Abstract
Synthetic polymer coatings are used extensively in modern medical devices and implants because of their material versatility and processability. These coatings are designed for specific applications by controlling composition and physical and chemical properties, and they can be formed into a variety of complex structures and shapes. However, implantation of these materials into the body elicits a strong inflammatory host response that significantly limits the integration and biological performance of devices. Biomaterial-mediated inflammation is a complex reaction involving protein adsorption, leukocyte recruitment and activation, secretion of inflammatory mediators, and fibrous encapsulation of the implant. Significant research efforts have focused on modifying material properties using various anti-inflammatory polymeric surface coatings to generate more biocompatible implants. This minireview provides a brief background on the events of biomaterial-mediated inflammation and highlights various approaches used for modifying material surfaces to modulate inflammatory responses. These include both passive and active strategies, such as nonfouling surface treatments and delivery of anti-inflammatory agents, respectively. Novel approaches will be needed to extend the in vivo lifetime and performance of devices and reduce the need for multiple implantation surgeries.
Keywords: biomaterial, polymer, coating, host response, implant, anti-inflammatory
Inflammation and Device Performance
Medical devices and biomaterial implants are clinically used in a variety of applications, and their performance is critical to a patient's overall health and quality of life. Surgical procedures injure micro-vasculature and tissue surrounding the implanted device, initiating a localized nonspecific inflammatory response (Figure 1).1 Although inflammation recruits native cells for remodeling and regenerating the damaged tissue, persistent and inflammatory stimuli significantly interfere with implant function and often result in device failure. Adverse host responses to implanted biomedical devices include thrombogenic responses on vascular grafts,2,3 degradation and stress cracking of pacemaker leads,4,5 tissue fibrosis surrounding mammary prostheses,6 osteolysis and loosening of orthopedic joint prostheses,7,8 reactive gliosis around neural probes,9 and degradation in biosensor function.10
Figure 1.
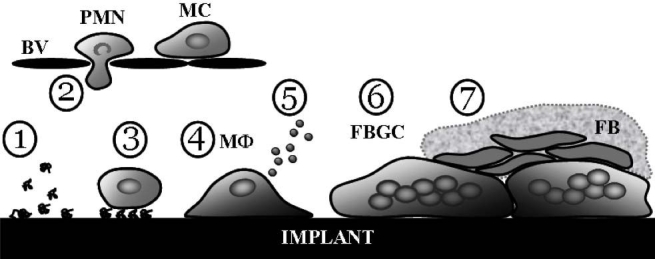
Events of host foreign body response to implanted materials. Neutrophils and monocytes recruited by stimulatory cues emigrate from the vasculature and adhere to the layer of adsorbed proteins on the implant surface (Phases 1–3). Differentiated macrophages become activated, secreting a variety of inflammatory mediators, and often fuse into multinucleated foreign body giant cells (Phases 4-6). Fibroblasts infiltrate the site and generate a collagenous fibrous capsule around the implant (Phase 7). BV, blood vessel; PMN, polymorphonuclear leukocyte; MC, immature monocyte; MΦ, differentiated macrophage; FBGC, foreign body giant cell; FB, fibroblast.
Host Foreign Body Response
Immediately following implantation, proteins and other biomolecules present in the blood plasma and biological fluids rapidly adsorb onto the surface of biomaterials. Adsorption of biomolecules from these multicomponent solutions is a dynamic process involving competition, rearrangements, and displacement of adsorbed species (the Vroman effect).11,12 Material surface chemistry often drives hydrated biomolecules to partially release bound water molecules, leading to structural changes and reversible, as well as irreversible, physisorption of biomolecules into the surface. This process occurs more rapidly than cell recruitment to the implantation site; therefore, the composition and configuration of this complex protein milieu dictates subsequent cellular responses.13–15 In many instances, adsorbed fibrinogen, IgG, and complement fragments mediate leukocyte-biomaterial interactions and subsequent inflammatory reactions.16–21
During the acute phase of this foreign body reaction (FBR), circulating polymorphonuclear leukocytes (e.g., neutrophils) are stimulated in response to inflammatory signals released at the implant site. This results in integrin receptor-mediated leukocyte recruitment, adhesion, and activation.22–24 Short-lived neutrophils are then replaced by inflammatory monocytes and macrophages. The layer of surface-adsorbed proteins modulates macrophage phenotype and subsequent functions, including phagocytosis, cytokine expression, and fusion into foreign body giant cells (FBGCs).14,15 Macrophages are considered the key mediators of implant-associated inflammation due to their distribution and motility, and they generate a multitude of biologically active products.25,26 They play central roles in directing both inflammatory and regenerative responses associated with implanted biomaterials.27–29
Persistent inflammatory stimuli lead to insufficient healing of local tissue at the device interface. The hallmark of a chronic response is fusion of monocyte-derived macrophages to form multinucleated FBGCs, a complex process involving myriad molecules.30,31 Foreign body giant cells have been implicated in the biodegradation of polymeric implants through surface oxidation and enzymatic degradation.32–34 Additionally, fibroblasts recruited to the implant site generate a thick collagenous fibrous capsule around the implant. For a detailed explanation of the cellular and molecular mediators of the host foreign body response to biomaterials, we refer the reader to an excellent review provided by Anderson et al.31 These cellular and tissue responses often impair in vivo device performance. In the case of indwelling biosensors, including continuous glucose sensors, cell-mediated inflammatory responses and fibrous scarring adversely impact sensor performance, including fluctuations in biosensor sensitivity, decreased response time, and material degradation.35–37
Accurate performance of glucose biosensors is critical to monitoring patient health, because diabetes is among the leading causes of death in the United States.38 Since the 1980s, a number of methods have been utilized to generate more biocompatible biosensors, including flow-based systems, Nafion membranes, and diamond-like carbon coatings.37 However, many glucose sensors only function reliably for a few days in vivo before failing.39 It has been suggested that these implants may require a stabilization period during fibrous capsule development, resulting in erroneous analyte measurements for weeks after implantation.40,41 Current limitations on device performance necessitate a new generation of coatings that are applicable to a wide variety of implantable materials. Novel, probably multipronged, approaches are needed to abrogate long-term inflammatory responses and extend the in vivo lifetime of medical implants in order to avoid the need for multiple surgical procedures.
Anti-Inflammatory Coating Strategies
The severity and extent of the biological response to an implanted biomaterial or device influences the probability for its successful integration with surrounding tissue, as well as overall device performance. Initial stages of the FBR are dictated largely by the extent of injury and surgical technique, implantation site, implant shape and size, material chemical and physical properties, and local and systemic health of the recipient.1,42–44 Significant research efforts have focused on modifying material properties using various anti-inflammatory surface coatings to generate more biocompatible implants.
Passive Strategies: Nonfouling Surface Treatments
The initial stages of the FBR involve nonspecific protein and biomolecule adsorption and subsequent leukocyte adhesion onto the biomaterial surface, events termed “biofouling.” It is generally believed that reducing biofouling can ameliorate subsequent adverse inflammatory responses such as leukocyte activation and tissue fibrosis. Several passive strategies have been explored to achieve this goal, including preadsorption of material surfaces with less inflammatory proteins or cells. Such passivation strategies are attractive, because they are relatively straightforward and simple.45,46 However, these coatings suffer from a lack of stability as other proteins, such as fibrinogen, can passively displace preadsorbed proteins such as albumin. Even covalently-tethered nonadhesive proteins can be degraded by leukocytes, resulting in deposition of proinflammatory adhesive components. Approaches involving cell deposition onto surfaces prior to implantation offer a possible strategy to promote wound healing by encouraging mass transport and reducing fibrotic responses at the tissue–implant interface.47 However, issues related to cell sourcing, host responses to the donor cells, and long-term stability limit these strategies.
Nonfouling (protein adsorption-resistant) thin-layer polymeric coatings offer more substantial routes to reduce acute inflammatory responses. The design requirements for implanted materials and devices vary considerably depending on the in vivo application and site of implantation. In particular, nonfouling polymeric surface coatings for implantable biosensors must ideally conform to the following considerations:
use of nontoxic materials
effectively prevent in vivo biofouling
appropriate thickness and permeability to allow analyte detection
techniques to deposit coating onto a variety of materials and architectures
mechanical, chemical, and electrical stability to withstand surface deposition, sterilization methods, implantation procedures, and in vivo environment.
