Abstract
Patients with cancer experience a host of behavioral alterations that include depression, fatigue, sleep disturbances and cognitive dysfunction. These behavioral co-morbidities are apparent throughout the process of diagnosis and treatment for cancer and can persist well into the survivorship period. There is a rich literature describing potential consequences of behavioral co-morbidities in patients with cancer including impaired quality of life, reduced treatment adherence and increased disease-related morbidity and mortality. Medical complications of cancer and its treatment such as anemia, thyroid dysfunction, and the neurotoxicity of cancer chemotherapeutic agents account in part for these behavioral changes. Nevertheless, recent advances in the neurosciences and immunology/oncology have revealed novel insights into additional pathophysiologic mechanisms that may significantly contribute to the development of cancer-related behavioral changes. Special attention has been focused on immunologic processes, specifically activation of innate immune inflammatory responses and their regulation by neuroendocrine pathways, which, in turn, impact central nervous system functions including neurotransmitter metabolism, neuropeptide function, sleep-wake cycles, regional brain activity and ultimately behavior. Further understanding of these immunological influences on the brain provides a novel conceptual framework for integrating the wide spectrum of behavioral alterations that occur in cancer patients and may reveal a more focused array of translational targets for therapeutic interventions and future research. Such developments warrant complementary advances in identification of cancer patients at risk as well as those currently suffering, including an increased emphasis on the status of behavior as a “sixth vital sign” to be assessed in all cancer patients throughout their disease encounter.
Introduction
Receiving a diagnosis of cancer and managing the subsequent psychological and physiological assaults presents a formidable challenge. While tremendous advancements have been made in the development of more effective and less traumatic cancer therapies, patients continue to struggle with a myriad of behavioral complications including depression, fatigue, sleep disturbances and cognitive dysfunction. Mounting research has begun to shed increasing light on these behavioral co-morbidities, not only in terms of their prevalence and consequences, but also, most importantly, in terms of potential common underlying mechanisms and related translational implications. Such increasing knowledge will provide a better understanding of treatment strategies and ultimately guidelines for clinical management. Moreover, this knowledge will serve as the basis for implementing more standardized assessments of behavior in the routine care of cancer patients and instantiate behavior as the “sixth vital sign”.
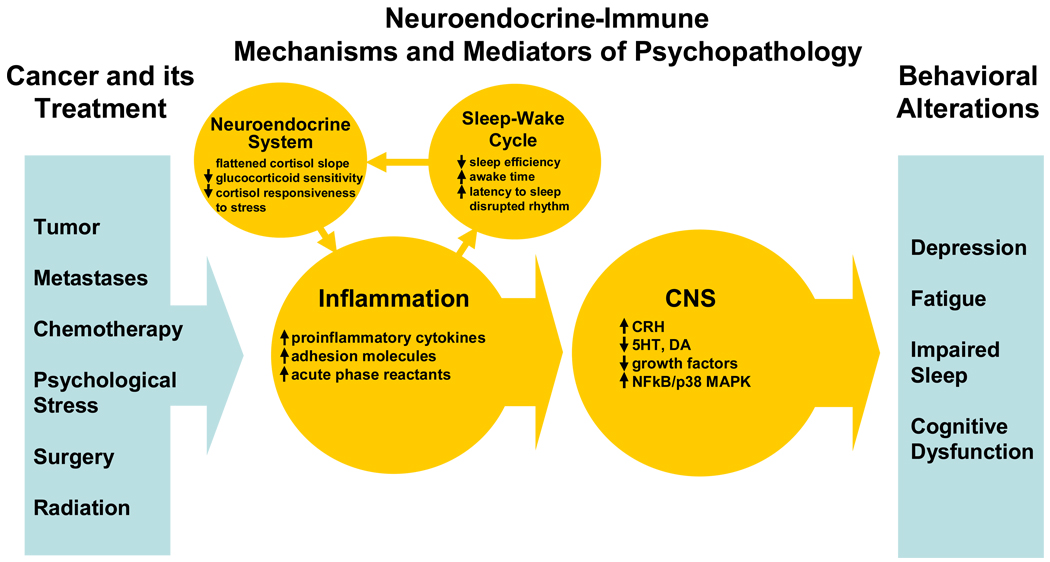
In this review, new research at the interface of immunology/oncology and neurobiology/neuroendocrinology will be described as it relates to the major behavioral challenges faced by cancer patients. More specifically, data will be presented indicating that increased inflammatory responses, in part related to impaired regulation by the neuroendocrine system, interact with pathophysiologic pathways known to be involved in the regulation of behavior and thus may mediate the development of behavioral symptoms in cancer patients. (Figure 1) Of note, this increasing appreciation of the role of inflammation in behavioral pathology is complementary to an increasing awareness of inflammation as a common mechanism in multiple diseases including cardiovascular disease, diabetes and cancer.1 Moreover, this novel conceptual framework may ultimately serve to integrate the spectrum of behavioral co-morbidities experienced by cancer patients and provide an organizing principle for determining which patients are at greatest risk under what treatment conditions. Relevant translational implications of this research as well as directions for future study are also explored.
Figure 1. Neuroendocrine-Immune Mechanisms and Mediators of Behavioral Co-Morbidities in Patients with Cancer.
Various aspects of being diagnosed with and treated for cancer activate inflammation through tissue damage/destruction and/or psychological stress. Cytokines of the innate immune response along with life style changes, pain and other consequences of cancer and its treatment alter the sleep-wake cycle, which in turn contributes to disruption of the neuroendocrine system, in particular, the hypothalamic-pituitary-adrenal (HPA) axis. Given the role of the HPA axis and glucocorticoids in regulating inflammatory responses, altered HPA axis function may disrupt glucocorticoid-mediated negative regulation of inflammation. Unrestrained inflammation and the associated increased release of proinflammatory cytokines, in turn, interacts with central nervous system (CNS) pathways that regulate behavior, leading to pathophysiologic changes that underlie depression, fatigue, impaired sleep and cognitive dysfunction.
Inflammation and Behavior
Increasing data indicates that activation of innate immune responses (inflammation) may contribute to the development of behavioral alterations in both medically ill and medically healthy individuals. Studies in laboratory animals and humans provide compelling evidence that administration of innate immune cytokines can induce a syndrome of “sickness behavior” that has many overlapping features with the behavioral co-morbidities commonly experienced by cancer patients, including depression, fatigue, impaired sleep, and cognitive dysfunction.2,3 These behavioral effects of cytokines appear to be secondary to the capacity of peripheral cytokine signals to access the brain and activate inflammatory responses within the brain, which then interact with pathophysiologic pathways known to be involved in behavioral disorders.4–7 Indeed, cytokine-induced behavioral changes have been associated with alterations in the metabolism of relevant neurotransmitters such as serotonin, norepinephrine and dopamine, all of which play a major role in the regulation of multiple behaviors and are the primary targets for currently available psychopharmacologic treatments of depression and anxiety as well as fatigue.8,9 For example, innate immune cytokines, including interferon (IFN)-alpha and interleukin (IL)-6, have been shown to deplete the amino acid, tryptophan, the primary precursor of serotonin, via induction of the enzyme, indolamine 2,3 dioxygenase (IDO).10–13 In addition, through activation of p38 mitogen activated protein kinase (MAPK) signaling pathways, tumor necrosis factor (TNF)-alpha and IL-1 have been found to increase the function and expression of the synaptic reuptake pumps for serotonin and norepinephrine. Taken together, these data suggest that innate immune cytokines can lead to a “double hit” on the synaptic availability of relevant neurotransmitters,14 influencing both their synthesis and reuptake, and thereby potentially contributing to the development of behavioral changes.8
Innate immune cytokines also have been found to increase mRNA and protein of the neuropeptide, corticotropin releasing hormone (CRH).15,16 CRH is a key regulator of the hypothalamic-pituitary-adrenal (HPA) axis and has been found to be increased in the cerebrospinal fluid of patients with a number of behavioral disorders including major depression.17 In addition, administration of CRH to laboratory animals has been found to lead to alterations in behavior including depressive and anxiety-like behaviors, impaired sleep, anorexia and reduced activity.17
Another mechanism by which innate immune cytokines may contribute to alterations in behavior is through their effects on regional brain activity. These effects have been investigated in the context of administration of IFN-alpha for cancer and infectious diseases. For example, administration of IFN-alpha has been associated with increased regional blood flow in the dorsal part of the anterior cingulate cortex (dACC) as revealed by functional magnetic resonance imaging during a task of visuo-spatial attention.18 The dACC is believed to play an important role in detecting physical and social threat, and subsequently recruiting attention and coping resources to minimize danger.19 Of note, increased dACC activity has been demonstrated in individuals at risk for mood and anxiety disorders, including subjects with high-trait anxiety, neuroticism and obsessive compulsive disorder.18 Studies using [18F]-fluorodeoxyglucose (FDG) and positron emission tomography (PET) have shown that IFN-alpha administration also results in significant changes in prefrontal cortex and basal ganglia activity, which have been correlated with the development of depression and fatigue, respectively.20,21 IFN-alpha-induced alterations in neurocognitive functions relevant to the basal ganglia (i.e. psychomotor slowing) also have been associated with the development of depressive symptoms in cancer patients.22
In addition to effects on the function of brain regions that subserve various cognitive processes and behavior, administration of innate immune cytokines to laboratory animals has been shown to disrupt long-term potentiation in the hippocampus and thereby disrupt memory consolidation.23,24 Moreover, the release of IL-6 from activated macrophages has been shown to mediate the inhibitory effects of cranial x-ray irradiation on the growth and development of neuronal progenitor cells in the hippocampus.25
Finally, ongoing research has revealed an emerging relationship between innate immune cytokines and disrupted sleep-wake cycles (Figure 1).26,27. Sleep loss induces cellular and genomic markers of inflammation28 and leads to increases in circulating levels of innate immune cytokines and markers of systemic inflammation such as C-reactive protein (CRP).29,30 Conversely, elevations of innate immune cytokines such as IL-6, prior to sleep onset correlate with prolonged sleep latency,31–33 and IL-6 administration decreases delta wave sleep.34
Psychological Stress and Inflammation
Given the well-known role of psychological stress in the development of a wide variety of behavioral disorders,35 it is intriguing to note that stress can activate inflammatory cytokines and their signaling pathways [e.g. nuclear factor kappa B (NFkB)] both in the periphery and in the brain.36–39 In addition, data in rats indicate that stress can activate microglia in the brain and increase their sensitivity to immunologic stimuli [i.e. lipopolysaccharide (LPS)].38 Of note, stress-induced IL-1 in the brain has been shown to significantly reduce the expression of brain derived neurotrophic factor (BDNF), which is believed to play a pivotal role in neuronal growth and development, learning, synaptic plasticity and ultimately behavioral disorders.40,41
The effects of stress on brain inflammatory pathways are believed to be mediated by activation of the sympathetic nervous system and the release of catecholamines which bind to alpha and beta adrenergic receptors on relevant cells.36,39 Interestingly, recent data suggest that the parasympathetic nervous system via the release of acetylcholine and subsequent activation of the alpha 7 subunit of the nicotinic acetylcholine receptor can inhibit inflammatory signaling pathways (e.g. NFkB),42 suggesting that sympathetic and parasympathetic pathways have an opposing influence on inflammatory responses during stress.
