Abstract
Background
There is a need for improved methods for display and analysis of self-monitoring of blood glucose (SMBG) data to facilitate identification of clinical problems, assist the clinician in the interpretation of daily patterns and longitudinal trends, serve as a guide to locating the most important segments of logbook data, and permit rapid analysis of the patient's pattern of glucose monitoring.
Methods
We developed prototype software to display SMBG data in a two-dimensional color-coded array: Time of day is displayed on the horizontal axis; date or sequential day is displayed on the vertical axis. Each glucose value is shown by a color-coded symbol categorizing it as “very high,” “high,” “within target range,” “low,” or “very low.” The number of categories and their ranges can be defined by the user, and different target ranges and limits for the categories can be used for different times of day. Placing the cursor over any observation activates a “pop-up box” showing the date, day of week, time of day, glucose value, and ancillary information. Several options and variations are available.
Results
This new type of display is compact, serves as a guide to assist the physician in locating the most important segments of the logbook, and permits display of glucose data from 90 or more days in a chart as small as 4 by 4 inches. This analysis permits rapid identification of measurements that are above or below the target range and facilitates rapid evaluation of patterns observed on different days or days of the week.
Conclusion
These new approaches complement other popular graphical displays by conveying information efficiently and effectively to the physician, other health care providers, the patient, and family caregivers in a new and novel, concise, standardized yet flexible format.
Keywords: circadian patterns, computer analysis, day of week, diabetes mellitus, longitudinal analysis, self-monitoring of blood glucose, graphical display, time of day
Introduction
Self-monitoring of blood glucose (SMBG) is one of thekeys to effective management of most patients with diabetes.1–3 These data are used for immediate action (e.g., response to hypoglycemia, adjustment of insulin dosage, control of timing or amount of food intake), for retrospective review to permit identification of patterns and problems, and as a basis for making adjustments in therapy. Many patients monitor their glucose values four or more times per day. Intervals between follow-up ambulatory care visits are typically 3 months apart, with a wide degree of variation. Thus, it is not unusual for a patient to present to the physician's office with a record of 90 days or more, involving perhaps 360 or more glucose values, and a mass of ancillary data (e.g., diet, exercise, insulin, and oral medications). In a typical office visit that may have a total duration of 10 to 15 minutes, the physician will usually have only a few minutes to review, digest, clarify, analyze, and make decisions based on the SBMG data. Some physicians prefer a tabular display of data as provided by the patient's logbook or as generated by a computer program after downloading of glucose data from a memory-equipped glucose meter. Other health care providers may prefer using the following various types of graphs currently in standard usage.
Longitudinal display of glucose values, for all times of day combined and for selected times of day in relation to meals.4,5
Display of glucose values by time of day, consolidating data from a selected range of dates (e.g., the most recent 2 weeks). This has been termed the “glucose profile,”5 the “ambulatory glucose profile,”5–7 “standard day,” and “modal day.” Such displays can be accompanied by a smoothed curve, using a variety of methods for curve smoothing, to help the user identify patterns that might otherwise be obscured by random variation.5–7 For example, the smoothed median (50th percentile) and 25 and 75th percentiles can be shown. The inter-quartile range, i.e., the difference between 75 and 25th percentiles, provides a reliable, robust measure of variability.
Display of glucose values by time of day, categorized in relationship to meals. Glucose values can usually be classified or categorized in relationship to meals, e.g., before and after breakfast, before and after lunch, before and after dinner, bedtime, and overnight (e.g., 3 to 4 a.m.).4,5
Display of glucose values by day of the week. This may be accompanied by the median, 25th and 75th percentiles, range and number of observations for each day of the week, or a “glucose profile by time of day” (as in item C), constructed separately for data from each day of the week.
