Abstract
Background
The ability to measure patient blood glucose levels at bedside in hospitalized patients and to transmit those values to a central database enables and facilitates glucose control and follow-up and is an integral component in the care of the hospitalized diabetic patient.
Objective
The goal of this study was to evaluate the performance of an institutional glucometer employed in the framework of the Program for the Treatment of the Hospitalized Diabetic Patient (PTHDP) at E. Wolfson Medical Center, Holon, Israel.
Methods
As part of the program to facilitate glucose control in hospitalized diabetic patients, an institutional glucometer was employed that permits uploading of data from stands located in each inpatient department and downloading of that data to a central hospital-wide database. Blood glucose values from hospitalized diabetic patients were collected from August 2007 to October 2008. The inpatient glucose control program was introduced gradually beginning January 2008.
Results
During the follow-up period, more than 150,000 blood glucose measures were taken. Mean glucose was 195.7 ± 99.12 mg/dl during the follow-up period. Blood glucose values declined from 206 ± 105 prior to PTHDP (August 2007–December 2007) to 186 ± 92 after its inception (January 2008–October 2008). The decline was associated significantly with time (r = 0.11, p < 0.0001). The prevalence of blood glucose values lower than 60 mg/dl was 1.48% [95% confidence interval (CI) 0.36%] prior to vs 1.55% (95% CI 0.37%) following implementation of the PTHDP. Concomitantly, a significant increase in the proportion of blood glucose values between 80 and 200 mg/dl was observed, from 55.5% prior to program initiation vs 61.6% after program initiation (p < 0.0001).
Conclusions
The present study was designed to observe changes in institution-wide glucose values following implementation of the PTHDP. Information was extracted from the glucometer system itself. Because the aforementioned study was not a clinical trial, we cannot rule out that factors other than introduction of the program could explain some of the variability observed. With these limitations in mind, it nevertheless appears that the PTHDP, of which the institutional glucometer is an integral, essential component, was associated with improved blood glucose values in the hospitalized diabetic patient.
Keywords: standards of care, hospitalization, institutional glucometer, point of care
Background
Hyperglycemia is a frequently observed metabolic disorder prevalent in approximately one-third of all hospitalized patients.1,2 In approximately two-thirds of these cases, the patients had been diagnosed previously with diabetes. The remaining cases of hyperglycemia reflect either stress secondary to acute illness or an expression of heretofore undiagnosed diabetes.3
Until recently, hyperglycemia during hospitalization was viewed as a phenomenon with relatively little clinical significance. More current studies have demonstrated the importance of regulating blood glucose levels in patients hospitalized in intensive care units.4–6 It has been estimated that one in four hospitalized patients has diagnosed diabetes and that one in five has undiagnosed diabetes.7
Despite the enormity and importance of the problem, diabetes care in the hospitalized patient is not always optimal. Improvement of diabetes control in the hospitalized patient requires the implementation of programs designed specifically to meet these objectives.8,9 Known obstacles to program implementation and success should be taken into consideration and addressed; for example, medical and nursing personnel frequently list concern surrounding increased hypoglycemic events as a reason for not striving for tighter glucose control.10
Prior to implementation of the institution-wide glucometer, results of blood glucose readings were recorded into the patient medical chart at bedside and into the medical record. This manual method of data recording makes efficient follow-up of blood glucose trends difficult, if not impossible, which decreases the likelihood of implementing effective treatment for hyperglycemia. Use of an institution-wide glucometer permits between-department comparisons of treatment efficacy, permits within-department evaluations over time, and, with wider use, may permit comparisons of efficacy between institutions.
Advancements in information technology permit the real-time transfer of capillary blood glucose values measured at point of care (bedside) directly to a central, institutional database as well as to the patient's electronic laboratory record. Additionally, the accompanying system permits centralized data storage and both retro- and prospective analyses blood glucose trends in the hospitalized patient.