Despite considerable research efforts, surface coatings that completely eliminate protein adsorption over the lifetime of a device have not been attained. Nevertheless, significant progress has been made in understanding the mechanisms driving protein adsorption, and several chemical groups that resist protein adsorption have been identified. Polyethylene glycol (PEG, [CH2CH2O]n) has proven to be the most protein-resistant functionality and remains the standard for comparison (Figure 2).48 Polyethylene glycol chain density, length, and conformation strongly influence resistance to protein adsorption.49–51 The mechanism of resistance to protein adsorption by PEG surfaces probably involves a combination of the ability of the polymer chain to retain interfacial water and the resistance of the polymer chain to compression due to its tendency to remain an extended coil conformation.52–54 Other hydrophilic polymers, such as poly(2-hydroxyethyl methacrylate),55 poly(N-isopropyl acrylamide),56,57 poly(acrylamide), and phosphoryl choline-based polymers58–61 also resist protein adsorption. In addition, mannitol, oligomaltose, and taurine groups have emerged as promising moieties to prevent protein adsorption.62–64
Figure 2.
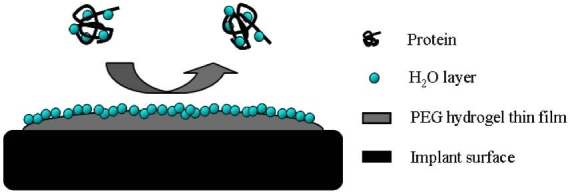
Passive anti-inflammatory surface coating for biomaterials. Hydrophilic polymeric coatings, such as PEG-based hydrogels, retain interfacial water molecules, rendering them highly resistant to protein adsorption.
These coatings have been applied as molecularly thin self-assembled monolayers (SAMs), polymer brushes, and thin or bulk hydrogels (Table 1) capable of reducing protein adsorption and leukocyte adhesion. Self-assembled monolayers are confined to inorganic planar surfaces and are only stable short-term in aqueous environments, limiting their use as coatings for in vivo biosensors.65 Polymer brushes are more mechanically robust than SAMs and can be generated on nonplanar surfaces, including colloidal suspensions and polymeric substrates. Moreover, surface-initiated polymerizations allow control over functionality, grafting density, and thickness of the brushes.66,67 Extensive research efforts have focused on hydrogel-based implant coatings. Hydrogels offer many advantages over traditional surface modification strategies, including a viscoelastic network structure, tunable material characteristics, incorporation of multiple chemical functionalities, nanoscale dimensions with complex architectures, and the ability to deposit onto a variety of material substrates.68–72
Table 1.
Examples of Nonfouling Ethylene Glycol-Based Surface Treatments
| Coating Structure | Selected References |
|---|---|
| SAM | Prime and Whitesides65 (1993)a |
| Chapman et al.77 (2001)a | |
| Zhang et al.78 (2001)a | |
| Polymer Brush or Surface Graft | Espadas-Torre and Meyerhoff79 (1995)a |
| Lee et al.80 (1997)a | |
| Du et al.81 (1997)a | |
| Zhang et al.82 (1998)a | |
| Jenney and Anderson83 (1999)a | |
| Shen et al.84 (2001)a | |
| Otsuka et al.85 (2001)a | |
| Boulmedais et al.86 (2004)a | |
| Ma et al.87 (2004)a | |
| Ma et al.88 (2006)a | |
| Zhou et al.89 (2007)a | |
| Waku et al.90 (2007)a | |
| Cao et al.91 (2007)a | |
| Hydrogel | West and Hubbell92 (1995) |
| Quinn et al.73 (1995) | |
| Quinn et al.93 (1997) | |
| Collier et al.94 (2004)a | |
| Nolan et al.56 (2005)a | |
| Singh et al.57 (2007)a | |
| Bridges et al.95 (2008) | |
| Yu et al.96 (2008) | |
Materials were tested only in vitro.
Although many of these coatings exhibit reduced protein adsorption and leukocyte adhesion in vitro, inconsistent results have been obtained regarding the ability of these polymeric coatings to reduce in vivo acute and chronic inflammatory responses.73–76 Possible explanations for the mixed in vivo results with these coatings include insufficient nonfouling behavior, coating degradation, and inflammatory mechanism(s) independent from protein adsorption. These results have motivated the development of active anti-inflammatory strategies.
Active Strategies: Delivery of Anti-Inflammatory Agents
In contrast to passive nonfouling surface treatments, coatings presenting or delivering anti-inflammatory agents offer a more interactive and directed approach to modulate cell behavior. Broad-spectrum drugs have typically been used to control chronic tissue inflammation. However, orally administered drugs may not achieve adequate local concentrations, and their long-term systemic use can cause major side effects. Therefore it is desirable to deliver therapeutics locally in a controlled, site-specific manner to improve the tissue–material response.
Various immunomodulatory agents can be immobilized onto nonfouling polymeric coatings or delivered in soluble form from the coating (Figure 3). Possible strategies for the controlled release of agents include passive diffusion from coatings or polyelectrolyte layers,97,98 bioerodible/degradable coatings to release drugs by passive dissolution,99 swelling coatings that release drugs by passive mechanisms, and hydrolysable or enzyme-degradable linkages to release the agent.100–103 These delivery systems offer several advantages over passive methods, including highly controlled presentation of immunomodulatory agents, control over reaction kinetics, and versatility through hybrid designs. In addition to the basic requirements for passive coatings, designs for these bioactive coatings must consider the following properties:
retain bioactivity of anti-inflammatory molecules for the intended lifetime
optimal tethering distance for recognition of immobilized agents
appropriate release profiles in terms of amounts, rates, total dosage, and release time (acute versus chronic release)
drug character (e.g., hydrophobicity), residence times, and stability
safety issues related to drug release (designed or accidental)
agent–matrix (coating) interactions
effects of material sterilization.
Figure 3.
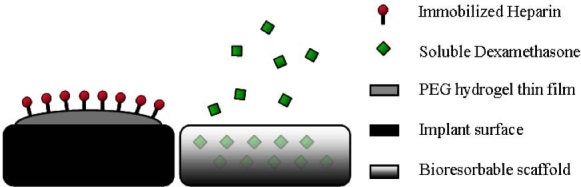
Bioactive implant coatings to deliver anti-inflammatory molecules. Representative schemes depict mechanisms for the active delivery of various immunomodulatory agents to reduce leukocyte adhesion and activation.
Examples of anti-inflammatory factors delivered from surface coatings are summarized in Table 2. Dexamethasone (DEX) is a synthetic glucocorticoid hormone with many applications in biomedical research, including treatment of inflammatory responses.104 Dexamethasone modulates macrophage behavior and reduces the levels of numerous proinflammatory cytokines, including tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, and interferon-γ.105,106 Dexamethasone-releasing coatings have reduced tissue inflammation and cell activation surrounding implanted glucose biosensors and neural implants.107–110 In addition, polypyrrole-based electrode coatings designed to electrically control delivery of DEX lowered the amount of reactive astrocytes in vitro.111
Table 2.
Active Surface Treatments for Biomaterial Coatings
| Agent | Delivery Mechanism | Selected References |
|---|---|---|
| DEX | electrochemical release | Wadhwa et al.111 (2006)a |
| passive release | Kim and Martin109 (2006) | |
| passive release | Norton et al.107 (2007) | |
| passive release | Zhong and Bellamkonda108 (2007) | |
| passive release | Patil et al.110 (2007) | |
| α-MSH | passive release | Benkirane-Jessel et al.97 (2004)a |
| passive release | Schultz et al.98 (2005) | |
| passive release | Zhong and Bellamkonda118 (2005)a | |
| surface immobilization | He et al.120 (2007) | |
| Heparin | surface immobilization | Gerritsen et al.121 (2000) |
| surface immobilization | Wang et al.122 (2003)a | |
| surface immobilization | van Bilsen et al.115 (2004) | |
| surface immobilization | Sung et al.123 (2004)a | |
| surface immobilization | Fu et al.124 (2005)a | |
| surface immobilization | Rele et al.116 (2005) | |
| surface immobilization | Tseng et al.117 (2006)a | |
| surface immobilization | Du et al.114 (2007)a | |
| IL-1Ra | immobilized or soluble | Kim et al.125 (2007)a |
| Superoxide dismutase mimetics | surface immobilization | Udipi et al.119 (2000) |
| Curcumin | passive release | Nguyen et al.126 (2004)a |
| passive release | Su et al.127 (2005)a | |
| passive release | Pan et al.128 (2006)a | |
| Vitamin E | passive release | Hahn et al.129 (2004)a |
Materials were tested only in vitro.
