Abstract
Background
The objective of this study was to assess the published literature on health literacy and diabetes, as well as identify opportunities for technology to strengthen information skills and modify behavior to improve diabetes health outcomes.
Methods
Medline (1990–2008), the Cumulative Index to Nursing and Allied Health Literature (1990-2008), and the Education Resources Information Center (1990–2008) were searched, and reference lists from included articles were reviewed to identify additional studies. Articles were included that presented measures of literacy or numeracy specific to diabetes, examined associations between health literacy and diabetes outcomes, or tested a health literacy intervention among persons with diabetes.
Results
Twenty-four articles were included in this review. Five articles reported on measures of literacy or numeracy specific to diabetes. Thirteen of the fifteen cross-sectional studies (87%) associated limited health literacy with poorer diabetes outcomes. Two of the four (50%) health literacy intervention studies lead to improved health outcomes.
Conclusions
The cross-sectional studies provide evidence of an association between health literacy and diabetes outcomes; however, there is a need to design and test strategies to improve diabetes health outcomes that consider health literacy. Information and communication technology opportunities could help to mediate the effect that limited health literacy has on diabetes-related health outcomes.
Keywords: diabetes mellitus, literacy, outcomes of care, process of care randomized controlled trials
Introduction
Often people with the greatest health burdens have the least access to health care information that they can understand.1 Health literacy is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”2 The ability to apply reading, listening, speaking, analytic, decision-making, and numeracy skills to health situations is affected by low health literacy.3
Health literacy is vital to enable people to manage their health. There are many activities that people are responsible for when self-managing their diabetes that can be particularly challenging when limited health literacy is an issue. These activities include taking medication, eating a healthy diet, glucose monitoring, and reduction of risks. Persons with diabetes who have multiple complications or experience repeated hospitalizations might have some of these problems because of unrecognized low health literacy.
Patients with low health literacy are usually embarrassed by their situation and hide it from other people who could possibly help (e.g., healthcare providers, friends, and family members). Approximately half of the adults in the United States have low health literacy.4 The poor health outcomes and costs to the health care system associated with low health literacy have been estimated to be as much as $58 billion per year.5
People need strong health information skills as we move toward a consumer-centric health care system, where individuals take an active role in health-care-related decisions. Effective interventions to help persons with low health literacy to strengthen their information skills and modify their health behaviors also are needed. The objective of this study was to assess the published literature on health literacy and diabetes, as well as identify opportunities for technology to strengthen information and communication skills and modify behaviors to improve diabetes health outcomes.
Methods
Data Sources
Medline (1990–2008), the Cumulative Index to Nursing and Allied Health Literature (CINAHL, 1990–2008), and the Education Resources Information Center (ERIC, 1990–2008) were searched for eligible articles using combinations of the following search terms: (1) diabetes mellitus, type 1 diabetes mellitus, or type 2 diabetes mellitus and (2) literacy, illiteracy, readability, reading ability, reading skill, numeracy, test of functional health literacy in adults (TOFHLA), rapid estimate of adult literacy in medicine (REALM), or wide range achievement test, third edition (WRAT3). The reference lists of included studies were also searched.
Study Selection and Data Extraction
The author screened the titles and abstracts of the identified citations and identified eligible articles based on the following criteria: measures of literacy or numeracy specific to diabetes, studies of associations between health literacy and diabetes outcomes, or health literacy intervention among persons with diabetes. The following information was collected from the eligible articles for each of the categories. Category 1—measures of literacy or numeracy specific to diabetes: name of measure, sample, psychometric properties, number of items, response format, and administration time. Category 2—associations among literacy and diabetes outcomes: sample, health literacy assessment used, and outcomes reported. Category 3—literacy interventions among persons with diabetes: sample, intervention and control groups, and results.