Objectives
In January 2008, the Program for the Treatment of the Hospitalized Diabetic Patient (PTHDP) was initiated at E. Wolfson Medical Center in Holon, Israel. The first step in program implementation was introduction of the institution-wide glucometer for blood glucose monitoring. The present report was designed to examine trends in blood glucose levels measured with the institutional glucometer among diabetic patients hospitalized at this institution, as an estimate of the efficacy of this tool and as an evaluation of the initial efficacy of the PTHDP. Clinical and demographic data were extracted from the glucometer system itself. The present study is observational, not a clinical trial, and cannot control for all potential confounders. As such, the authors acknowledge that factors other than introduction of the program could explain some of the variability observed.
Methods
Setting, Data Collection, and Definitions
In August 2007, the Edith Wolfson Medical Center, a 700-bed government hospital, which serves approximately 500,000 residents of the Holon-Bat Yam-Yaffo-West RishonLeziyon area south of Tel Aviv, launched the PTHDP by introducing use of the institutional blood glucose monitoring system (IGMS) first to the internal medicine departments and later to the various surgical departments so that it was gradually employed by all inpatient departments. The remaining components of the PTHDP were introduced in January 2008.
Included in the present report are data from all internal medicine and surgical departments and intensive care units. Data from pediatric, obstetrics, and emergency care departments were not included. Data reported are those from the 15th day of each month, starting from August 2007 to October 2008. Included were the results of any blood glucose test measured using the time stamped from 12:01 through 23:59 on the 15th day of a given month. Hypoglycemia was defined as a blood glucose test <60 mg/dl, whereas hyperglycemia was defined as any blood glucose test >300 mg/dl. Target blood glucose values were defined as between 80 and 200 mg/dl.
The Glucose Monitoring System
The IGMS consisted of a point-of-care, automated gluco-meter and an interactive database. The automated glucometer (Accu-Chek Inform, Roche Diagnostics, Indianapolis, IN) was located in each inpatient department. The hand-held device is powered by a rechargeable lithium battery, and its base unit can be mounted on a wall or desktop. Measuring 3.6 × 9.6 × 19.4 cm, the device has a curved target area for blood application and blood is pulled to the test strip via capillary action; however, blood does not actually enter the meter, reducing the risk of contamination. Data may be entered using a touch screen and/or bar code scanner. As many as 4000 results may be stored in the memory with up to three, user-defined or free text comments per test. Test results are stored with a test identifier code (meter serial number), patient identification, identification of the clinician performing the test, and date and time stamp. Precision of the Accu-Chek in critically ill hospitalized patients has been reported.11 Data are transmitted and downloaded automatically to the central database of the hospital's biochemistry laboratory. The information system (Roche Cobas IT 1000, Roche Diagnostics) permits authorized personnel to access, monitor, and analyze data, which can be downloaded in spreadsheet format for the assessment of temporal trends and the identification of out-of-range values. The information flow in this system is depicted in Figure 1.
Figure 1.
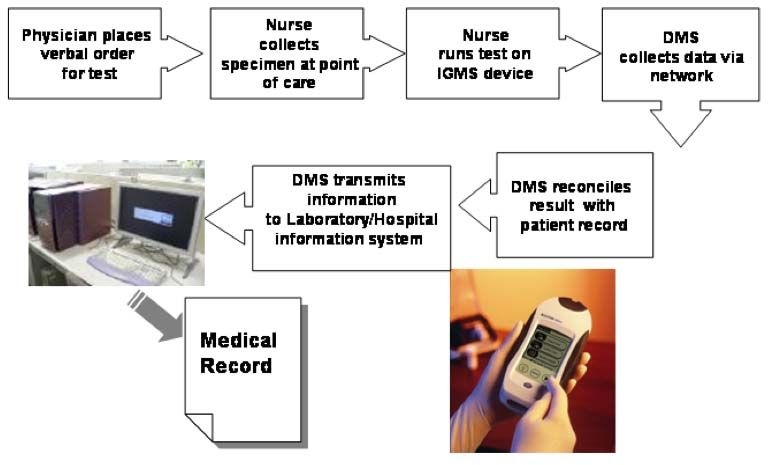
Information flow using the institutional blood glucose monitoring system and data management system (DMS).