Neuroendocrine Regulation of Inflammatory Responses
The neuroendocrine system, specifically the hypothalamic pituitary adrenal (HPA) axis and glucocorticoids, plays a primary role in the negative regulation of inflammatory responses. Indeed, glucocorticoids, such as cortisol, are the most potent anti-inflammatory hormones in the body.43 These effects are largely mediated by protein-protein interactions between the glucocorticoid receptor and relevant inflammatory signaling molecules including NF-kB.44 Thus, disruption of glucocorticoid signaling either through altered release of glucocorticoid hormones (including changes in the circadian cortisol rhythm) or disruption of glucocorticoid receptor function may contribute to increased inflammatory responses. Of relevance to the potential role of cytokines in this process, cytokine signaling pathways including p38 MAPK have been shown to disrupt glucocorticoid receptor signaling,45,46 and thereby may contribute to reduced sensitivity of immune cells to the anti-inflammatory effects of glucocorticoids. Disruption of glucocorticoid receptor function may also contribute to altered HPA axis function, including flattening of diurnal cortisol production and the inability to shut down cortisol production (non-suppression) following administration of the synthetic glucocorticoid, dexamethasone [as manifested by an abnormal dexamethasone suppression test (DST)]. Of note, abnormal DST responses have been associated with increased production of IL-1 by peripheral blood mononuclear cells (PBMCs) in healthy subjects with major depression.47 Intense and/or chronic stress has also been associated with alterations in HPA axis function including decreased cortisol production, flattening of the cortisol diurnal rhythm and reduced glucocorticoid receptor function as manifested by altered responses to dexamethasone.48 Taken together, these data suggest that both cytokines and stress can conspire to alter HPA axis and glucocorticoid receptor function, leading to a reduced ability of endogenous glucocorticoids to contain inflammatory responses.
Evidence for the Role of Inflammation and its Altered Regulation by the Neuroendocrine System in Behavioral Co-Morbidities in Patients with Cancer
There are a number of factors that increase the likelihood that cancer patients will exhibit activation of inflammatory pathways (Figure 1). Surgery, chemotherapy and radiation are all associated with significant tissue damage and destruction, which in turn is related to activation of innate immune responses. In addition, chemotherapeutic agents and gamma-irradiation are capable of directly inducing NF-kB and its downstream proinflammatory gene products.1 Moreover, receiving a diagnosis of cancer and battling with chronic uncertainties regarding treatment, recurrence, and mortality is one of the greatest stressors imaginable. Given the impact of stress on inflammatory responses, the confluence of the physical and psychological challenges inherent to having and being treated for cancer place the cancer patient at high risk for the development of inflammation-induced behavioral alterations. The most common of these behavioral changes will be reviewed below in the context of evidence that inflammation and its regulation by the neuroendocrine system may be involved.
Depression
Of all the behavioral co-morbidities that plague cancer patients, major depression, a syndrome characterized by depressed mood and/or anhedonia and accompanied by alterations in appetite, sleep, activity levels, and cognitive function, has been one of the most studied and best-characterized. Major depression in patients with cancer occurs at a high rate with a median point prevalence (15–29%) that is approximately 3–5 times greater than the general population.49,50 Aside from a profound impact on quality of life, major depression in patients with cancer is associated with increased healthcare utilization, poor treatment adherence and in some cases increased rates of cancer recurrence and mortality.49–52
Relevant to the role of the immune system in depression in cancer patients, increased plasma concentrations of IL-6, have been found in two separate studies in cancer patients diagnosed with major depression (Table 1).53,54 Nevertheless, results have been inconsistent, especially in studies looking at correlations between inflammatory biomarkers and depressive symptoms (as measured by standardized depression rating scales). Of note, however, there is a surprising paucity of studies on depressed cancer patients compared to the rich literature examining patients with other medical illnesses, including cardiovascular disease, as well as healthy depressed subjects, where a large number of studies have revealed a clear relationship between inflammatory markers and both a diagnosis of major depression and depressive symptom severity.6
Table 1.
Biomarkers of Inflammation in Cancer Patients with Behavioral Co-Morbidities
| Investigator | Cancer Type | Patient Sample | Immune Parameter | Behavioral Co-Morbidity | Results |
|---|---|---|---|---|---|
| Greenberg et al. 199363 | Prostate | 15 male patients receiving local radiation | IL-1 (serum) | Fatigue | IL-1 levels were increased in parallel with fatigue. |
| Morant et al. 199374 | Mixed | 31 male and female patients with advanced cancer and 30 healthy controls | CRP, TNF, IL-1, IL-2R (serum) | Asthenia | No statistically significant correlation was found between asthenia and immune parameters. |
| Knobel et al. 200071 | Lymphoma | 33 male and female patients 4–10 years post BMT | IL-6, TNF-alpha, sTNFR p55 and p75 (serum) | Fatigue | No statistically significant correlation was found between fatigue and immune parameters. |
| Musselman et al. 200153 | Mixed | 21 male and female patients with pancreatic, breast and esophageal cancer | IL-6 (plasma) | Major Depression | IL-6 was significantly elevated in cancer patients with depression compared to non-depressed patients. |
| Geinitz et. al. 200166 | Breast | 41 female patients with breast-conserving surgery and RT | IL-1 beta, IL-6, TNF-alpha (serum) | Fatigue | No correlation was found between fatigue and immune parameters. |
| Bower et al. 200269 | Breast | 40 female breast cancer survivors | IL-1 beta, IL-1ra, sTNFR p75, neopterin (serum) | Fatigue | IL-1ra, TNFR-p75, and neopterin were significantly higher in fatigued patients. IL-1 beta was not detectable in the majority of patients. |
| Bower et al. 2003150 | Breast | 39 female breast cancer survivors | Peripheral blood lymphocyte phenotypic markers, IL-1ra (serum) | Fatigue | CD3+, CD4+ and CD56+ numbers were significantly higher in fatigued patients, and CD3+ numbers correlated with IL-1ra. |
| Wratten et al. 200464 | Breast | 52 female patients receiving local radiation | IL-6, TNF-alpha, sICAM-1, TGF-beta, PDGF, FGF, CRP (serum) | Fatigue | Fatigue correlated with IL-6, sICAM-1, and CRP at baseline, and with IL-6 at week 5 of RT. No correlation was found between fatigue and immune parameters after controlling for BMI. |
| Dimeo et al. 200472 | Lymphoma, AML, CML ALL, CLL | 71 male and female patients without chemotherapy, radiation of immunotherapy with 3 months | IL-1-alpha, IL-1ra, IL-6, neopterin (serum) | Fatigue | No correlation was found between fatigue and immune parameters. |
| Ahlberg et al., 200467 | Uterine | 15 female patients receiving local radiation | IL-1, IL-6, TNF-alpha (blood, not otherwise specified) | Fatigue | No changes in cytokines were found during RT. No correlations were found between change in fatigue and change in IL-1 and TNF. Change in fatigue negatively correlated with change in IL-6. IL-1 and TNF were not detectable in the majority of patients. |
| Gelinas et al., 2004151 | Breast | 103 female breast cancer survivors | IL-1beta (serum) | Fatigue | No correlation was found between fatigue and IL-1beta. IL-1 concentrations were extremely high (mean = 1,152 pg/ml) |
| Pusztai et al., 200427 | Breast | 90 female patients receiving chemotherapy | IL-1beta, IL-6, TNF-alpha, IL-8, IL-10, IL-12 (plasma) | Fatigue, Depressive symptoms | Baseline cytokine levels were not detectable in the majority of patients. Increases in IL-6, IL-8, and IL-10 were observed in patients receiving paclitaxel chemotherapy. No correlation was found between changes in cytokines and changes in fatigue or depression. |
| Brown et al., 200575 | Lung cancer | 38 patients with advanced cancer | CRP (blood, not otherwise specified) | Fatigue | Fatigue was positively correlated with CRP. |
| Costanzo et al., 200562 | Ovarian | 61 female patients with advanced cancer before surgery | IL-6 (plasma and ascites) | Fatigue, Depressive symptoms | Fatigue was positively correlated with plasma IL-6. No correlation was found between depression and IL-6. |
| Shafqat et al., 200568 | Mixed | 174 male and female patients treated within the last 6 months | TNF-alpha (blood, not otherwise specified) | Fatigue | No correlation was found between fatigue and TNF. |
| Rich et al. 200579 | Colorectal | 80 male and female patients with metastatic disease | TNF-alpha, IL-6, TGF-alpha (serum) | WHO performance, Fatigue | IL-6 and TGF-alpha were increased in patients with WHO performance status >1. TGF-alpha correlated with fatigue. Dampened cortisol rhythm was associated with increased TNF-alpha, IL-6 and TGF-alpha. |
| Meyers et al. 200561 | Leukemia | 54 male and female patients with ALS/MDS | TNF-alpha, IL-1, IL1ra, IL-6, IL-8 (serum) | Neuropsychological Performance, fatigue | Higher IL-6 was associated with poorer executive function. Higher IL-8 was associated with better memory performance. IL-6, IL-1ra, and TNF-alpha were correlated with fatigue. |
| Mills et al. 200565 | Breast | 29 women with Stage I-IIIA disease before and during anthracycline-based chemotherapy | IL-6, sICAM, VEGF (plasma) | Fatigue, Quality of Life | sICAM and VEGF were related to increased fatigue and poorer quality of life. |
| Collado-Hidalgo et al. 200670 | Breast | 50 female breast cancer survivors | Peripheral blood lymphocyte phenotypic markers; IL-6, sIL-6R, IL-1ra, TNFR-p75 (plasma); LPS-stimulated intracellular expression of IL-6 and TNF-alpha | Fatigue | Plasma IL-1ra and sIL-6R and LPS-stimulated IL-6 and TNF-alpha were elevated in patients with fatigue along with decreased monocyte cell-surface IL-6R and decreased activated T lymphocytes and myeloid dendritic cells. |
| Jehn et al. 200654 | Metastatic Cancer | 114 male and female patients with metastatic (Stage 4) disease | IL-6 (plasma) | Major Depression | Plasma IL-6 was significantly elevated in depressed patients. |
| Bower et al.78 | Breast | 25 female breast cancer survivors | Peripheral blood lymphocyte phenotypic markers; LPS-stimulated production of IL-1-beta, IL-6, TNF-alpha after stress | Fatigue | LPS-stimulated IL-1-beta and IL-6 were increased in fatigued patients versus non-fatigued patients following stress. |
ALL-acute lymphocytic leukemia; AML-acute myelogenous leukemia; BMT-bone marrow transplant; CML-chronic myelogenous leukemia; CLL-chronic lymphocytic leukemia; CRP-C-reactive protein; FGF, fibroblast growth factor; IL-interleukin; IL-1ra-interleukin-1 receptor antagonist; IL-2R-interleukin 2 receptor; LPS-lipopolysaccharide; MDS-myelodysplastic syndrome; PDGF-platelet-derived growth factor; RT-radiation therapy; sICAM-soluble intracellular adhesion molecule; sIL-6R-soluble interleukin 6 receptor; TGF-transforming growth factor; TNF-tumor necrosis factor; TNFR-TNF receptor; VEGF-vascular endothelial growth factor
Cancer patients with major depression also have been shown to exhibit neuroendocrine changes that might predispose to activation of inflammatory responses including two studies demonstrating reduced sensitivity to glucocorticoids as manifested by DST nonsuppression53,55 (Table 2) and one study showing a flattening of the diurnal cortisol curve.53 No study to date has linked HPA axis and/or glucocorticoid receptor function and increased inflammatory markers in depressed cancer subjects.
