Abstract
Background
Satisfactory glycemic control, meeting American Diabetes Association recommendations, is difficult to achieve. Technologically, this is most likely because the circle of care is incomplete. Many have suggested that the introduction of information technology may remedy the situation. However, previous attempts have not succeeded. Recognizing this, we evolved firmware that supports and links both the patient at home and their care providers in the clinic.
Firmware Design and Methods
The device includes software and a database, all contained in a standard USB flash drive. At home, patients use the database portion of the device (MyDiaBase). It fully complements their diabetes education while capturing pertinent self-management information by tracking self-monitored blood glucose data, body weight, medication dosing, physical activity, diet, lifestyle, and stress. In the clinic, providers use the RxChecker program to perform prescription checks that are based on their patients' outcomes data, thereby effectively closing the circle of care.
Keywords: algorithms, blood glucose control, disease management, evidence-based medicine, glucose monitoring, glycated hemoglobin, hypoglycemia, insulin resistance, intervention, outcome measures, remote monitoring, simulation, telemedicine
We hypothesize that closing the circle of care in diabetes may serve to empower both patients and providers, thereby safely improving glycemic control. Accordingly, this article describes a new educational support device for diabetes. The device takes in both personal and medical information. It facilitates the systematic review of treatment outcomes by supporting the provider to step through a pertinent prescription check. It also allows the provider to simulate the consequences of possible changes in the patient's prescription, overlaying all these visually in such a way as to highlight where the user may draw comfort or where the patient needs crucial medical intervention. Preliminary clinical experience with the device in a homogeneous group of type 1 patients all suffering intractable hypoglycemia is presented elsewhere.1
Materials
Educational Hardware and Software
The new, educational device is called MyDiaBase+RxChecker. It is firmware that is distributed in a standard, USB flash memory drive.2 The drive can be inserted into any USB port on any computer running any contemporary Microsoft Windows operating system. Macintosh users must have Intel OS-X and a PC emulator. The MyDiaBase portion of the device is suited for home use. The RxChecker portion of the device supports executing a prescription check by the provider at any office or clinic encounter. Together these occupy about 8 Mbytes of memory, which grow slowly with the accumulation of data entered by the patient. Flash drives of 10 Mbytes or more are fully adequate for this application.
Novel Features of MyDiaBase
For persons with diabetes, MyDiaBase is a personal diabetes registry and database. It stores patients' individual self-monitored blood glucose (SMBG) and the diabetes medical prescription (Rx). It is like a minielectronic medical record that allows users to review stored results graphically or to print all treatment outcomes as a diary or logbook.
Novel Features of RxChecker
With RxChecker, providers can improve the care of their patients by: (1) tracking body weight closely; (2) determining when any prescribed medications drift outside safe limits; (3) achieving better blood glucose control; (4) realizing safer hemoglobin A1c values; (5) using a built-in simulator to explore ±changes in their medications; (6) fostering less hypoglycemia, (7) allowing less hyperglycemia; (8) signaling when the patient should contact their doctor; (9) and clearly indicating what to talk about. All of these serve to keep the Rx in step with the patient's (changing) needs.
Impact on the Circle of Care
Together the MyDiaBase and RxChecker components help care providers track their diabetes management. The flash drive is a hardware platform that has become highly conducive to personal use. Reliability and portability with data safety and security are achieved at a relatively insignificant cost. Data in flash drives can be backed up and then restored if the device is lost.
Closing the circle of care may be facilitated when both patients and providers make use of the MyDiaBase+RxChecker technology.
Developer and Availability
The firmware was developed by a team directed by one of us (AMA). The rationale for the technology, along with its efficacy, validity, and safety, has been described elsewhere.3–6 Devices are available, and professional user training is offered.
Because this technology is novel, an educational initiative called the Diabetes Control and Complications Treatment Initiative has been launched. Its goal is to educate interested care providers in the advantages of using this technology in their clinical and private medical practices. Accordingly, repeating 1½-day courses are being scheduled that teach small groups of health care professionals how to use the technology as well as how to interpret the results of its use in patients. Free samples, along with subsequent access to MyDiaBase+RxChecker devices, are provided to participants in the courses. More information can be obtained by contacting albisser@nidm.org or browsing http://www.nidm.org.
Installation and Personalization
Each flash drive includes all the resources with which to install the MyDiaBase+RxChecker program. Installation must be done once on each computer where the user will be running the program in the future. Once installed, each MyDiaBase+RxChecker flash drive can be personalized with the patient's demographics, the providers' demographics, and the diabetes pharmacologic Rx. These are stored internally in a database that is secured, private, and password protected in case the flash drive is lost or stolen. At any time the patient can insert their current or previous self-management data, which are then also stored in the same database. These include their self-monitored blood glucose levels, medication dosing, body weight, and, optionally, other pertinent diet, lifestyle, exercise, and stress factors. Also, at anytime the provider can execute a comprehensive eight-point check of the patient's outcomes in view of their current prescription. Additionally, using a built-in simulator, providers can explore changes in the pharmacologic prescription that may reduce the risks of hypoglycemia or lower hyperglycemia. The impact of each change on the patient's glycated hemoglobin A1c (A1C) is predicted.