Program for the Treatment of the Hospitalized Diabetic Patient
Underlying the PTHDP is the view that hospitalization provides a window of opportunity to improve patient care and to provide patients with the necessary tools to continue/improve self-care following discharge from the hospital. To that end, the PTHDP was established as a hospital-wide care protocol based on the American Diabetes Association Standards of Medical Care in Diabetes 2007.12
Hyperglycemia is treated using a basal, long-acting insulin analog such as glargine or detemir, administered in the morning while bolus doses of such rapid-acting analogs as aspart, lispro, or glulisine are administered at mealtimes. Using this approach, basal insulin is administered initially at a dose of 0.3–0.5 units/kg, which is approximately half the calculated required dose. Additionally, approximately half the calculated rapid-acting insulin dose is administered prior to each of the three daily meals. Titration is tailored according to individual response. Patients who are not eating do not receive boluses of rapid-acting insulin.
In addition to insulin treatment protocols, the PTHDP relies on a multidisciplinary team composed of physicians, dedicated PTHDP nurses, dietitians, social workers, an epidemiologist, and psychologists. This team participates in patient care during hospitalization and arranges for outpatient continuing care following patient discharge. Additionally, team members provide expert consultations to inpatient departments with the goal of providing staffand patient education and instruction. Members also participate in the PTHDP forum, which directs and facilitates the program.
PTHDP dedicated nurses are representatives from each inpatient department and are responsible for diabetes care program implementation. These nurses undergo continuous training and participate in the PTHDP forum, where their input is integral to problem solving.
Also central to the PTHDP is measuring hemoglobin A1cduring hospitalization due to its implications for continuing treatment recommendations during confinement and at discharge. Patient education prior to discharge includes all aspects of patient care and is aimed at facilitating patient empowerment in self-care.
Data Analysis
Data were transferred from the IGMS-generated database and analyzed on SPSS 10.0 (SPSS Inc., Chicago, IL). Normality of distribution was assessed using the Kolmogorov–Smirnov test. Glucose values were found to have a distribution deviating significantly from normal. Continuous variables are described as mean ± standard deviation. Nominal variables are described using frequency counts [n (%)]. Glucose values were compared across months of follow-up using the Kruskal–Wallis test followed post hoc by the Mann–Whitney U test to make pair wise comparisons. This analysis was repeated using one-way analysis of variance (ANOVA) followed post hoc with Bonferroni's test and is thus reported because findings were consistent by method and the reported findings were more intuitive using ANOVA. Associations between nominal variables were assessed using the χ2 test. All tests are two-sided and considered significant at p < 0.05.
Results
Through the period from August 2007 to October 2008, more than 150,000 blood glucose tests were performed using the IGMS. Included in the present 14-month follow-up period are the 5951 IGMS-measured blood glucose tests taken on the 15th of each reporting month, with the exception of January 2008, during which month the system was being restructured, so values are not available.
During the total follow-up period, mean blood glucose values were 195.7 ± 99.12 mg/dl. Figure 2 displays the distribution of blood glucose values measured on the 15th of each month over time. As can be seen, a significant, inverse association between blood glucose and time was detected, indicating a reduction in mean blood glucose levels over time in hospitalized patients, concomitant with the introduction of the PTHDP. Indeed, mean glucose values prior to establishment of the program (August 2007 through December 2007) were significantly higher than those after program initiation (January through October 2008): 206 ± 105 vs 186 ± 92 mg/dl, p < 0.0001.
Figure 2.
