Abstract
Background
Evidence-based primary prevention of allergic conditions is important in view of their increasing prevalence in Western industrialized countries.
Methods
The Cochrane and Medline databases were searched for relevant scientific publications that appeared from February 2003 to May 2008. Articles in the reference lists of recent reviews were also considered, and experts were directly asked for their opinions. The retrieved publications were screened for relevance by evaluation of the title and abstract, and then by evaluation of the entire text. Each study chosen for inclusion was assigned an evidence grade as well as a grade for study quality relating to its potential for bias (low or high). The revised recommendations were then formally accepted by a consensus of representatives of medical specialist societies and other organizations, including a patient self-help group.
Results
The search initially yielded 4556 results out of which 217 articles (4 Cochrane reviews, 14 meta-analyses, 19 randomized clinical trials, 135 cohort studies, and 45 case-control studies) were chosen for inclusion and critical appraisal. No major changes ensued in the existing recommendations to avoid exposure to tobacco smoke, breast-feed for 4 months (or use hypoallergenic formulas), avoid a mould-promoting indoor climate, avoid exposure to furry pets (particularly cats), and vaccinate according to the current recommendations of the Standing Committee on Vaccination of the Robert Koch Institute (Ständige Impfkommission, STIKO). Neither the delayed introduction of solid food nor the avoidance of potent dietary allergens is recommended as a means of primary prevention. New recommendations were issued regarding fish consumption (by the mother while breastfeeding and nursing, and by the infant as solid food), avoidance of overweight, and reduction of exposure to air pollutants.
Conclusions
This updated guideline serves as an aid in giving patients current, evidence-based recommendations for allergy prevention.
Keywords: allergy, evidence-based medicine, guideline, prevention
Atopic diseases such as allergic asthma, hay fever, and atopic eczema have become even more prevalent in Western industrialized countries in recent years (1). The causes of allergy and of the increased prevalence of atopic disease remain largely unexplained. As there is little opportunity for etiologically directed treatment, prevention takes on special importance (2). In 2004, the first S3 guideline for allergy prevention was issued in Germany by the Task Force on Allergy Prevention (Aktionsbündnis Allergieprävention, abap) with the support of the German Federal Ministry of Health and Social Security (3). This guideline has now been revised in accordance with the currently accepted methodology for evidence-based guidelines that are agreed upon by consensus.
Methods
The methods by which this guideline was revised were in accordance with national and international standards for the development of evidence-based guidelines agreed upon by consensus (4– 6).
Goal definition and target group
The primary objective of this guideline is prevention of the main types of atopic disease: atopic eczema, allergic rhinoconjunctivitis, and allergic asthma.
The guideline exclusively concerns measures for primary prevention. It makes use of the modified definitions in the area of allergy that were issued by abap (3). In the first edition of the guideline, the algorithm for children at risk was termed "secondary prevention"; in the new, revised edition, it is called "primary prevention" in accordance with the current definition, and it is subdivided into measures for persons with, and without, a genetic predisposition. Studies performed on persons already suffering from allergic disease, including studies whose aim was to prevent the development of a second disease, are no longer considered in the revised guideline.
The target population consists of all persons, especially children, with and without a genetic predisposition for atopic disease. By definition, genetically predisposed children (so-called children at risk) are those with at least one parent or sibling suffering from one of the atopic diseases mentioned above.
The guideline is intended for use by all medical and non-medical persons and groups concerned with preventive measures and, in particular, with allergy prevention.
The members of the guideline steering committee are C. Muche-Borowski, M. Kopp (German Society for Pediatrics and Adolescent Medicine, DGKJ), I. Reese (Task Force on Dietetics in Allergology [Arbeitskreis Diätetik in der Allergologie]), H. Sitter (Association of Scientific Medical Societies in Germany, AWMF), T. Werfel (German Society of Allergology and Clinical Immunology, DGAKI), and T. Schäfer (coordinator; German Dermatological Society, DDG).
Literature search for scientific evidence
The Medline and Cochrane databases were electronically searched for relevant literature appearing from February 2003 to May 2008.