Heparin is a highly sulfated glycosaminoglycan with strong anticoagulant activity, and it also exhibits anti-inflammatory properties. It is synthesized and secreted by mast cells at sites of infection and inhibits endotoxin-induced monocyte activation.112 Heparin pretreatment significantly attenuates leukocyte transmigration through its actions on P- and L-selectin and the leukocyte-specific αMβ2 integrin, and it also binds cytokines and suppresses superoxide generation by neutrophils.112,113 Heparin-based coatings have reduced protein adsorption and leukocyte recruitment.114–117
Alpha melanocyte-stimulating hormone (α-MSH) is an endogenous linear peptide with potent anti-inflammatory properties. In vitro, α-MSH reduced levels of pro-inflammatory TNF-α while increasing levels of anti-inflammatory IL-10 in stimulated human monocytes.97 It stimulated production of the anti-inflammatory cytokine IL-10 and revealed a less obstructive cell layer on coatings for tracheal prostheses.98 In addition, α-MSH inhibited nitric oxide production by stimulated microglia and reduced the magnitude of electrical impedance of neural implants.118
Superoxide anions are potent cytotoxic oxidants secreted during macrophage phagocytosis. Superoxide dismutase is an endogenous scavenger enzyme that catalyzes its breakdown into less reactive hydrogen peroxide and oxygen. Superoxide dismutase mimetics were developed as an anti-inflammatory mechanism. When covalently attached to ultrahigh molecular weight polyethylene, neutrophil recruitment was significantly reduced.119
Receptor antagonists, antibodies, and soluble receptors are endogenous molecules that competitively inhibit binding to the corresponding agonist, effectively acting as a molecular trap. Decoy antagonists have been developed against proinflammatory cytokines, such as IL-1, as a strategy to regulate inflammation.130,131 In one interesting study, a fusion protein of recombinant human IL-1 receptor antagonist and elastin-like polypeptide was covalently immobilized onto SAMs.125 This fusion protein was able to prevent endotoxin-stimulated human monocytes from differentiating and reduced the expression of proinflammatory cytokines while increasing the production of anti-inflammatory and pro-wound-healing cytokines. Additional therapeutic strategies include inhibition of intracellular signaling cascades that result in cytokine production and the application of anti-inflammatory cytokines such as IL-10.132 It is highly desirable to develop methods for targeting delivery of anti-inflammatory factors in order to limit systemic adverse effects and concentrate therapeutic molecules at sites of inflammation.
Novel approaches for controlled delivery of immuno-modulatory proteins have been enabled by the development of micro- and nanoparticles of biodegradable polymers.133,134 Biodegradable polymeric microspheres have been utilized for sustained delivery of IL-1Ra, which effectively inhibited production of pro-inflammatory cytokines.135 Synthetic thrombin receptor (PAR1) agonist peptide encapsulated in biodegradable microspheres shortened the inflammatory phase and accelerated tissue healing in a rat ulcer model.136 Short half-lives and requirements for high dosing frequencies limit the use of therapeutic proteins; however, PEGylation strategies have been investigated as a potential approach to extend the therapeutic lifetime of molecules such as IL-1Ra.137 Using layer-by-layer deposition techniques, Pierstorff et al. have developed a copolymer nanofilm system as a multifunctional platform to release a variety of anti-inflammatory drugs; additionally, it may be possible to functionalize these agents onto implant surfaces to enhance delivery specificity over traditional systemic drug administration.138
Using small polymeric carriers complexed with oligonucleotides, including small interfering ribonucleic acid to silence harmful genes, cellular uptake of anti-inflammatory agents can be optimized.139,140 Delivery of nucleic acid structures has proven to be an effective strategy to downregulate specific endogenous inflammatory factors.141–145 These approaches may create less inflammatory macrophages and attract wound-healing cells. In one particular case, multilayered polyelectrolyte assemblies complexed with deoxyribonucleic acid (DNA) were coated onto intravascular stents;146 this process could be extended to incorporate DNA encoding a variety of anti-inflammatory mediators. Although many of these techniques utilize micro- and nanoscale polymeric systems to deliver biomolecules, similar strategies could be implemented to develop anti-inflammatory coatings for biomaterials and implants as a general platform to release nucleic acid-based therapeutics at sites of inflammation.
Existing Considerations and Future Prospects
Biomaterial-mediated inflammation poses a complex problem, limiting the function of implanted devices and influencing overall patient health. Significant efforts have focused on developing passive nonfouling surface treatments to prevent protein adsorption and leukocyte adhesion, as well as active mechanistic approaches for the delivery of anti-inflammatory agents. While these coating technologies have reduced protein adsorption and cell adhesion in vitro, considerable fibrous encapsulation and adverse inflammatory responses are still evident following implantation.107,115,147 These marginal reductions in adverse inflammation can be attributed to persistent leukocyte adhesion and activation in vivo and suboptimal pharmacodelivery.74,107
Although current polymeric coatings successfully modulate acute inflammatory events, new strategies will be critical to extend the in vivo lifetime and performance of implanted devices. Coating designs will probably need to be material and application-specific in order to achieve the desired in vivo response. Biologically interactive implants are gaining considerable interest. Tunable, stimuli-responsive materials and biomimetic molecules may be able to actively direct cell behavior and activity surrounding the implant, encouraging more desirable interactions.68,69 In addition, these “smart” materials will lend a higher degree of sensitivity and specificity to polymeric coatings, enabling tighter control over pharmacokinetics and complex dosing schemes using multiple biomolecules or drugs. For example, the use of anti-inflammatory polymeric carrier systems enables modifications, including biomolecule conjugation, which may promote targeted delivery of therapeutics to specific cells or tissues.139 In addition, these systems may be engineered for controlled release of anti-inflammatory cargo molecules based on external stimuli.148
It will also be important to focus on successfully integrating implanted devices with surrounding tissue and regenerating damaged microvasculature. Tissue integration is particularly important in neural and orthopedic applications.9,13 In addition, the delivery of angiogenic factors may help facilitate in vivo performance of implanted biosensors by offsetting tissue fibrosis.107,110,149 Clearly, progress in the development of effective and long-term implantable materials, including biosensors, will require the integration of multiple strategies and disciplines, as well as rigorous testing in relevant in vivo models.
Acknowledgements
Elements of this work were presented at the TATRC's Integrated Research Team meeting, “Nanotechnology Solutions for Long-Term Implantable Devices,” on October 23–25, 2007, in Houston, TX.