Table 2.
Neuroendocrine Alterations in Cancer Patients with Behavioral Co-Morbidities
| Investigator | Cancer Type | Patient Sample | Neuroendocrine Parameter | Behavioral Co-Morbidity | Results |
|---|---|---|---|---|---|
| Evans et al. 198655 | Mixed | 47 females with cervical, endometrial and vaginal cancer of varying stages | DST | Major Depression | 21% of patients were DST non-suppressors. 40% of patients with major depression were DST non-suppressors. |
| Sephton et al. 200086 | Breast | 104 women with metastatic disease | Diurnal salivary cortisol rhythm | Sleep | Flattened cortisol slope was associated with increased nocturnal awakenings and decreased survival. |
| Musselman et al. 200153 | Mixed | 21 male and female patients with pancreatic, breast and esophageal cancer | DST | Major Depression | Post dexamethasone plasma cortisol concentrations correlated with depression, but not with IL-6. |
| Capuron et al. 200310 | Melanoma | 20 male and female subjects, Stage III–IV | ACTH and cortisol response to IFN-alpha | Major Depression | Exaggerated ACTH and cortisol responses to the first injection of IFN-alpha were associated with the development of depression during IFN-alpha therapy. |
| Bower et al. 200576 | Breast | 29 female breast cancer survivors | Salivary cortisol samples collected upon awakening and at 1200, 1700, and 2200 h on two consecutive days | Fatigue | Flattened cortisol slope was found in patients with fatigue. |
| Bower et al. 2005;77 200778 | Breast | 27 female breast cancer survivors | Salivary cortisol samples collected at 15-minute intervals throughout a stressful public speaking and mental arithmetic task | Fatigue | Salivary cortisol responses to stress were blunted in fatigued patients versus controls. Blunted cortisol responses in fatigued patients were associated with increased LPS-stimulated IL-6 production. |
| Rich et al. 200579 | Colorectal | 80 male and female patients with metastatic disease | Serum cortisol obtained at 800 and 1600 h | WHO performance, Fatigue | Flattened cortisol rhythm was associated with increased TNF-alpha, IL-6 and TGF-alpha. |
| Jehn et al. 200654 | Metastatic Cancer | 114 male and female patients with metastatic (Stage 4) disease | Diurnal cortisol secretion | Major Depression | Decreased variance in diurnal cortisol secretion (i.e. flattened cortisol rhythm) was found in depressed patients compared to controls. |
ACTH-adrenocorticotropin; DST-dexamethasone suppression test; IL-interleukin; h-hour; IFN-interferon; LPS-lipopolysaccharide; TGF-transforming growth factor; TNF-tumor necrosis factor.
Fatigue
Fatigue is one of the most common and distressing side effects of cancer treatment.56 Prevalence estimates of fatigue during treatment range from 25–99% depending on the sample and method of assessment.56,57 Although fatigue typically declines after cancer treatment, there is growing evidence that fatigue may persist for months or years in a significant subpopulation of patients.58,59 Indeed, a recent study found that 34% of disease-free breast cancer survivors reported significant fatigue 5–10 years after diagnosis,60 similar to estimates obtained in a heterogeneous sample of 5-year cancer survivors.59
A number of studies have shown an association between inflammatory markers and fatigue in cancer patients before treatment onset61,62 and during treatment with radiation63,64 and chemotherapy,65 although negative findings have been reported (Table 1).27,66–68 There is also evidence that inflammatory processes play a role in post-treatment fatigue. For example, breast cancer survivors with persistent fatigue were found to exhibit significant elevations in several markers of immune activation [i.e., IL-1 receptor antagonist (IL-1ra), soluble TNF receptor p75, neopterin] compared to non-fatigued survivors.69 These findings were recently replicated in a larger cohort of breast cancer patients, with fatigued survivors again showing elevations in circulating IL-1ra and soluble IL-6 receptor as well as increased production of innate immune cytokines by monocytes following in vitro stimulation with LPS.70 Two studies conducted with patients with hematological malignancies who had completed treatment found no association between fatigue and inflammatory markers.71,72 However, in both of these reports, there was considerable variability in diagnosis, disease stage, length of time since treatment, and duration of fatigue symptomatology. Moreover, a recent meta-analysis of the available literature has supported a relationship between inflammatory biomarkers and fatigue in cancer survivors.73 Among patients with advanced cancer (active disease), there is mixed evidence for an association between fatigue and inflammatory measures.74,75
Evidence suggests that enhanced cytokine production in fatigued cancer survivors may stem in part from altered HPA axis function including altered diurnal cortisol secretion and a decreased cortisol response to stress (Table 2). For example, lower levels of morning serum cortisol,69 flattened diurnal cortisol slopes,76 and a blunted cortisol response to acute psychosocial stress77 have been found in breast cancer survivors with persistent fatigue. Interestingly in a recent study of fatigued breast cancer patients, increased stress-induced inflammatory responses (as manifested by increased IL-6 responses to LPS stimulation of whole blood) were associated with decreased stress-induced salivary cortisol responses.78 Increased inflammatory cytokines have also been associated with dampened cortisol rhythm in patients with metastatic colorectal cancer.79 Taken together, these data suggest that alterations in cortisol secretion over the circadian cycle and in response to stress may play a role in exaggerated inflammatory responses which in turn may be associated with behavioral changes including fatigue.
Sleep Disturbance
Over 50% of cancer patients report problems with sleep, with polysomnographic data confirming reduced sleep efficiency, prolonged latency to fall asleep, and increased awake time during the night.80,81 Even before treatment, patients with cancer have reported significant sleep impairment,82 and among cancer survivors, sleep problems persist well beyond treatment. Indeed, nearly 20% of breast cancer survivors report greater than 6 months of chronic insomnia.80,83 Sleep disturbances come at a considerable price. For example, insomnia is a powerful predictor of cancer-related fatigue,58,84,85 and disturbances in sleep-wake activity as well as circadian rhythms have been found to predict increases in mortality in patients with metastatic disease.86,87
Interestingly, despite data indicating a relationship between innate immune cytokines such as IL-6 and sleep, the relationship between inflammatory markers and sleep in cancer patients has not been examined. Given the strong relationship between fatigue and inflammatory markers, it appears likely that similar relationships may exist with sleep. Clearly, studies are needed in this area.
An important potential mechanism whereby sleep disturbances may contribute to increased inflammation is through desynchronization of circadian rhythms, including the release of cortisol (Figure 1).88 Twenty-four hour circadian cortisol secretion is regulated in the hypothalamus in conjunction with the circadian pacemaker located within the suprachiasmatic nucleus. Forced changes in circadian sleep-wake patterns as well as the induction of sleep debt (as occurs in the context of chronic sleep impairment) have been associated with flattening of cortisol rhythms, especially as manifested by increased cortisol secretory activity in the evening, a normally quiescent period of cortisol release.89,90 In addition, sleep restriction has been associated with reduced ACTH responses to stress in rats.91 Although not adequately studied, there is at least one report in cancer patients that disruption of circadian cycles as manifested by frequent nocturnal awakenings was associated with flattening of circadian cortisol rhythms, which in turn, was associated reduced long term survival.86,87 Disruption of circadian rhythms may be initiated during cancer treatment as a result of a vicious cycle of fatigue and daytime inactivity (with resultant impairment in night-time sleep) and/or the impact of immune activation secondary to cancer treatment and/or psychological stress on sleep-wake cycles. Further studies examining sleep-wake cycles, activation of inflammatory responses and circadian cortisol rhythms are clearly warranted to further clarify these relationships and identify points of therapeutic intervention.