For the search strategy, the authors defined three categories of key words, one each concerning diseases (asthma, allergy, allergic, atopic, hay fever, dermatitis, eczema, rhinitis), preventive measures (prevention, risk factor, epidemiology), and study types (randomized controlled trials, clinical trials, controlled study, case control study, cohort study, systematic review, meta-analysis). The connective term "or" was used within groups, and "and" was used between them.
Studies on human subjects published in either English or German were included. Studies whose primary target was non-allergic disease were excluded, as were therapeutic and medication studies.
Furthermore, the authors looked over the reference lists of current review articles for relevant literature, and asked all members of the consensus group to provide a list of relevant citations. Screening was performed in two steps, first by title and abstract, and then by consideration of the full text.
Assessment of evidence
In addition to the assignment of formal evidence levels (1a to 4), the studies were evaluated by methodologically critical reading according to predefined criteria (including case numbers, the temporal relation of exposure and disease, and consideration of further factors) and by the filling out of corresponding extraction tables. This critical assessment of study methods led to a binary grading of each study’s potential for bias as either high (–) or low (+).
The overall state of the evidence for each subject area was displayed in tabular form, including information on the number of studies, the study types, the evidence levels, and the classes of recommendation. Furthermore, for each subject area, the authors prepared evidence tables (not shown here) in which the number of studies retrieved by the literature search, and the number of studies assessed, were listed by type of study, main result (protective effect, risk factor, or no effect) and methodological quality (+ high, – low).
Draft guideline
On the basis of the publications that were retrieved and assessed, the authors prepared a draft proposal for the revised recommendations on prevention and circulated it among the members of the guideline and consensus groups.
Suggestions for amplification and updating were discussed and incorporated into the new guideline where appropriate.
Consensus
The consensus group initially consisted of all persons who had participated in the preparation of the first edition of the guideline and in the consensus process for it. Representatives of other specialist societies were then proposed for inclusion and invited to join the consensus group.
The consensus group that was formed in this way (box) approved the recommendations in the revised guidelines. The nominal group process (3) was chosen as the formal consensus procedure.
Box. Participating experts, specialist societies, and institutions.
Dr. hum. biol. Cathleen Muche-Borowski
-
Prof. Dr. med. Matthias Kopp
German Society for Pediatrics and Adolescent Medicine
(Deutsche Gesellschaft für Kinder- und Jugendmedizin e.V.; DGKJ)
-
Dr. med. Imke Reese
Task Force on Dietetics in Allergology
(Arbeitskreis Diätetik in der Allergologie)
-
PD Dr. rer. nat. Helmut Sitter
Association of Scientific Medical Societies in Germany
(Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften e.V.; AWMF)
-
Prof. Dr. med. Thomas Werfel
German Society of Allergology and Clinical Immunology
(Deutsche Gesellschaft für Allergologie und Klinische Immunologie; DGAK)
-
Prof. Dr. med. Torsten Schäfer
Coordinator, German Dermatological Society
(Deutsche Dermatologische Gesellschaft; DDG)
Dr. med. Kirsten Beyer
Dr. med. Frank Friedrichs
Prof. Dr. med. Eckard Hamelmann
Mechthild Hellermann
PD Dr. med. Johannes Huss-Marp
PD Dr. med. Susanne Lau
Dr. med. Ernst Rietschel
Dr. med. Sabine Schmidt
Sabine Schnadt
Dr. med. Andreas Kleinheinz
Prof. Dr. med. Claudia Rudack
Dr. med. Sylvia Schnitzer
The consensus meeting took place in Hanover, Germany, in January 2009 under the moderation of PD Dr. med. H. Sitter (University of Marburg and AWMF).
In the consensually approved recommendations, levels of evidence are denoted by the terms "well-documented" and "supported" (original German: Beleg/Hinweis). This terminology is based on the methods formulated by the German Institute for Quality and Efficiency in Health Care (Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen, IQWIG, General Methods 3.0).
The consensus group assigned a recommendation class (A, B, or C) to each of its recommendations, with the class appearing in parentheses after each recommendation. These recommendation classes were assigned on the basis of evidence levels according to a formalized procedure (table 1), but an allowance was made for well-founded deviations from this procedure in individual cases during the consensus-forming process. If no recommendations could be made in any particular area, the area was assigned evidence levels, but no recommendation class.