Results
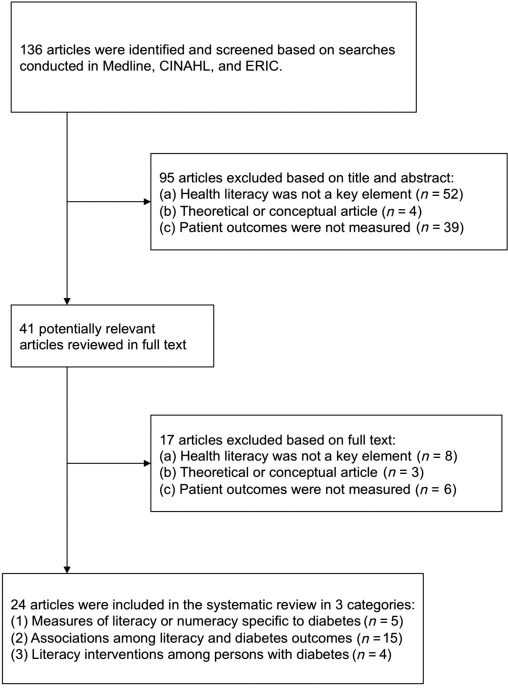
Comprehensive literature searches identified 136 articles. The articles were screened by the author, and 24 articles met the eligibility criteria (Figure 1). While the literature was searched back to 1990, only one eligible article had been published prior to 2000, and 19 of the 24 articles (79%) were published in the past five years. The studies represented in the articles involved more than 10,000 persons with diabetes.
Figure 1.
Trial flow diagram.
Measure Development Studies
Five measures of literacy or numeracy specific to diabetes or tested among persons with diabetes were identified (Table 1).6–10 The purpose of these measures was to assess adults' ability to comprehend nutritional information;6 measure numeracy skills in persons with diabetes;7 identify limited reading ability;8 assess a patient's ability to pronounce terms that they would encounter (e.g., during clinic visits, in reading menus, and in self-care instructions);9 and gauge diabetes knowledge among persons with poor literacy.10 Most of these instruments are brief and only take a few minutes to complete,6,8–10 or there is an abbreviated version of the instrument available.7
Table 1.
Measures of Literacy or Numeracy Specific to Diabetes
| Study | Measure | Sample | Psychometric properties | Number of items | Response format and administration time |
|---|---|---|---|---|---|
| Diamond6 | Nutritional Literacy Scale | 341 primary care patients | internal consistency (Chronbach alpha 0.84); construct validity (Pearson correlation 0.61) | 32 | written; 10 min to complete |
| Huizinga et al.7 | Diabetes Numeracy Test | 398 persons with diabetes | internal reliability (Kuder–Richardson | 43 or a shortened version with 15 | written or verbally administered; 33 min to complete the long version |
| Morris et al.8 | Single Item Literacy Screener | 999 persons with diabetes | sensitivity 54%; specificity 83% | 1 | verbally administered; less than 1 min to complete |
| Nath et al.9 | Literacy Assessment for Diabetes | 203 persons | concurrent validity (correlation coefficient of 0.81 with the WRAT3 and 0.90 with the REALM); test–retest reliability interclass correlation coefficient of reliability of 0.86 (p < .0001)). | 3 lists of words, 60 words total | read and spoken; 3 min or less to complete |
| Rothman et al.10 | Spoken Knowledge in Low Literacy Patients with Diabetes | 217 persons with type 2 diabetes | internal reliability (Kuder–Richardson coefficient 0.72) | 10 | verbally administered; less than 10 min to complete |
Association Studies
Fifteen studies examined associations between health literacy and diabetes outcomes (Table 2).11–25 There is a lack of information in the studies about how well or poorly controlled the patients were; however, seven of the studies provided information about the number of years the patients had been living with diabetes, and this ranged from 5 to 11 years.11,15,17–21 The studies used a variety of health literacy assessments [e.g., TOFHLA,25 short-form of the TOFHLA (S-TOFHLA),13–15,18,20–22,24 REALM,11,12,16,23 WRAT3,11,17 diabetes numeracy test (DNT),11Raven's standard progressive metric (RSPM),17 and national adult reading test (NART)17]. A few studies administered the assessment in Spanish20,22 or Chinese.24
Table 2.