Cognitive Function
Cognitive dysfunction during cancer treatment significantly impacts quality of life and social/occupational function, and represents a major concern in patient management.92 Complaints of cognitive impairment, including alterations in memory, concentration, executive function and psychomotor skills, are frequent in patients with cancer. Aside from cancers that directly affect the central nervous system (CNS), cancers originating in peripheral tissues have also been associated with the occurrence of neuropsychological changes. These cognitive changes are often secondary to cancer treatments, including most notably chemotherapy and radiation. About 25–33% of patients undergoing systemic chemotherapy exhibit impaired performance on tests of cognitive functions.93–96 Cognitive dysfunction related to chemotherapy appears to be dose-dependent; with high-doses being associated with greater impairment.95,97 Although cognitive dysfunction during chemotherapy generally resolves after treatment, several studies have reported residual long-term effects.98–100 Data indicate that chemotherapy is also associated with alterations in regional brain activity that correlate with cognitive dysfunction.101,102 For example, a [18F]-FDG PET study on patients treated with chemotherapy for breast cancer demonstrated significant decreases in metabolic activity in the dorsolateral prefrontal cortex that correlated with cognitive impairment.103 When directed at the brain, not surprisingly, radiation therapy is often accompanied by neurological complications that may be severe and persist years after treatment.104 Interestingly, however, moderate/transient cognitive alterations have been reported after radiation of sites other than the brain. For example, a study conducted in 48 women undergoing postoperative radiation therapy after breast-conserving surgery indicated significant increases in the cognitive fatigue subscale of the Fatigue Assessment Questionnaire 4 and 5 weeks after initiation of radiation therapy in comparison to baseline.66
Findings suggest that inflammatory factors may play a role in the pathophysiology of cognitive dysfunction in cancer patients.23 For example, a significant negative correlation has been found between plasma IL-6 and executive function in patients with acute myelogenous leukemia or myelodysplastic syndrome (Table 1).61 Probably the most striking example of the effects of cytokines on cognition in cancer patients is the neuropsychological sequelae of cytokine-based immunotherapies such as IFN-alpha and IL-2. A study conducted in patients treated with high-dose IFN-alpha for malignant melanoma indicate that complaints of moderate to severe cognitive symptoms are frequent, especially loss of concentration (30% of patients), psychomotor retardation (40%), memory disturbances (15%) and word-finding problems (15%).105 Cognitive dysfunction in patients undergoing cytokine therapy largely depends on the parameters of treatment (dose, duration and route of administration) and the cytokine administered.106 Thus, whereas IFN-alpha therapy is generally associated with reduced psychomotor speed and concentration difficulties, IL-2 therapy is more frequently associated with alterations in working memory and executive function.22 Cognitive alterations secondary to high-dose cytokine therapy treatment typically reverse after treatment; however, residual cognitive impairment has been reported.107,108
Translational Implications
Identification of Behavioral Risk
Based on the proposed conceptual framework (Figure 1), individuals with high levels of perceived stress (as a function of the cancer diagnosis or other life circumstances) who are undergoing treatments associated with activation of inflammatory responses (e.g. surgery, chemotherapy, radiation therapy) may be most at risk for developing behavioral change. In addition, increased risk may be associated with significant disruption of sleep-wake cycles. The relative risk for the development of behavioral co-morbidities is also likely influenced by genetic factors. Functional polymorphisms in the IL-6 gene and the serotonin transporter gene may be especially relevant, given the association of IL-6 with several behavioral pathologies in cancer patients and the demonstrated role of serotonin transporter polymorphisms in the relationship between stress and behavior alterations.109,110 Future studies identifying psychological and genetic profiles of risk for behavioral change during cancer and its treatment are clearly warranted. Finally, as part of ongoing research into the role of inflammation in behavioral co-morbidities and the identification of risk, consideration should be given to the development of standardized assessments of inflammatory biomarkers in cancer patients. Based on studies to date, alterations in IL-6 (as assessed by high sensitivity enzyme-linked immunoabsorbent assay) and the downstream, liver-derived, acute phase reactant, CRP [as measured by high sensitivity (hs) assay techniques], appear to be the most reliable regarding both behavioral pathology and medical illness.6,111–115 Indeed, as shown in Table 1, a number of studies in cancer patients have revealed associations between IL-6 and CRP and depression, fatigue, and cognitive dysfunction. Furthermore, hsCRP can be run in certified commercial/hospital laboratories, thereby reducing variability across research sites. Moreover, in the case of hsCRP, cut-off values have been established that have both predictive validity and categorization of risk in relation to disease outcome in cardiovascular disorders.113 Given the fluctuating status of cancer patients during treatment, it is also suggested that longitudinal assessments of both behavior and relevant inflammatory biomarkers be obtained to increase the likelihood of identifying relevant associations between these variables that might otherwise be confounded by the vicissitudes of the cancer treatment experience. Examination of inflammatory biomarkers in cancer survivors versus healthy age- and sex-matched controls is yet another strategy to reduce the impact of treatment on the relationship between inflammation and behavioral change.
Therapeutic Ramifications
Given the prevailing knowledge regarding the potential integrated mechanisms involved in behavioral co-morbidities in cancer patients, there are multiple opportunities for translational studies targeting pathways that contribute to the wide range of symptoms (Table 3).
Table 3.
Neuroendocrine-Immune Interactions and the Development of Behavioral Co-morbidities in Cancer Patients: Translational Targets
| Immune System |
| Cytokine Antagonists (e.g. TNF-alpha, IL-1, IL-6) |
| Cytokine Signaling Pathway Antagonists (e.g. NFkB inhibitors, p38 MAPK inhibitors) |
| Anti-inflammatory Medications (e.g. COX-2 inhibitors, PGE2 inhibitors) |
| Exercise |
| Neuroendocrine System |
| CRH antagonists |
| Glucocorticoid Receptor Facilitators (e.g. phosphodiesterase Type IV inhibitors) |
| Sleep-Wake Cycle |
| Chronotherapy (e.g. melatonin, light therapy, or sleep regulation) |
| Behavioral Therapy (cognitive behavioral therapy, graded exercise, improved sleep hygiene) |
| Central Nervous System |
| 5HT, NE, DA Reuptake Inhibitors (e.g. antidepressants) |
| DA agonists |
| Neuroprotective Agents (e.g. growth factors) |
| Stress |
| Cognitive-Behavioral Therapy (e.g. Stress Management, Coping Skills, Graded Exercise) |
| Relaxation Training |
| Supportive Psychotherapy |
| Anti-anxiety Medication (e.g. benzodiazepines) |
5HT-serotonin; COX-cyclo-oxygenase; DA-dopamine; IL-interleukin; MAPK-mitogen activated protein kinase; NE-norepinephrine; NFkB-nuclear factor kappa B; PG-prostaglandin; TNF-tumor necrosis factor
Psychotherapeutic/Behavioral interventions
Cognitive-behavioral, supportive or insight-oriented psychotherapies that reduce stress and restore regular circadian cycles may be especially relevant, given the potential role of stress-induced inflammation and altered regulation of inflammatory responses by the neuroendocrine system. Relevant cognitive-behavioral strategies include relaxation training, enhancement of coping skills, graded exercise, and establishment of appropriate sleep-wake habits and social rhythms (e.g. standardized bed and wake-up times, avoidance of daytime napping, and correction of maladaptive beliefs about sleep).116–127 Such interventions may limit the impact of stress on the immune response and may have direct effects on neuroendocrine-immune interactions. Indeed, psychological interventions such as cognitive-behavioral stress management and mindfulness-based stress reduction have been shown to alleviate psychological distress in breast cancer patients, while increasing lymphocyte proliferative responses and normalizing diurnal cortisol secretion.122–127 There is also evidence that aerobic exercise can lead to reductions in inflammatory markers in cancer survivors,128 and the possibility that changes in inflammation may mediate the beneficial effects of exercise (and possibly other behavioral therapies) on cancer-related behavioral co-morbidities is an important avenue for future research.129 Interestingly in this regard, a recent cognitive-behavioral therapy program focusing on coping, sleep, physical activity and social support was found to lead to significant improvement in fatigue in 54% of cancer survivors compared to 4% of patients assigned to a control condition.116 Regarding the impact of altered sleep-wake cycles on neuroendocrine and immune function in cancer patients, Irwin and colleagues found that multiple types of behavioral treatments (e.g., cognitive behavioral therapies, relaxation, behavioral only) induced robust improvements in subjective measures of sleep quality, sleep onset, and sleep maintenance in adults with primary insomnia130 extending the findings of prior studies.131,132 However, much less is known about the efficacy of these approaches for insomnia in cancer patients.83,133 Indeed, only one controlled study has examined the efficacy of a behavioral intervention for insomnia in cancer patients,134 with other studies limited by lack of a control group and/or small sample sizes.135,136 Moreover, no study has included assessments of the impact of these interventions on cortisol rhythms, inflammatory mediators, or behavioral changes.
Biologic Interventions
Although further studies are required to characterize the relationship between inflammatory markers and behavior in cancer patients; cytokine antagonists, anti-inflammatory agents and drugs that disrupt cytokine signaling pathways (e.g. NFkB and p38 MAPK) are logical treatment considerations that target the most upstream elements in the cytokine-to-CNS-to-behavior cascade. Of note, given the role of NF-kB and p38 pathways in cancer development and progression, exciting opportunities exist for behavioral scientists to work with oncologists to examine the full spectrum of activity of relevant antagonists of inflammatory pathways. For example, several recent trials have demonstrated that TNF-alpha blockade with etanercept is safe in patients with advanced cancer, and there was suggestion in at least one study that tolerability of chemotherapy (including reduced fatigue) was improved.137–139
Moving into the CNS, inflammation-induced alterations in neurotransmitter systems may be best addressed by pharmacologic agents that target specific monoamine systems for specific symptom domains (e.g. serotonin active drugs for mood/anxiety symptoms, dopamine active drugs for fatigue and psychomotor slowing). For example, in at least two double-blind placebo-controlled trials in cancer patients undergoing treatment, paroxetine (a serotonin reuptake inhibitor) was found to reduce depression while having limited effect on fatigue.105,140 On the other hand, preliminary evidence suggests that dopaminergic agents such as the psychostimulant, methylphenidate, may treat fatigue and improve neuropsychological functioning in patients undergoing cancer treatments141 and patients with tumor-related organic brain dysfunction.142,143
CRH, which as noted above is stimulated by innate inflammatory cytokines, is another rational CNS target, and although CRH antagonists are not currently available, there is preliminary indication that these agents may have efficacy in treating depression in otherwise healthy individuals.144 Drugs that enhance glucocorticoid-mediated negative feedback on CRH pathways, through facilitation of glucocorticoid receptor function, may control CRH over-expression. Such drugs (including phosphodiesterase type IV inhibitors), may have the advantage of additionally inhibiting inflammatory pathways.145 Novel treatments supporting neuronal integrity/plasticity (neuroprotective agents) including drugs that stimulate the activity or signaling of relevant growth factors (e.g. BDNF) may be especially important for future development.146,147
Regarding sleep and neuroendocrine rhythms, therapies that combine chronobiotics (e.g., melatonin receptor agonists, light therapy, or sleep regulation) might synchronize the circadian rhythms of cancer patients to their environment, in the same manner as these strategies are used to treat transient rhythm disturbances caused by jet lag or shift work. Such treatment may help restore neuroendocrine rhythmicity, reduce inflammation, and potentially improve therapeutic efficacy of cancer treatments.148,149
Summary
The research described herein provides a conceptual framework designed to integrate a host of behavioral co-morbidities which may share common pathophysiologic features that lend themselves to identification of risk and targeted interventions with broad therapeutic relevance. Further studies examining neuroendocrine-immune interactions as they relate to altered sleep-wake cycles and behavioral co-morbidities in patients with a wide variety of cancers will likely lead to novel insights to the contribution of cancer and its treatment to behavioral changes and, possibly, the contributions of behavioral co-morbidities to cancer development, progression and recurrence. Finally, given the increasing understanding of the pathophysiology and treatment of behavioral co-morbidities in cancer patients, it is especially important that standardized behavioral assessments become part of the routine care of cancer patients. As such, instantiating behavior as the sixth vital sign will go a long way to emphasizing the need for further research and the importance of both recognizing and treating the behavioral consequences of cancer and its treatment.