Table 1. Levels of evidence.
| 1a | Systematic review of randomized controlled trials |
| 1b | Individual randomized controlled trials |
| 1c | (All or none) |
| 2a | Systematic review of cohort studies |
| 2b | Individual cohort study (including low-quality randomized controlled trials) |
| 2c | ("Outcomes" research; ecological studies) |
| 3a | Systematic review of case-control studies |
| 3b | Individual case-control study |
| 4 | (Case series and) low-quality cohort and case-control studies |
(Modified from: Oxford Centre for Evidence-Based Medicine; www.cebm.net; May 2001)
Results
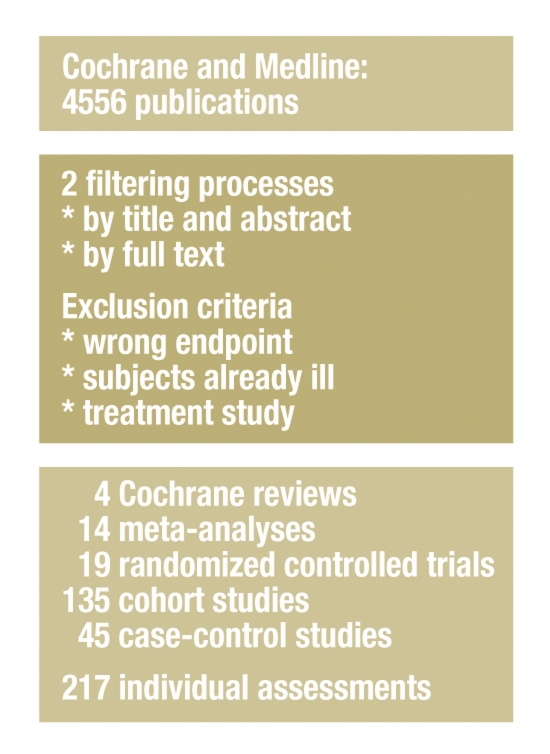
The search strategy described above turned up 4556 publications in Medline. 4228 of these were excluded in the first selection process, leaving 328 for the second selection process. Once the second selection process had been carried out and a number of additional publications had been included on the recommendation of members of the Consensus Group, there were a total of 217 original articles for analysis. These comprised 4 Cochrane reviews (CR), 14 meta-analyses (MA), 19 randomized controlled trials (RCT), 135 cohort studies (CS), and 45 case-control studies (figure 1). The overall state of the evidence is depicted in Table 2.
Figure 1.
Diagrammatic representation of the results of the search for evidence
Table 2. Complete tabular representation of the studies that were assessed and considered in the formulation of the recommendations, classified by subject area and by study types and numbers, derived evidence levels, and consensus recommendation classes.
| Subject area | Study types and numbers | Evidence levels | Recommendation classes |
| Breastfeeding | 0 CR, 1 MA, 3 RCT, 13 CS, 1 CC | 3×1b, 1×2a, 13×2b, 1×3b | A |
| Maternal nutrition during pregnancy and/or breastfeeding | 1 CR, 0 MA, 2 RCT, 13 CS, 1 CC | 1×1a, 2×1b, 13×2b, 1×3b | A and B |
| Feeding of children at risk with mother’s milk substitutes | 2 CR, 0 MA, 3 RCT, 2 CS, 0 CC | 2×1a, 3×1b, 2×2b | A |
| Introduction of solid food and child nutrition in the first year | 0 CR, 1 MA, 3 RCT, 12 CS, 3 CC | 1×1a, 3×1b, 12×2b, 3×3b | A and B |
| Nutrition after the first year | 0 CR, 0 MA, 0 RCT, 3 CS, 6 C | 3×2b, 6×3b | A |
| Pets | 0 CR, 2 MA, 0 RCT, 13 CS, 0 CC | 2×2a, 13×2b | B |
| Housedust mites | 0 CR, 0 MA, 2 RCT, 6 CS, 1 CC | 2×1b, 6×2b, 1×3b | B |
| Mold and damp | 0 CR, 1 MA, 0 RCT, 4 CS, 2 CC | 4×2b, 1×3a, 2×3b | B |
| Exposure to tobacco smoke | 0 CR, 1 MA, 0 RCT, 7 CS, 2 C | 1×2a, 7×2b, 2×3b | A |
| Indoor air pollutants | 0 CR, 1 MA, 0 RCT, 4 CS, 7 CC | 4×2b, 1×3a, 7×3b | B |