Associations Among Literacy and Diabetes Outcomesa
| Study | Sample | Health literacy assessment used | Outcomes reported |
|---|---|---|---|
| Cavanaugh et al.11 | 398 adult patients with type 1 or type 2 diabetes | REALM; WRAT3; DNT | Lower DNT scores were associated with older age, nonwhite race, fewer years of education, lower reported income, lower literacy and general numeracy skills, and higher HbA1c. |
| DeWalt et al.12 | 268 patients with diabetes | REALM | Patients with low literacy had less desire to participate in medical decision making (p < .001) and less diabetes-related knowledge (p < .001). Literacy was not associated with trust, self-efficacy, or diabetes outcomes. |
| Gazmararian et al.13 | 653 new Medicare enrollees aged 65 years or older who had at least one chronic disease (115 asthma, 266 diabetes, 166 chronic heart failure, 214 hypertension) | S-TOFHLA | Patients with inadequate health literacy knew significantly less about their disease than those with adequate health literacy. Health literacy was independently related to disease knowledge. |
| Gazmararian et al.14 | 1549 patients newly enrolled in Medicare identified as having coronary heart disease, hypertension, diabetes, or hyperlipidemia | S-TOFHLA | Health literacy was related to medication refill adherence (p < .05). Patients with inadequate health literacy skills had increased odds of low refill adherence compared with those with adequate literacy skills (OR = 1.37; 95% CI: 1.08 to 1.74). |
| Morris et al.15 | 1002 English-speaking adults with diabetes | S-TOFHLA | Health literacy was not significantly associated with HbA1c (p = .88), systolic blood pressure (p = .39), diastolic blood pressure (p = .59), low density lipoprotein (p = .77), or selfreported diabetes complications. |
| Powell et al.16 | 68 patients with type 2 diabetes | REALM | Health literacy was significantly associated with the diabetes knowledge test score (p = .004) and HbA1c (p = .02). Health literacy was not significantly associated with DHBM (p = .29). |
| Ross et al.17 | 78 children and adolescents with type 1 diabetes and their mothers | NART; WRAT3; RSPM | The HbA1c of the children correlated with their age (p =.02), social class (p = .03), and NART score of their mother (p = .01). The child's WRAT3 and RSPM did not correlate with HbA1c. |
| Sarkar et al.18 | 408 ethnically diverse patients with diabetes | S-TOFHLA | Associations between self-efficacy and self-management were consistent across health literacy and race/ethnicity levels. For each 10% increase in self-efficacy score, patients were more likely to report optimal diet (p < .01), exercise (p < .01), self-monitoring of blood glucose (p < .01), and foot care (p < .01), but not medication adherence (p = .40). |
| Sarkar et al.19 | 796 low-income English- and Spanish-speaking patients with diabetes | Self-reported health literacy. Interviewers asked participants how often they have problems learning about their medical condition because of difficulty understanding written information. | Patients with limited self-reported health literacy were more likely to be interested in telephone support (instead of group visits or internet support) than those not reporting literacy deficits. |
| Schillinger et al.20 | 408 English- and Spanishspeaking patients who were older than 30 years and had type 2 diabetes | S-TOFHLA in English or Spanish | Patients with inadequate health literacy were less likely to achieve tight glycemic control (p = .05) and were more likely to have poor glycemic control (p = .02) and to report retinopathy (p = .01). |
| Schillinger et al.21 | 408 English- and Spanishspeaking patients with diabetes | S-TOFHLA | Patients with inadequate health literacy were more likely to report worse communication in general clarity (p < .01), explanation of condition (p = .03), and explanation of processes of care (p = .03). |
| Schillinger et al.22 | 395 low-income patients with diabetes | S-TOFHLA | Health literacy mediated the relationship between education and HbA1c (p < .01) |
| Sudore et al.23 | 2512 black and white community-dwelling older people who did not have functional difficulties or dementia | REALM | Limited health literacy was associated with being male, being black, low income, low education, diabetes, depressive symptoms, and fair/poor self-rated health (p < .02). Older people with a sixth-grade reading level or lower were twice as likely to have indicators of poor healthcare access (OR = 1.96; 95% CI: 1.34 to 2.88). |
| Tang et al.24 | 149 Chinese patients with type 2 diabetes | Chinese version of the S-TOFHLA | Health literacy was negatively correlated to HbA1c (p < .001) |
| Williams et al.25 | 402 patients with hypertension and 114 patients with diabetes | TOFHLA | Knowledge scores for patients with diabetes with inadequate, marginal, or adequate literacy were 5.8 ± 2.1, 6.8 ± 1.9, and 8.1 ± 1.6 (p < .001), and 94% of patients with adequate functional health literacy knew the symptoms of hypoglycemia compared with 50% of those with inadequate health literacy. |
CI, confidence interval; OR, odds ratio.
