Abstract
Background
Health-care workers are at risk of occupational exposure to influenza and can also transmit the disease to their patients.
Methods
Selective literature review and description of the influenza vaccination program at the Frankfurt University Hospital.
Results and conclusions
Many studies demonstrate that influenza vaccination for health-care workers lowers morbidity and mortality in their patients. Official immunization recommendations and free, voluntary immunization programs for health-care workers have been in existence for many years. Nevertheless, influenza vaccination rates are unacceptably low. Therefore, mandatory vaccination ought to be considered. In addition, infection-control measures (covering the mouth and nose with a mask, meticulous hand disinfection) should be rigorously observed in the hospital to prevent the nosocomial transmission of influenza and other infectious diseases. Vaccination rates might be improved if health-care workers were made aware that they themselves face a risk of infection.
Keywords: influenza, vaccination, health-care workers, nosocomial infection, prevention
During a normal influenza season around 5% to 15% of adults (1, 2) become infected with one of the prevalent influenza viruses. Among health-care workers (HCWs), up to a quarter of unvaccinated personnel are affected (2, 3). As many as three quarters of them continue working despite their illness and are thus a source of infection for unvaccinated colleagues and for patients, potentially causing nosocomial outbreaks of influenza (4).
The extent of the annual waves of influenza, the number of influenza-related hospital admissions, and the number of fatalities depends on the virus variants in circulation and on the immunization coverage in different population groups (2).
In Germany, seasonal waves of influenza result in an average of 2 to 5 million additional visits to the doctor, an estimated 10 000 to 20 000 additional hospital admissions, and approximately 10 000 deaths (5, 6). These influenza-related fatalities are often the consequence of pneumonia or exacerbation of cardiopulmonary disease and in an estimated 90% of cases involve elderly, multimorbid patients (2).
This review article describes potential ways of increasing the influenza vaccination rate of HCWs with the aim of avoiding nosocomial infections in a German university hospital center. While the discussion herein primarily concerns the classic seasonal influenza, the same considerations also apply, of course, to the recent “swine flu” epidemic.
Methods
We searched PubMed for relevant English- and German-language articles published between 1966 and March 2009. The search terms were "Healthcare workers" AND "Influenza vaccination" (80 articles), "Mask" AND "Influenza" (64 articles), and "Mandatory influenza vaccination" (41 articles). If the abstract satisfied the criteria, the complete article was included.
The search terms "Influenza vaccination" (7567 articles) and "Influenza vaccination rates" (1064 articles) were used to help answer specific questions.
Both original articles and review articles were included. We checked the reference lists of the articles for further relevant publications.
Transmission and duration of infectiousness
The influenza virus is very infectious: infected individuals begin secreting the virus via throat and nose 24 hours before the first clinical symptoms appear, in the case of children up to 48 hours before. The symptoms are often sudden in onset, coming on over a period of just a few hours or even minutes, and vary in severity—from severe systemic symptoms and feeling very ill to relatively slight respiratory manifestations. Even in mild cases, however, the virus is released in considerable amounts.
The virus is secreted for ca. 3 to 5 days in adults and older children, for 1 to 2 weeks in infants and young children, and for a number of weeks or even months in immune-suppressed individuals. Owing to the prolonged period of secretion these patients may serve as a reservoir for the influenza virus. Close monitoring is therefore required to detect any secretion of virus (2).
The incubation time for influenza infection is 1 to 3 days, while the contagion index ranges from 15% to 75% depending on the strain of virus, with 30% regarded as "normal" during an epidemic. Influenza principally spreads via airborne droplets transmitted while speaking, coughing, or sneezing, less frequently by direct intranasal inoculation (e.g., via contaminated hands). In experimentally infected volunteers the infective dose of influenza virus was 10 to 100 times lower via inhalation of small aerosol particles than via direct nasal application (e1). The nasopharyngeal lavage fluid of infected individuals evinces large quantities of virus (up to 10 million infectious viruses/mL), whereas the human infective dose (the dose at which 50% of those exposed become ill) is fewer than 3 (inhalation) or 127 to 320 infectious virus particles (intranasal inoculation).
Influenza virus particles can remain infectious for 24 to 48 hours on smooth surfaces and for up to 5 minutes on the hands (e2).