| Vaccinations | 0 CR, 1 MA, 1 RCT, 9 CS, 3 CC | 1×1a, 1×1b, 9×2b, 3×3b | A |
| Body weight | 0 CR, 3 MA, 0 RCT, 11 CS, 1 CC | 3×2a, 11×2b, 1×3b | A |
| Motor vehicle emissions | 0 CR, 0 MA, 0 RCT, 4 CS, 2 CC | 4×2b, 2×3b | B |
| Effect of probiotics | 1 CR, 1 MA, 5 RCT, 1 CS, 0 CC | 2×1a, 5×1b, 1×2b | – |
| Nonspecific immune modulation | 0 CR, 1 MA, 0 RCT, 10 CS, 5 CC | 10×2b, 1×3a, 5×3b | – |
| Antibiotics | 0 CR, 1 MA, 0 RCT, 3 CS, 1 CC | 1×2a, 3×2b, 1×3b | – |
| Overall | 4 CR, 14 MA, 19 RCT, 115 CS, 35 CC | 7×1a, 19×1b, 8×2a, 35 FK | |
| 115×2b, 2×3a, 35×3b |
CR, Cochrane review; MA, meta-analysis; RCT, randomized controlled trial; CS, cohort study; CC, case-control study
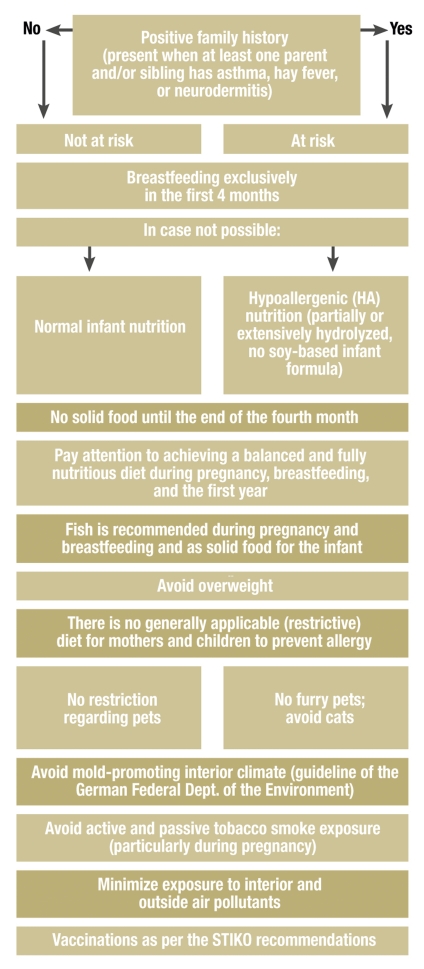
The consensus-derived recommendations for the primary prevention of asthma, hay fever, and atopic eczema are intended to apply both to persons at risk and to persons not at risk, as long as a distinction between these groups is not explicitly mentioned (figure 2). The recommendations are as follows:
Figure 2.
Algorithm for the primary prevention of asthma, hay fever, and atopic eczema in persons at risk and not at risk
With regard to nutrition, the consensus group unanimously supports the recommendations of the German specialist societies and organizations (www.fke-do.de, www.dge.de) concerning a balanced and fully nutritious diet for infants and toddlers and for pregnant women and nursing mothers.
Breastfeeding
The available data mostly support the recommendation that infants should be exclusively breast-fed in the first four months to prevent atopic diseases (A).
Maternal nutrition during pregnancy and breastfeeding
A balanced and fully nutritious diet is recommended during pregnancy and breastfeeding.
There is no well-documented evidence favoring a recommendation for any type of dietary restriction during pregnancy or breastfeeding (avoidance of potent dietary allergens) (A).
There is evidence supporting a protective effect of fish in the maternal diet during pregnancy and/or breastfeeding on the development of atopic diseases in the child (B).
Feeding of children at risk with mother’s milk substitutes
If breastfeeding is not possible or cannot be used as the sole means of feeding the child, then it is recommended that infants at risk should be given partially or extensively hydrolyzed formula till the end of the fourth month (A). (Note: Some of the types of infant formula that were tested in the studies incorporated in this recommendation are no longer available in Germany.)
