Abstract
Background
Annual retinal screening of patients with diabetes is the standard clinical practice to prevent visual impairment and blindness from diabetic retinopathy. Telemedicine-based diabetic retinopathy screening (DRS) in primary care settings can effectively detect sight-threatening retinopathy and significantly increase compliance with annual retinal exams. EyePACS is a license-free Web-based DRS system designed to simplify the process of image capture, transmission, and review. The system provides a flexible platform for collaboration among clinicians about diabetic retinopathy.
Methods
Primary clinic personnel (i.e., nursing, technical, or administrative staff) are trained and certified by the EyePACS program to acquire retinal images from standard digital retinal cameras. Relevant clinical data and eight high-resolution images per patient (two external and six retinal images) are encrypted and transmitted to a secure Internet server, using a standard computer and Web browser. Images are then interpreted by certified EyePACS reviewers or local eye care providers who are certified through the EyePACS Retinopathy Grading System. Reports indicating retinopathy level and referral recommendations are transmitted back to primary care providers through the EyePACS Web site or through interfaces between EyePACS and Health Level 7-compliant electronic medical records or chronic disease registries.
Results
The pilot phase of the EyePACS DRS program in California (2005–2006) recorded 3562 encounters. Since 2006, EyePACS has been expanded to over 120 primary care sites throughout California and elsewhere recording over 34,000 DRSs. The overall rate of referral is 8.21% for sight-threatening retinopathy and 7.83% for other conditions (e.g., cataract and glaucoma).
Conclusion
The use of license-free Web-based software, standard interfaces, and flexible protocols has allowed primary care providers to adopt retinopathy screening with minimal effort and resources.
Keywords: diabetes, Internet, ophthalmology, optometry, retinopathy, telemedicine
Introduction
Annual retinal screening of patients with diabetes is the standard clinical practice to prevent visual impairment and blindness from diabetic retinopathy.1,2 The traditional examination of the retina by ophthalmoscopy usually requires dilated pupils, a skilled examiner, and a visit to the eye care provider (ophthalmologist or optometrist) separate from the primary care visits. Numerous studies in the United States have shown that many diabetes patients fail to seek or receive this important examination on a regular basis. Depending on the health care system, the average compliance rate may vary from approximately 30–60%.3 Under the Healthcare Effectiveness Data and Information Set program, a quality assessment program for managed care organizations sponsored by the National Committee for Quality Assurance, examinations to detect diabetic retinopathy remains one of the poorest quality measures.3 This shortfall has been attributed to a variety of factors such as socioeconomic barriers (e.g., income level, inadequate health insurance, and time away from work), health system barriers (e.g., inadequate specialist referral system, insufficient number of eye care providers, and inadequate public health funding), and educational/cultural barriers (e.g., education level, health illiteracy, language barriers, and competing nonmedical healing traditions).4,5
A number of these problems can be overcome by incorporating retinopathy screening into primary care practices, using telemedicine evaluation of retinal images. Once a digital retinal camera is acquired by a primary care center, clinic personnel can be trained to use the camera, and remote evaluation of retinal images by eye care specialists can be performed reliably. The screening process can be simpler and more cost-efficient than sending the patients to an eye care provider's office for a live evaluation. Compliance with the recommended annual retinal evaluation can be significantly increased by using such a system, especially if the digital retinal imaging can be performed at the same time as a regular primary care visit.6,7
A successful and reliable telemedicine diabetic retinopathy screening (DRS) system must be comparable to a live retinal examination in the detection of vision-threatening retinopathy. Both the sensitivity to detect important retinal disease and the specificity with which the system operates are important to the public health acceptability and utility of the system. If clinically important retinopathy is missed too often (false negatives/low sensitivity) or patients without important retinopathy are referred to an ophthalmologist too frequently (false positives/low specificity), then the telemedicine screening system may not be an acceptable alternative. Numerous studies have shown that adequate sensitivity and specificity can been achieved with a number of telemedicine systems.8–14 This includes systems in which nonmydriatic cameras are used to capture retinal images through undilated pupils or systems in which images are taken with a mydriatic or nonmydriatic digital retinal camera through dilated pupils. Some studies advocate taking stereoscopic (three-dimensional) images, while others find nonstereoscopic images adequate. The main arguments favoring undilated pupils are the reduction in time required and greater patient acceptability. Pupillary dilation, while relatively safe, requires higher level medical supervision in many settings and places some constraints on patients' performing certain visual tasks until the pupillary dilation dissipates. There is good evidence, however, that pupillary dilation reduces the proportion of patients with ungradeable retinal images.10,11