Diagnosis and principles of testing
In the acute phase of illness, particularly in the first 3 days after onset of symptoms, direct demonstration of the pathogen, e.g., by PCR, ELISA, rapid immunochromatography or virus isolation on cell culture, is the method of choice. The following materials are suitable for the detection of human influenza virus:
Nasal swabs
Nasal lavage fluid (2 mL saline solution)
Throat swabs and throat lavage fluid (the latter as last resort owing to the dilution effect).
Among other factors, the efficacy of detection is dependent on sample quality and—depending on the method used—sample transportation. The sensitivity of the (rapid) tests varies between 50% and >90%, the specificity between 70% and >95%.
If a patient does not present until over 4 to 5 days after onset of illness, demonstration of the virus (antigen) generally no longer serves any useful purpose. Antibody diagnosis (e.g., the complement binding reaction [CBR], hemagglutinin inhibition test [HIT], enzyme-linked immunosorbent assay [ELISA], or direct immunofluorescence test [IFT]) can be employed instead. However, the antibodies usually cannot be detected until 8 to 10 days after the onset of illness.
In epidemic phases, i.e., when 20% or more of the population is infected, the disease is diagnosed on the basis of the following clinical symptoms:
Acute onset
Severe feeling of illness
Temperature >38.5°C
Dry cough
Frequently biphasic course.
In such circumstances there is usually no laboratory diagnosis.
Prevention and control of infection
Annual vaccination against influenza is the most efficacious and cost-effective preventive measure for combating this disease in all age groups (7). The vaccine is a trivalent split vaccine with two influenza-A components and one influenza-B component. However, only 50% to 70% of immune-suppressed individuals, the chronically ill, and the aged are protected by the vaccination. Nevertheless, some studies show that influenza vaccination is also effective in elderly persons and in multimorbid patients (8, e3). Although the immune response of immune-suppressed patients is usually lower than in those with intact immunity, they should still be vaccinated in order to prevent serious infections (7, e4). The World Health Organization (WHO) has set the verifiable goal of a vaccination rate of 75% for the target groups—persons at risk and those over 60 years of age—by the year 2010 (7, 9, e5).
Among health-care workers, who are largely relatively young, vaccination achieves an adequate antibody titer against influenza viruses in up to 90% of cases (8, 10, e6, e7). Moreover, they visit the doctor less often (42% reduction, 95% confidence interval [CI] 9–63) and are less frequently absent from work owing to illness (8, 11).
From the point of view of hospital hygiene, patients with suspected or confirmed influenza should be isolated for at least 5 days to avoid nosocomial outbreaks. Under some circumstances it may be advisable to separate cohorts of patients infected by similar virus variants (2). Isolation of the infected means that no other patients can be accommodated in the same room; thus, beds are usually blocked.
All people who enter the room must wear a mask over their mouth and nose, a lab coat, and gloves. The patient’s freedom of movement is restricted, and all diagnostic or therapeutic procedures have to comply with the strict hygiene regulations and are thus costly and organizationally complex. Health-care workers who display symptoms typical of influenza should be sent home to avoid the risk of transmission to patients or colleagues (2).
Vaccination of health-care workers
Health-care workers are at higher risk of infection and can also transmit highly contagious influenza viruses to patients and colleagues, causing nosocomial outbreaks of influenza. Particularly in immune-suppressed patients this can lead to serious illness and even influenza-related deaths. Nosocomial influenza outbreaks have been reported from neonatology wards, intensive care units, and transplantation wards as well as general wards. The rates of infection ranged between 3% and 50% for patients, and between 11% and 59% for hospital employees (2, 12, e8, e9). Various studies have shown that up to 70% of influenza infections in organ-transplanted patients and those with acute leukemia are of nosocomial origin (e10– e12).
The most effective way of preventing nosocomial outbreaks of influenza is annual vaccination of health-care workers. The Robert Koch Institute (RKI) has recommended influenza vaccination for health-care workers since the beginning of the 1980s. In Germany, assumption of the costs by the employer is regulated by §15 of the Biostoffverordnung (Biological Agents Ordinance).
Irrespective of this, health-care workers display low acceptance of influenza vaccination, both in Germany and elsewhere. Voluntary programs rarely attain vaccination rates exceeding 50% (13– 16). In some states of the USA, however, influenza vaccination is compulsory for health-care workers. The Virginia Mason Medical Center, for example, where mandatory influenza vaccination was introduced in 2004, has achieved vaccination rates of 98% (14, e13).