Acknowledgements
The authors would like to thank Dr. Paige McDonald for her valuable input and support regarding this manuscript. This project was funded in part by the National Cancer Institute (NCI), Cancer Control and Population Sciences, Basic and Biobehavioral Research, Biological Mechanisms of Psychosocial Effects in Disease; NCI CA85264, NCI CA112035, and CBCRP 11IB-0034, M01-RR00865 grants to SA-I; NCI CA090407 grant to JEB; National Institute of Mental Health grant MH069124 to AHM; and National Institutes of Health grants AG026364, HL079955, T32-MH19925, CA 0014152 to MRI and the Cousins Center for Psychoneuroimmunology.
Contributor Information
Andrew H. Miller, Emory University School of Medicine, Atlanta, GA
Sonia Ancoli-Israel, University of California San Diego, San Diego, CA
Julienne E. Bower, University of California Los Angeles, Los Angeles, CA
Lucile Capuron, Université Bordeaux, Bordeaux, France
Michael R. Irwin, University of California Los Angeles, Los Angeles, CA
References
- 1.Aggarwal BB, Shishodia S, Sandur SK, et al. Inflammation and cancer: how hot is the link? Biochem Pharmacol. 2006;72:1605–1621. doi: 10.1016/j.bcp.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 2.Dantzer R. Cytokine-induced sickness behavior: where do we stand? Brain Behav Immun. 2001;15:7–24. doi: 10.1006/brbi.2000.0613. [DOI] [PubMed] [Google Scholar]
- 3.Yirmiya R, Weidenfeld J, Pollak Y, et al. Cytokines, "depression due to a general medical condition, " and antidepressant drugs. Adv Exp Med Biol. 1999;461:283–316. doi: 10.1007/978-0-585-37970-8_16. [DOI] [PubMed] [Google Scholar]
- 4.Dantzer R. Cytokine-induced sickness behavior: mechanisms and implications. Ann N Y Acad Sci. 2001;933:222–234. doi: 10.1111/j.1749-6632.2001.tb05827.x. [DOI] [PubMed] [Google Scholar]
- 5.Dantzer R, Kelley KW. Twenty years of research on cytokine-induced sickness behavior. Brain Behav Immun. 2007;21:153–160. doi: 10.1016/j.bbi.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee BN, Dantzer R, Langley KE, et al. A cytokine-based neuroimmunologic mechanism of cancer-related symptoms. Neuroimmunomodulation. 2004;11:279–292. doi: 10.1159/000079408. [DOI] [PubMed] [Google Scholar]
- 8.Szabo S, Gould TD, Manji HK. Neurotransmitters, receptors, signal transduction, and second messengers in psychiatric disorders. In: Schatzberg A, Nemeroff CB, editors. Textbook of Psychopharmacology. Third Edition. Washington, DC: American Psychiatric Publishing; 2004. pp. 3–52. [Google Scholar]
- 9.Dunn AJ, Wang J, Ando T. Effects of cytokines on cerebral neurotransmission. Comparison with the effects of stress. Adv Exp Med Biol. 1999;461:117–127. doi: 10.1007/978-0-585-37970-8_8. [DOI] [PubMed] [Google Scholar]
- 10.Capuron L, Raison CL, Musselman DL, et al. Association of exaggerated HPA axis response to the initial injection of interferon-alpha with development of depression during interferon-alpha therapy. Am J Psychiatry. 2003;160:1342–1345. doi: 10.1176/appi.ajp.160.7.1342. [DOI] [PubMed] [Google Scholar]
- 11.Gisslinger H, Svoboda T, Clodi M, et al. Interferon-alpha stimulates the hypothalamic-pituitary-adrenal axis in vivo and in vitro. Neuroendocrinology. 1993;57:489–495. doi: 10.1159/000126396. [DOI] [PubMed] [Google Scholar]
- 12.Capuron L, Neurauter G, Musselman DL, et al. Interferon-alpha-induced changes in tryptophan metabolism. relationship to depression and paroxetine treatment. Biol Psychiatry. 2003;54:906–914. doi: 10.1016/s0006-3223(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 13.Bonaccorso S, Marino V, Puzella A, et al. Increased depressive ratings in patients with hepatitis C receiving interferon-alpha-based immunotherapy are related to interferon-alpha-induced changes in the serotonergic system. J Clin Psychopharmacol. 2002;22:86–90. doi: 10.1097/00004714-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Zhu CB, Blakely RD, Hewlett WA. The proinflammatory cytokines interleukin-1beta and tumor necrosis factor-alpha activate serotonin transporters. Neuropsychopharmacology. 2006;31:2121–2131. doi: 10.1038/sj.npp.1301029. [DOI] [PubMed] [Google Scholar]
- 15.Besedovsky HO, del Rey A. Immune-neuro-endocrine interactions: facts and hypotheses. Endocr Rev. 1996;17:64–102. doi: 10.1210/edrv-17-1-64. [DOI] [PubMed] [Google Scholar]
- 16.Ericsson A, Kovacs KJ, Sawchenko PE. A functional anatomical analysis of central pathways subserving the effects of interleukin-1 on stress-related neuroendocrine neurons. J Neurosci. 1994;14:897–913. doi: 10.1523/JNEUROSCI.14-02-00897.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Owens MJ, Nemeroff CB. Physiology and pharmacology of corticotropin-releasing factor. Pharmacol Rev. 1991;43:425–473. [PubMed] [Google Scholar]
- 18.Capuron L, Pagnoni G, Demetrashvili M, et al. Anterior cingulate activation and error processing during interferon-alpha treatment. Biol Psychiatry. 2005;58:190–196. doi: 10.1016/j.biopsych.2005.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eisenberger NI, Lieberman MD. Why rejection hurts: a common neural alarm system for physical and social pain. Trends Cogn Sci. 2004;8:294–300. doi: 10.1016/j.tics.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 20.Capuron L, Pagnoni G, Demetrashvili MF, et al. Basal Ganglia Hypermetabolism and Symptoms of Fatigue during Interferon-alpha Therapy. Neuropsychopharmacology. 2007 doi: 10.1038/sj.npp.1301362. [DOI] [PubMed] [Google Scholar]
- 21.Juengling FD, Ebert D, Gut O, et al. Prefrontal cortical hypometabolism during low-dose interferon alpha treatment. Psychopharmacology (Berl) 2000;152:383–389. doi: 10.1007/s002130000549. [DOI] [PubMed] [Google Scholar]
- 22.Capuron L, Ravaud A, Dantzer R. Timing and specificity of the cognitive changes induced by interleukin-2 and interferon-alpha treatments in cancer patients. Psychosom Med. 2001;63:376–386. doi: 10.1097/00006842-200105000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Maier SF. Bi-directional immune-brain communication: Implications for understanding stress, pain, and cognition. Brain Behav Immun. 2003;17:69–85. doi: 10.1016/s0889-1591(03)00032-1. [DOI] [PubMed] [Google Scholar]
- 24.Maier SF, Watkins LR. Immune-to-central nervous system communication and its role in modulating pain and cognition: Implications for cancer and cancer treatment. Brain Behav Immun. 2003;17 Suppl 1:S125–S131. doi: 10.1016/s0889-1591(02)00079-x. [DOI] [PubMed] [Google Scholar]
- 25.Monje ML, Toda H, Palmer TD. Inflammatory blockade restores adult hippocampal neurogenesis. Science. 2003;302:1760–1765. doi: 10.1126/science.1088417. [DOI] [PubMed] [Google Scholar]
- 26.Mills PJ, Parker B, Jones V, et al. The effects of standard anthracycline-based chemotherapy on soluble ICAM-1 and vascular endothelial growth factor levels in breast cancer. Clin Cancer Res. 2004;10:4998–5003. doi: 10.1158/1078-0432.CCR-0734-04. [DOI] [PubMed] [Google Scholar]
- 27.Pusztai L, Mendoza TR, Reuben JM, et al. Changes in plasma levels of inflammatory cytokines in response to paclitaxel chemotherapy. Cytokine. 2004;25:94–102. doi: 10.1016/j.cyto.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 28.Irwin MR, Wang M, Campomayor CO, et al. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. Arch Intern Med. 166 doi: 10.1001/archinte.166.16.1756. in press. [DOI] [PubMed] [Google Scholar]
- 29.Meier-Ewert HK, Ridker PM, Rifai N, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- 30.Vgontzas AN, Zoumakis E, Bixler EO, et al. Adverse effects of modest sleep restriction on sleepiness, performance, and inflammatory cytokines. J Clin Endocrinol Metab. 2004;89:2119–2126. doi: 10.1210/jc.2003-031562. [DOI] [PubMed] [Google Scholar]
- 31.Motivala SJ, Sarfatti A, Olmos L, et al. Inflammatory markers and sleep disturbance in major depression. Psychosom Med. 2005;67:187–194. doi: 10.1097/01.psy.0000149259.72488.09. [DOI] [PubMed] [Google Scholar]
- 32.Irwin M, Rinetti G, Redwine L, et al. Nocturnal proinflammatory cytokine-associated sleep disturbances in abstinent African American alcoholics. Brain Behav Immun. 2004;18:349–360. doi: 10.1016/j.bbi.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 33.Redwine L, Dang J, Hall M, et al. Disordered sleep, nocturnal cytokines, and immunity in alcoholics. Psychosom Med. 2003;65:75–85. doi: 10.1097/01.psy.0000038943.33335.d2. [DOI] [PubMed] [Google Scholar]
- 34.Spath-Schwalbe E, Hansen K, Schmidt F, et al. Acute effects of recombinant human interleukin-6 on endocrine and central nervous sleep functions in healthy men. J Clin Endocrinol Metab. 1998;83:1573–1579. doi: 10.1210/jcem.83.5.4795. [DOI] [PubMed] [Google Scholar]