Most commercial telemedicine systems are proprietary in that the end users (primary care centers) must use licensed software built into the imaging system for storage and transmission of images; in some cases, purchase of the system may require the use of costly image evaluation services as part of the package. The development of EyePACS has been driven by a desire to simplify the process of image capture, transmission, and storage, to maintain flexibility in how the images are evaluated, and to keep the costs low.15 Some systems, such as the U.S. Veterans Administration VistA program, are license-free; however, implementation of these public domain programs has been reported to be costly and complex. Efforts, such as the OpenVista project, aspire to reduce the complexity and cost of implementing these picture archive and communication system (PACS) and image-capable electronic medical record (EMR) programs; however, many clinics and diabetes programs often require a simple specific solution that is easily implemented for diabetic retinopathy detection. Moreover, many PACS and EMR systems restrict activity to users within an enterprise-specific network, making it difficult to connect with specialists and other users outside an organization. It is the goal of this article to demonstrate how end users of the EyePACS system can relatively easily avail themselves of telemedicine-based DRS services, even with limited resources, geographic remoteness, and lack of prior experience.
Methodology in EyePACS
Acquisition of Retinal Images
The EyePACS system can accommodate digital retinal images from a variety of camera sources. For simplicity, it is recommended that a nonmydriatic digital retinal camera be used. The protocol using the Canon CR-DGi and Canon CR-1 nonmydriatic cameras can be accessed on the EyePACS Web site (see EyePACS Related Resources, EyePACS Photographer Manual, www.eyepacs.org). This describes the protocol used in the EyePACS program in California, an effort sponsored by the California Health Care Foundation (CHCF) and implemented in a number of federally qualified “safety net clinics” throughout the state (see the CHCF Web site at www.chcf.org/topics/view.cfm?itemID=133378.)
Photographers participating in this program undergo a training and certification process. It is recommended that the training be led by someone proficient in the use of the camera and familiar with the specific EyePACS imaging protocol. In California, this function is performed by one of several regional EyePACS coordinators or by suppliers of the retinal cameras. The photographer candidates are usually recruited from the clinic staff and may be nursing personnel, technical staff, or administrative staff. In the EyePACS program in Guanajuato, Mexico, the primary care physicians perform the imaging. For certification, candidates must submit 10 sets of images that are of adequate quality for grading before they can begin to capture images on diabetes patients.
End users in other settings can set up their own training and certification programs for photographers. It is strongly recommended, however, that experienced personnel perform the training and that the certification program be rigorous enough to ensure adequate quality images. End users can contract with EyePACS to oversee the certification process. In that case, EyePACS personnel evaluate test images uploaded to the EyePACS Web site and provide feedback on quality and technique to the photographer candidates.
The specific imaging protocol in the EyePACS California program includes the following:
one external image of each eye for an assessment of the corneal clarity, pupil size, and lens clarity;
three internal imaging fields of each eye: primary field including the optic disk and macula, disk field centered on the optic disk, and temporal fieldincluding the macula and the retina temporal to the macula (an EyePACS study is underway to test whether three internal imaging fields are needed or whether fewer fields can achieve adequate sensitivity and specificity to detect vision-threatening retinopathy); and
undilated pupils, unless the pupil is small and adequate images cannot be obtained, in which case one or both pupils are dilated according to protocol.
The three-field imaging strategy has been validated in several studies.16 Sensitivity and specificity, when compared to the seven-field Early Treatment Diabetic Retinopathy Study (ETDRS) gold standard, were found to be 89% and 97%, respectively, by Bursell and colleagues for proliferative retinopathy,12 and Cavellerano and associates found 89.3% agreement within one level of retinopathy when compared to dilated comprehensive examination by a retinal specialist.20 The EyePACS research group is currently conducting a study to validate the current protocol against the seven-field ETDRS gold standard.