Soy-based infant formula is not recommended for the purpose of allergy prevention (A).
Independently of the above, the specialist societies for dietary science recommend soy-based infant formula only for a very narrow range of indications, partly because of health-related concerns (7, 8). There is no well-documented evidence for an allergy-preventing effect of other types of animal milk (goat’s, sheep’s, or mare’s milk).
Solid food and nutrition of the child in the first year
There is no clear and well-documented evidence for a preventive effect of delaying the introduction of solid food beyond the end of the fourth month. Such a delay, therefore, cannot be recommended (A).
Nor is there any well-documented evidence for a preventive effect of dietary restriction involving the avoidance of potent dietary allergens in the first year. Therefore, this cannot be recommended (B).
There is evidence supporting a protective effect of fish consumption by the child in the first year on the development of atopic diseases (B).
The current recommendation in Germany that solid food should not be introduced till the end of the fourth month is reasonable from the point of view of dietary science.
Nutrition after the first year of life
There is no generally applicable diet that can be recommended for the prevention of allergy (A).
Pets
For persons not at elevated risk of allergy, there is no reason to restrict contact with pets as a preventive measure. The effect of contact with pets on the development of allergy in children at risk cannot be determined with certainty at the present time. Obtaining furry pets as a putatively preventive measure is not recommended.
Most of the studies concerning pet cats have found them to be a risk factor for allergy. Thus, cats should be avoided in households with a child at risk. Pet dogs, on the other hand, are probably not associated with a higher risk of allergy (B).
Housedust mites
The reduction of exposure to housedust mite allergens cannot be recommended as a primary preventive measure (B). Note: This statement concerns only primary, not secondary or tertiary prevention.
Mold and damp
An interior climate promoting the growth of mold (high air humidity, lack of ventilation) should be avoided to prevent allergy (B).
Tobacco smoke
Active and passive exposure to tobacco smoke elevates the risk of allergy, and of asthma in particular, and should be avoided. This is particularly true during pregnancy (A).
Interior air pollutants
There is evidence in support of an increased risk of atopic diseases, especially bronchial asthma, due to interior air pollutants. (Volatile organic compounds, e.g., formaldehyde, can be released from new furniture and during interior house-painting and renovation). Limiting exposure to interior air pollutants is recommended (B).
Vaccinations
There is no well-documented evidence for an allergy-promoting effect of vaccinations. There is evidence, however, that vaccinations can lower the risk of allergy. It is recommended that all children, including those at elevated risk of allergy, should be vaccinated according to the recommendations of the German Standing Vaccination Committee (Ständige Impfkommission, STIKO) (A).
Body weight
There is a well-documented positive association between an elevated body-mass index (BMI) and asthma in particular. Avoidance of overweight, especially in children, is recommended not only for general reasons, but also for allergy prevention (A).
Motor vehicle emissions
Exposure to nitrogen oxides and particulate matter (PM 2.5), particularly in persons living on streets with heavy motor vehicle traffic, is associated with an elevated risk of allergy, especially asthma.
Limiting exposure to motor vehicle emissions is recommended (B).
For the remaining subject areas, a position is stated, but no recommendation is made. The evidence level is given in parentheses.
Probiotics
Conflicting data have been published regarding the effect of probiotics on the development of allergy. At present, evidence of a preventive effect is seen only in Scandinavian studies and only with respect to the development of atopic eczema. Thus, no recommendation can be given (1a–2b).
Nonspecific immune modulation
There is evidence supporting a protective effect of early, nonspecific immune stimulation on the development of atopic diseases. Growing up on a farm, attending a day-care center in the first two years of life, and having older siblings are all considered to be types of nonspecific immune stimulation. Helminthic infections, especially hookworm, are negatively associated with asthma (2b–3b).
Antibiotics
A putative causal relationship between the administration of antibiotics and the development of asthma, allergic rhinitis, and atopic eczema has not been demonstrated (2a–3b).
Discussion
The updated guideline continues to support some of the first edition’s recommendations, gives others in revised form, and makes new recommendations as well. Extensive evidence, derived from 217 individual publications, was assessed in the preparation of the guideline.
Ideally, the qualitative recommendations would be supplemented with quantitative information about the extent of risk reduction. For methodological reasons, however, no more than limited information of this type can be provided. This prevention guideline also differs from classical treatment guidelines.