- 35.Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. Am J Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- 36.Bierhaus A, Wolf J, Andrassy M, et al. A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci U S A. 2003;100:1920–1925. doi: 10.1073/pnas.0438019100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pace TW, Mletzko TC, Alagbe O, et al. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. Am J Psychiatry. 2006;163:1630–1633. doi: 10.1176/ajp.2006.163.9.1630. [DOI] [PubMed] [Google Scholar]
- 38.Frank MG, Baratta MV, Sprunger DB, et al. Microglia serve as a neuroimmune substrate for stress-induced potentiation of CNS pro-inflammatory cytokine responses. Brain Behav Immun. 2007;21:47–59. doi: 10.1016/j.bbi.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 39.Johnson JD, Campisi J, Sharkey CM, et al. Catecholamines mediate stress-induced increases in peripheral and central inflammatory cytokines. Neuroscience. 2005;135:1295–1307. doi: 10.1016/j.neuroscience.2005.06.090. [DOI] [PubMed] [Google Scholar]
- 40.Barrientos RM, Sprunger DB, Campeau S, et al. BDNF mRNA expression in rat hippocampus following contextual learning is blocked by intrahippocampal IL-1beta administration. J Neuroimmunol. 2004;155:119–126. doi: 10.1016/j.jneuroim.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 41.Duman RS, Monteggia LM. A neurotrophic model for stress-related mood disorders. Biol Psychiatry. 2006;59:1116–1127. doi: 10.1016/j.biopsych.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 42.Pavlov VA, Tracey KJ. The cholinergic anti-inflammatory pathway. Brain Behav Immun. 2005;19:493–499. doi: 10.1016/j.bbi.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 43.Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids--new mechanisms for old drugs. N Engl J Med. 2005;353:1711–1723. doi: 10.1056/NEJMra050541. [DOI] [PubMed] [Google Scholar]
- 44.Smoak KA, Cidlowski JA. Mechanisms of glucocorticoid receptor signaling during inflammation. Mech Ageing Dev. 2004;125:697–706. doi: 10.1016/j.mad.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 45.Wang X, Wu H, Miller AH. Interleukin 1alpha (IL-1alpha) induced activation of p38 mitogen-activated protein kinase inhibits glucocorticoid receptor function. Mol Psychiatry. 2004;9:65–75. doi: 10.1038/sj.mp.4001339. [DOI] [PubMed] [Google Scholar]
- 46.Pace TW, Hu F, Miller AH. Cytokine-effects on glucocorticoid receptor function: Relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun. 2007;21:9–19. doi: 10.1016/j.bbi.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maes M, Bosmans E, Meltzer HY, et al. Interleukin-1 beta: a putative mediator of HPA axis hyperactivity in major depression? Am J Psychiatry. 1993;150:1189–1193. doi: 10.1176/ajp.150.8.1189. [DOI] [PubMed] [Google Scholar]
- 48.Raison CL, Miller AH. When not enough is too much: the role of insufficient glucocorticoid signaling in the pathophysiology of stress-related disorders. Am J Psychiatry. 2003;160:1554–1565. doi: 10.1176/appi.ajp.160.9.1554. [DOI] [PubMed] [Google Scholar]
- 49.McDaniel JS, Musselman DL, Porter MR, et al. Depression in patients with cancer. Diagnosis, biology, and treatment. Arch Gen Psychiatry. 1995;52:89–99. doi: 10.1001/archpsyc.1995.03950140007002. [DOI] [PubMed] [Google Scholar]
- 50.Raison CL, Miller AH. Depression in cancer: new developments regarding diagnosis and treatment. Biol Psychiatry. 2003;54:283–294. doi: 10.1016/s0006-3223(03)00413-x. [DOI] [PubMed] [Google Scholar]
- 51.Spiegel D, Giese-Davis J. Depression and cancer: mechanisms and disease progression. Biol Psychiatry. 2003;54:269–282. doi: 10.1016/s0006-3223(03)00566-3. [DOI] [PubMed] [Google Scholar]
- 52.Onitilo AA, Nietert PJ, Egede LE. Effect of depression on all-cause mortality in adults with cancer and differential effects by cancer site. Gen Hosp Psychiatry. 2006;28:396–402. doi: 10.1016/j.genhosppsych.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 53.Musselman DL, Miller AH, Porter MR, et al. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry. 2001;158:1252–1257. doi: 10.1176/appi.ajp.158.8.1252. [DOI] [PubMed] [Google Scholar]
- 54.Jehn CF, Kuehnhardt D, Bartholomae A, et al. Biomarkers of depression in cancer patients. Cancer. 2006;107:2723–2729. doi: 10.1002/cncr.22294. [DOI] [PubMed] [Google Scholar]
- 55.Evans DL, McCartney CF, Nemeroff CB, et al. Depression in women treated for gynecological cancer: clinical and neuroendocrine assessment. Am J Psychiatry. 1986;143:447–452. doi: 10.1176/ajp.143.4.447. [DOI] [PubMed] [Google Scholar]
- 56.Lawrence DP, Kupelnick B, Miller K, et al. Evidence report on the occurrence, assessment, and treatment of fatigue in cancer patients. J Natl Cancer Inst Monogr. 2004:40–50. doi: 10.1093/jncimonographs/lgh027. [DOI] [PubMed] [Google Scholar]
- 57.Servaes P, Verhagen C, Bleijenberg G. Fatigue in cancer patients during and after treatment: prevalence, correlates and interventions. Eur J Cancer. 2002;38:27–43. doi: 10.1016/s0959-8049(01)00332-x. [DOI] [PubMed] [Google Scholar]
- 58.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in breast cancer survivors: occurrence, correlates, and impact on quality of life. J Clin Oncol. 2000;18:743–753. doi: 10.1200/JCO.2000.18.4.743. [DOI] [PubMed] [Google Scholar]
- 59.Cella D, Davis K, Breitbart W, et al. Cancer-related fatigue: prevalence of proposed diagnostic criteria in a United States sample of cancer survivors. J Clin Oncol. 2001;19:3385–3391. doi: 10.1200/JCO.2001.19.14.3385. [DOI] [PubMed] [Google Scholar]
- 60.Bower JE, Ganz PA, Desmond KA, et al. Fatigue in long-term breast carcinoma survivors: a longitudinal investigation. Cancer. 2006;106:751–758. doi: 10.1002/cncr.21671. [DOI] [PubMed] [Google Scholar]
- 61.Meyers CA, Albitar M, Estey E. Cognitive impairment, fatigue, and cytokine levels in patients with acute myelogenous leukemia or myelodysplastic syndrome. Cancer. 2005;104:788–793. doi: 10.1002/cncr.21234. [DOI] [PubMed] [Google Scholar]
- 62.Costanzo ES, Lutgendorf SK, Sood AK, et al. Psychosocial factors and interleukin-6 among women with advanced ovarian cancer. Cancer. 2005;104:305–313. doi: 10.1002/cncr.21147. [DOI] [PubMed] [Google Scholar]
- 63.Greenberg DB, Gray JL, Mannix CM, et al. Treatment-related fatigue and serum interleukin-1 levels in patients during external beam irradiation for prostate cancer. J Pain Symptom Manage. 1993;8:196–200. doi: 10.1016/0885-3924(93)90127-h. [DOI] [PubMed] [Google Scholar]
- 64.Wratten C, Kilmurray J, Nash S, et al. Fatigue during breast radiotherapy and its relationship to biological factors. Int J Radiat Oncol Biol Phys. 2004;59:160–167. doi: 10.1016/j.ijrobp.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 65.Mills PJ, Parker B, Dimsdale JE, et al. The relationship between fatigue and quality of life and inflammation during anthracycline-based chemotherapy in breast cancer. Biol Psychol. 2005;69:85–96. doi: 10.1016/j.biopsycho.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 66.Geinitz H, Zimmermann FB, Stoll P, et al. Fatigue, serum cytokine levels, and blood cell counts during radiotherapy of patients with breast cancer. Int J Radiat Oncol Biol Phys. 2001;51:691–698. doi: 10.1016/s0360-3016(01)01657-1. [DOI] [PubMed] [Google Scholar]
- 67.Ahlberg K, Ekman T, Gaston-Johansson F. Levels of fatigue compared to levels of cytokines and hemoglobin during pelvic radiotherapy: a pilot study. Biol Res Nurs. 2004;5:203–210. doi: 10.1177/1099800403259500. [DOI] [PubMed] [Google Scholar]
- 68.Shafqat A, Einhorn LH, Hanna N, et al. Screening studies for fatigue and laboratory correlates in cancer patients undergoing treatment. Ann Oncol. 2005;16:1545–1550. doi: 10.1093/annonc/mdi267. [DOI] [PubMed] [Google Scholar]
- 69.Bower JE, Ganz PA, Aziz N, et al. Fatigue and proinflammatory cytokine activity in breast cancer survivors. Psychosom Med. 2002;64:604–611. doi: 10.1097/00006842-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 70.Collado-Hidalgo A, Bower JE, Ganz PA, et al. Inflammatory biomarkers for persistent fatigue in breast cancer survivors. Clin Cancer Res. 2006;12:2759–2766. doi: 10.1158/1078-0432.CCR-05-2398. [DOI] [PubMed] [Google Scholar]
- 71.Knobel H, Loge JH, Nordoy T, et al. High level of fatigue in lymphoma patients treated with high dose therapy. J Pain Symptom Manage. 2000;19:446–456. doi: 10.1016/s0885-3924(00)00144-5. [DOI] [PubMed] [Google Scholar]
- 72.Dimeo F, Schmittel A, Fietz T, et al. Physical performance, depression, immune status and fatigue in patients with hematological malignancies after treatment. Ann Oncol. 2004;15:1237–1242. doi: 10.1093/annonc/mdh314. [DOI] [PubMed] [Google Scholar]
