Abstract
Background
The purpose of this article was to communicate our experience with point-of-care testing (POCT) using Bayer's A1CNow+® device to test glycated hemoglobin (A1C) in the management of diabetes and to share the observations of our quality control efforts.
Methods
Forty-seven patients' POCT samples were compared with laboratory samples to determine the validity of the POCT sample being drawn. Data collected represent a 10-month time period that were drawn on-site with the following distribution: 36 samples were drawn the same day, 7 samples were drawn 1 day later, 3 samples were drawn within 3 days, and 1 sample was drawn 4 days later. Although all samples were collected on-site, some of the samples were sent to other local branches of nationally recognized laboratories for analysis.
Results
The range of A1C results for the POCT group was 5.6 to >13%. The range of A1C results for the laboratorydrawn group was 5 to 12.6%. Twenty-four patients had laboratory results that read lower than the result obtained in the clinic, with an A1C range of 5 to 12.6%, and two patients had laboratory results that read exactly the same as the result obtained in the clinic when using POCT. These two individuals had A1C results of 9.1 and 12.6%. Analysis of data collected determined an r value of 0.918 demonstrating agreement between the POCT samples and the laboratory samples.
Conclusions
POCT with the A1CNow+ is an effective, economical tool for use in a pharmacist-based diabetes clinic that serves a high-risk underserved population. POCT allows the pharmacist the ability to use on-site results to inform patients of their progress, modify their therapy immediately with an immediate face-to-face opportunity to assure understanding, and provide a self-management goal.
Keywords: diabetes, patient-centered care, pharmacist-based care, point-of-care testing, underserved
Background
There are 23.6 million people in the United States, or 8% of the population, who have diabetes. The total prevalence of diabetes increased 13.5% from 2005 to 2007, and 24% of diabetes is undiagnosed, which is down from 30% in 2005 and down from 50% ten years ago.1 A new study by Novo Nordisk estimated the total cost associated with diabetes to be $218 billion in 2008. This is a comprehensive estimate of the financial toll diabetes takes, including both direct and indirect costs of diabetes.2
The increased prevalence of diabetes and the cost associated with it are especially concerning in underserved populations because of the disproportionate incidence of this disease. Diabetes is a complex and chronic disease that requires routine monitoring for disease control to help avoid or delay various complications. Underserved patient populations often experience problems with lack of health insurance, transportation, and problems related to low health literacy. These patients can benefit significantly from immediate education and adjustment of therapy when they are a captive audience during their scheduled medical appointment. The concept of patient-centered care is absolutely vital, and point-of-care testing (POCT) plays an integral part in the success of this health care delivery system approach. The “real-world” reality is that this one encounter may be the only opportunity the health care professional (HCP) has to interact with this patient for weeks or months. The health information that is communicated can help influence future care, stress the benefits of early intervention, and provide the patient an opportunity to avoid unnecessary complications that can result from uncontrolled disease states.
Point-of-care testing is simply defined as diagnostic testing at or near the site of patient care. As the patient is brought into the visit, the POCT is the first thing performed so that it runs in 5 minutes as the nurse is performing the usual functions parallel to the POCT. As a result, the visit time is not increased but instead the workflow is arranged to better utilize the time spent with the patient.3 The alternative to POCT would be laboratory testing. If the patient has the laboratory tests drawn, 1 or more days may pass before the results are available. After reviewing the result within the context of the patient's medical history (which also requires pulling the patient chart or reviewing the electronic medical record), the HCP makes the decision to contact the patient. When the result is mailed, the assumption is made that the patient will be able to read and comprehend the written instructions provided in the mailing. The patient must now take the necessary steps to make an appointment and arrange transportation. The delay from collection of the blood sample in the laboratory to comprehension of the results and medical interventions necessary, if applicable, can be days. Being able to avoid all of these steps with POCT can and does save administrative time that is otherwise spent providing education and adherence counseling immediately. In a recently published study, Rust and colleagues4 described a similar experience highlighting the value of POCT in improving primary care outcomes in an urban community health center serving low-income patients. They observed that by utilizing POCT to eliminate a missed opportunity for face-to-face counseling, they were able to achieve a significant practice-level improvement in diabetic regimen intensification.