Numerical Analyses
The RxChecker portion of the device supports the performance of “prescription checks.” To these ends, a body mass index (BMI) analysis is done according to accepted standards.7 Levels of A1C are predicted from mean SMBG, as defined previously.8 Body weight regression analysis is done as described elsewhere.9
Resources
Nutritional considerations,10 physical activity/exercise parameters,11 education elements,12 and SMBG methodology13–15 where included in the software all follow formal guidelines.
MyDiaBase: The Patient Graphical User Interface (GUI)
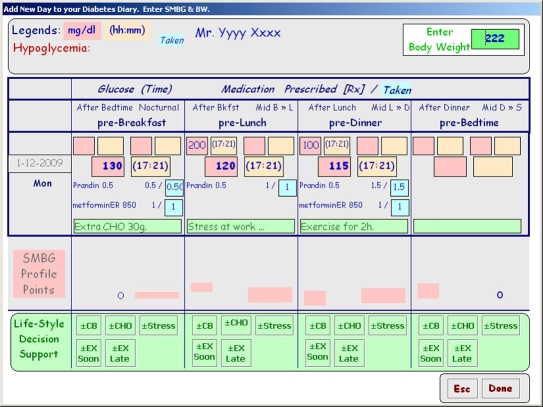
Figure 1 shows an image of the patient GUI. As an electronic diary, it captures the patient's self-management data at home, including date and time, up to 12 meal-related SMBGs per day, all medication dosing, and body weight, along with any typed comments to document diet, exercise, lifestyle, and/or stress. The diary serves to reinforce the patient's diabetes education. Glycemic profiles are formed from recent SMBG data (up to 7 antecedent days) and then used by the providers to review the safety and efficacy of their prescriptions and therapy.
Figure 1.
GUI screen image showing the patient interface of MyDiaBase. Note body weight; date and time fields; meal identifiers; and overnight, premeal, and postmeal categories, along with fields for medications prescribed and taken. SMBG profile points visually indicate to the patient when sufficient data have been entered to form a valid profile. Diet, stress, and exercise (lifestyle) annotations are shown with 19± buttons to facilitate the documentation task. bw, body weight; CHO, carbohydrate; CB, correction bolus.
The patient's interactions with the device are active. In this way, patients become more involved in their own care. This device does not passively accept SMBG readings downloaded intermittently from meters.
RxChecker: The Provider GUI Sequence
Each prescription check begins with an almost empty screen on the provider's GUI that fills progressively with each step. The process starts with current body weight entry. This leads to a comment about the BMI, which for this subject is “You are both overweight and obese.” Acknowledging this message leads to a graphic display of body weight over time (not shown) where the user can trigger a mathematical analysis that fits a regression line to recent body weight data. Statistical conclusions inform the user that their patient's body weight has been (1) rising, (2) stable, or (3) falling.
Next, the medical prescription is checked in order to determine if the total daily dose of each medication falls inside limits specified for each meal, for the whole day, or for both. As appropriate, either comforting or warning messages are displayed for the user to acknowledge.
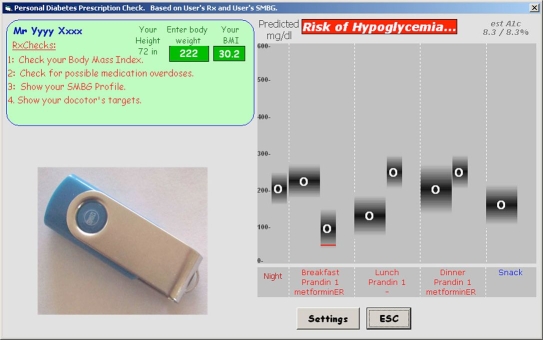
Then, using previously entered SMBG data, a profile is displayed so that the provider can view their patient's currently expected glycemic ranges at each profile point. The display helps the provider visually appreciate their patient's overall glycemic control with emphasis on those profile points that risk hypoglycemia and/or hyperglycemia. Such a profile is shown in Figure 2 on the right. Medications taken at the start of the breakfast, lunch, and dinner meal periods are shown beneath the individual profiles. No medication is taken in this example at bedtime (snack). In the upper left and under the heading RxChecks, Figure 2 also shows a list naming the first four items in the prescription check completed so far. Shown in the upper right corner of Figure 2, A1C predicted for this profile is 8.3%.