Abbreviations
- α-MSH
alpha melanocyte-stimulating hormone
- DEX
dexamethasone
- DNA
deoxyribonucleic acid
- FBGC
foreign body giant cell
- FBR
foreign body reaction
- IL
interleukin
- PEG
polyethylene glycol
- SAM
self-assembled monolayer
- TNF
tumor necrosis factor
References
- 1.Anderson JM. Biological responses to materials. Annu Rev Mater Res. 2001;31:81–110. [Google Scholar]
- 2.Gorbet MB, Sefton MV. Biomaterial-associated thrombosis: roles of coagulation factors, complement, platelets and leukocytes. Biomaterials. 2004;25:5681–5703. doi: 10.1016/j.biomaterials.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 3.Kottke-Marchant K, Anderson JM, Umemura Y, Marchant RE. Effect of albumin coating on the in vitro blood compatibility of Dacron arterial prostheses. Biomaterials. 1989;10(3):147–155. doi: 10.1016/0142-9612(89)90017-3. [DOI] [PubMed] [Google Scholar]
- 4.Sutherland K, Mahoney JR, 2nd, Coury AJ, Eaton JW. Degradation of biomaterials by phagocyte-derived oxidants. J Clin Invest. 1993;92(5):2360–2367. doi: 10.1172/JCI116841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhao Q, Topham N, Anderson JM, Hiltner A, Lodoen G, Payet CR. Foreign-body giant cells and polyurethane biostability: in vivo correlation of cell adhesion and surface cracking. J Biomed Mater Res. 1991;25(2):177–183. doi: 10.1002/jbm.820250205. [DOI] [PubMed] [Google Scholar]
- 6.Destouet JM, Monsees BS, Oser RF, Nemecek JR, Young VL, Pilgram TK. Screening mammography in 350 women with breast implants: prevalence and findings of implant complications. AJR Am J Roentgenol. 1992;159(5):973–978. doi: 10.2214/ajr.159.5.1414810. [DOI] [PubMed] [Google Scholar]
- 7.Ambrose CG, Clanton TO. Bioabsorbable implants: review of clinical experience in orthopedic surgery. Ann Biomed Eng. 2004;32(1):171–177. doi: 10.1023/b:abme.0000007802.59936.fc. [DOI] [PubMed] [Google Scholar]
- 8.Voronov I, Santerre JP, Hinek A, Callahan JW, Sandhu J, Boynton EL. Macrophage phagocytosis of polyethylene particulate in vitro. J Biomed Mater Res. 1998;39(1):40–51. doi: 10.1002/(sici)1097-4636(199801)39:1<40::aid-jbm6>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 9.McGraw J, Hiebert GW, Steeves JD. Modulating astrogliosis after neurotrauma. J Neurosci Res. 2001;63(2):109–115. doi: 10.1002/1097-4547(20010115)63:2<109::AID-JNR1002>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 10.Wisniewski N, Moussy F, Reichert WM. Characterization of implantable biosensor membrane biofouling. Fresenius J Anal Chem. 2000;366(6-7):611–621. doi: 10.1007/s002160051556. [DOI] [PubMed] [Google Scholar]
- 11.Vroman L, Adams AL, Klings M. Interactions among human blood proteins at interfaces. Fed Proc. 1971;30(5):1494–1502. [PubMed] [Google Scholar]
- 12.Xu LC, Siedlecki CA. Effects of surface wettability and contact time on protein adhesion to biomaterial surfaces. Biomaterials. 2007;28(22):3273–3283. doi: 10.1016/j.biomaterials.2007.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson CJ, Clegg RE, Leavesley DI, Pearcy MJ. Mediation of biomaterial-cell interactions by adsorbed proteins: a review. Tissue Eng. 2005;11(1-2):1–18. doi: 10.1089/ten.2005.11.1. [DOI] [PubMed] [Google Scholar]
- 14.Collier TO, Anderson JM. Protein and surface effects on monocyte and macrophage adhesion, maturation, and survival. J Biomed Mater Res. 2002;60(3):487–496. doi: 10.1002/jbm.10043. [DOI] [PubMed] [Google Scholar]
- 15.Shen M, Garcia I, Maier RV, Horbett TA. Effects of adsorbed proteins and surface chemistry on foreign body giant cell formation, tumor necrosis factor alpha release and procoagulant activity of monocytes. J Biomed Mater Res A. 2004;70(4):533–541. doi: 10.1002/jbm.a.30069. [DOI] [PubMed] [Google Scholar]
- 16.Tang L, Eaton JW. Fibrin(ogen) mediates acute inflammatory responses to biomaterials. J Exp Med. 1993;178(6):2147–2156. doi: 10.1084/jem.178.6.2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tang L, Liu L, Elwing HB. Complement activation and inflammation triggered by model biomaterial surfaces. J Biomed Mater Res. 1998;41(2):333–340. doi: 10.1002/(sici)1097-4636(199808)41:2<333::aid-jbm19>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 18.Tang L, Lucas AH, Eaton JW. Inflammatory responses to implanted polymeric biomaterials: role of surface-adsorbed immunoglobulin?G. J Lab Clin Med. 1993;122:292–300. [PubMed] [Google Scholar]
- 19.Hu WJ, Eaton JW, Ugarova TP, Tang L. Molecular basis of biomaterial-mediated foreign body reactions. Blood. 2001;98(4):1231–1238. doi: 10.1182/blood.v98.4.1231. [DOI] [PubMed] [Google Scholar]
- 20.McNally AK, Anderson JM. Complement C3 participation in monocyte adhesion to different surfaces. Proc Natl Acad Sci U S A. 1994;91(21):10119–10123. doi: 10.1073/pnas.91.21.10119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu Y, Simonovsky FI, Ratner BD, Horbett TA. The role of adsorbed fibrinogen in platelet adhesion to polyurethane surfaces: a comparison of surface hydrophobicity, protein adsorption, monoclonal antibody binding, and platelet adhesion. J Biomed Mater Res A. 2005;74(4):722–738. doi: 10.1002/jbm.a.30381. [DOI] [PubMed] [Google Scholar]
- 22.Hynes RO. Integrins: bidirectional, allosteric signaling machines. Cell. 2002;110(6):673–687. doi: 10.1016/s0092-8674(02)00971-6. [DOI] [PubMed] [Google Scholar]
- 23.McNally AK, Anderson JM. Beta1 and beta2 integrins mediate adhesion during macrophage fusion and multinucleated foreign body giant cell formation. Am J Pathol. 2002;160(2):621–630. doi: 10.1016/s0002-9440(10)64882-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ley K. The role of selectins in inflammation and disease. Trends Mol Med. 2003;9(6):263–268. doi: 10.1016/s1471-4914(03)00071-6. [DOI] [PubMed] [Google Scholar]
- 25.Thomsen P, Gretzer C. Macrophage interactions with modified material surfaces. Current Opinion in Solid State and Materials Science. 2001;5(2-3):163–176. [Google Scholar]
- 26.Nathan CF. Secretory products of macrophages. J Clin Invest. 1987;79(2):319–326. doi: 10.1172/JCI112815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3(1):23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 28.Mosser DM. The many faces of macrophage activation. J Leukoc Biol. 2003;73(2):209–212. doi: 10.1189/jlb.0602325. [DOI] [PubMed] [Google Scholar]
- 29.Mills CD, Kincaid K, Alt JM, Heilman MJ, Hill AM. M-1/M-2 macrophages and the Th1/Th2 paradigm. J Immunol. 2000;164(12):6166–6173. doi: 10.4049/jimmunol.164.12.6166. [DOI] [PubMed] [Google Scholar]
- 30.Chen EH, Grote E, Mohler W, Vignery A. Cell-cell fusion. FEBS Lett. 2007;581(11):2181–2193. doi: 10.1016/j.febslet.2007.03.033. [DOI] [PubMed] [Google Scholar]
- 31.Anderson JM, Rodriguez A, Chang DT. Foreign body reaction to biomaterials. Semin Immunol. 2008;20(2):86–100. doi: 10.1016/j.smim.2007.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Henson PM. The immunologic release of constituents from neutrophil leukocytes. II. Mechanisms of release during phagocytosis, and adherence to nonphagocytosable surfaces. J Immunol. 1971;107(6):1547–1557. [PubMed] [Google Scholar]
- 33.Henson PM. The immunologic release of constituents from neutrophil leukocytes. I. The role of antibody and complement on nonphagocytosable surfaces or phagocytosable particles. J Immunol. 1971;107(6):1535–1546. [PubMed] [Google Scholar]