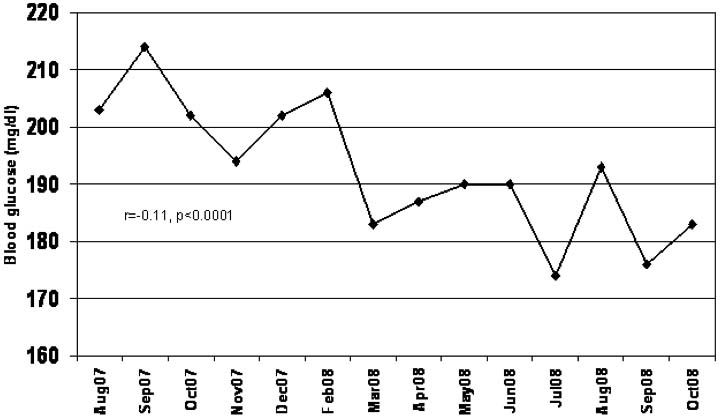
Mean blood glucose for the 15th of each month over time.
Hypoglycemic events were defined as blood glucose values <60 mg/dl. The proportion of hypoglycemic events was 1.4% for the entire follow-up period, ranging from a high of 2.7% in October 2007 to a low of 0% reported in March 2008. Pre- and post-PTHDP implementation values are shown in Figure 3. The mean proportion of hypoglycemic events prior to initiation of the PTHDP was 1.48% [95% confidence interval (CI) 0.36%]. For the period following program initiation, the mean proportion of hypoglycemic events was 1.4% (95% CI 0.36%) if the 0% report in March was included and 1.55% (95% CI 0.37%) if the value for March was excluded. A trend over time was not detected (p = 0.2).
Figure 3.
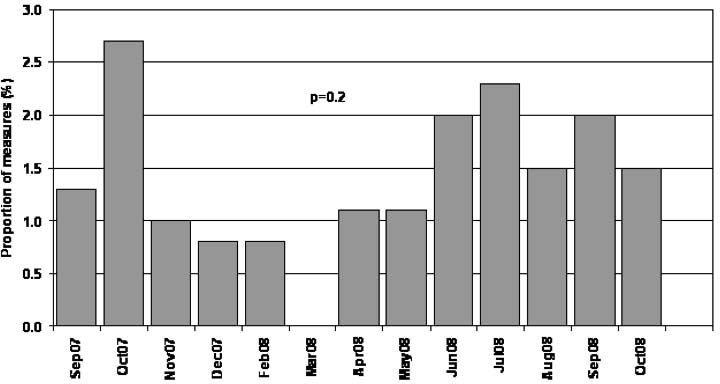
Proportion of glucose measures <60 mg/dl.
Hyperglycemic events were defined as blood glucose values exceeding 300 mg/dl. During the follow-up period, 13.4% of blood glucose levels were in the hyperglycemic range. The proportion of hyperglycemic readings is shown by month in Figure 4. Prior to program commencement, 16.2% of values were >300 mg/dl, compared to 10.2% after initiation, p < 0.0001.
Figure 4.
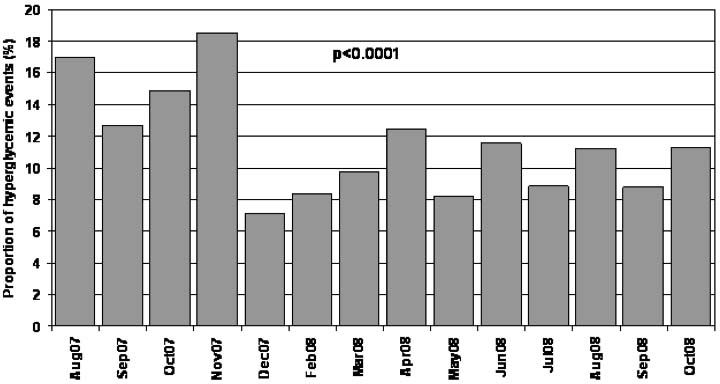
Proportion of glucose measures >300 mg/dl.