Pie charts showing the percentage of observations in the three ranges (percentage in target range, percentage high, and percentage low). These charts can summarize data for all times of day or for individual segments of the 24-hour day (e.g., 7:00 to 9:00 a.m. or “before breakfast”).4,5
The most practical way that data of this nature can be presented to the physician, for review within the available few minutes at the time of an office visit, is for these data to have been downloaded and charts, graphs, and other reports generated previously. The reports can be made available to the physician by placing them on the patient's medical record or chart prior to the onset of the patient encounter.8–13
Computer analysis of SMBG data can provide an analysis of the major problems.5,11–14 We have previously developed algorithms and programs to identify (1) overall level of control; (2) problems with hypoglycemia; (3) problems with hyperglycemia; (4) patterns, e.g., postprandial excursions, circadian fluctuations, including dawn phenomenon andpatterns according to day of the week; and (5) variability.5,9,11 The software can make recommendations regarding possible changes in the therapeutic regimen for the patient. 9–14
There is a need for a simple, standardized method to display all data in a “snapshot” that can immediately be viewed, used, and interpreted, while facilitating access to more detail, if desired. This report describes one such approach together with a number of optional features and variations.
Methods
We describe an algorithm for display of SMBG data. We have developed a prototype computational method using Microsoft Excel to demonstrate feasibility and generate displays to permit exploration of multiple options and optimization of usability, “intuitiveness,” and utility and acceptance by the intended audiences. Glucose data are stored in a file or database with the date, time, glucose value, an optional assignment to a category of “time of day” (e.g., “before lunch”), and any comments as entered by the patient into the logbook (or electronic logbook). The “target range” may be the same for all times of day or can be adjusted according to time of day or even day of the week. The user has the option to select the range of dates for analysis using an icon to open a pop-up calendar or by entering two of the following: initial date, final date, and number of days. The size of the symbols can be adjusted automatically depending on the number of days of data analyzed to reduce the likelihood that two data points will be superimposed.
Glucose values are transformed from the continuous measurement scale into clinically important categories, e.g., “very high,” “high,” within the “target range,” “low,” and “very low.” The user is provided with the ability to change the color coding and symbols for each of the categories of blood glucose. Alternatively, glucose levels can be represented by a continuous spectrum of colors. The background color of the plot area can be specified by the user: We generally use a black background to provide maximal contrast and enable one to visualize light colors (e.g., yellow) that are not easily seen against a white or gray background. Other options can be made available for individuals with impaired color vision and for use with black and white (B&W) printers.
When data are available from only a small number of days, e.g., less than 14, then it is possible to display glucose values versus time of day with vertical modulation according to the glucose value. The position on the vertical axis is given by
| (1) |
where c is a constant. Typically, c can be set equal to the maximal value of the measurement range (e.g., 600 mg/dl). This ensures that data from any one day will be displayed in a narrow vertical strip and not overlap data from previous or subsequent days. The user is provided with an option to adjust the extent of vertical modulation by adjusting the scaling factor (c). When viewing data from more than 14 days, it becomes progressively more difficult to visualize vertical modulation: instead, one can simply show all data from any specified day on the same horizontal line. The user may wish to focus on particular subsets or ranges of glucose values, e.g., “very low” and “low” values for an analysis of hypoglycemia. Accordingly, the viewer is provided with the ability to specify which of the several categories will be displayed, e.g., to “drill down” on values that are out of the target range. The user interface can include a series of check boxes for the user to select the ranges he/she wishes to display. Alternatively, the user can select from a cyclical series of previously selected options, e.g., all data, very low, all low values (very low and low), target range, very high, all high values (very high and high), and finally return to all data. The nature of the categories and the order of display in this cycle can be specified by the end user.
Another option would permit the user to select a subset of data by day of the week. For example, one might have the option to look at “all days of the week,” “work/school days (M–F),” weekends, or any arbitrary combination of days of the week and then return to “all days of the week.” In this manner, one can examine glycemic control and extent of monitoring on workdays, weekends, and then each of the days of the week individually or in various combinations.
The program can highlight selected values in a variety of ways, e.g., by making the symbol larger, allowing it to “blink” or flash, surrounding it with a circle or halo, or identifying it with an arrow.
When the user places the cursor directly over an observation, alphanumeric data appear in a small text box, showing date, time, day of week, relationship to meals, and ancillary data, including user-entered comments. It is desirable to provide the user the ability to zoom in on a selected region of the graph.
Table 1 provides a number of options, which are discussed each in turn.
-
Choice of Date Range for Analysis
It is essential for the user to have the ability to select the range of dates for analysis. This can be done by allowing the user to enter the starting and ending dates or one of these together with the number of days to be analyzed. Alternatively, one can use a calendar icon to select the dates from a pop-up calendar.