Figure 2.
GUI screen image illustrating the predicted glycemic profile on the right. (From left to right) Eight profile points illustrate, respectively, overnight, pre- and postbreakfast, pre- and postlunch, pre- and postdinner, and prebedtime measurement time points. Premeal medications are shown in the spaces spanning the breakfast, lunch, and dinner meal periods. There is no medication at bedtime (snack) in this case. A listing of the first four prescription checks completed thus far is shown on the upper left under the heading RxChecks. Estimated A1C is 8.3% as shown in the upper right corner. A sample device is also shown.
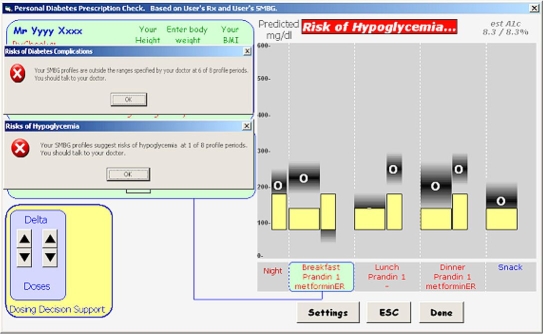
To determine how well the daily profile meets the physician's targets, a click of the mouse pointer applies the desired ranges to the SMBG profile. As shown in Figure 3, this GUI screen image again presents the predicted SMBG profile on the right as in Figure 2 but with the physician's target ranges applied. Also, superimposed on the upper left of Figure 3 is a comment emphasizing that six of eight profile points are outside the target ranges. Superimposed in the middle left is a comment emphasizing that one of eight profile points risks hypoglycemia. A large banner at the top to the right of Figure 3 reinforces the warning of risks of hypoglycemia. All comments as to the number of profile points outside the specified ranges and the number risking hypoglycemia are displayed for the user to acknowledge. This acknowledgment dismisses them from the screen to the database.
Figure 3.
GUI screen image showing predicted SMBG profile on right as in Figure 1 but with physician's target ranges applied. Also, superimposed on the upper left is a comment emphasizing that six of eight profile points are outside the physician's target ranges, risking diabetes complications. Superimposed in the middle left is a comment emphasizing that one of eight profile points risks hypoglycemia. Note banner at the top right with a similar warning. Up–down buttons titled delta doses in the lower left are used to simulate the impact of potential medication dosing changes on the profile shown.
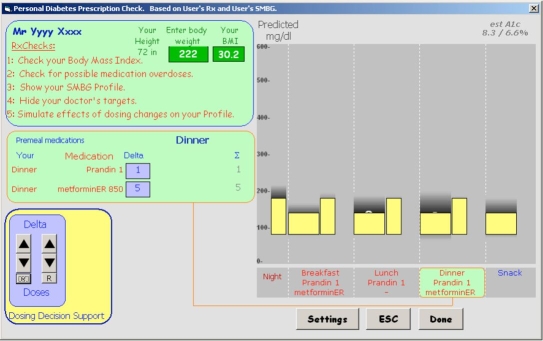
Finally, using the up–down buttons titled delta doses shown in the lower left of Figure 3, the provider can simulate the impact of potential medication dosing changes on the displayed profile. In this way, simulated interventions can be explored that may help eliminate the risks of hypoglycemia and/or improve overall glycemic control. An estimated A1C that is recalculated with each dosing change shows the predicted impact on overall glycemic control. As shown in Figure 4, four such prescription changes are predicted to consolidate all profile points into the target ranges. To achieve this, the simulator suggests (1) decreasing Prandin at breakfast to reduce the risks of hypoglycemia in the after breakfast period, (2) increasing Prandin at lunch to lower the postmeal rise, and (3) increasing Prandin at dinner to lower that postmeal rise. The simulator also suggests that the prescribed metformin ER at breakfast may need to be complemented with more metformin ER at dinner. As this is an educational resource, the simulation suggests more the direction of changes than actual amounts. In any case, with these potential changes, A1C is predicted to fall favorably from 8.3 to 6.6% and to do so without risking hypoglycemia.
Figure 4.
Potential impact of prescription changes predicted by the simulator to consolidate all profile points into physician-specified, target ranges. The simulator suggests decreasing Prandin at breakfast and increasing Prandin at lunch and at dinner while also adding metformin ER at dinner. Glycated hemoglobin A1c is predicted to fall from 8.3 to 6.6% without risking hypoglycemia.
Each potential change explored in the simulation is added to the database where it appears as a text comment that can be viewed in the diary (not shown). Where appropriate, the users are encouraged to talk to each other.