“In target” values were defined as those between 80 and 200 mg/dl. The proportion of “in target” values increased from 55.4% prior to program launch to 61.6% after its implementation (p < 0.0001) (Figure 5).
Figure 5.
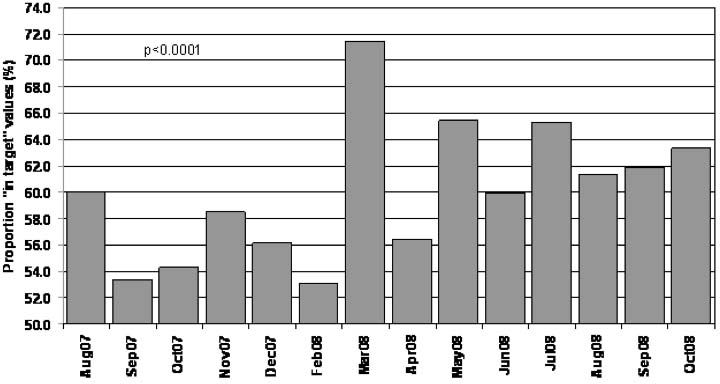
Proportion of “in target” glucose measures: 80–200 mg/dl.
Discussion
This report described the PTHDP, of which IGMS is an integral factor facilitating improved patient follow-up and treatment. Evidence for this improvement can be inferred from the change in inpatient glucose values after program implementation compared to before program implementation. This improvement can be visualized continuously over time. While a significant reduction in hyperglycemic (glucose >300 mg/dl) measures was detected following inauguration of the PTHDP, a concomitant increase in the proportion of hypoglycemic (glucose <60 mg/dl) measures was not observed. Further, a significant postprogram increase in the proportion of “in target” (glucose 80–200 mg/dl) measures was documented.
Hyperglycemia during hospitalization is not a benign condition and clinicians should strive to improve blood glucose control during this time, as urged by current guidelines.12 Systems streamlining the transfer of data from point of care to the patient medical record and to the central laboratory database facilitate efficient and accurate patient follow-up and lead to more informed and rapid treatment decisions.13 The system described in this report, which eliminates the need for transcribing data manually from the glucometer to a paper record and then transferring that record to a laboratory record, reduces the risk for error at each step. Data stored in a central laboratory database facilitate the clinical follow-up of a given patient. Furthermore, this system enables institution-wide, prospective follow-up permitting the identification of temporal trends. Between-department comparisons can also be made, which may identify departmental differences in the implementation of treatment guidelines.
Undoubtedly, other components of the PTHDP contributed meaningfully to the results observed herein. For example, the use of clear protocols has been shown to be associated with greater staff compliance with guidelines and improved patient outcomes.14,15 The use of multidisciplinary care teams has been demonstrated to improve both glycemic control and patient quality of life.16 Safe and effective glycemic control, featuring reduced glycemic variability, has been shown to be associated with reduced mortality in hospitalized patients.17 Insulin therapy using the basal-bolus paradigm has been associated with reduced glycemic variability18; furthermore, the present study did not identify an increase in the incidence of hypoglycemic events concomitant with basal-bolus therapy, consistent with other reports.19
At present, the PTHDP, and the IGMS in particular, has limitations. For example, the follow-up currently does not consider patient diagnosis or concomitant illnesses that may influence blood glucose values. Medication lists are also not presently recorded in the system. Perhaps these data fields can be added in the future, permitting more in-depth analysis of medical and clinical trends. Additionally, the system presently does not identify a given blood glucose sample as fasting or postprandial, which of course restricts the analyses to those using random samples or overall means, but not fasting values, which may reflect diabetes control more precisely.