- 34.Mathur AB, Collier TO, Kaw WJ, Wigging M, Schubert MA, Hiltner A, Anderson JM. In vivo biocompatibility and biostability of modified polyurethanes. J Biomed Mater Res. 1997;36(2):246–257. doi: 10.1002/(sici)1097-4636(199708)36:2<246::aid-jbm14>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 35.Gerritsen M, Jansen JA, Kros A, Nolte RJ, Lutterman JA. Performance of subcutaneously implanted glucose sensors: a review. J Invest Surg. 1998;11(3):163–174. doi: 10.3109/08941939809098031. [DOI] [PubMed] [Google Scholar]
- 36.Kyrolainen M, Rigsby P, Eddy S, Vadgama P. Bio-/haemocompatibility: implications and outcomes for sensors? Acta Anaesthesiol Scand Suppl. 1995;104:55–60. doi: 10.1111/j.1399-6576.1995.tb04255.x. [DOI] [PubMed] [Google Scholar]
- 37.Wisniewski N, Reichert M. Methods for reducing biosensor membrane biofouling. Colloids Surf B Biointerfaces. 2000;18(3-4):197–219. doi: 10.1016/s0927-7765(99)00148-4. [DOI] [PubMed] [Google Scholar]
- 38.Department of Health and Human Services, Centers for Disease Control and Prevention. Atlanta: 2005. National diabetes fact sheet: general information and national estimates on diabetes in the United States. [Google Scholar]
- 39.Gilligan BJ, Shults MC, Rhodes RK, Updike SJ. Evaluation of a subcutaneous glucose sensor out to 3 months in a dog model. Diabetes Care. 1994;17(8):882–887. doi: 10.2337/diacare.17.8.882. [DOI] [PubMed] [Google Scholar]
- 40.Updike SJ, Shults MC, Rhodes RK, Gilligan BJ, Luebow JO, von Heimburg D. Enzymatic glucose sensors. Improved long-term performance in vitro and in vivo. ASAIO J. 1994;40(2):157–163. [PubMed] [Google Scholar]
- 41.Updike SJ, Shults MC, Gilligan BJ, Rhodes RK. A subcutaneous glucose sensor with improved longevity, dynamic range, and stability of calibration. Diabetes Care. 2000;23(2):208–214. doi: 10.2337/diacare.23.2.208. [DOI] [PubMed] [Google Scholar]
- 42.Luttikhuizen DT, van Amerongen MJ, de Feijter PC, Petersen AH, Harmsen MC, van Luyn MJ. The correlation between difference in foreign body reaction between implant locations and cytokine and MMP expression. Biomaterials. 2006;27(34):5763–5770. doi: 10.1016/j.biomaterials.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 43.Andersson M, Suska F, Johansson A, Berglin M, Emanuelsson L, Elwing H, Thomsen P. Effect of molecular mobility of polymeric implants on soft tissue reactions: an in vivo study in rats. J Biomed Mater Res A. 2008;84(3):652–660. doi: 10.1002/jbm.a.31389. [DOI] [PubMed] [Google Scholar]
- 44.Nair A, Zou L, Bhattacharyya D, Timmons RB, Tang L. Species and density of implant surface chemistry affect the extent of foreign body reactions. Langmuir. 2008;24(5):2015–2024. doi: 10.1021/la7025973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Geelhood SJ, Horbett TA, Ward WK, Wood MD, Quinn MJ. Passivating protein coatings for implantable glucose sensors: evaluation of protein retention. J Biomed Mater Res B Appl Biomater. 2007;81(1):251–260. doi: 10.1002/jbm.b.30660. [DOI] [PubMed] [Google Scholar]
- 46.Amiji M, Park H, Park K. Study on the prevention of surface-induced platelet activation by albumin coating. J Biomater Sci Polym Ed. 1992;3(5):375–388. doi: 10.1163/156856292x00196. [DOI] [PubMed] [Google Scholar]
- 47.Prichard HL, Reichert WM, Klitzman B. Adult adipose-derived stem cell attachment to biomaterials. Biomaterials. 2007;28(6):936–946. doi: 10.1016/j.biomaterials.2006.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kingshott P, Griesser HJ. Surfaces that resist bioadhesion. Current Opinion in Solid State and Materials Science. 1999;4(4):403–412. [Google Scholar]
- 49.Unsworth LD, Sheardown H, Brash JL. Polyethylene oxide surfaces of variable chain density by chemisorption of PEO-thiol on gold: adsorption of proteins from plasma studied by radiolabelling and immunoblotting. Biomaterials. 2005;26(30):5927–5933. doi: 10.1016/j.biomaterials.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 50.Unsworth LD, Sheardown H, Brash JL. Protein-resistant poly(ethylene oxide)-grafted surfaces: chain density-dependent multiple mechanisms of action. Langmuir. 2008;24(5):1924–1929. doi: 10.1021/la702310t. [DOI] [PubMed] [Google Scholar]
- 51.Michel R, Pasche S, Textor M, Castner DG. Influence of PEG architecture on protein adsorption and conformation. Langmuir. 2005;21(26):12327–12332. doi: 10.1021/la051726h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Morra M. On the molecular basis of fouling resistance. J Biomater Sci Polym Ed. 2000;11(6):547–569. doi: 10.1163/156856200743869. [DOI] [PubMed] [Google Scholar]
- 53.Szleifer I. Protein adsorption on tethered polymer layers: effect of polymer chain architecture and composition. Physica A. 1997;244(1-4):370–388. [Google Scholar]
- 54.Szleifer I. Polymers and proteins: interactions at interfaces. Current Opinion in Solid State and Materials Science. 1997;2(3):337–344. [Google Scholar]
- 55.Wang C, YuB , Knudsen B, Harmon J, Moussy F, Moussy Y. Synthesis and performance of novel hydrogels coatings for implantable glucose sensors. Biomacromolecules. 2008;9(2):561–567. doi: 10.1021/bm701102y. [DOI] [PubMed] [Google Scholar]
- 56.Nolan CM, Reyes CD, Debord JD, García AJ, Lyon LA. Phase transition behavior, protein adsorption, and cell adhesion resistance of poly(ethylene glycol) cross-linked microgel particles. Biomacromolecules. 2005;6(4):2032–2039. doi: 10.1021/bm0500087. [DOI] [PubMed] [Google Scholar]
- 57.Singh N, Bridges AW, García AJ, Lyon LA. Covalent tethering of functional microgel films onto poly(ethylene terephthalate) surfaces. Biomacromolecules. 2007;8(10):3271–3275. doi: 10.1021/bm700516v. [DOI] [PubMed] [Google Scholar]
- 58.Yang Y, Zhang SF, Kingston MA, Jones G, Wright G, Spencer SA. Glucose sensor with improved haemocompatibilty. Biosens Bioelectron. 2000;15(5-6):221–227. doi: 10.1016/s0956-5663(00)00082-8. [DOI] [PubMed] [Google Scholar]
- 59.Iwasaki Y, Ishihara K, Nakabayashi N, Khang G, Jeon JH, Lee JW, Lee HB. Platelet adhesion on the gradient surfaces grafted with phospholipid polymer. J Biomater Sci Polym Ed. 1998;9(8):801–816. doi: 10.1163/156856298x00163. [DOI] [PubMed] [Google Scholar]
- 60.Kudo H, Sawada T, Kazawa E, Yoshida H, Iwasaki Y, Mitsubayashi K. A flexible and wearable glucose sensor based on functional polymers with soft-MEMS techniques. Biosens Bioelectron. 2006;22(4):558–562. doi: 10.1016/j.bios.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 61.Goreish HH, Lewis AL, Rose S, Lloyd AW. The effect of phosphorylcholine-coated materials on the inflammatory response and fibrous capsule formation: in vitro and in vivo observations. J Biomed Mater Res A. 2004;68(1):1–9. doi: 10.1002/jbm.a.10141. [DOI] [PubMed] [Google Scholar]
- 62.Luk Y-Y, Kato M, Mrksich M. Self-assembled monolayers of alkanethiolates presenting mannitol groups are inert to protein adsorption and cell attachment. Langmuir. 2000;16(24):9604–9608. [Google Scholar]
- 63.Holland NB, Qiu Y, Ruegsegger M, Marchant RE. Biomimetic engineering of non-adhesive glycocalyx-like surfaces using oligosaccharide surfactant polymers. Nature. 1998;392(6678):799–801. doi: 10.1038/33894. [DOI] [PubMed] [Google Scholar]
- 64.Kane RS, Deschatelets P, Whitesides GM. Kosmotropes form the basis of protein-resistant surfaces. Langmuir. 2003;19(6):2388–2391. [Google Scholar]