Less than a third of German health-care workers have themselves vaccinated against influenza, although the vaccination is safe and effective and has been proved to prevent nosocomial outbreaks (10, 16– 18). Numerous studies demonstrate that the numbers of influenza-related illnesses (19), hospitalizations (20), and deaths (e14, e15) among elderly residents of nursing homes can be significantly reduced when just half of the nursing personnel have been vaccinated against influenza. A randomized study by Hayward et al. (10) embraced more than 1700 medical and paramedical staff and 2600 elderly patients in 44 old people’s homes and showed significant reductions in
the incidence of influenza-like infections (p = 0.004),
the frequency of medical consultations (p = 0.002),
the number of hospital admissions (p = 0.009), and
mortality (p = 0.002).
According to these authors the number of fatalities decreased by one for every eight vaccinated employees, and the number of illnesses of a home resident went down by one for every five vaccinated employees.
Motives for refusing vaccination
Several anonymous questionnaires that we distributed to the health-care workers of Frankfurt University Hospital included questions on their attitudes to influenza vaccination. Analysis of their responses showed that the HCWs had themselves vaccinated primarily to protect themselves (92.3%) and their family, friends, and colleagues (66.8%). Concern for the patients only took third place (54.5%) (15). The most frequently given reasons for not having the vaccination were:
The employees saw no specific risk for themselves (42.3%)
Fear of side effects of the vaccination (29.1%)
Not convinced that the vaccine would have an adequate protective effect (28.0%)
The assumption that "influenza is not a serious illness" (17.7%)
The opinion that "the influenza vaccination might cause influenza" (17.1%).
A higher proportion of the nursing staff (31.6%) feared side effects, whereas the doctors particularly doubted the efficacy of the vaccine (42.6%) (17).
However, our group’s data also demonstrate good overall tolerance of the influenza vaccine. Slight increases in temperature (<38.5°C) were reported by 1.6% of those questioned, and in no case did the temperature rise to >38.5°C. Headache and joint pains were reported by 8.5% of the respondents overall, but there is no adequate degree of certainty that the symptoms were caused by the influenza vaccination rather than just coincidentally occurring at the same time (17).
Face masks
The transmission of influenza viruses is generally aerogenic. The greatest proportion of the infectious viruses are found in the "large droplets" expelled by sneezing, which have a range of around 1.8 m. It is therefore not surprising that the majority of influenza infections are transmitted in overcrowded, poorly ventilated rooms.
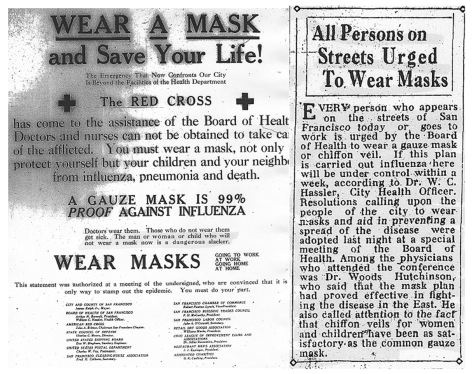
Even without this knowledge, the wearing of protective masks was recommended during the "Spanish flu" epidemic to prevent transmission of the disease. The Mayor and the Health Officer of the city of San Francisco called for all inhabitants to wear masks over their mouths from October 1918 to February 1919. The masks were supplied by the Red Cross and were assumed to provide 99% protection against influenza (San Francisco Chronicle, October 20, 1918; Figure 1). As a result, the infection and mortality rates were indeed lower there than in other parts of the USA (e16).
Figure 1: An article on the wearing of masks printed in the San Francisco Chronicle on October 20, 1918, together with the associated Red Cross appeal to the population
In light of the changes in resistance to the neuraminidase inhibitors zanamivir and oseltamivir, the wearing of protective masks remains an effective means of avoiding transmission of infection and preventing nosocomial outbreaks of influenza (21). In the 2007/2008 influenza season, 24.3% of the influenza A (H1N1) isolates in Europe proved to be resistant to oseltamivir but sensitive to zanamivir (www.eiss.org/documents/antiviral/CNRL_antiviral_resistance_H1N1_update_24-09-2008_12-06.pdf [e17]), while in the 2008/2009 influenza season 98.5% of influenza A viruses (H1N1) in the USA were resistant to oseltamivir (22). It was also shown that compulsory mask wearing for unvaccinated health-care workers significantly increased the vaccination rate among the HCWs (23).