In order to make a robust quantitative estimate of risk reduction, the effect estimators should be derived from studies of high methodological quality, i.e., ideally, from randomized and prospective studies in which the intervention in question was investigated for its effect on risk or risk reduction.
For most of the interventions discussed here, however, such studies are not available and, for understandable reasons, would be difficult or impossible to perform, because parameters such as breastfeeding, smoking, or pets cannot be studied in a randomized design.
Therefore, most the studies to be considered are necessarily cohort and case-control studies, i.e., studies with a lower level of evidence, nor were they primarily performed to investigate the preventive effect of the individual factors in question. The recommendations for prevention were thus derived from the reported results in an indirect and post-hoc manner. As the methodological quality of the individual observational studies leaves much to be desired, post-hoc analyses of this type are also vulnerable to systematic bias.
A further difference from treatment guidelines is that multiple diseases and multiple potential risk factors are considered in this prevention guideline. These special methodological features and the qualitative and quantitative heterogeneity of some of the results further limit our ability to derive robust estimates of effect strength. For subject areas where enough study data are available and the homogeneous results could be examined together in meta-analyses (breastfeeding and smoking), the estimated effect strengths will be given below. For the remaining subject areas, the reader is referred to the evidence and extraction tables available online at www.leitlinien.net (AWMF-Reg.-Nr.061/016), in which results are given at the level of the individual studies.
The recommendations of the first edition of the guideline with respect to breastfeeding, pets, mold and damp, and tobacco smoke exposure remain well supported by the current study data.
Current data support breastfeeding for at least four months, as this reduces the risk of developing atopic disease—in particular, asthma or eczema—by 20% (9) to 40% (10, 11) compared to breastfeeding for shorter times. In Germany, the prevalence of medically diagnosed asthma and atopic eczema among children beginning school is 1.2%–3.8% and 6.8%–14.3%, respectively (12).
A meta-analysis regarding childhood exposure to tobacco smoke revealed a 30% increase in the risk of developing asthma (13).
The guideline contains altered or new statements about the following:
Many studies have shown a preventive effect of fish consumption by both the mother and the child.
Some of the types of hydrolyzed infant formula that were tested in studies are no longer available in Germany. As for soy-based formulae, there is not merely a lack of evidence for a protective effect; there is also concern about a deleterious effect to health from the phytoestrogens that they contain.
The current German cohort studies no longer show any effect from a delay in the introduction of solid food.
Reducing housedust mite allergens as a single primary preventive measure was found to have no effect. Accordingly, this recommendation was removed. This change does not concern secondary or tertiary prevention.
There was also a further development with regard to environmental air pollutants (motor vehicle emissions).
The recommendation to vaccinate was augmented with the statement that vaccination may even reduce the risk of allergy.
The positive association between an elevated body-mass index and asthma was supported by only a small amount of evidence in 2004 but has now been well documented in more recent studies.
In view of the current data, no dietary restrictions of any kind are recommended for either mothers or children. The topic of child nutrition is addressed in the chapter on solid food.
The revised guideline no longer contains information about specific immune therapy, as it exclusively concerns primary prevention.
The five formal prerequisites for an S3 guideline—logic (clinical algorithm) (14), consensus/formal consensus procedure (5), evidence-based medicine, decision analysis (15), and outcome analysis (16)—were met in a manner appropriately adapted to the topic of prevention.