While the benefit of inpatient glucose control seems intuitive, it is not without controversy. Hyperglycemia is associated with increased morbidity and mortality with and without diabetes20; however, intensive glucose control has been associated with increased mortality in intensive care unit patients,21 and in-hospital blood glucose levels have not been shown to reduce the length of hospital stay.22,23 Perhaps the main concern regarding glycemic control strategies is the increased risk of hypo-glycemic events.10 Hypoglycemia is indeed associated with increased mortality risk, but it has been reported that this risk increase is limited to patients who develop hypoglycemia spontaneously and is not applicable to hypoglycemia following insulin therapy.24 In the present study, improved glucose control was achieved without a concomitant increase in hypoglycemic events.
In summary, the program, relying on the IGMS, has been shown to be beneficial in terms of reducing blood glucose levels in the hospitalized diabetic patient without an accompanying increase in hypoglycemic events.
Abbreviations
- ANOVA
analysis of variance
- CI
confidence interval
- IGMS
institutional blood glucose monitoring system
- PTHDP
Program for the Treatment of the Hospitalized Diabetic Patient
References
- 1.Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB. American Diabetes Association Diabetes in Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27(2):553–591. doi: 10.2337/diacare.27.2.553. [DOI] [PubMed] [Google Scholar]
- 2.Garber AJ, Moghissi ES, Bransome ED, Jr, Clark NG, Clement S, Cobin RH, Furnary AP, Hirsch IB, Levy P, Roberts R, Van den Berghe G, Zamudio V. American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. Endocr Pract. 2004;10(Suppl 2):4–9. doi: 10.4158/EP.10.S2.4. [DOI] [PubMed] [Google Scholar]
- 3.Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978–982. doi: 10.1210/jcem.87.3.8341. [DOI] [PubMed] [Google Scholar]
- 4.Malmberg K, Rydén L, Wedel H, Birkeland K, Bootsma A, Dickstein K, Efendic S, Fisher M, Hamsten A, Herlitz J, Hildebrandt P, MacLeod K, Laakso M, Torp-Pedersen C. Waldenström A; DIGAMI 2 Investigators. Intense metabolic control by means of insulin in patients with diabetes mellitus and acute myocardial infarction (DIGAMI 2): effects on mortality and morbidity. Eur Heart J. 2005;26(7):650–661. doi: 10.1093/eurheartj/ehi199. [DOI] [PubMed] [Google Scholar]
- 5.Van den Berghe G, Mesotten D, Vanhorebeek I. Intensive insulin therapy in the intensive care unit. cmAJ. 2009;180(8):799–800. doi: 10.1503/cmaj.090500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furnary AP, Braithwaite SS. Effects of outcome on in-hospital transition from intravenous insulin infusion to subcutaneous therapy. Am J Cardiol. 2006;98(4):557–564. doi: 10.1016/j.amjcard.2006.02.065. [DOI] [PubMed] [Google Scholar]
- 7.Wexler DJ, Nathan DM, Grant RW, Regan S, Van Leuvan AL, Cagliero E. Prevalence of elevated hemoglobin A1c among patients admitted to the hospital without a diagnosis of diabetes. J Clin Endocrinol Metab. 2008;93(11):4238–4244. doi: 10.1210/jc.2008-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook CB, Moghissi E, Joshi R, Kongable GL, Abad VJ. Inpatient point-of-care bedside glucose testing: preliminary data on use of connectivity informatics to measure hospital glycemic control. Diabetes Technol Ther. 2007;9(6):493–500. doi: 10.1089/dia.2007.0232. [DOI] [PubMed] [Google Scholar]