Point-of-care testing is not new. It has been used for years in various settings. A historical utilization of various POCT methods would be tests such as urine dip analysis or bedside blood glucose monitors. Over time, POCT has become more advanced and provides an opportunity for intervention within various disease states. The rationale behind POCT has always been to provide accurate test results that are convenient and immediate. POCT has evolved to provide cost efficiency and now offers portable handheld instrumentation and test kits. When the results are available they can be shared immediately with the health care team and, more importantly, the patient. Including the patient at the time the results are obtained is very important, as the patient's interest in participating in their own health care can be assessed and involvement in this process is facilitated. This is a key concept of the chronic care model that can result in improvements in health outcomes.5
Concepts in Health Care Delivery
Over time, various health institutions have adapted to the changing health care climate to better meet the needs of those they serve. Changes in insurance coverage, lack of coverage, poor access to medications, lack of ability to understand instructions given, and uninvolvement in one's own health care are just some of the concerns that facilitated modifications. The Institute of Medicine advocated a partnership between clinicians and patients that is characterized by informed, shared decision making, development of patient knowledge, self-management skills, and preventive behaviors. Adopting this new health care model meant that health clinicians would provide recommendations and make decisions that were influenced by an understanding of patients' needs and environment. This needed to include various factors such as home life, livelihood, family dynamics, personal relationships, cultural influence and background, and many other factors.6
With many chronic diseases, the role as a provider should change from being a source of information to a role where we clarify misunderstandings, expand upon existing knowledge, promote self-confidence in self-management, and provide the knowledge tools to make our patients their own best advocate. A study of the patient-centered approach found that when patients perceived their physician visit to be patient centered (i.e., they felt they understood or had been adequately involved in developing the treatment plan), they experienced better recovery, better emotional health, and dramatically fewer diagnostic tests and referrals 2 months later.7
The benefit of practicing patient-centered care is that a patient's current needs influence the agenda for the visit and the HCP can use this encounter as an opportunity to address other health issues that also warrant attention. When this open form of communication is utilized, patient satisfaction often increases. In addition, regardless of insurance coverage, provider access or availability, or financial restraints that often keep patients away, the mystery and fear of disease begin to be dispelled. As early as 1 year after exposure to a chronic disease self-management program that emphasized greater patient involvement in goal setting and self-management in a “real-world” setting, most patients experienced statistically significant improvements in a variety of health outcomes and had fewer emergency department visits.8
Purpose
The purpose of this article was to communicate our experience with Bayer's A1CNow+® POCT in the management of diabetes and to share the observations of our quality control efforts.
Methods
Data included in this report were obtained from two independent pharmacist-run diabetes clinics located within the largest community health center in southern Arizona. The pharmacists work with the health care team under collaborative practice agreements that allow for pharmacists to order the appropriate laboratory tests to monitor disease control.
The adopted process for the clinic settings is to utilize glycated hemoglobin A1c (A1C) POCT when the patient is due for only that analyte evaluation. If other laboratory tests are due at the same time the A1C is needed (i.e., renal panel, liver function test, lipid profile), the A1C test is simply added to the other laboratory orders and all test results are requested to be performed 1 week prior to the scheduled appointment. This process is encouraged so that when the patient has a face-to-face encounter with the provider, clinical data in the form of laboratory results are made available for the discussion and development of action items. For quality control, the health center implements a process that requires every 10th A1C POCT to be validated against a venous blood sample obtained from the on-site laboratory. Each individual patient result selected for quality controls is examined on an individual basis to determine the difference between the POCT and the laboratory method, in addition to the clinical relevance of that difference. For cost containment, the providers try to coordinate routine laboratory monitoring, mentioned earlier, with this verification process when they are able to do so. The venous samples that were drawn on-site were obtained with the following distribution: 36 samples were drawn the same day, 7 samples were drawn 1 day later, 3 samples were drawn within 3 days, and 1 sample was drawn 4 days later. Although all samples were collected on-site, some of the samples were sent to other local branches of nationally recognized laboratories for analysis.