Flexible Technology for Transmitting Retinal Images
Retinal images and related patient data for one or more patients can be uploaded to the encrypted EyePACS Web site on a standard computer with broadband Internet access. The standard memory card from the retinal camera is placed into a typical card reader attached to the computer. The minimum technical requirements for efficient connectivity to the internet are (1) allowing the upload of images to a trusted Internet site, (2) having at least 128 KB/sec Internet connection speed, and (3) allowing a Secure Socket Link connection at 128-bit encryption in a Web browser (all recent versions of major Web browsers include this feature) to verify the identity of users when setting up local user accounts.
Storage of Digital Retinal Images and Relevant Patient Data and Secure Access to the Data
EyePACS uses license-free software at a secure central server to store digital retinal images and relevant patient data. Users of EyePACS (e.g., individual providers, clinics, and health departments) are assigned IDs and passwords that provide access to the patient database for their particular clinic. In larger health care systems, such as health departments with multiple clinic sites, each clinic can be assigned an ID and password that allows clinic personnel access to their patient data only, while administrators or medical directors can be allowed access to the data for all the clinics in their jurisdiction.
Structured Image Evaluation Protocol
EyePACS uses an image evaluation protocol, the EyePACS Retinopathy Grading System (ERGS), based on the ETDRS.18 The protocol evaluates the presence and severity of the discrete retinal lesions associated with diabetic retinopathy. The lesions graded are: microaneurysms, retinal hemorrhages with or without microaneurysms (HMA), cotton wool spots, intraretinal microvascular abnormalities (IRMA), venous beading, new vessels (new vessels on the disk and new vessels elsewhere), fibrous proliferation, vitreous hemorrhage or preretinal hemorrhage, and hard exudates (HE). In addition, the presence or absence of laser scars (focal and panretinal) is graded.
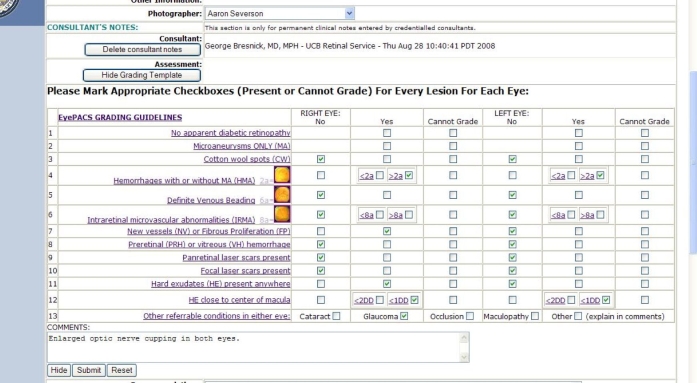
Readers grade each lesion type separately in each eye, using an online grading template that records a choice for each lesion type among “no” (absent), “yes” (present), or “cannot grade”(Figure 1). For some of the lesions (HMA and IRMA), the lesion severity is graded in comparison to a specific ETDRS standard photograph.18 In order to facilitate this comparison, a link is provided in the body of the template to the relevant ETDRS standard photographic image.
Figure 1.
Grading template used for recording observations.
After the severity of all of the lesions has been graded, a computer algorithm processes the severity grades of the discrete retinal lesions and computes two summary grades:
Overall retinopathy severity level.
Macular edema severity level.
Calculating the overall retinopathy severity and macular edema severity with a computer algorithm, rather than having each reader determine the levels, affords greater standardization and reliability to the system. Since the definition of the levels is rule based (determined by the aggregate of the severity of individual lesion types), more reproducible summary severity levels can be achieved by a rule-based algorithm rather than by the gestalt impression of the reader.
The overall retinopathy severity levels are based on those established by the ETDRS modification of the Airlie House classification of diabetic retinopathy.19 The EyePACS retinopathy levels are adapted from the international classification of diabetic retinopathy developed by the International Council of Ophthalmology (www.icoph.org/standards/pdrclass.html) and adopted by the American Academy of Ophthalmology.17
The first level, for eyes in which no retinal lesions associated with diabetic retinopathy are found, is
no apparent diabetic retinopathy.