- 9.American College of Endocrinology and American Diabetes Association Consensus statement on inpatient diabetes and glycemic control. ACE/ADA Task Force on Inpatient Diabetes. Diabetes Care. 2006;29(8):1955–1962. doi: 10.2337/dc06-9913. [DOI] [PubMed] [Google Scholar]
- 10.Giangola J, Olohan K, Longo J, Goldstein JM, Gross PA. Barriers to hyperglycemia control in hospitalized patients: a descriptive epidemiologic study. Endocr Pract. 2008;14(7):813–819. doi: 10.4158/EP.14.7.813. [DOI] [PubMed] [Google Scholar]
- 11.Ghys T, Goedhuys W, Spincemaille K, Gorus F, Gerlo E. Plasma-equivalent glucose at the point-of-care: evaluation of Roche Accu-Chek Inform and Abbott Precision PCx glucose meters. Clin Chim Acta. 2007;386(1–2):63–68. doi: 10.1016/j.cca.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 12.Standards of medical care in diabetes-2007. Diabetes Care. 2007;30(Suppl 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- 13.Shekelle PG, Morton SC, Keeler EB. Costs and benefits of health information technology. Evid Rep Technol Assess (Full Rep) 2006;132:1–71. doi: 10.23970/ahrqepcerta132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munk MD, White SD, Perry ML, Platt TE, Hardan MS, Stoy WA. Physician medical direction and clinical performance at an established emergency medical services system. Prehosp Emerg Care. 2009;13(2):185–192. doi: 10.1080/10903120802706120. [DOI] [PubMed] [Google Scholar]
- 15.O'Connor C, Adhikari NK, DeCaire K, Friedrich JO. Medical admission order sets to improve deep vein thrombosis prophylaxis rates and other outcomes. J Hosp Med. 2009;4(2):81–89. doi: 10.1002/jhm.399. [DOI] [PubMed] [Google Scholar]
- 16.Codispoti C, Douglas MR, McCallister T, Zuniga A. The use of a multidisciplinary team care approach to improve glycemic control and quality of life by the prevention of complications among diabetic patients. J Okla State Med Assoc. 2004;97(5):201–204. [PubMed] [Google Scholar]
- 17.Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 2008;36(11):3008–3013. doi: 10.1097/CCM.0b013e31818b38d2. [DOI] [PubMed] [Google Scholar]
- 18.Guerci B, Sauvanet JP. Subcutaneous insulin: pharmacokinetic variability and glycemic variability. Diabetes Metab. 2005;31(4 Pt 2):4S7–4S24. doi: 10.1016/s1262-3636(05)88263-1. [DOI] [PubMed] [Google Scholar]
- 19.Murphy DM, Vercruysse RA, Bertucci TM, Wall MJ, Schriever AE, Nabhan FA, Barron WM, Emanuele MA. Reducing hyperglycemia hospitalwide: the basal-bolus concept. Jt Comm J Qual Patient Saf. 2009;35(4):216–223. doi: 10.1016/s1553-7250(09)35029-1. [DOI] [PubMed] [Google Scholar]
- 20.Juneja R. Hyperglycemia management in the hospital: about glucose targets and process improvements. Postgrad Med. 2008;120(4):38–50. doi: 10.3810/pgm.2008.11.1937. [DOI] [PubMed] [Google Scholar]
- 21.NICE-SUGAR Study Investigators. Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hébert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 22.Reyes M, Jensen L, Stewart J, Kidd WT. Glycemic control in diabetic and non-diabetic cardiac surgical patients and length of hospital stay. Dynamics. 2008;19(4):18–24. [PubMed] [Google Scholar]
- 23.Eastman DK, Bottenberg MM, Hegge KA, Ourth H, Kabadi U. Intensive insulin therapy in critical care settings. Curr Clin Pharmacol. 2009;4(1):71–77. doi: 10.2174/157488409787236100. [DOI] [PubMed] [Google Scholar]
- 24.Kosiborod M, Inzucchi SE, Spertus JA, Wang Y, Masoudi FA, Havranek EP, Krumholz HM. Elevated admission glucose and mortality in elderly patients hospitalized with heart failure. Circulation. 2009;119(14):1899–1907. doi: 10.1161/CIRCULATIONAHA.108.821843. [DOI] [PubMed] [Google Scholar]