In the past, some concern was raised regarding the validity of the testing and the potential impact of operator error. To avoid POCT results being falsely reported or influenced by operator error, only two trained medical assistants were responsible for performing all A1C testing. The A1CNow testing kit was used for the entire observation period in this report, but has since been replaced by the A1CNow+, Bayer HealthCare, Diabetes Care. The A1CNow+ is a simple, portable, handheld device that is Clinical Laboratory Improvement Amendments waived, requires no calibration, and needs no refrigeration if it is used within 4 months. Study results with health care professionals showed that the laboratory accuracy of A1CNow+ with finger stick samples was, on average, 99%. This means that, on average, a true 7.0% A1C could read approximately 6.9% A1C. An individual A1CNow+ result may differ by as much as –1.0 to +0.8% A1C from the true result. This represents the 95% confidence limits of a Bland–Altman plot. The A1CNow+ is National Glycohemoglobin Standardization Program certified.9
Results
Based on the aforementioned process, over 200 patients had A1C POCT performed, but a minimum of every 10th test was required to be correlated with a venous blood sample. In some instances the tests were more frequent if, for example, the patient had a laboratory requisition given to them by a provider and also had the test performed during the visit. Information was collected from patients with diagnosed type 1 and type 2 diabetes and spanned a 10-month time period. Of those patients referred to the pharmacists for intensive diabetes management, 47 patients were included in the analysis spanning the dates of 02/16/07 to 12/13/07. Although there are over 1600 patients that are served by the efforts of the pharmacists working under collaborative practice in this organization, the included evaluation may appear somewhat limited. This is due to the fact that only a limited time period was chosen for evaluation and current quality control measures guided the frequency of the verification process used.
Of those tested, 21 patients had laboratory results that read higher than the result obtained in clinic after using the point-of-care method. The range of A1C results for the POCT group was 5.6 to >13%. The range of A1C results for the laboratory-drawn group was 5 to 12.6%. Twenty-four patients had laboratory results that read lower than the result obtained in clinic, with a A1C range of 5 to 12.6%, and two patients had laboratory results that read exactly the same as the result obtained in clinic when using POCT. These two individuals had A1C results of 9.1 and 12.6%. There will usually be differences between multiple A1C test results due to normal variation, time between tests, and differences between methods, as demonstrated by the results in this study. However, the clinical relevance of the differences between methods is the critical element that was examined. These results are summarized in Table 1.
Table 1.
Summary of In-Clinic A1C Results
| In-clinic A1C result (%) | Laboratory-drawn A1C result (%) | Difference | Point of Care |
|---|---|---|---|
| 7.50 | 7.60 | 0.1 | Less |
| 7.10 | 7.70 | 0.6 | Less |
| 7.20 | 8.30 | 1.1 | Less |
| 5.80 | 6.20 | 0.4 | Less |
| 8.30 | 8.60 | 0.3 | Less |
| 8.40 | 8.70 | 0.3 | Less |
| 7.40 | 8.60 | 1.2 | Less |
| 10.50 | 11.50 | 1 | Less |
| 8.40 | 9.00 | 0.6 | Less |
| 7.00 | 7.60 | 0.6 | Less |
| 8.00 | 8.70 | 0.7 | Less |
| 9.30 | 9.40 | 0.1 | Less |
| 6.70 | 7.70 | 1 | Less |
| 7.90 | 8.20 | 0.3 | Less |
| 5.60 | 6.30 | 0.7 | Less |
| 7.20 | 7.50 | 0.3 | Less |
| 7.00 | 7.10 | 0.1 | Less |
| 7.20 | 7.90 | 0.7 | Less |
| 7.00 | 7.70 | 0.7 | Less |
| 6.50 | 7.10 | 0.6 | Less |
| 8.40 | 9.10 | 0.7 | Less |
| 6.60 | 6.50 | 0.1 | More |
| 9.30 | 8.90 | 0.4 | More |
| 5.70 | 5.00 | 0.7 | More |
| 10.10 | 9.60 | 0.5 | More |
| 7.80 | 7.40 | 0.4 | More |
| 10.10 | 9.30 | 0.8 | More |
| 9.20 | 8.70 | 0.5 | More |
| 5.60 | 5.10 | 0.5 | More |
| 6.40 | 6.00 | 0.4 | More |
| 7.30 | 7.20 | 0.1 | More |
| 9.60 | 8.50 | 1.1 | More |
| 6.50 | 5.80 | 0.8 | More |
| 6.80 | 6.40 | 0.4 | More |
| 7.60 | 7.50 | 0.1 | More |