- 65.Prime KL, Whitesides GM. Adsorption of proteins onto surfaces containing end-attached oligo(ethylene oxide): a model system using self-assembled monolayers. J Am Chem Soc. 1993;115:10714–10721. [Google Scholar]
- 66.Zhao B, Brittain WJ. Polymer brushes: surface-immobilized macromolecules. Prog Polym Sci. 2000;25:677–710. [Google Scholar]
- 67.Edmondson S, Osborne VL, Huck WT. Polymer brushes via surface-initiated polymerizations. Chem Soc Rev. 2004;33(1):14–22. doi: 10.1039/b210143m. [DOI] [PubMed] [Google Scholar]
- 68.Kopecek J. Hydrogel biomaterials: a smart future? Biomaterials. 2007;28(34):5185–5192. doi: 10.1016/j.biomaterials.2007.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nath N, Chilkoti A. Creating “smart” surfaces using stimuli responsive polymers. Adv Mater. 2002;14(17):1243–1247. [Google Scholar]
- 70.Hoffman AS. Hydrogels for biomedical applications. Adv Drug Deliv Rev. 2002;54(1):3–12. doi: 10.1016/s0169-409x(01)00239-3. [DOI] [PubMed] [Google Scholar]
- 71.Mendelsohn JD, Yang SY, Hiller J, Hochbaum AI, Rubner MF. Rational design of cytophilic and cytophobic polyelectrolyte multilayer thin films. Biomacromolecules. 2003;4(1):96–106. doi: 10.1021/bm0256101. [DOI] [PubMed] [Google Scholar]
- 72.Nayak S, Lyon LA. Ligand-functionalized core/shell microgels with permselective shells. Angew Chem Int Ed Engl. 2004;43(48):6706–6709. doi: 10.1002/anie.200461090. [DOI] [PubMed] [Google Scholar]
- 73.Quinn CP, Pathak CP, Heller A, Hubbell JA. Photo-crosslinked copolymers of 2-hydroxyethyl methacrylate, poly(ethylene glycol) tetra-acrylate and ethylene dimethacrylate for improving biocompatibility of biosensors. Biomaterials. 1995;16(5):389–396. doi: 10.1016/0142-9612(95)98856-9. [DOI] [PubMed] [Google Scholar]
- 74.Shen M, Martinson L, Wagner MS, Castner DG, Ratner BD, Horbett TA. PEO-like plasma polymerized tetraglyme surface interactions with leukocytes and proteins: in vitro and in vivo studies. J Biomater Sci Polym Ed. 2002;13(4):367–390. doi: 10.1163/156856202320253910. [DOI] [PubMed] [Google Scholar]
- 75.Park HJ, Bae YH. Hydrogels based on poly(ethylene oxide) and poly(tetramethylene oxide) or poly(dimethyl siloxane). III. In vivo biocompatibility and biostability. J Biomed Mater Res A. 2003;64(2):309–319. doi: 10.1002/jbm.a.10424. [DOI] [PubMed] [Google Scholar]
- 76.Ronneberger B, Kao WJ, Anderson JM, Kissel T. In vivo biocompatibility study of ABA triblock copolymers consisting of poly(L-lactic-co-glycolic acid) A blocks attached to central poly(oxyethylene) B blocks. J Biomed Mater Res. 1996;30(1):31–40. doi: 10.1002/(SICI)1097-4636(199601)30:1<31::AID-JBM5>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 77.Chapman RG, Ostuni E, Liang MN, Meluleni G, Kim E, Yan L, Pier G, Warren HS, Whitesides GM. Polymeric thin films that resist the adsorption of proteins and the adhesion of bacteria. Langmuir. 2001;17(4):1225–1233. [Google Scholar]
- 78.Zhang F, Kang ET, Neoh KG, Huang W. Modification of gold surface by grafting of poly(ethylene glycol) for reduction in protein adsorption and platelet adhesion. J Biomater Sci Polym Ed. 2001;12(5):515–531. doi: 10.1163/156856201300194252. [DOI] [PubMed] [Google Scholar]
- 79.Espadas-Torre C, Meyerhoff ME. Thrombogenic properties of untreated and poly(ethylene oxide)-modified polymeric matrices useful for preparing intraarterial ion-selective electrodes. Anal Chem. 1995;67(18):3108–3114. doi: 10.1021/ac00114a003. [DOI] [PubMed] [Google Scholar]
- 80.Lee JH, Jeong BJ, Lee HB. Plasma protein adsorption and platelet adhesion onto comb-like PEO gradient surfaces. J Biomed Mater Res. 1997;34(1):105–114. doi: 10.1002/(sici)1097-4636(199701)34:1<105::aid-jbm14>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 81.Du H, Chandaroy P, Hui SW. Grafted poly-(ethylene glycol) on lipid surfaces inhibits protein adsorption and cell adhesion. Biochim Biophys Acta. 1997;1326(2):236–248. doi: 10.1016/s0005-2736(97)00027-8. [DOI] [PubMed] [Google Scholar]
- 82.Zhang M, Desai T, Ferrari M. Proteins and cells on PEG immobilized silicon surfaces. Biomaterials. 1998;19(10):953–960. doi: 10.1016/s0142-9612(98)00026-x. [DOI] [PubMed] [Google Scholar]
- 83.Jenney CR, Anderson JM. Effects of surface-coupled polyethylene oxide on human macrophage adhesion and foreign body giant cell formation in vitro. J Biomed Mater Res. 1999;44(2):206–216. doi: 10.1002/(sici)1097-4636(199902)44:2<206::aid-jbm11>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 84.Shen M, Pan YV, Wagner MS, Hauch KD, Castner DG, Ratner BD, Horbett TA. Inhibition of monocyte adhesion and fibrinogen adsorption on glow discharge plasma deposited tetraethylene glycol dimethyl ether. J Biomater Sci Polym Ed. 2001;12(9):961–978. doi: 10.1163/156856201753252507. [DOI] [PubMed] [Google Scholar]
- 85.Otsuka H, Nagasaki Y, Kataoka K. Self-assembly of poly(ethylene glycol)-based block copolymers for biomedical applications. Current Opinion in Colloid and Interface Science. 2001;6(1):3–10. [Google Scholar]
- 86.Boulmedais F, Frisch B, Etienne O, Lavalle P, Picart C, Ogier J, Voegel JC, Schaaf P, Egles C. Polyelectrolyte multilayer films with pegylated polypeptides as a new type of anti-microbial protection for biomaterials. Biomaterials. 2004;25(11):2003–2011. doi: 10.1016/j.biomaterials.2003.08.039. [DOI] [PubMed] [Google Scholar]
- 87.Ma H, Hyun J, Stiller P, Chilkoti A. “Non-fouling” oligo(ethylene glycol)-functionalized polymer brushes synthesized by surface-initiated atom transfer radical polymerization. Adv Mater. 2004;16(4):338–341. [Google Scholar]
- 88.Ma H, Li D, Sheng X, Zhao B, Chilkoti A. Protein-resistant polymer coatings on silicon oxide by surface-initiated atom transfer radical polymerization. Langmuir. 2006;22(8):3751–3756. doi: 10.1021/la052796r. [DOI] [PubMed] [Google Scholar]
- 89.Zhou Y, Liedberg B, Gorochovceva N, Makuska R, Dedinaite A, Claesson PM. Chitosan-N-poly(ethylene oxide) brush polymers for reduced nonspecific protein adsorption. J Colloid Interface Sci. 2007;305(1):62–71. doi: 10.1016/j.jcis.2006.09.058. [DOI] [PubMed] [Google Scholar]
- 90.Waku T, Matsusaki M, Kaneko T, Akashi M. PEG brush peptide nanospheres with stealth properties and chemical functionality. Macromolecules. 2007;40(17):6385–6392. [Google Scholar]
- 91.Cao L, Chang M, Lee CY, Castner DG, Sukavaneshvar S, Ratner BD, Horbett TA. Plasma-deposited tetraglyme surfaces greatly reduce total blood protein adsorption, contact activation, platelet adhesion, platelet procoagulant activity, and in vitro thrombus deposition. J Biomed Mater Res A. 2007;81(4):827–837. doi: 10.1002/jbm.a.31091. [DOI] [PubMed] [Google Scholar]
- 92.West JL, Hubbell JA. Comparison of covalently and physically cross-linked polyethylene glycol-based hydrogels for the prevention of postoperative adhesions in a rat model. Biomaterials. 1995;16(15):1153–1156. doi: 10.1016/0142-9612(95)93579-3. [DOI] [PubMed] [Google Scholar]
- 93.Quinn CA, Connor RE, Heller A. Biocompatible, glucose-permeable hydrogel for in situ coating of implantable biosensors. Biomaterials. 1997;18(24):1665–1670. doi: 10.1016/s0142-9612(97)00125-7. [DOI] [PubMed] [Google Scholar]