-
Choice of Color-Coding Schemes and Symbols for Various Ranges of Blood Glucose
Table 2 shows one example of the various plotting symbols and color schemes that may be used. Our goal is to make it as easy as possible for the end user to unambiguously identify any particular range of interest, employing multiple cues (symbol and color). It is important that these cues be used in a consistent manner.
-
Choice of Target Ranges
If the target range values vary according to time of day, then the definitions of the categories can be defined in terms of the distance above or below the upper or lower limits for the appropriate time of day (compare column 3 of Table 2). For example, the “low” range might be defined as 1 to 20 mg/dl below the lower limit of the target range for any specified time of day. This would allow the user to select a different target range, e.g., for the overnight period, if there was particular concern about problems with nocturnal hypoglycemia. Similarly, “very high” might be defined as glucose values that were at a specified level above the upper limit of the target range (e.g., gt;40 mg/dl above the upper limit). If desired, one can use additional categories for glucose levels, e.g., “borderline low”, “borderline high”, “very, very low”, “very, very high”.
-
“Vertical Modulation” of Glucose Values
This feature may be helpful to those individuals accustomed to conventional “x–y” plots or scattergrams of glucose versus date or glucose versus time of day.
-
Format and Labels for Axes
Several options are available for this feature. (a) The “longitudinal time” axis may be shown in terms of date, sequential day, or both (e.g., using both left and rightvertical axes). If only the sequential day number is utilized, one must indicate the starting and ending date for data being displayed. (b) The display can be in chronological order or reverse chronological order, i.e., the starting date may be shown at either the top or bottom of the date axis, depending on the preference of the user, and correspond to a chronological or reverse chronological order for display of data in the logbook. (c) If desired, one can reverse the position of the variables shown on the ordinate and abscissa, e.g., time of day could be shown on the vertical axis and sequential day or longitudinal date can be shown on the horizontal axis.
-
Analysis of Subsets of Data
It is important to have the ability to analyze subsets of data, e.g., data for any specified day of the week.
-
Units
It is essential to be able to select the units for display of blood glucose (mg/dl or mmol/liter).
-
Data Format
It is essential to be able to select the format for dates (MM/DD/YYYY or DD/MM/YYYY).
-
Background Color
Choice of the color for the plot area may affect the other choices of the colors and symbols representing the individual glucose values.
Table 1.
Selected Options for Display of Blood Glucose and Date
| 1. Choice of date range for analysis |
| 2. Choice of color-coding schemes and symbols for various ranges of blood glucose |
| 3. Choice of target range or ranges |
| 4. Use of vertical modulation for glucose data |
5. Format and labels for axes
|
| 6. Ability to analyze subsets of data, e.g., separate analyses for data from different days of the week |
| 7. Choice of units for blood glucose |
| 8. Choice of format for dates |
| 9. Choice of color or “fill” for plot area |
Table 2.
An Example of One Arbitrary Set of Parameters for Ranges of Blood Glucose and Choice of Plotting Symbols and Colorsa
| (1) | (2) | (3) | (4) | (5) |
|---|---|---|---|---|
| Glucose category | Range of blood glucose (mg/dl) | Blood glucose relative to target rangeb | Color and symbol | Size |
| Very high | >180 | Elevated gt; 40 mg/dl | Red square with super-imposed white “plus” signc | Large (6 point) |
| High | 141–180 | Elevated 1–40 mg/dl | Orange square with white “x” | Medium (3 point) |
| Target range | 80–140 | Within range | Green circle | Small (5 point) |
| Low | 60–79 | Low, by 1 to 20 mg/dl | Turquoise triangle | Medium (6 point) |
| Very low | < 60 | Low, by gt;20 mg/dl | Blue diamond | Large (7 point) |
Parameters will often require customization.
This column is particularly useful if the target range varies by time of day.
For increased emphasis and clarity, one can use a symbol with a superimposed “plus” (+) sign for very high values or a superimposed “minus” (−) sign for very low values.
It is desirable to permit the use of different settings for each patient and to permit the settings for a given patient to change with time. Further, it is desirable to provide the clinician with the ability to store metadata to document the rationale used for selection of these settings, e.g., “Focus on normalizing postprandial excursions after dinners on weekends.”