Closing the Circle of Care
Prescription checks done by providers may result in improved diabetes care in general and better (safer) glycemic control in particular. Among other benefits, triggered interventions may serve to correct details of a medical prescription that is no longer applicable. Prescription checks may teach the provider the effects (on their patient's glycemic control) of simulated changes in the pharmacologic prescription. This would be a valuable extension to medical practice. Furthermore, the knowledge so gained may offer substance for discussion at the next encounter.
Closing the circle of care in this way promises to empower users of the technology, both patients and providers, thereby improving the care of persons with diabetes.
Abbreviations
- A1C
glycated hemoglobin A1c
- BMI
body mass index
- GUI
graphical user interface
- Rx
prescription
- SMBG
self-monitored blood glucose
References
- 1.Albisser AM, Alejandro R, Sperlich M, Ricordi C. Prescription checking device promises to resolve intractable hypoglycemia. J Diabetes Science Technol. 2009;3:524–532. doi: 10.1177/193229680900300317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. USB flash drives [cited 2008 Feb]. Available from: http://en.wikipedia.org/wiki/USB_flash_drive.
- 3.Albisser AM, Harris RI, Albisser JB, Sperlich M. The impact of initiatives in education, self-management training, and computer-assisted self-care on outcomes in diabetes disease management. Diabetes Technol Ther. 2001;3(4):571–579. doi: 10.1089/15209150152811199. [DOI] [PubMed] [Google Scholar]
- 4.Albisser AM, Sakkal S, Wright C. Home blood glucose prediction: validation, efficacy and safety testing in clinical diabetes. Diabetes Technol Ther. 2005;7(3):487–496. doi: 10.1089/dia.2005.7.487. [DOI] [PubMed] [Google Scholar]
- 5.Albisser AM. A graphical user interface for diabetes management that integrates glucose prediction and decision support. Diabetes Technol Ther. 2005;3(2):264–273. doi: 10.1089/dia.2005.7.264. [DOI] [PubMed] [Google Scholar]
- 6.Albisser AM, Wright CE, Sakkal S. Averting iatrogenic hypoglycemia through glucose prediction in clinical practice: progress towards a new procedure in diabetes. Diabetes Res Clin Pract. 2007;76(2):207–214. doi: 10.1016/j.diabres.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Dietary Guidelines for Americans. 2005. Available from: http://www.health.gov/dietaryguidelines/dga2005/document/default.htm.
- 8.Rohlfing CL, Wiedmeyer HM, Little RR, England JD, Tennill A, Goldstein DE. Defining the relationship between plasma glucose and HbA(1c): analysis of glucose profiles and HbA1c in the Diabetes Control and Complications Trial. Diabetes Care. 2002;25(2):275–278. doi: 10.2337/diacare.25.2.275. [DOI] [PubMed] [Google Scholar]
- 9. Web pages that perform statistical calculations [cited 2008 Feb]. Available from: http://statpages.org/#Comparisons.
- 10.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD, Purnell JQ, Wheeler M. American Diabetes Association. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2003;26(Suppl 1):S51–S61. doi: 10.2337/diacare.26.2007.s51. [DOI] [PubMed] [Google Scholar]
- 11.Zinman B, Ruderman N, Campaigne BN, Devlin JT, Schneider SH. American Diabetes Association. Physical activity/exercise and diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S73–S77. doi: 10.2337/diacare.26.2007.s73. [DOI] [PubMed] [Google Scholar]
- 12.Mensing C, Boucher J, Cypress M, Weinger K, Mulcahy K, Barta P, Hosey G, Kopher W, Lasichak A, Lamb B, Mangan M, Norman J, Tanja J, Yauk L, Wisdom K, Adams C. National standards for diabetes self-management education. Diabetes Care. 2005;28(Suppl 1):S72–S79. doi: 10.2337/diacare.28.suppl_1.s72. [DOI] [PubMed] [Google Scholar]
- 13.American Diabetes Association. Self-monitoring of blood glucose. Diabetes Care. 1994;17(1):81–86. doi: 10.2337/diacare.17.1.81. [DOI] [PubMed] [Google Scholar]
- 14.Ziegler O, Kolopp M, Got I, Genton P, Debry G, Drouin P. Reliability of self-monitoring of blood glucose by CSII-treated patients with type I diabetes. Diabetes Care. 1989;12(3):184–188. doi: 10.2337/diacare.12.3.184. [DOI] [PubMed] [Google Scholar]
- 15.Kabadi UM, O'Connell KM, Johnson J, Kabadi M. The effect of recurrent practice at home on the acceptability of capillary blood glucose readings. Accuracy of self blood glucose testing. Diabetes Care. 1994;17(10):1110–1123. doi: 10.2337/diacare.17.10.1110. [DOI] [PubMed] [Google Scholar]