The outcomes reported by these studies indicated significant associations between health literacy and knowledge,12,14,16,25 hemoglobin A1C (HbA1c),11,16,17,20,21,24 medication refill adherence,13 access to health care,23 and retinopathy.20 Those with limited health literacy were more likely to be interested in telephone support,19 more likely to report worse communication with their health care provider,22 and have less desire to participate in medical decision making.12 The outcomes reported by these studies also identified several nonsignificant associations between health literacy and trust,12 self-efficacy,12 the diabetes health belief model (DHBM) scale,16 HbA1c,15 systolic blood pressure,15 diastolic blood pressure,15 low-density lipoprotein,15 and self-reported diabetes complications.15
Intervention Studies
Four studies that tested a health literacy intervention in a sample of patients with diabetes were identified (Table 3).26–29 Two of the studies were randomized controlled trials28,29 and two were multicenter randomized controlled trials.26,27 These interventions were diverse and included patient education, a low-literacy reminder card,26 computer multimedia that included audio/video sequences to communicate information, provide psychological support, and promote diabetes self-management skills without extensive text or complex navigation,27 individually tailored disease management communication,28 and notifying physicians of patients with limited health literacy with a reminder notice affixed to the patient's chart.29
Table 3.
Literacy Interventions among Persons with Diabetesa
| Study | Sample | Intervention and Control Groups | Results Reported |
|---|---|---|---|
| Echeverry et al.26 | 166 patients with diabetes hospitalized for cardiovascular disease, 55 years of age or older | I: Education and a low-literacy reminder card describing risk factors of cardiovascular disease. Instructions to discuss the risk factors described on the card with their primary care physician on their first appointment after discharge. | HbA1c (NS); blood pressure (NS); lipid levels (NS); aspirin use higher in control group (p = .001); angiotensinconverting enzyme inhibitor use higher in control group (p = .03) |
| C: No Intervention. | |||
| Gerber et al.27 | 244 patients with diabetes | I: Use of computer multimedia that included audio/video sequences to communicate information, provided psychological support, and promoted diabetes selfmanagement skills without extensive text or complex navigation. | HbA1c (NS), weight (NS), blood pressure (NS), knowledge (NS), self-efficacy (NS), self-reported medical care (NS). Increase in perceived susceptibility to diabetes complications in the intervention group was greatest among subjects with lower health literacy. Time spent on the computer was greater for subjects with higher health literacy within the intervention group. |
| C: Standard of care only. | |||
| Rothman et al.28 | 217 patients aged 18 years or older with type 2 diabetes and poor glycemic control (HbA1c ≥ 8.0%) | I: All communication to patients was individualized and delivered to enhance comprehension among patients with low literacy. Patients received intensive disease management from a multidisciplinary team. | Among patients with low literacy, intervention patients were more likely than control patients to achieve goal HbA1c levels (≤7.0%) (42% versus 15%, respectively; adjusted OR, 4.6; and 95% CI, 1.3 to 17.2; p =.02). Patients with higher literacy had similar odds of achieving goal HbA1c levels regardless of intervention status (24% versus 23%; adjusted OR, 1.0; and 95% CI, 0.4 to 2.5; p = .98). |
| C: Patients received an initial management session and continued with usual care. | |||
| Seligman et al.29 | 63 primary care physicians and 182 patients with diabetes and limited health literacy | I: Physicians were notified if their patients had limited health literacy skills. | Intervention physicians were more likely than control physicians to use management strategies recommended for patients with limited health literacy (OR 3.2, p = .04). Intervention physicians felt less satisfied with their visits (81% versus 93%, p = .01). Intervention physicians felt less effective (38% versus 53%, p = .10). Intervention and control patients' postvisit self-efficacy scores were similar (12.6 versus 12.9, p = .60). And 64% of intervention physicians and 96% of patients felt health literacy screening was useful. |
| C: Physicians were not notified if their patients had low health literacy skills. |
C, control; CI, confidence interval; I, intervention; NS, not significant; OR, odds ratio.
The findings of the intervention studies were mixed. A low-literacy reminder card did not significantly improve any of the outcomes measured.26 Access to multimedia lessons resulted in an increase in perceived susceptibility to diabetes complications, particularly in subjects with lower health literacy; however, there was relatively less use of the computer among participants with lower health literacy.27 Patients with low literacy who received individually tailored communication were more likely to reach their HbA1c-level goal.28 Physicians were more likely to use the recommended management strategies to improve communication if they were notified of their patients' limited health literacy; however, these physicians felt less satisfied and less effective regarding their visits, while patient self-efficacy remained unchanged.29
Discussion
This review assessed the published literature on health literacy and its association with health outcomes and processes of care for persons with diabetes. The 24 studies in this review contributed information on the measurement of diabetes-related literacy, associations between health literacy and diabetes outcomes, and health literacy interventions for persons with diabetes.