Results
Some selected examples of graphical displays created according to these principles are provided in the series of graphs shown in Figures 1 and 2.
Figures 1A and 1B.
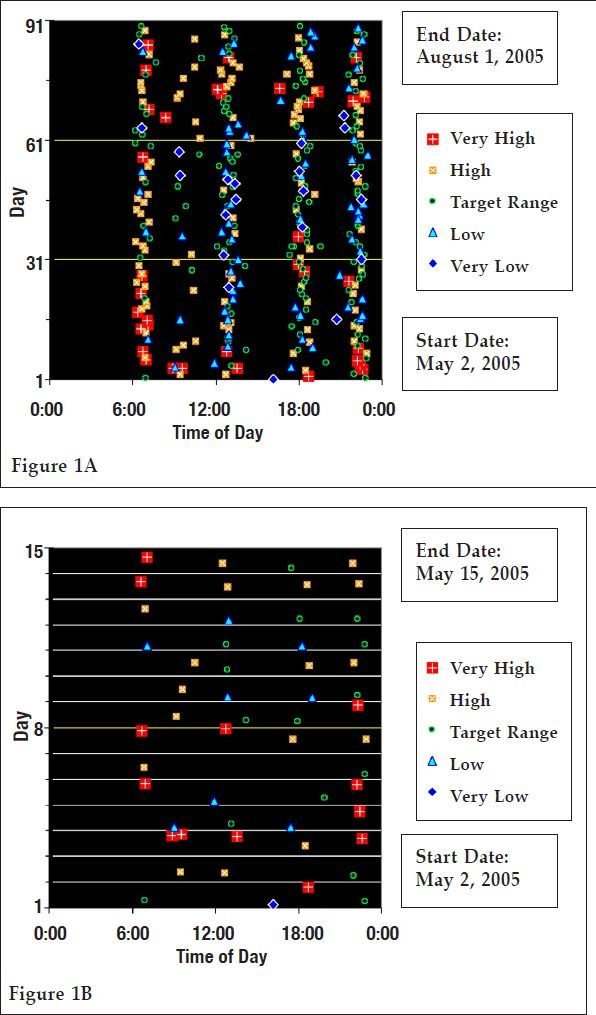
Display of SMBG glucose values by time of day and date (sequential days). (A) SMBG data from 91 days between two consecutive office visits. (B) SMBG data from 14 days showing vertical modulation as in conventional x–y plot. Horizontal axis: time of day using a 24-hour (military) time scale from 00:00 to 24:00. Vertical axis: sequential day. Each symbol represents a blood glucose value on a specified day and specified time of day. Symbols and colors as defined in Table 2. Large blue diamonds: glucose below 60 mg/dl; turquoise triangles: glucose 60–79 mg/dl; green circles: glucose 80–140 mg/dl; orange squares with superimposed white “x”: glucose 141–180 mg/dl; larger red squares with superimposed white “+”: glucose gt;180 mg/dl. This kind of display enables the user to evaluate data in terms of the following criteria, among others: frequency of glucose testing by time of day and date; distribution of glucose values by time of day and date; identification of values significantly outside the target range; longitudinal trends for any specified time of day; and any significant interactions of time of day and date. Placing the cursor over a data point activates a pop-up box showing underlying data (date, time of day, glucose, medications, diet, exercise, illness, comments).
Figure 2.
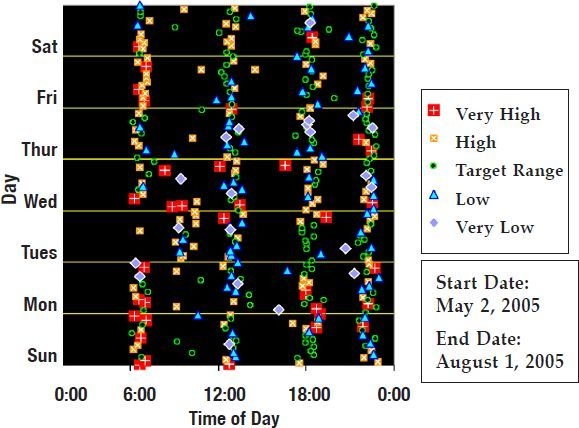
Display of SMBG glucose values (data as in Figure 1A) by time of day, date (sequential days), and day of the week. Data for each of the days of the week were analyzed separately and then arrayed vertically.