Dissemination and implementation
The updated guideline will be published in other organs of the involved societies and organizations and will appear on the Internet on the AWMF homepage (www.awmf.org) and elsewhere (17, 18). Furthermore, flyers are being developed with a concise summary of the recommendations for both laypersons and physicians.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Professor Kopp has received study support from Infectopharm (Heppenheim, Germany). The remaining authors declare that they have no conflict of interest as defined by the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Asher M, Montefort S, Björkstén B, et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC phases one and three repeat multi-country cross-sectional surveys. Lancet. 2006;368:733–743. doi: 10.1016/S0140-6736(06)69283-0. [DOI] [PubMed] [Google Scholar]
- 2.Hamelmann E, Beyer K, Gruber C, et al. Primary prevention of allergy: avoiding risk or providing protection? Clin Exp Allergy. 2008;38:233–245. doi: 10.1111/j.1365-2222.2007.02901.x. [DOI] [PubMed] [Google Scholar]
- 3.Schäfer T, Borowski C, Diepgen T, et al. Evidenz-basierte und konsentierte Leitlinie „Allergieprävention“. Allergo J. 2004;13:252–260. doi: 10.1046/j.1439-0353.2004.04533.x. [DOI] [PubMed] [Google Scholar]
- 4.AWMF, ÄZQ. Das Leitlinienmanual. ZaeFQ. 2001;95(Supp 1) [Google Scholar]
- 5.Grimshaw J, Eccles M, Russell I. Developing clinically valid practice guidelines. J Eval Clin Pract. 1995;1:37–48. doi: 10.1111/j.1365-2753.1995.tb00006.x. [DOI] [PubMed] [Google Scholar]
- 6.Sackett D, Rosenberg W, Gray J, Haynes R. Evidence-based medicine. How to practice and teach EbM. New York: Churchill Livingstone; 1997. [Google Scholar]
- 7.Ernährungskommission der Deutschen Gesellschaft für Kinder- und Jugendmedizin und Ernährungskommission der Schweizerischen Gesellschaft für Pädiatrie. Stellungnahme zur Verwendung von Säuglingsnahrungen auf Sojaeiweißbasis. Monatsschr Kinderheilkd. 2006;154:913–916. [Google Scholar]
- 8.ESPGHAN Committee on Nutrition [Agostoni C, Axelsson I, Goulet O,et al.] Soy protein infant formulae and follow-on formulae: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2006;42:352–361. doi: 10.1097/01.mpg.0000189358.38427.cd. [DOI] [PubMed] [Google Scholar]
- 9.Kull I, Böhme M, Wahlgren C-F, Nordvall L, Pershagen G, Wickamn M. Breast-feeding reduces the risk for childhood eczema. J Allergy Clin Immunol. 2005;116:657–661. doi: 10.1016/j.jaci.2005.04.028. [DOI] [PubMed] [Google Scholar]
- 10.Kull I, Almqvist C, Lilja G, Pershagen G, Wickman M. Breast-feeding reduces the risk of asthma during the first 4 years of life. J Allergy Clin Immunol. 2004;114:755–760. doi: 10.1016/j.jaci.2004.07.036. [DOI] [PubMed] [Google Scholar]
- 11.Oddy WH, Sherriff J L, de Klerk N H, et al. The relation of breastfeeding and body mass index to asthma and atopy in children: a prospective cohort study to age 6 years. Am J Public Health. 2004;94(9):1531–1537. doi: 10.2105/ajph.94.9.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinmann S, Kamtsiuris P, Henke KD, Wickman M, Jenner A, Wahn U. The costs of atopy and asthma in children: assessment of direct costs and their determinants in a birth cohort. Pediatr Allergy Immunol. 2003;14:18–26. doi: 10.1034/j.1399-3038.2003.02085.x. [DOI] [PubMed] [Google Scholar]
- 13.Vork KL, Broadwin RL, Blaisdell RJ. Developing asthma in childhood from exposure to secondhand tobacco smoke: insights from a meta-regression. Environ Health Perspect. 2007 115;(10):1394–1400. doi: 10.1289/ehp.10155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoenbaum S, Gottlieb L. Algorithm based improvement of clinical quality. BMJ. 1990;301:1374–1376. doi: 10.1136/bmj.301.6765.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Black C, Peterson S, Mansfield J, Thliveris M. Using population-based data to enhance clinical practice guideline development. Med Care. 1999;37(6 Suppl):254–263. doi: 10.1097/00005650-199906001-00019. [DOI] [PubMed] [Google Scholar]
- 16.Lorenz W, Troidl H, Solomkin J, et al. Second step: testing-outcome measurements. World J Surg. 1999;23:768–780. doi: 10.1007/s002689900578. [DOI] [PubMed] [Google Scholar]
- 17.Muche-Borowski C, et al. Allergiepräventionsleitlinie. Allergo J. 2009;18:332–341. [Google Scholar]
- 18.Muche-Borowski C, et al. Allergiepräventionsleitlinie. Pädiatrische Allergologie. 2009;12:14–22. [Google Scholar]