Most literacy measures are of reading; however, health information services and modes of delivery are changing. Advances in consumer health informatics offer the convergence of many technologies (e.g., computers, internet, email, television, video, telephones, radio, and audio) and the opportunity to move beyond the traditional focus on print-based health literacy. When selecting a literacy measure, it is important to select a measure validated with a similar population.
Far fewer studies examined interventions designed to mitigate the effects of low literacy on diabetes outcomes than simply the association between literacy and diabetes outcomes. The small number of intervention studies highlights the need for additional studies to examine the relationship between health literacy and health outcomes and the mediating or moderating role of technology. An evidence-based review observed that patient factors (i.e., knowledge/skills, beliefs, participation in decision making, motivation, problem solving, self-efficacy, navigation skills, and perceived barriers), provider factors (i.e., communication skills, teaching ability, time, and patient-centeredness), and extrinsic factors (i.e., education and support technologies) are plausible causal pathways between limited health literacy and diabetes outcomes.30
Diabetes interventions that address literacy may be particularly beneficial for patients with limited literacy, and increasing access to such interventions could help reduce the disparities in health outcomes.3,28 While some health information technologies have been evaluated, such as diabetes self-management care via cell phone31 or computerized learning technologies for diabetes,32 testing these types of interventions with populations of all literacy levels is needed.
When designing the interventions that are suitable for persons with limited literacy, the information needs of the population as well as the existing evidence base in diabetes or other chronic disease models for related interventions should be considered. A few of the information and communication technology opportunities that might be appropriate for intervention are listed here.
Communication techniques and interactive communication strategies for patients and providers; Viewpoints and experiences of the patient population to determine the optimal context, channels, and content;
Computer-based algorithms that take a patient's characteristics into account such as language, age, gender, ethnicity, reading ability, health literacy level, and specific goals or needs;
Electronic medical record to prompt the use of plain language, limit the number of concepts covered, and assess patient understanding by using tell back or teach back;
Interactive multimedia programs for education and counseling;
Health information prescriptions that include a link or recommendation to an appropriate website and/or referral to a health librarian; and
Telephone or cell phone interventions for education, counseling, and reminding.
Abbreviations
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
- DHBM
diabetes health belief model
- DNT
diabetes numeracy test
- ERIC
Education Resources Information Center
- HbA1c
hemoglobin A1c
- NART
national adult reading test
- REALM
rapid estimate of adult literacy in medicine
- RSPM
Raven's standard progressive metric
- S-TOFHLA
short-form test of functional health literacy in adults
- TOFHLA
test of functional health literacy in adults
- WRAT3
wide range achievement test, third edition
References
- 1.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy people 2010: understanding and improving health. http://www.healthypeople.gov/Publications. Accessed September 8, 2008. [PubMed]
- 2.Ratzan SC, Parker RM. Selden CR, Zorn M, Ratzan SC, Parker RM, editors. Introduction. National Library of Medicine current bibliographies in medicine: health literacy 2000–1. http://www.nlm.nih.gov/archive//20061214/pubs/cbm/hliteracy.html. Accessed December 1, 2008.