The first patients with influenza were admitted to Frankfurt University Hospital on January 7, 2009. On January 9, laboratory tests confirmed further infections in immune-suppressed patients. In view of the prevailing epidemiological circumstances, with reports of high influenza activity (Portugal: penultimate week of 2008; Ireland: first week of 2009; Switzerland: second week of 2009) (e17), the hospital authorities made the wearing of a surgical mask compulsory for all non-vaccinated employees whose work brought them into direct contact with patients. The intention was to break chains of infection within the hospital complex.
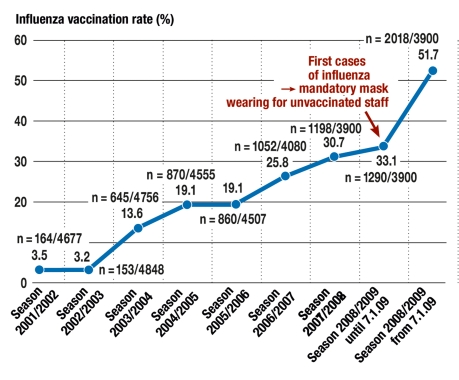
Within 10 days of its introduction, mandatory mask wearing increased the vaccination coverage from 33% (n = 1290/3900) to 51.7% (n = 2018/3900) (p<0.000001, chi-square test 278.2). This was the most effective means of increasing the vaccination rate in a 6-year vaccination program (figure 2). Doctors showed the highest acceptance of vaccination throughout the program, and in 2008/2009 their vaccination rate was 95.4%. The vaccination rate among the nursing staff in 2008/2009, at 49.6%, was also very high in comparison with other centers in Germany.
Figure 2.
The influenza vaccination rate at Frankfurt University Hospital, Frankfurt am Main, Germany. Measures to increase the vaccination rate began in the influenza season 2003/2004. Since January 7, 2009, unvaccinated workers in direct contact with patients have to wear a mask. (modified from [23])
Despite these good vaccination rates, health-care workers’ reasons for deciding whether to be vaccinated or not require clarification. The decision for vaccination seems not to be based on facts (influenza vaccination is safe and effective), but is taken under the pressure of compulsory protective measures (mandatory mask wearing) and the resulting "inconvenience," or the fear of infection in an acute outbreak.
Nevertheless, sufficient herd immunity against influenza is required in health-care workers to protect endangered patients and avoid transmission of infection in other HCWs (e18). To this end, at least 50% of them need to be vaccinated (15, 24). Mathematical calculations go still further and demonstrate that every additional vaccination of a health-care worker results in greater protection for patients; for this reason, an increase of the vaccination rate from 80% to 90% is just as important as an increase from 10% to 20%. The underlying mathematical model shows a linear relationship between the proportion of vaccinated employees and the expected number of cases of influenza among the patients. No threshold value could be found for herd immunity: even if employees’ vaccination rates are high, stochastic effects can still lead to nosocomial outbreaks of infection (25).
Since adequate vaccination rates seemingly cannot be achieved by means of voluntary programs, despite exhaustive public awareness measures, compulsory vaccination should be considered for employees responsible for the care of immune-suppressed patients (13, e19– e25).
The ethical obligation to cause no harm to others—in this context, not to transmit influenza—outweighs the relatively minor risk of adverse effects from the influenza vaccination (e26).
Key messages.
A multifunctional approach is needed to increase the low influenza vaccination rate among health-care workers.
Continual, sustained action is required to focus attention on the importance of influenza vaccination for health-care workers. Important roles can be played by public bodies such as the Robert Koch Institute and the public health service, by hospital administrators and employers, e.g., the German Hospital Association, and by professional associations, such as the German Society for Hygiene and Microbiology, the German Society for Hospital Hygiene, The German Association for Combating Viral Diseases, and the German Society for Occupational and Environmental Medicine.
The introduction of measures such as compulsory mask wearing by unvaccinated personnel during influenza epidemics and mandatory vaccination of those responsible for the care of immune-suppressed patients should be considered.
Acknowledgments
Translated from the original German by David Roseveare.