| 7.80 | 7.70 | 0.1 | More |
| 8.30 | 7.90 | 0.4 | More |
| 9.00 | 8.60 | 0.4 | More |
| 9.20 | 8.20 | 1 | More |
| 9.30 | 7.30 | 2 | More |
| 8.90 | 8.40 | 0.5 | More |
| >13.0 | 12.10 | 0.9 | More |
| 11.90 | 11.00 | 0.9 | More |
| 8.30 | 8.20 | 0.1 | More |
| 8 | 7.80 | 0.2 | More |
| 12.60 | 12.60 | 0 | Same |
| 9.10 | 9.10 | 0 | Same |
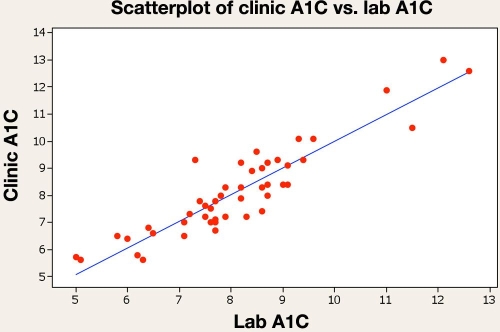
After analysis of data collected, it was determined that the r value for the samples was 0.914, demonstrating an agreement between POCT and laboratory values (Figure 1). The correlation between samples has allowed for POCT and laboratory values to be used interchangeably, resulting in immediate therapeutic decisions and education offered to the patient in the face-to-face intervention for those with POCT results. The usefulness of the immediate outcomes for education and intervention has ultimately improved the control of the patients in the practice, as noted in a study that documented the pharmacist-based treatment approach, resulting in an average decreased A1C from baseline to 90 days of 2%.10 In addition, the cost for our facility to process a serum laboratory A1C on-site is approximately three times the cost of using the laboratory A1CNow+ device.
Figure 1.
Pearson correlation of clinic A1C and laboratory A1C = 0.918. P value = 0.000.
Conclusion
The A1CNow+ is an effective, economical tool for use in a pharmacist-based diabetes clinic that serves a high-risk underserved population. This POCT device allows the pharmacist the ability to use the rapid results to inform patients of their progress, modify their therapy on-site with an immediate face-to-face opportunity to assure understanding, and provide a self-management goal for their next appointment. The involvement of the patient as the team leader who is setting treatment goals established a positive framework for which other HCPs involved could customize the care of the patient. All of these concepts of the chronic care model ultimately supported an informed patient who is more likely to succeed in self-management of their disease.
Acknowledgments
We acknowledge Martha Leyva and Gladys Dimas, the two medical assistants who performed the POCT for the patients and gathered data for analysis. In addition, we acknowledge Jack Lin, the Pharm.D. candidate who assisted with data support. Finally, we would like to thank Jon J. Glover, Pharm.D., for his assistance with data analysis.
Abbreviations
- A1C
glycated hemoglobin
- HCP
health care professional
- POCT
point-of-care testing
References
- 1.American Diabetes Association (ADA) Diabetes statistics. Available from: http://www.diabetes.org/diabetes-statistics.jsp.
- 2.USA Today. Study: cost of diabetes $218B. Available from: http://www.usatoday.com/news/health/2008-11-18-diabetes-cost_N.htm.
- 3.Kost GJ. Guidelines for point-of-care testing. Improving patient outcomes. Am J Clin Pathol. 1995;104(4 Suppl 1):S111–S127. [PubMed] [Google Scholar]
- 4.Rust G, Gailor M, Daniels E, McMillan-Persaud B, Strothers H, Mayberry R. Point-of-care testing to improve glycemic control. Int J Health Care Qual Assur. 2008;21(3):325–335. doi: 10.1108/09526860810868256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, Salivaras S. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Quart. 2003;7(1):73–82. doi: 10.12927/hcq.2003.16763. [DOI] [PubMed] [Google Scholar]
- 6.Educating health professional to be patient centered: current reality, barriers, and related actions, Institute of Medicine. Available from: http://www.iom.edu/Object.File/Master/10/460/0.pdf.
- 7.Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 8.Redelmeier DA, Molin JR, Tibshirani RJ. A randomized trial of compassionate care for the homeless in an emergency department. Lancet. 1995;345(8958):1131–1134. doi: 10.1016/s0140-6736(95)90975-3. [DOI] [PubMed] [Google Scholar]
- 9. Available from: http://www.a1cnow.com/medical-professionals/a1c-now-overview.
- 10.Leal S, Glover JJ, Herrier RN, Felix A. Improving quality of care in diabetes through a comprehensive pharmacist-based disease management program. Diabetes Care. 2004;27(12):2983–2984. doi: 10.2337/diacare.27.12.2983. [DOI] [PubMed] [Google Scholar]