- 73.Schubert C, Hong S, Natarajan L, et al. The association between fatigue and inflammatory marker levels in cancer patients: a quantitative review. Brain Behav Immun. 2007;21:413–427. doi: 10.1016/j.bbi.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 74.Morant R, Stiefel F, Berchtold W, et al. Preliminary results of a study assessing asthenia and related psychological and biological phenomena in patients with advanced cancer. Support Care Cancer. 1993;1:101–107. doi: 10.1007/BF00366904. [DOI] [PubMed] [Google Scholar]
- 75.Brown DJ, McMillan DC, Milroy R. The correlation between fatigue, physical function, the systemic inflammatory response, and psychological distress in patients with advanced lung cancer. Cancer. 2005;103:377–382. doi: 10.1002/cncr.20777. [DOI] [PubMed] [Google Scholar]
- 76.Bower JE, Ganz PA, Dickerson SS, et al. Diurnal cortisol rhythm and fatigue in breast cancer survivors. Psychoneuroendocrinology. 2005;30:92–100. doi: 10.1016/j.psyneuen.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 77.Bower JE, Ganz PA, Aziz N. Altered cortisol response to psychologic stress in breast cancer survivors with persistent fatigue. Psychosom Med. 2005;67:277–280. doi: 10.1097/01.psy.0000155666.55034.c6. [DOI] [PubMed] [Google Scholar]
- 78.Bower JE, Ganz PA, Aziz N, et al. Inflammatory responses to psychological stress in fatigued breast cancer survivors: relationship to glucocorticoids. Brain Behav Immun. 2007;21:251–258. doi: 10.1016/j.bbi.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 79.Rich T, Innominato PF, Boerner J, et al. Elevated serum cytokines correlated with altered behavior, serum cortisol rhythm, and dampened 24-hour rest-activity patterns in patients with metastatic colorectal cancer. Clin Cancer Res. 2005;11:1757–1764. doi: 10.1158/1078-0432.CCR-04-2000. [DOI] [PubMed] [Google Scholar]
- 80.Savard J, Simard S, Blanchet J, et al. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24:583–590. doi: 10.1093/sleep/24.5.583. [DOI] [PubMed] [Google Scholar]
- 81.Lee K, Cho M, Miaskowski C, et al. Impaired sleep and rhythms in persons with cancer. Sleep Med Rev. 2004;8:199–212. doi: 10.1016/j.smrv.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 82.Ancoli-Israel S, Liu L, Marler MR, et al. Fatigue, sleep, and circadian rhythms prior to chemotherapy for breast cancer. Support Care Cancer. 2006;14:201–209. doi: 10.1007/s00520-005-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Savard J, Morin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001;19:895–908. doi: 10.1200/JCO.2001.19.3.895. [DOI] [PubMed] [Google Scholar]
- 84.Holley S. Cancer-related fatigue. Suffering a different fatigue. Cancer Pract. 2000;8:87–95. doi: 10.1046/j.1523-5394.2000.82007.x. [DOI] [PubMed] [Google Scholar]
- 85.Poulson MJ. Not just tired. J Clin Oncol. 2001;19:4180–4181. doi: 10.1200/JCO.2001.19.21.4180. [DOI] [PubMed] [Google Scholar]
- 86.Sephton SE, Sapolsky RM, Kraemer HC, et al. Diurnal cortisol rhythm as a predictor of breast cancer survival. J Natl Cancer Inst. 2000;92:994–1000. doi: 10.1093/jnci/92.12.994. [DOI] [PubMed] [Google Scholar]
- 87.Mormont MC, Waterhouse J, Bleuzen P, et al. Marked 24-h rest/activity rhythms are associated with better quality of life, better response, and longer survival in patients with metastatic colorectal cancer and good performance status. Clin Cancer Res. 2000;6:3038–3045. [PubMed] [Google Scholar]
- 88.Fiorentino L, Ancoli-Israel S. Insomnia and its treatment in women with breast cancer. Sleep Med Rev. doi: 10.1016/j.smrv.2006.03.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 90.Caufriez A, Moreno-Reyes R, Leproult R, et al. Immediate effects of an 8-h advance shift of the rest-activity cycle on 24-h profiles of cortisol. Am J Physiol Endocrinol Metab. 2002;282:E1147–E1153. doi: 10.1152/ajpendo.00525.2001. [DOI] [PubMed] [Google Scholar]
- 91.Meerlo P, Koehl M, van der Borght K, et al. Sleep restriction alters the hypothalamic-pituitary-adrenal response to stress. J Neuroendocrinol. 2002;14:397–402. doi: 10.1046/j.0007-1331.2002.00790.x. [DOI] [PubMed] [Google Scholar]
- 92.Tannock IF, Ahles TA, Ganz PA, et al. Cognitive impairment associated with chemotherapy for cancer: report of a workshop. J Clin Oncol. 2004;22:2233–2239. doi: 10.1200/JCO.2004.08.094. [DOI] [PubMed] [Google Scholar]
- 93.Ferguson RJ, Ahles TA. Low neuropsychologic performance among adult cancer survivors treated with chemotherapy. Curr Neurol Neurosci Rep. 2003;3:215–222. doi: 10.1007/s11910-003-0081-2. [DOI] [PubMed] [Google Scholar]
- 94.Castellon SA, Silverman DH, Ganz PA. Breast cancer treatment and cognitive functioning: current status and future challenges in assessment. Breast Cancer Res Treat. 2005;92:199–206. doi: 10.1007/s10549-005-5342-0. [DOI] [PubMed] [Google Scholar]
- 95.van Dam FS, Schagen SB, Muller MJ, et al. Impairment of cognitive function in women receiving adjuvant treatment for high-risk breast cancer: high-dose versus standard-dose chemotherapy. J Natl Cancer Inst. 1998;90:210–218. doi: 10.1093/jnci/90.3.210. [DOI] [PubMed] [Google Scholar]
- 96.Anderson-Hanley C, Sherman ML, Riggs R, et al. Neuropsychological effects of treatments for adults with cancer: a meta-analysis and review of the literature. J Int Neuropsychol Soc. 2003;9:967–982. doi: 10.1017/S1355617703970019. [DOI] [PubMed] [Google Scholar]
- 97.Ganz PA. Cognitive dysfunction following adjuvant treatment of breast cancer: a new doselimiting toxic effect? J Natl Cancer Inst. 1998;90:182–183. doi: 10.1093/jnci/90.3.182. [DOI] [PubMed] [Google Scholar]
- 98.Schagen SB, van Dam FS, Muller MJ, et al. Cognitive deficits after postoperative adjuvant chemotherapy for breast carcinoma. Cancer. 1999;85:640–650. doi: 10.1002/(sici)1097-0142(19990201)85:3<640::aid-cncr14>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 99.Ahles TA, Saykin AJ, Furstenberg CT, et al. Neuropsychologic impact of standard-dose systemic chemotherapy in long-term survivors of breast cancer and lymphoma. J Clin Oncol. 2002;20:485–493. doi: 10.1200/JCO.2002.20.2.485. [DOI] [PubMed] [Google Scholar]
- 100.Wefel JS, Lenzi R, Theriault RL, et al. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;100:2292–2299. doi: 10.1002/cncr.20272. [DOI] [PubMed] [Google Scholar]
- 101.Stemmer SM, Stears JC, Burton BS, et al. White matter changes in patients with breast cancer treated with high-dose chemotherapy and autologous bone marrow support. AJNR Am J Neuroradiol. 1994;15:1267–1273. [PMC free article] [PubMed] [Google Scholar]
- 102.Brown MS, Simon JH, Stemmer SM, et al. MR and proton spectroscopy of white matter disease induced by high-dose chemotherapy with bone marrow transplant in advanced breast carcinoma. AJNR Am J Neuroradiol. 1995;16:2013–2020. [PMC free article] [PubMed] [Google Scholar]
- 103.Silverman DH, Dy CJ, Castellon SA, et al. Altered frontocortical, cerebellar, and basal ganglia activity in adjuvant-treated breast cancer survivors 5–10 years after chemotherapy. Breast Cancer Res Treat. 2006 doi: 10.1007/s10549-006-9380-z. [DOI] [PubMed] [Google Scholar]
- 104.Keime-Guibert F, Napolitano M, Delattre JY. Neurological complications of radiotherapy and chemotherapy. J Neurol. 1998;245:695–708. doi: 10.1007/s004150050271. [DOI] [PubMed] [Google Scholar]
- 105.Capuron L, Gumnick JF, Musselman DL, et al. Neurobehavioral effects of interferon-alpha in cancer patients: phenomenology and paroxetine responsiveness of symptom dimensions. Neuropsychopharmacology. 2002;26:643–652. doi: 10.1016/S0893-133X(01)00407-9. [DOI] [PubMed] [Google Scholar]
- 106.Valentine AD, Meyers CA, Kling MA, et al. Mood and cognitive side effects of interferon-alpha therapy. Semin Oncol. 1998;25:39–47. [PubMed] [Google Scholar]
- 107.Meyers CA, Yung WK. Delayed neurotoxicity of intraventricular interleukin-2: a case report. J Neurooncol. 1993;15:265–267. doi: 10.1007/BF01050073. [DOI] [PubMed] [Google Scholar]
- 108.Meyers CA, Scheibel RS, Forman AD. Persistent neurotoxicity of systemically administered interferon-alpha. Neurology. 1991;41:672–676. doi: 10.1212/wnl.41.5.672. [DOI] [PubMed] [Google Scholar]
- 109.Fishman D, Faulds G, Jeffery R, et al. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Invest. 1998;102:1369–1376. doi: 10.1172/JCI2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 111.Zorrilla EP, Luborsky L, McKay JR, et al. The relationship of depression and stressors to immunological assays: a meta-analytic review. Brain Behav Immun. 2001;15:199–226. doi: 10.1006/brbi.2000.0597. [DOI] [PubMed] [Google Scholar]
- 112.Ridker PM, Rifai N, Stampfer MJ, et al. Plasma concentration of interleukin-6 and the risk of future myocardial infarction among apparently healthy men. Circulation. 2000;101:1767–1772. doi: 10.1161/01.cir.101.15.1767. [DOI] [PubMed] [Google Scholar]
- 113.Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation. 2003;107:363–369. doi: 10.1161/01.cir.0000053730.47739.3c. [DOI] [PubMed] [Google Scholar]