Figure 1A shows a display of simulated blood glucose data from a patient using SMBG for 90 days. This demonstrates the feasibility of displaying data for the entire time interval between two office visits, if desired. This graph enables one to quickly evaluate (1) the frequency and patterns of SMBG monitoring throughout the day and longitudinally; (2), by inference, the approximate timing of meals and the extent of variation in meal times; (3) the distribution of values among the five ranges; (4), by means of “mouse over,” the exact date, time of day, and numerical value of the glucose measurement and ancillary data of special interest.
Figure 1B shows data for a selected range of dates for the 14 days (e.g., immediately preceding an office visit) to permit the care provider and patient to focus on the recent history and identify current or recent problems. Here, a small degree of vertical modulation is utilized based on equation (1), using c = 400 mg/dl.
Use of a different background color (for “plot area”) can dramatically change the appearance of these graphs. By virtue of the use of different symbols for the five categories for glucose values, the graphs can also be displayed effectively using a black-and-white video display or printer, typically using white as the background color (data not shown).
Similar presentations can be constructed for each of the days of the week separately to identify any changes in patterns associated with certain lifestyle factors (work, school, etc.). These can be displayed by “vertical stacking” of data for each day of the week, e.g., all Mondays, followed by all Tuesdays, and so on, above one another (Figure 2). Alternatively, some users may prefer a graph with the horizontal axis combining information regarding day of the week and time of day (within each day) on one continuous axis, e.g., corresponding to the 168 hours between the start of the week and the start of the subsequent week (data not shown).
Discussion
The new “family” of methods described and illustrated here (Figures 1 and 2) has several advantages relative to other methods that have been used previously. It provides information in a very compact format and can be customized by the user with regard to a large number of options (e.g., Tables 1 and 2). The method can show data from a few days or from more than 3 months. Analyses can be provided by time of day and day of week.
Interpretation of this new “family” of methods can be learned easily and quickly by health care professionals. Additional information can be provided by “mouse overs” and by display of one or several conventional graphical methods [e.g., glucose by date, glucose by time of day (“glucose profile”), or glucose by day of the week, among others].
It is desirable to enable the user to select any subset of data (by date and by time of day), e.g., by using the cursor to select (encircle) a series of SMBG values, and to be able to generate descriptive statistics for that subset of data. The layout of the new graphical display has an important and deliberate resemblance to a conventional logbook. Accordingly, the present type of display can be regarded as a “guide to” (or “map of”) the logbook. It enables the user to identify features or patterns of special interest (e.g., a cluster of hypoglycemic values, either by date or by time of day). One can then obtain the numerical values, either by placing the cursor on one “point” after another manually or by selecting a “region” (in terms of date and time of day) and then viewing the corresponding section of the electronic logbook.
By sorting data according to day of the week prior to preparing graphs and displays of this type, one can inspect data for patterns or clusters of events related to various aspects of lifestyle (Figure 2).
The displays (Figures 1 and 2) are new and novel. As the data density increases, data points are likely to begin to overlap and the patterns may become difficult to interpret. One can automatically reduce the size of the plotting symbols to minimize this problem. An extensive formal study of acceptance by the audience of end users would be desirable to evaluate usability, cognition, relevance, and clinical utility; such a study is currently being planned.
Conclusion
This article describes new approaches to display SMBG data that provide a very compact picture of the quality of glycemic control for patients with diabetes. These approaches are versatile and flexible and can be customized to the needs of individual users. One can automate the method to the point where it can be generated by a single mouse click or keystroke, i.e., a “single button” approach. These new approaches to graphical display of SMBG data are expected to complement previously described systematic approaches used to analyze and interpret SMBG data.5–14
Acknowledgments
These data were presented in part at the 67th Scientific Session of the American Diabetes Association in San Francisco, 2008. We appreciate the assistance of Mrs. Kelly Allerton in preparation of this manuscript.