- 94.Collier TO, Anderson JM, Brodbeck WG, Barber T, Healy KE. Inhibition of macrophage development and foreign body giant cell formation by hydrophilic interpenetrating polymer network. J Biomed Mater Res A. 2004;69(4):644–650. doi: 10.1002/jbm.a.30030. [DOI] [PubMed] [Google Scholar]
- 95.Bridges AW, Singh N, Burns KL, Babensee JE, Lyon AL, García AJ. Reduced acute inflammatory responses to microgel conformal coatings. Biomaterials. 2008;29(35):4605–4615. doi: 10.1016/j.biomaterials.2008.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Yu B, Wang C, Ju YM, West L, Harmon J, Moussy Y, Moussy F. Use of hydrogel coating to improve the performance of implanted glucose sensors. Biosens Bioelectron. 2008;23(8):1278–1284. doi: 10.1016/j.bios.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 97.Benkirane-Jessel N, Lavalle P, Meyer F, Audouin F, Frisch B, Schaaf P, Ogier J, Decher G, Voegel J-C. Control of monocyte morphology on and response to model surfaces for implants eqipped with anti-inflammatory agents. Adv Mater. 2004;16(17):1507–1511. [Google Scholar]
- 98.Schultz P, Vautier D, Richert L, Jessel N, Haikel Y, Schaaf P, Voegel JC, Ogier J, Debry C. Polyelectrolyte multilayers functionalized by a synthetic analogue of an anti-inflammatory peptide, alpha-MSH, for coating a tracheal prosthesis. Biomaterials. 2005;26(15):2621–2630. doi: 10.1016/j.biomaterials.2004.06.049. [DOI] [PubMed] [Google Scholar]
- 99.Shive MS, Anderson JM. Biodegradation and biocompatibility of PLA and PLGA microspheres. Adv Drug Deliv Rev. 1997;28(1):5–24. doi: 10.1016/s0169-409x(97)00048-3. [DOI] [PubMed] [Google Scholar]
- 100.Lutolf MP, Raeber GP, Zisch AH, Tirelli N, Hubbell JA. Cell-responsive synthetic hydrogels. Adv Mater. 2003;15(11):888–892. [Google Scholar]
- 101.Zisch AH, Lutolf MP, Ehrbar M, Raeber GP, Rizzi SC, Davies N, Schmökel H, Bezuidenhout D, Djonov V, Zilla P, Hubbell JA. Cell-demanded release of VEGF from synthetic, biointeractive cell ingrowth matrices for vascularized tissue growth. FASEB J. 2003;17(15):2260–2262. doi: 10.1096/fj.02-1041fje. [DOI] [PubMed] [Google Scholar]
- 102.Tauro JR, Gemeinhart RA. Matrix metalloprotease triggered delivery of cancer chemotherapeutics from hydrogel matrixes. Bioconjug Chem. 2005;16(5):1133–1139. doi: 10.1021/bc0501303. [DOI] [PubMed] [Google Scholar]
- 103.Bae M, Cho S, Song J, Lee GY, Kim K, Yang J, Cho K, Kim SY, Byun Y. Metalloprotease-specific poly(ethylene glycol) methyl ether-peptide-doxorubicin conjugate for targeting anticancer drug delivery based on angiogenesis. Drugs Exp Clin Res. 2003;29(1):15–23. [PubMed] [Google Scholar]
- 104.Barnes PJ. Anti-inflammatory actions of glucocorticoids: molecular mechanisms. Clin Sci (Lond) 1998;94(6):557–572. doi: 10.1042/cs0940557. [DOI] [PubMed] [Google Scholar]
- 105.Cupps TR, Fauci AS. Corticosteroid-mediated immunoregulation in man. Immunol Rev. 1982;65:133–155. doi: 10.1111/j.1600-065x.1982.tb00431.x. [DOI] [PubMed] [Google Scholar]
- 106.Kiefer R, Kreutzberg GW. Effects of dexamethasone on microglial activation in vivo: selective downregulation of major histocompatibility complex class II expression in regenerating facial nucleus. J Neuroimmunol. 1991;34(2-3):99–108. doi: 10.1016/0165-5728(91)90119-r. [DOI] [PubMed] [Google Scholar]
- 107.Norton LW, Koschwanez HE, Wisniewski NA, Klitzman B, Reichert WM. Vascular endothelial growth factor and dexamethasone release from nonfouling sensor coatings affect the foreign body response. J Biomed Mater Res A. 2007;81(4):858–869. doi: 10.1002/jbm.a.31088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhong Y, Bellamkonda RV. Dexamethasone-coated neural probes elicit attenuated inflammatory response and neuronal loss compared to uncoated neural probes. Brain Res. 2007;1148:15–27. doi: 10.1016/j.brainres.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim DH, Martin DC. Sustained release of dexamethasone from hydrophilic matrices using PLGA nanoparticles for neural drug delivery. Biomaterials. 2006;27(15):3031–3037. doi: 10.1016/j.biomaterials.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 110.Patil SD, Papadmitrakopoulos F, Burgess DJ. Concurrent delivery of dexamethasone and VEGF for localized inflammation control and angiogenesis. J Control Release. 2007;117(1):68–79. doi: 10.1016/j.jconrel.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 111.Wadhwa R, Lagenaur CF, Cui XT. Electrochemically controlled release of dexamethasone from conducting polymer polypyrrole coated electrode. J Control Release. 2006;110(3):531–541. doi: 10.1016/j.jconrel.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 112.Anastase-Ravion S, Blondin C, Cholley B, Haeffner-Cavaillon N, Castellot JJ, Letourneur D. Heparin inhibits lipopolysaccharide (LPS) binding to leukocytes and LPS-induced cytokine production. J Biomed Mater Res A. 2003;66(2):376–384. doi: 10.1002/jbm.a.10604. [DOI] [PubMed] [Google Scholar]
- 113.Salas A, Sans M, Soriano A, Reverter JC, Anderson DC, Piqué JM, Panés J. Heparin attenuates TNF-alpha induced inflammatory response through a CD11b dependent mechanism. Gut. 2000;47(1):88–96. doi: 10.1136/gut.47.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Du YJ, Brash JL, McClung G, Berry LR, Kelment P, Chan AK. Protein adsorption on polyurethane catheters modified with a novel antithrombin-heparin covalent complex. J Biomed Mater Res A. 2007;80(1):216–225. doi: 10.1002/jbm.a.30977. [DOI] [PubMed] [Google Scholar]
- 115.van Bilsen PH, Popa ER, Brouwer LA, Vincent J, Taylor CE, de Leij LF, Hendriks M, van Luyn MJ. Ongoing foreign body reaction to subcutaneous implanted (heparin) modified Dacron in rats. J Biomed Mater Res A. 2004;68(3):423–427. doi: 10.1002/jbm.a.20069. [DOI] [PubMed] [Google Scholar]
- 116.Rele SM, Cui W, Wang L, Hou S, Barr-Zarse G, Tatton D, Gnanou Y, Esko JD, Chaikof EL. Dendrimer-like PEO glycopolymers exhibit anti-inflammatory properties. J Am Chem Soc. 2005;127(29):10132–10133. doi: 10.1021/ja0511974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Tseng PY, Rele SS, Sun XL, Chaikof EL. Membrane-mimetic films containing thrombomodulin and heparin inhibit tissue factor-induced thrombin generation in a flow model. Biomaterials. 2006;27(12):2637–2650. doi: 10.1016/j.biomaterials.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 118.Zhong Y, Bellamkonda RV. Controlled release of anti-inflammatory agent alpha-MSH from neural implants. J Control Release. 2005;106(3):309–318. doi: 10.1016/j.jconrel.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 119.Udipi K, Ornberg RL, Thurmond KB, 2nd, Settle SL, Forster D, Riley D. Modification of inflammatory response to implanted biomedical materials in vivo by surface bound superoxide dismutase mimics. J Biomed Mater Res. 2000;51(4):549–560. doi: 10.1002/1097-4636(20000915)51:4<549::aid-jbm2>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 120.He W, McConnell GC, Schneider TM, Bellamkonda RV. A novel anti-inflammatory surface for neural electrodes. Adv Mater. 2007;19:3529–3533. [Google Scholar]
- 121.Gerritsen M, Kros A, Sprakel V, Lutterman JA, Nolte RJ, Jansen JA. Biocompatibility evaluation of sol-gel coatings for subcutaneously implantable glucose sensors. Biomaterials. 2000;21(1):71–78. doi: 10.1016/s0142-9612(99)00136-2. [DOI] [PubMed] [Google Scholar]