Nonproliferative diabetic retinopathy (NPDR) is collapsed from the ETDRS classification into 3 levels:
Mild NPDR.
Moderate NPDR.
Severe NPDR.
Proliferative diabetic retinopathy (PDR) is collapsed into
one level:
PDR.
The grading of macular edema is not based on retinal thickening in the macula, as in the ETDRS grading protocol, but rather on the surrogate lesion of HE, which is usually associated with adjacent retinal thickening and is predictive of the presence of macular edema.21 (Because the EyePACS DRS protocol uses nonstereo images, it is not possible to grade retinal thickening in the images.)
The EyePACS macular edema severity levels are as follows:
No macular edema: No HE within 2 disk diameters of the center of the macula.
Macular edema, not clinically significant: Any HE within 2 disk diameters of the center of the macula but not within 1 disk diameter of the center of the macula.
Macular edema, clinically significant: Any HE within 1 disk diameter of the center of the macula.
Based on a published retrospective analysis of the ETDRS photographic database,21 this algorithm should detect “clinically significant macular edema” (CSME) as defined in the ETDRS (based on retinal thickening and HE graded in stereo color photographs) with a sensitivity of 94% and a specificity of 54%.22 This level of sensitivity is considered adequate by accepted public health screening criteria. While one would like to see a greater specificity (i.e., fewer false positives), unpublished data from the ETDRS have shown that, among eyes with HE within 1 disk diameter of the center of the macula and without CSME at baseline examination, more than 50% of such eyes develop CSME within the first year of follow-up.23 Therefore, while false positives may result in the “over-referral” of patients to an ophthalmologist, placing these patients under close surveillance has merits because of their high risk for developing CSME.
The primary purpose for establishing the summary levels for overall retinopathy severity and macular edema severity is to guide clinicians (eye care providers and primary care physicians) in determining follow-up recommendations for patients based on the screening results. The severity levels in both eyes (or in the worse eye, if the screening results are asymmetrical in the two eyes) are used as the referral guideline. In general, patients with severe NPDR, PDR, or CSME are recommended for prompt referral to an ophthalmologist because of the relatively high risk for developing vision loss without closer surveillance and, in appropriate cases, therapeutic intervention with laser, vitrectomy, and/or other treatment.
Patients with lesser degrees of retinopathy and macular edema are usually recommended for repeat imaging in one year. However, the EyePACS grading system allows the reader (eye care provider) to override the standard follow-up recommendations and to add explanatory notes in such cases. For example, the reader may consider an eye with a summary level of moderate NPDR to be on the border between moderate and severe NPDR. The reader may choose to recommend follow-up in less than one year, either through repeat imaging in 4–6 months or through a nonurgent referral to an ophthalmologist.
The follow-up decision may also be influenced by the capacity of the health care system to accommodate referrals or by the perceived reliability of the patient to return for repeat imaging. In a health care system where referral resources are severely limited (because of fiscal restraints, limited capacity of specialty services, or geographic remoteness), the grader or the primary care physician may choose to repeat imaging in 4–6 months for a patient with severe NPDR rather than immediately referring the patient to an ophthalmologist.
The reader also grades images for the presence of certain ocular conditions other than diabetic retinopathy that can be discerned in the external and internal images of each eye. These include cataract, glaucoma (based on optic disk appearance), retinal vascular occlusion, maculopathy (besides diabetic maculopathy), or “other” to be specified. The presence of clinically significant nondiabetic abnormalities are used by the reader (in addition to the diabetic retinopathy assessment) to determine follow-up recommendations.
In order to maintain an appropriate level of quality in the grading program, EyePACS offers subscribers a quality control option in which 3–5% of eyes already graded by a certified eye care provider will undergo repeat grading by a retinal subspecialist who is an expert in the EyePACS grading protocol. Clinically significant discrepancies in grading between the certified reader and the expert reader are flagged and discussed with the certified reader as part of a grading remediation intervention program.