Abbreviations
- SMBG
self-monitoring of blood glucose
References
- 1.Karter AJ, Parker MM, Moffet HH, Spence MM, Chan J, Ettner SL, Selby JV. Longitudinal study of new and prevalent use of self-monitoring of blood glucose. Diabetes Care. 2006 Aug 29;8:1757–1763. doi: 10.2337/dc06-2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blonde L, Karter AJ. Current evidence regarding the value of self-monitored blood glucose testing. Am J Med. 2005 Sep;118(Suppl 9A):20S–26S. doi: 10.1016/j.amjmed.2005.07.053. [DOI] [PubMed] [Google Scholar]
- 3.Saudek CD, Derr RL, Kalyani RR. Assessing glycemia in diabetes using self-monitoring blood glucose and hemoglobin A1c. JAMA. 2006 Apr 12;295(14):1688–1697. doi: 10.1001/jama.295.14.1688. [DOI] [PubMed] [Google Scholar]
- 4.Pernick NL, Rodbard D. Personal computer programs to assist with self-monitoring of blood glucose and self-adjustment of insulin dosage. Diabetes Care. 1986 Jan–Feb;9(1):61–69. doi: 10.2337/diacare.9.1.61. [DOI] [PubMed] [Google Scholar]
- 5.Rodbard D. Potential role of computers in clinical investigation and management of diabetes mellitus. Diabetes Care. 1988 Nov–Dec;11(Suppl 1):54–61. [PubMed] [Google Scholar]
- 6.Mazze RS, Lucido D, Langer O, Hartmann K, Rodbard D. Ambulatory glucose profile: representation of verified self-monitored blood glucose data. Diabetes Care. 1987 Jan–Feb;10(1):111–117. doi: 10.2337/diacare.10.1.111. [DOI] [PubMed] [Google Scholar]
- 7.Mazze RS, Strock E, Wesley D, Borgman S, Bergenstal R, Cuddihy R. Characterizing glucose exposure for individuals with normal glucose tolerance using continuous glucose monitoring and ambulatory glucose profile analysis. Diabetes Technol Ther. 2009 Jun;10(3):149–159. doi: 10.1089/dia.2007.0293. [DOI] [PubMed] [Google Scholar]
- 8.Shultz EK, Bauman A, Hayward M, Rodbard D, Holzman R. Improved diabetic prognosis following telecommunication and graphical processing of diabetic data. Proc Annu Symp Comput Appl Med Care. 1991:53–57. [PMC free article] [PubMed] [Google Scholar]
- 9.Rodbard D, Berger M, Pernick N. Computer, networking, and information systems to facilitate delivery of health care to patients with diabetes. In: Baba S, Kaneko T, editors. Diabetes 1994; Proceedings of the 15th International Diabetes Federation Congress; 1994 Nov 6–11; Kobe, Japan. Amsterdam. Elsevier; 1995. pp. 800–803. [Google Scholar]
- 10.Rodbard D, Vigersky R. Development of algorithms for clinical decision support for primary care providers. Diabetes Technol Ther; Annual Meeting; 2004 Oct 28; Philadelphia, PA. 2005. p. 409. [Google Scholar]
- 11.Rodbard D. Optimizing display, analysis, interpretation and utility of self-monitoring of blood glucose (SMBG) data for management of patients with diabetes. J Diabetes Sci Technol. 2007 Jan;1(1):62–71. doi: 10.1177/193229680700100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirsch IB. Blood glucose monitoring technology: translating data into practice. Endocr Pract. 2004 Jan–Feb;10(1):67–76. doi: 10.4158/EP.10.1.67. [DOI] [PubMed] [Google Scholar]
- 13.Deutsch T, Gergely T, Trunov V. A computer system for interpreting blood glucose data. Comput Methods Programs Biomed. 2004 Oct;76(1):41–51. doi: 10.1016/j.cmpb.2004.02.008. [DOI] [PubMed] [Google Scholar]
- 14.Berger MP, Gelfand RA, Miller PL. Combining statistical, rule-based, and physiologic model-based methods to assist in the management of diabetes mellitus. Comput Biomed Res. 1990 Aug;23(4):346–357. doi: 10.1016/0010-4809(90)90026-9. [DOI] [PubMed] [Google Scholar]