Footnotes
Conflict of interest statement
Professor Kempf has received reimbursement of travel costs from Bayer Health Care. The remaining authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Watson R. Vaccinate people at risk and healthcare workers against flu, says European public health office. BMJ. 2009;338 doi: 10.1136/bmj.b127. [DOI] [PubMed] [Google Scholar]
- 2.Salgado CD, Farr BM, Hall KK, Hayden FG. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2:145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 3.Elder A, O’Donnell B, McCruden E, Symington I, Carman W. Incidence and recall of influenza in a cohort of Glasgow healthcare workers during the 1993-4 epidemic: results of serum testing and questionnaire. BMJ. 1996;313:1241–1242. doi: 10.1136/bmj.313.7067.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weingarten S, Riedinger M, Bolton L, Miles P, Ault M. Barriers to influenza vaccine acceptance: a survey of physicians and nurses. Am J Infect Control. 1989;17:201–207. doi: 10.1016/0196-6553(89)90129-6. [DOI] [PubMed] [Google Scholar]
- 5.Robert Koch-Institut (RKI) Influenza RKI-Ratgeber Infektionskrankheiten - Merkblätter für Ärzte. Stand 18.2.2008. Ladbar unter: www.rki.de/cln_091/nn_200120/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_Mbl_Influenza.html Last accessed on 17 April 2009. [Google Scholar]
- 6.Szucs TD, Wahle K, Müller D. Grippeimpfung in Deutschland. Eine bevölkerungsbezogene Querschnittsanalyse der drei Influenzasaisons. Med Klin. 2006;101:537–545. doi: 10.1007/s00063-006-1076-y. [DOI] [PubMed] [Google Scholar]
- 7.Wutzler P. Influenza-Schutzimpfung - Wo steht Deutschland? Dtsch Med Wochenschr. 2006;131:453–457. doi: 10.1055/s-2006-932543. [DOI] [PubMed] [Google Scholar]
- 8.Nichol KL. Efficacy and effectiveness of influenza vaccination. Vaccine. 2008;26S:D17–D22. doi: 10.1016/j.vaccine.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 9.Mereckiene J, Cotter S, Nicoll A, et al. National seasonal influenza vaccination survey in Europe, 2008. Euro Surveill. 2008;13(43) doi: 10.2807/ese.13.43.19017-en. [DOI] [PubMed] [Google Scholar]
- 10.Hayward AC, Harling R, Wetten S, et al. Effectiveness of an influenza vaccine programme for home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333(7581) doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nichol KL, S’Heilly SJ, Greenberg ME, Ehlinger E. Burden of influenza-like illness and effectiveness of influenza vaccination among working adults aged 50-64 year. CID. 2009;48:292–298. doi: 10.1086/595842. [DOI] [PubMed] [Google Scholar]
- 12.Apisarnthanarak A, Puthavathana P, Kitphati R, Auewarakul P, Mundy LM. Outbreaks of influenza A among nonvaccinated healthcare workers: implications for resource-limited settings. Infect Control Hosp Epidemiol. 2008;29:777–780. doi: 10.1086/588162. [DOI] [PubMed] [Google Scholar]
- 13.Poland GA, Tosh P, Jacobson RM. Requiring influenza vaccination for health care workers: seven truths we must accept. Vaccine. 2005;23:2251–2255. doi: 10.1016/j.vaccine.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 14.Talbot TR. Improving rates of influenza vaccination among healthcare workers: educate; motivate; mandate? Infect Control Hosp Epidemiol. 2008;29:107–110. doi: 10.1086/527573. [DOI] [PubMed] [Google Scholar]
- 15.Wicker S, Doerr HW, Gottschalk R, Rabenau HF, Allwinn R. Influenza: Akzeptanz der Schutzimpfung bei medizinischem Personal - Auswertung zur Influenzasaison 2006/2007. Dtsch Med Wochenschr. 2007;132:1683–1687. doi: 10.1055/s-2007-984949. [DOI] [PubMed] [Google Scholar]
- 16.Müller D, Wutzler P, Szucs TD. Influenza vaccination coverage rates in Germany a population-based cross-sectional analysis of the seasons 2002/2003 and 2003/2004. Med Klin. 2005;100:6–13. doi: 10.1007/s00063-005-1113-2. [DOI] [PubMed] [Google Scholar]
- 17.Wicker S, Rabenau HF, Doerr HW, Allwinn R. Influenza vaccination compliance among health care workers in a German university hospital. Infection. 2008 doi: 10.1007/s15010-008-8200-2. doi: 10.1007/s15010-008-8200-2. [DOI] [PubMed] [Google Scholar]