At the end of the grading process, the reader assesses the quality of the images for grading purposes. One of the following categories of image quality is chosen from a drop-down menu: “excellent,” “good,” “adequate,” “insufficient for full interpretation,” or “insufficient for any interpretation.” EyePACS administrative personnel use the results of the image quality assessments to identify individual photographers who need remedial intervention to improve the quality of their imaging techniques and/or equipment if a pattern of image quality problems is seen. In a given patient, image quality problems may indicate that the patient has clinically significant ocular media abnormalities such as cataracts or corneal disease. If the images are inadequate for interpretation, the grader and/or the primary care physician can determine whether repeat imaging (possibly with pupillary dilation) or referral to an ophthalmologist is the more appropriate course of action.
Flexible Reader Program
EyePACS allows for a variety of arrangements for the grading of the retinal images. In this sense, it is a distributive virtual system and allows readers to function in dispersed locations linked to EyePACS through the EyePACS Web site. In order to assure adequate image quality for grading purposes, the reader must have a computer monitor with a minimum of 1000/1 contrast ratio and 32-bit color quality at 1200 by 1024 pixels.
The most common models of grading strategies based on actual current arrangements are as follows:
Grading performed under contract by certified EyePACS eye care provider readers. Health care entities can contract with EyePACS to grade image sets on a per-case basis. Per-case charges are kept low in order to extend this option to health care systems with limited resources.
Grading performed by local eye care providers, internal to the health care system. A primary care clinic or public health department that has “in-house” eye care providers (optometrists and/or ophthalmologists) on staff can have those eye care providers certified for grading under the EyePACS certification program. The eye care providers can then perform the gradings on patients within that system as part of the providers' regular or “add-on” duties. This option is advantageous both for reasons of cost control and for clinical care efficiency. For example, a large group practice with a substantial number of diabetes patients may find it more cost-effective to have their in-house ophthalmologist or optometrist satisfy the annual retinal screening requirement for the diabetes patients by grading retinal images and examining a selective group of patients rather than by examining all the patients in the system. Since, on average, 80% of all diabetes patients will have no or minimal retinopathy at any point in time, it is considerably more efficient for the eye care provider selectively to see only the 20% or less of patients who have moderate NPDR or worse, compared to examining all the diabetes patients on an annual basis. Readers are encouraged to be trained and certified in the ERGS and to participate in the grading quality control program.
Grading performed by local eye care providers, external to the health care system. In health care systems where there are no in-house eye care providers, the image grading can be performed by an eye care provider outside of the system, preferably, a clinician in the community who has a referral relationship with the health care system. This way, the local eye care provider has an added stake in performing accurate and timely gradings of the image sets. In addition, this reinforces the relationship between the eye care provider and the clinic and perhaps encourages the eye care provider to accept the broad spectrum of patients ranging from uninsured to fully insured. As in the two previous models, readers are encouraged to be trained and certified in ERGS and to participate in the grading quality control program.
Electronic Reporting System
A report with patient data and grading results for each patient screened are transmitted to the referring primary care physician electronically through the EyePACS Web site. In order to facilitate the integration of screening reports with clinical data from other applications, EyePACS has a Health Level 7 (www.hl7.org) interface that allows bidirectional communication with chronic disease registries, such as i2iTracks, and EMR systems, such as Epicare. The EyePACS interface strategy has had to incorporate version 2.x, the predominant Health Level 7 version standard; however, interoperability will follow Health Level 7's Clinical Document Architecture in version 3 for interoperability in the future. Visible light object and ophthalmic image object standards within Digital Imaging and Communications in Medicine have been considered for implementation within EyePACS; however, JPEG images appear to be the most pervasive output of current retinal imaging devices.
Results of EyePACS Diabetic Retinopathy Screening Programs
During an initial pilot phase of the CHCF-supported EyePACS DRS program in California (2005–2006), a total of 3562 encounters were recorded. Since 2006, EyePACS has been expanded to over 120 primary care sites throughout California and elsewhere. At the end of 2008, EyePACS recorded over 34,100 DRS encounters. The overall rate of referral is 8.21% for sight-threatening retinopathy and 7.83% for other conditions.