- 114.Schmidt MI, Duncan BB, Sharrett AR, et al. Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet. 1999;353:1649–1652. doi: 10.1016/s0140-6736(99)01046-6. [DOI] [PubMed] [Google Scholar]
- 115.Browning LM, Krebs JD, Jebb SA. Discrimination ratio analysis of inflammatory markers: implications for the study of inflammation in chronic disease. Metabolism. 2004;53:899–903. doi: 10.1016/j.metabol.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 116.Gielissen MF, Verhagen S, Witjes F, et al. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24:4882–4887. doi: 10.1200/JCO.2006.06.8270. [DOI] [PubMed] [Google Scholar]
- 117.Jacobsen PB, Meade CD, Stein KD, et al. Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol. 2002;20:2851–2862. doi: 10.1200/JCO.2002.08.301. [DOI] [PubMed] [Google Scholar]
- 118.Stanton AL, Ganz PA, Kwan L, et al. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23:6009–6018. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- 119.Pinto BM, Frierson GM, Rabin C, et al. Home-based physical activity intervention for breast cancer patients. J Clin Oncol. 2005;23:3577–3587. doi: 10.1200/JCO.2005.03.080. [DOI] [PubMed] [Google Scholar]
- 120.Courneya KS, Mackey JR, Bell GJ, et al. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol. 2003;21:1660–1668. doi: 10.1200/JCO.2003.04.093. [DOI] [PubMed] [Google Scholar]
- 121.Frank E. Interpersonal and social rhythm therapy: a means of improving depression and preventing relapse in bipolar disorder. J Clin Psychol. 2007;63:463–473. doi: 10.1002/jclp.20371. [DOI] [PubMed] [Google Scholar]
- 122.Carlson LE, Speca M, Patel KD, et al. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571–581. doi: 10.1097/01.psy.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 123.Andersen BL, Farrar WB, Golden-Kreutz D, et al. Distress reduction from a psychological intervention contributes to improved health for cancer patients. Brain Behav Immun. 2007 doi: 10.1016/j.bbi.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Andersen BL, Farrar WB, Golden-Kreutz DM, et al. Psychological, behavioral, and immune changes after a psychological intervention: a clinical trial. J Clin Oncol. 2004;22:3570–3580. doi: 10.1200/JCO.2004.06.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Antoni MH, Wimberly SR, Lechner SC, et al. Reduction of cancer-specific thought intrusions and anxiety symptoms with a stress management intervention among women undergoing treatment for breast cancer. Am J Psychiatry. 2006;163:1791–1797. doi: 10.1176/ajp.2006.163.10.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Cruess DG, Antoni MH, McGregor BA, et al. Cognitive-behavioral stress management reduces serum cortisol by enhancing benefit finding among women being treated for early stage breast cancer. Psychosom Med. 2000;62:304–308. doi: 10.1097/00006842-200005000-00002. [DOI] [PubMed] [Google Scholar]
- 127.McGregor BA, Antoni MH, Boyers A, et al. Cognitive-behavioral stress management increases benefit finding and immune function among women with early-stage breast cancer. J Psychosom Res. 2004;56:1–8. doi: 10.1016/S0022-3999(03)00036-9. [DOI] [PubMed] [Google Scholar]
- 128.Fairey AS, Courneya KS, Field CJ, et al. Effect of exercise training on C-reactive protein in postmenopausal breast cancer survivors: a randomized controlled trial. Brain Behav Immun. 2005;19:381–388. doi: 10.1016/j.bbi.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 129.Mock V. Evidence-based treatment for cancer-related fatigue. J Natl Cancer Inst Monogr. 2004:112–118. doi: 10.1093/jncimonographs/lgh025. [DOI] [PubMed] [Google Scholar]
- 130.Irwin MR, Cole JC, Nicassio PM. Comparative meta-analysis of behavioral interventions for insomnia and their efficacy in middle-aged adults and in older adults 55+ years of age. Health Psychol. 2006;25:3–14. doi: 10.1037/0278-6133.25.1.3. [DOI] [PubMed] [Google Scholar]
- 131.Morin C, Cholecchi C, Stone J, et al. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA. 1999;281:991–999. doi: 10.1001/jama.281.11.991. [DOI] [PubMed] [Google Scholar]
- 132.Espie CA. Insomnia: conceptual issues in the development, persistence, and treatment of sleep disorder in adults. Annu Rev Psychol. 2002;53:215–243. doi: 10.1146/annurev.psych.53.100901.135243. [DOI] [PubMed] [Google Scholar]
- 133.Montgomery P, Dennis J. Cognitive behavioural interventions for sleep problems in adults aged 60+ Cochrane Database Syst Rev. 2002 doi: 10.1002/14651858.CD003161. CD003161. [DOI] [PubMed] [Google Scholar]
- 134.Savard J, Simard S, Ivers H, et al. Randomized study on the efficacy of cognitive-behavioral therapy for insomnia secondary to breast cancer, part II: Immunologic effects. J Clin Oncol. 2005;23:6097–6106. doi: 10.1200/JCO.2005.12.513. [DOI] [PubMed] [Google Scholar]
- 135.Davidson J, Waisberg J, Brundage M, et al. Nonpharmacologic group treatment of insomnia: a preliminary study with cancer survivors. Psychooncology. 2001;10:389–397. doi: 10.1002/pon.525. [DOI] [PubMed] [Google Scholar]
- 136.Quesnel C, Savard J, Simard S, et al. Efficacy of congitive behavioral therapy for insomnia in women treated for nonmetastatic breast cancer. J Consult Clin Psychol. 2003;71:189–200. [PubMed] [Google Scholar]
- 137.Monk JP, Phillips G, Waite R, et al. Assessment of tumor necrosis factor alpha blockade as an intervention to improve tolerability of dose-intensive chemotherapy in cancer patients. J Clin Oncol. 2006;24:1852–1859. doi: 10.1200/JCO.2005.04.2838. [DOI] [PubMed] [Google Scholar]
- 138.Madhusudan S, Foster M, Muthuramalingam SR, et al. A phase II study of etanercept (Enbrel), a tumor necrosis factor alpha inhibitor in patients with metastatic breast cancer. Clin Cancer Res. 2004;10:6528–6534. doi: 10.1158/1078-0432.CCR-04-0730. [DOI] [PubMed] [Google Scholar]
- 139.Madhusudan S, Muthuramalingam SR, Braybrooke JP, et al. Study of etanercept, a tumor necrosis factor-alpha inhibitor, in recurrent ovarian cancer. J Clin Oncol. 2005;23:5950–5959. doi: 10.1200/JCO.2005.04.127. [DOI] [PubMed] [Google Scholar]
- 140.Musselman DL, Lawson DH, Gumnick JF, et al. Paroxetine for the prevention of depression induced by high-dose interferon alfa. N Engl J Med. 2001;344:961–966. doi: 10.1056/NEJM200103293441303. [DOI] [PubMed] [Google Scholar]
- 141.Schwartz AL, Thompson JA, Masood N. Interferon-induced fatigue in patients with melanoma: a pilot study of exercise and methylphenidate. Oncol Nurs Forum. 2002;29:E85–E90. doi: 10.1188/02.ONF.E85-E90. [DOI] [PubMed] [Google Scholar]
- 142.Weitzner MA, Meyers CA, Valentine AD. Methylphenidate in the treatment of neurobehavioral slowing associated with cancer and cancer treatment. J Neuropsychiatry Clin Neurosci. 1995;7:347–350. doi: 10.1176/jnp.7.3.347. [DOI] [PubMed] [Google Scholar]
- 143.Meyers CA, Weitzner MA, Valentine AD, et al. Methylphenidate therapy improves cognition, mood, and function of brain tumor patients. J Clin Oncol. 1998;16:2522–2527. doi: 10.1200/JCO.1998.16.7.2522. [DOI] [PubMed] [Google Scholar]
- 144.Zobel AW, Nickel T, Kunzel HE, et al. Effects of the high-affinity corticotropin-releasing hormone receptor 1 antagonist R121919 in major depression: the first 20 patients treated. J Psychiatr Res. 2000;34:171–181. doi: 10.1016/s0022-3956(00)00016-9. [DOI] [PubMed] [Google Scholar]
- 145.Miller AH, Vogt GJ, Pearce BD. The phosphodiesterase type 4 inhibitor, rolipram, enhances glucocorticoid receptor function. Neuropsychopharmacology. 2002;27:939–948. doi: 10.1016/S0893-133X(02)00381-0. [DOI] [PubMed] [Google Scholar]
- 146.Kuipers SD, Bramham CR. Brain-derived neurotrophic factor mechanisms and function in adult synaptic plasticity: new insights and implications for therapy. Curr Opin Drug Discov Devel. 2006;9:580–586. [PubMed] [Google Scholar]
- 147.Bianchi R, Brines M, Lauria G, et al. Protective effect of erythropoietin and its carbamylated derivative in experimental Cisplatin peripheral neurotoxicity. Clin Cancer Res. 2006;12:2607–2612. doi: 10.1158/1078-0432.CCR-05-2177. [DOI] [PubMed] [Google Scholar]
- 148.Liu L, Marler MR, Parker BA, et al. The relationship between fatigue and light exposure during chemotherapy. Support Care Cancer. 2005;13:1010–1017. doi: 10.1007/s00520-005-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Canaple L, Kakizawa T, Laudet V. The days and nights of cancer cells. Cancer Res. 2003;63:7545–7552. [PubMed] [Google Scholar]
- 150.Bower JE, Ganz PA, Aziz N, et al. T-cell homeostasis in breast cancer survivors with persistent fatigue. J Natl Cancer Inst. 2003;95:1165–1168. doi: 10.1093/jnci/djg0019. [DOI] [PubMed] [Google Scholar]
- 151.Gelinas C, Fillion L. Factors related to persistent fatigue following completion of breast cancer treatment. Oncol Nurs Forum. 2004;31:269–278. doi: 10.1188/04.ONF.269-278. [DOI] [PubMed] [Google Scholar]