to overcome technical problems, such as LAN connection issues and camera operation issues, can provide a valuable service for diabetic patients. Because the procedure is noninvasive and does not require dilation, it may be possible to expand the project to provide services to all types of patients, not just those with diabetes.
The average glycosylated hemoglobin percentage was 7.3, which is 0.3% higher than the American Diabetes Association-suggested level for diabetic patients. Even though eye examinations are recommended annually for patients with diabetes, more than 47% of our study population had their last eye examination more than a year before being screened. The presence of a higher-than-recommended glycosylated hemoglobin percentage and the lack of annual screenings may suggest a greater need for diabetes maintenance education. Because patients with diabetes are encouraged to receive annual eye examinations, the 1-year recommendation rating was used for patients who had no retinopathy present in their eyes. Seventy-six percent of the participants who were screened had a 1-year follow-up recommendation. These data may suggest that we are screening a “worried-well” population. Our mobile system was deployed to various community events focused around diabetes; however, our study may have only screened patients who were already more interested in attending health fairs and more likely to get their eyes checked. Future programs may want to use the camera system to screen the general population for diabetic retinopathy in an effort to screen people who may not be aware that they have diabetes.
Alternative applications of the prototype system are currently under consideration, and UPMC ophthalmologists are meeting with health plan administrators and optical businesses to strategize the incorporation of routine screenings into preventative health care curriculums.
Abbreviations
- BRFSS
Behavioral Risk Factor Surveillance System
- GIM
General Internal Medicine
- LAN
local area network
- NPDR
nonproliferative diabetic retinopathy
- UPMC
University of Pittsburgh Medical Center
Funding
This work was supported by funding from the U.S. Air Force administered by the U.S. Army Medical Research Acquisition Activity, Fort Detrick, Maryland (Award No. W81XWH-04-2-0030 and Contract No. DAMD 17-0302-0017).
Disclaimer
The content of the information does not imply U.S. Air Force or Government endorsement of factual accuracy or opinion.
References
- 1.National Institute of Diabetes and Digestive and Kidney Diseases. National Diabetes Statistics fact sheet: general information and national estimates on diabetes in the United States, 2005. Bethesda, MD: U.S. Department of Health and Human Services, National Institute of Health; 2005. [Google Scholar]
- 2.Narayan KM, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk for diabetes mellitus in the United States. JAMA. 2003;290(14):1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 3. The National Eye Institute (NEI) online resource guide adapted from Don't Lose Sight of Diabetic Eye Disease (NIH Publication No. 04–3252) and Diabetic Retinopathy: What You Should Know (NIH Publication No. 03–2171)[accessed 2008 Mar]. Available from: http://www.nei.nih.gov/health/diabetic/retinopathy.asp.
- 4.Executive summary: standards of medical care in diabetes-2008. Diabetes Care. 2008;31:S5–S11. doi: 10.2337/dc14-S005. [DOI] [PubMed] [Google Scholar]
- 5.Levels of diabetes-related preventive-care practices—-United Sates, 1997–1999. MMWR Morb Mortal Wkly Rep. 2000;49(42):954–959. [PubMed] [Google Scholar]
- 6.Phillips MM. Targeting diabetes preventive care programs: insights from the 2001 behavioral risk factor surveillance survey. Prev Chronic Dis. 2004;1(1):A07. [PMC free article] [PubMed] [Google Scholar]
- 7.Chronic Disease Indicators. National Center for Chronic Disease Prevention and Health [accessed 2008 Mar]. Available from: http://apps.nccd.cdc.gov/cdi/IndDefinition.aspx?IndicatorDefinitionID=34.
- 8.Lipp E. Telemedicine: will it ease the burden on the retina community? Retinal Physician. 2006 Mar–Apr [Google Scholar]
- 9. California HealthCare Foundation (CHCF), chronic disease care, technology-—diabetic retinopathy screening report [accessed 2007 Dec]. Available from: http://www.chcf.org/topics/chronicdisease/index.cfm?itemID=133378.
- 10.Cavallerano AA, Conlin PR. Teleretinal imaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol. 2008;2(1):33–39. doi: 10.1177/193229680800200106. [DOI] [PMC free article] [PubMed] [Google Scholar]