Conclusion
EyePACS was designed to reduce barriers to access to retinal exams for diabetes patients. The use of license-free Web-based software, standard interfaces, and flexible protocols has allowed primary care providers to adopt retinopathy screening with minimal effort and resources. EyePACS continues to develop as a Web 2.0 system,24 providing interclinician communication, patient services, and clinical education in a rapidly growing online community.
Abbreviations
- CHCF
California Health Care Foundation
- CSME
clinically significant macular edema
- DRS
diabetic retinopathy screening
- EMR
electronic medical record
- ERGS
EyePACS Retinopathy Grading System
- ETDRS
Early Treatment of Diabetic Retinopathy Study
- HE
hard exudates
- HMA
retinal hemorrhages with or without microaneurysms
- IRMA
intraretinal microvascular abnormalities
- NPDR
nonproliferative diabetic retinopathy
- PACS
picture archive and communication system
- PDR
proliferative diabetic retinopathy
References
- 1.Fong DS, Aiello L, Gardner TW, King GL, Blankenship G, Cavallerano JD, Ferris FL III, Klein R. American Diabetes Association. Retinopathy in diabetes. Diabetes Care. 2004;27(Suppl 1:S84–7) doi: 10.2337/diacare.27.2007.s84. [DOI] [PubMed] [Google Scholar]
- 2.Screening guidelines for diabetic retinopathy. American College of Physicians, American Diabetes Association, and American Academy of Ophthalmology. Ann Intern Med. 1992;116(8):683–685. [PubMed] [Google Scholar]
- 3.Lee PP, Feldman ZW, Ostermann J, Brown DS, Sloan FA. Longitudinal rates of annual eye examination of persons with diabetes and chronic eye diseases. Ophthalmology. 2003;110(10):1952–1959. doi: 10.1016/S0161-6420(03)00817-0. [DOI] [PubMed] [Google Scholar]
- 4.Mukamel DB, Bresnick GH, Wang Q, Dickey CF. Barriers to compliance with screening guidelines for diabetic retinopathy. Ophthalmic Epidemiol. 1999;6(1):61–72. doi: 10.1076/opep.6.1.61.1563. [DOI] [PubMed] [Google Scholar]
- 5.Moss SE, Klein R, Klein BE. Factors associated with having eye examinations in persons with diabetes. Arch Fam Med. 1995;4(6):529–534. doi: 10.1001/archfami.4.6.529. [DOI] [PubMed] [Google Scholar]
- 6.Wilson C, Horton M, Cavallerano J, Aiello LM. Addition of primary care-based retinal imaging technology to an existing eye care professional referral program increased the rate of surveillance and treatment of diabetic retinopathy. Diabetes Care. 2005;28(2):318–322. doi: 10.2337/diacare.28.2.318. [DOI] [PubMed] [Google Scholar]
- 7.Taylor CR, Merin LM, Salunga AM, Hepworth TJ, Crutcher TD, O'Day DM, Pilon BA. Improving diabetic retinopathy screening ratios using telemedicine-based digital retinal imaging technology: the Vine Hill study. Diabetes Care. 2007;30(3):574–578. doi: 10.2337/dc06-1509. [DOI] [PubMed] [Google Scholar]
- 8.Klein R, Klein BE, Neider MW, Hubbard LD, Meuer SM, Brothers RJ. Diabetic retinopathy as detected using ophthalmoscopy, a non-mydriatic camera and a standard fundus camera. Ophthalmology. 1985;92(4):485–491. doi: 10.1016/s0161-6420(85)34003-4. [DOI] [PubMed] [Google Scholar]
- 9.Lin DY, Blumenkranz MS, Brothers RJ, Grosvenor DM. The sensitivity and specificity of single-field nonmydriatic mono-chromatic digital fundus photography with remote image interpretation for diabetic retinopathy screening: a comparison with ophthalmoscopy and standardized mydriatic color photography. Am J Ophthalmol. 2002;134(2):204–213. doi: 10.1016/s0002-9394(02)01522-2. [DOI] [PubMed] [Google Scholar]
- 10.Lawrence MG. The accuracy of digital-video retinal imaging to screen for diabetic retinopathy: an analysis of two digital-video retinal imaging systems using standard stereoscopic seven-field photography and dilated clinical examination as reference standards. Trans Am Ophthalmol Soc. 2004;102:321–340. [PMC free article] [PubMed] [Google Scholar]