- 3.Nath C. Literacy and diabetes self-management. A J Nurs. 2007;107(6 Suppl):43–49. doi: 10.1097/01.NAJ.0000277829.28043.93. [DOI] [PubMed] [Google Scholar]
- 4.Kutner M, Greenberg E, Baer J. National Assessment of Adult Literacy: a first look at the literacy of America's adults in the 21st century. NCES; 2005. U.S. Department of Education, National Center for Education Statistics. [Google Scholar]
- 5.Institute of Medicine of the National Academies. Health literacy: a prescription to end confusion. In: Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Washington DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 6.Diamond JJ. Development of a reliable and construct valid measure of nutritional literacy in adults. Nutr J. 2007;6:5. doi: 10.1186/1475-2891-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huizinga MM, Elasy TA, Wallston KA, Cavanaugh K, Davis D, Gregory RP, Fuchs LS, Malone R, Cherrington A, DeWalt DA, Buse J, Pignone M, Rothman RL. Development and validation of the Diabetes Numeracy Test (DNT) BMC Health Serv Res. 2008;8:96. doi: 10.1186/1472-6963-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morris NS, MacLean CD, Chew LD, Littenberg B. BMC Fam Pract. 2006. The single item literacy screener: evaluation of a brief instrument to identify limited reading ability; pp. 7–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nath CR, Sylvester ST, Yasek V, Gunel E. Development and validation of a literacy assessment tool for persons with diabetes. Diabetes Educ. 2001;27(6):857–864. doi: 10.1177/014572170102700611. [DOI] [PubMed] [Google Scholar]
- 10.Rothman RL, Malone R, Bryant B, Wolfe C, Padgett P, DeWalt DA, Weinberger M, Pignone M. The spoken knowledge in low literacy in diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educ. 2005;31(2):215–224. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 11.Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, Gregory RP, Fuchs L, Malone R, Cherrington A, Pignone M, DeWalt DA, Elasy TA, Rothman RL. Association of numeracy and diabetes control. Ann Intern Med. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- 12.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav. 2007;31(Suppl 1):S27–S35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 13.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21(12):1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 15.Morris NS, MacLean CD, Littenberg B. Literacy and health outcomes: a cross-sectional study in 1002 adults with diabetes. BMC Fam Pract. 2006:7–49. doi: 10.1186/1471-2296-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33(1):144–151. doi: 10.1177/0145721706297452. [DOI] [PubMed] [Google Scholar]
- 17.Ross LA, Frier BM, Kelnar CJ, Deary IJ. Child and parental mental ability and glycaemic control in children with type 1 diabetes. Diabet Med. 2001;18(5):364–369. doi: 10.1046/j.1464-5491.2001.00468.x. [DOI] [PubMed] [Google Scholar]
- 18.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 19.Sarkar U, Piette JD, Gonzales R, Lessler D, Chew LD, Reilly B, Johnson J, Brunt M, Huang J, Regenstein M, Schillinger D. Preferences for self-management support: findings from a survey of diabetes patients in safety-net health systems. Patient Educ Couns. 2008;70(1):102–110. doi: 10.1016/j.pec.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 21.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121(3):245–254. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schillinger D, Bindman AB, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician–patient communication among diabetes patients. Patient Educ Couns. 2004;52(3):315–323. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 23.Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, Rosano C, Rooks RN, Rubin SM, Ayonayon HN, Yaffe K. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 2006;54(5):770–776. doi: 10.1111/j.1532-5415.2006.00691.x. [DOI] [PubMed] [Google Scholar]
- 24.Tang YH, Pang SM, Chan MF, Yeung GS, Yeung VT. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nurs. 2008;62(1):74–83. doi: 10.1111/j.1365-2648.2007.04526.x. [DOI] [PubMed] [Google Scholar]
- 25.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 26.Echeverry D, Dike M, Jovanovic L, Wollitzer AO, Westphal S, Mudaliar S, Washington C, Davidson MB. Efforts to improve subsequent treatment of cardiovascular risk factors in older patients with diabetes hospitalized for a cardiac event. Am J Manag Care. 2005;11(12):758–764. [PubMed] [Google Scholar]
- 27.Gerber BS, Brodsky IG, Lawless KA, Smolin LI, Arozullah AM, Smith EV, Berbaum ML, Heckerling PS, Eiser AR. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care. 2005;28(7):1574–1580. doi: 10.2337/diacare.28.7.1574. [DOI] [PubMed] [Google Scholar]
- 28.Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, Weinberger M, Pignone M. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292(14):1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 29.Seligman HK, Wang FF, Palacios JL, Wilson CC, Daher C, Piette JD, Schillinger D. Physician notification of their diabetes patients' limited health literacy. A randomized, controlled trial. J Gen Intern Med. 2005;20(11):1001–1007. doi: 10.1111/j.1525-1497.2005.00189.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 31.Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol. 2008;2(3):509–517. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boren SA, Gunlock TL, Peeples MM, Krishna S. Computerized learning technologies for diabetes: a systematic review. J Diabetes Sci Technol. 2008;2(1):139–146. doi: 10.1177/193229680800200121. [DOI] [PMC free article] [PubMed] [Google Scholar]