- 122.Wang XH, Li DP, Wang WJ, Feng QL, Cui FZ, Xu YX, Song XH. Covalent immobilization of chitosan and heparin on PLGA surface. Int J Biol Macromol. 2003;33(1-3):95–100. doi: 10.1016/s0141-8130(03)00072-2. [DOI] [PubMed] [Google Scholar]
- 123.Sung WJ, Na K, Bae YH. Biocompatibility and interference eliminating property of pullulan acetate/polyethylene glycol/heparin membrane for the outer layer of an amperometric glucose sensor. Sens Actuators B Chem. 2004;99(2-3):393–398. [Google Scholar]
- 124.Fu J, Ji J, Yuan W, Shen J. Construction of anti-adhesive and antibacterial multilayer films via layer-by-layer assembly of heparin and chitosan. Biomaterials. 2005;26(33):6684–6692. doi: 10.1016/j.biomaterials.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 125.Kim DH, Smith JT, Chilkoti A, Reichert WM. The effect of covalently immobilized rhIL-1ra-ELP fusion protein on the inflammatory profile of LPS-stimulated human monocytes. Biomaterials. 2007;28(23):3369–3377. doi: 10.1016/j.biomaterials.2007.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Nguyen KT, Shaikh N, Shukla KP, Su SH, Eberhart RC, Tang L. Molecular responses of vascular smooth muscle cells and phagocytes to curcumin-eluting bioresorbable stent materials. Biomaterials. 2004;25(23):5333–5346. doi: 10.1016/j.biomaterials.2003.12.033. [DOI] [PubMed] [Google Scholar]
- 127.Su SH, Nguyen KT, Satasiya P, Greilich PE, Tang L, Eberhart RC. Curcumin impregnation improves the mechanical properties and reduces the inflammatory response associated with poly(L-lactic acid) fiber. J Biomater Sci Polym Ed. 2005;16(3):353–370. doi: 10.1163/1568562053654077. [DOI] [PubMed] [Google Scholar]
- 128.Pan ChJ, Tang JJ, Weng YJ, Wang J, Huang N. Preparation, characterization and anticoagulation of curcumin-eluting controlled biodegradable coating stents. J Control Release. 2006;116(1):42–49. doi: 10.1016/j.jconrel.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 129.Hahn SK, Jelacic S, Maier RV, Stayton PS, Hoffman AS. Anti-inflammatory drug delivery from hyaluronic acid hydrogels. J Biomater Sci Polym Ed. 2004;15(9):1111–1119. doi: 10.1163/1568562041753115. [DOI] [PubMed] [Google Scholar]
- 130.Mantovani A, Locati M, Vecchi A, Sozzani S, Allavena P. Decoy receptors: a strategy to regulate inflammatory cytokines and chemokines. Trends Immunol. 2001;22(6):328–336. doi: 10.1016/s1471-4906(01)01941-x. [DOI] [PubMed] [Google Scholar]
- 131.Kao WJ, Liu Y, Gundloori R, Li J, Lee D, Einerson N, Burmania J, Stevens K. Engineering endogenous inflammatory cells as delivery vehicles. J Control Release. 2002;78(1-3):219–233. doi: 10.1016/s0168-3659(01)00503-x. [DOI] [PubMed] [Google Scholar]
- 132.Konstan MW, Davis PB. Pharmacological approaches for the discovery and development of new anti-inflammatory agents for the treatment of cystic fibrosis. Adv Drug Deliv Rev. 2002;54(11):1409–1423. doi: 10.1016/s0169-409x(02)00146-1. [DOI] [PubMed] [Google Scholar]
- 133.Mundargi RC, Babu VR, Rangaswamy V, Patel P, Aminabhavi TM. Nano/micro technologies for delivering macromolecular therapeutics using poly(D,L-lactide-co-glycolide) and its derivatives. J Control Release. 2008;125(3):193–209. doi: 10.1016/j.jconrel.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 134.Luten J, van Nostrum CF, De Smedt SC, Hennink WE. Biodegradable polymers as non-viral carriers for plasmid DNA delivery. J Control Release. 2008;126(2):97–110. doi: 10.1016/j.jconrel.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 135.Lavi G, Dinarello CA, Apte RN, Cohen S. Sustained release of IL-1Ra from biodegradable microspheres prolongs its IL-1-neutralizing effects. Isr J Chemistry. 2005;45:457–464. [Google Scholar]
- 136.Rusanova AV, Makarova AM, Strukova SM, Markvicheva EA, Gorbachyova LR, Stashevskaya KS, Vasil'eva TV, Sidorova EI, Bespalova ZhD, Grandfils Ch. Thrombin receptor agonist Peptide immobilized in microspheres stimulates reparative processes in rats with gastric ulcer. Bull Exp Biol Med. 2006;142(1):35–38. doi: 10.1007/s10517-006-0285-y. [DOI] [PubMed] [Google Scholar]
- 137.Yu P, Zheng C, Chen J, Zhang G, Liu Y, Suo X, Zhang G, Su Z. Investigation on PEGylation strategy of recombinant human interleukin-1 receptor antagonist. Bioorg Med Chem. 2007;15(16):5396–5405. doi: 10.1016/j.bmc.2007.05.061. [DOI] [PubMed] [Google Scholar]
- 138.Pierstorff E, Krucoff M, Ho D. Apoptosis induction and attenuation of inflammatory gene expression in murine macrophages via multitherapeutic nanomembranes. Nanotechnology. 2008;19(26) doi: 10.1088/0957-4484/19/26/265103. [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 139.Juliano R, Alam MR, Dixit V, Kang H. Mechanisms and strategies for effective delivery of antisense and siRNA oligonucleotides. Nucleic Acids Res. 2008;36(12):4158–4171. doi: 10.1093/nar/gkn342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Gary DJ, Puri N, Won YY. Polymer-based siRNA delivery: perspectives on the fundamental and phenomenological distinctions from polymer-based DNA delivery. J Control Release. 2007;121(1-2):64–73. doi: 10.1016/j.jconrel.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 141.Mori R, Shaw TJ, Martin P. Molecular mechanisms linking wound inflammation and fibrosis: knockdown of osteopontin leads to rapid repair and reduced scarring. J Exp Med. 2008;205(1):43–51. doi: 10.1084/jem.20071412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Andersen MØ, Howard KA, Paludan SR, Besenbacher F, Kjems J. Delivery of siRNA from lyophilized polymeric surfaces. Biomaterials. 2007;29(4):506–512. doi: 10.1016/j.biomaterials.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 143.Chiarantini L, Cerasi A, Fraternale A, Millo E, Benatti U, Sparnacci K, Laus M, Ballestri M, Tondelli L. Comparison of novel delivery systems for antisense peptide nucleic acids. J Control Release. 2005;109(1-3):24–36. doi: 10.1016/j.jconrel.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 144.Kovacs JR, Zheng Y, Shen H, Meng WS. Polymeric microspheres as stabilizing anchors for oligonucleotide delivery to dendritic cells. Biomaterials. 2005;26(33):6754–6761. doi: 10.1016/j.biomaterials.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 145.Jeong JH, Kim SW, Park TG. Molecular design of functional polymers for gene therapy. Prog Polym Sci. 2007;32:1239–1274. [Google Scholar]
- 146.Jewell CM, Zhang J, Fredin NJ, Wolff MR, Hacker TA, Lynn DM. Release of plasmid DNA from intravascular stents coated with ultrathin multilayered polyelectrolyte films. Biomacromolecules. 2006;7(9):2483–2491. doi: 10.1021/bm0604808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.DeFife KM, Shive MS, Hagen KM, Clapper DL, Anderson JM. Effects of photochemically immobilized polymer coatings on protein adsorption, cell adhesion, and the foreign body reaction to silicone rubber. J Biomed Mater Res. 1999;44(3):298–307. doi: 10.1002/(sici)1097-4636(19990305)44:3<298::aid-jbm8>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 148.Gil PR, del Mercato LL, del Pino P, Javier AM, Parak WJ. Nanoparticle-modified polyelectrolyte capsules. Nano Today. 2008;3(3-4):12–21. [Google Scholar]
- 149.Klueh U, Dorsky DI, Kreutzer DL. Enhancement of implantable glucose sensor function in vivo using gene transfer-induced neovascularization. Biomaterials. 2005;26(10):1155–1163. doi: 10.1016/j.biomaterials.2004.04.017. [DOI] [PubMed] [Google Scholar]