- 11.Boucher MC, Gresset JA, Angioi K, Olivier S. Effectiveness and safety of screening for diabetic retinopathy with two nonmydriatic digital images compared with the seven standard stereoscopic photographic fields. Can J Ophthalmol. 2003;38(7):557–568. doi: 10.1016/s0008-4182(03)80109-6. [DOI] [PubMed] [Google Scholar]
- 12.Joslin Vision Network Research Team. Bursell SE, Cavallerano JD, Cavallerano AA, Clermont AC, Birkmire-Peters D, Aiello LP, Aiello LM. Stereo nonmydriatic digital-video color retinal imaging compared with Early Treatment Diabetic Retinopathy Study seven standard field 35-mm stereo color photos for determining level of diabetic retinopathy. Ophthalmology. 2001;108(3):572–585. doi: 10.1016/s0161-6420(00)00604-7. [DOI] [PubMed] [Google Scholar]
- 13.Fransen SR, Leonard-Martin TC, Feuer WJ, Hildebrand PL. Inoveon Health Research Group. Clinical evaluation of patients with diabetic retinopathy: accuracy of the Inoveon diabetic retinopathy-3DT system. Ophthalmology. 2002;109(3):595–601. doi: 10.1016/s0161-6420(01)00990-3. [DOI] [PubMed] [Google Scholar]
- 14.Schiffman RM, Jacobsen G, Nussbaum JJ, Desai UR, Carey JD, Glasser D, Zimmer-Galler IE, Zeimer R, Goldberg MF. Comparison of a digital retinal imaging system and seven-field stereo color fundus photography to detect diabetic retinopathy in the primary care environment. Ophthalmic Surg Lasers Imaging. 2005;36(1):46–56. [PubMed] [Google Scholar]
- 15.Rudnisky CJ, Tennant MT, Weis E, Ting A, Hinz BJ, Greve MD. Web-based grading of compressed stereoscopic digital photography versus standard slide film photography for the diagnosis of diabetic retinopathy. Ophthalmology. 2007;114(9):1748–1754. doi: 10.1016/j.ophtha.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for progression of diabetic retinopathy. Ophthalmology. 1991;98(5 Suppl):823–833. ETDRS report number 12. [PubMed] [Google Scholar]
- 17.Wilkinson CP, Ferris FL III, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT. Global Diabetic Retinopathy Project Group. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677–1682. doi: 10.1016/S0161-6420(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 18.Cuadros J, Sim I. EyePACS: an open source clinical communication system for eye care. Stud Health Technol Inform. 2004;107(Pt 1):207–211. [PubMed] [Google Scholar]
- 19.Whited JD. Accuracy and reliability of teleophthalmology for diagnosing diabetic retinopathy and macular edema: a review of the literature. Diabetes Technol Ther. 2006;8(1):102–111. doi: 10.1089/dia.2006.8.102. [DOI] [PubMed] [Google Scholar]
- 20.Cavallerano AA, Cavallerano JD, Katalanic P, Tolson AM, Aiello LP, Aiello LM. Joslin Vision Network Clinical Team. Use of Joslin Vision Network digital-video nonmydriatic retinal imaging to assess diabetic retinopathy in a clinical program. Retina. 2003;23(2):215–223. doi: 10.1097/00006982-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Early Treatment Diabetic Retinopathy Study Research Group. Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the Airlie House classification. Ophthalmology. 1991;98(5 Suppl):786–806. ETDRS report number 10. [PubMed] [Google Scholar]
- 22.Bresnick GH, Mukamel DB, Dickinson JC, Cole DR. A screening approach to the surveillance of patients with diabetes for the presence of vision-threatening retinopathy. Ophthalmology. 2000;107(1):19–24. doi: 10.1016/s0161-6420(99)00010-x. [DOI] [PubMed] [Google Scholar]
- 23.Bresnick GH. Unpublished data [Google Scholar]
- 24.Eysenbach G. Medicine 2.0: social networking, collaboration, participation, apomediation, and openness. J Med Internet Res. 2008;10(3):e22. doi: 10.2196/jmir.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]