- 18.Poland GA, Jacobson RM. Protection patients from harm. Legislating vaccinations for healthcare workers. Am J Prev Med. 2007;32:544–545. doi: 10.1016/j.amepre.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 19.Wang CS, Wang ST, Lai CT, Lin LJ, Chou P. Impact of influenza vaccination on major cause-specific mortality. Vaccine. 2007;25:1196–1203. doi: 10.1016/j.vaccine.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 20.Nichol KL, Nordin J, Mullooly J, Lask R, Fillbrandt KM. Influenza vaccination and reduction in hospitalizations for cardiac disease and stroke among the elderly. N Engl J Med. 2003;348:1322–1332. doi: 10.1056/NEJMoa025028. [DOI] [PubMed] [Google Scholar]
- 21.Jefferson T, Foxlee R, Del Mar C, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2008;336:77–80. doi: 10.1136/bmj.39393.510347.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dharan NJ, Gubareva LV, Okomo-Adhiambo M, et al. Infections with Oseltamivir-resistant influenza A(H1N1) virus in the United States. JAMA. 2009 doi: 10.1001/jama.2009.294. published online Mar 2, DOI:10.1001/jama.2009.294. [DOI] [PubMed] [Google Scholar]
- 23.Wicker S. Unvaccinated health care workers must wear masks during flu season—A possibility to improve influenza vaccination rates? Vaccine. 2009;27:2631–2632. doi: 10.1016/j.vaccine.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 24.van Delden JJ, Ashcroft R, Dawson A, Marckmann G, Upshur R, Verweij MF. The ethics of mandatory vaccination against influenza for health care workers. Vaccine. 2008;26:5562–5566. doi: 10.1016/j.vaccine.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 25.van den Dool C, Bonten MJM, Hak E, Heijne JCM, Wallinga J. The effects of influenza vaccination of health care workers in nursing homes: Insights from a mathematical model. PLoS Med. 5(10) doi: 10.1371/journal.pmed.0050200. doi:10.1371/journal.pmed.0050200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e1.Alford R, Kasel J, Gerome P, Knight V. Human influenza resulting from aerosol inhalation. Proc Soc Exp Biol Med. 1966;122:800–804. doi: 10.3181/00379727-122-31255. [DOI] [PubMed] [Google Scholar]
- e2.Bean B, Moore BM, Sterner B, Peterson LR, Gerding DN, Balfour HH., Jr Survival of influenza viruses on environmental surfaces. J Infect Dis. 1982;146:47–51. doi: 10.1093/infdis/146.1.47. [DOI] [PubMed] [Google Scholar]
- e3.Nichol KL. Influenza vaccination in the elderly. Impact on hospitalization and mortality. Drugs Aging. 2005;22:495–515. doi: 10.2165/00002512-200522060-00004. [DOI] [PubMed] [Google Scholar]
- e4.Robert Koch-Institut (RKI) Mitteilung der Ständigen Impfkommission (STIKO) am RKI: Hinweise zu Impfungen für Patienten mit Immundefizienz. Epidemiologisches Bulletin. 2005;39 [Google Scholar]
- e5.World Health Organization (WHO) Resolution of the World Health Assembly (WHA 56.19). Prevention and control of influenza pandemics and annual epidemics. WHA 10th plenary meeting. 2003 May 28; Ref Type: Bill/resolution. [Google Scholar]
- e6.Pearson ML, Bridges CB, Harper SA. Influenza vaccination of health-care personnel. MMWR. 2006;55:1–16. [PubMed] [Google Scholar]
- e7.Nichol KL, Lind A, Margolis KL, et al. The effectiveness of vaccination against influenza in healthy, working adults. N Engl J Med. 1995;333:889–893. doi: 10.1056/NEJM199510053331401. [DOI] [PubMed] [Google Scholar]
- e8.Malavaud S, Malavaud B, Sandres K, et al. Nosocomial outbreak of influenza A (H3N2) infection in a solid organ transplant department. Transplantation. 2001;72:535–537. doi: 10.1097/00007890-200108150-00032. [DOI] [PubMed] [Google Scholar]
- e9.Cunney RJ, Bialachowski A, Thornley D, Smaill FM, Pennie RA. An outbreak of influenza A in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2000;21:449–454. doi: 10.1086/501786. [DOI] [PubMed] [Google Scholar]
- e10.Mauch TJ, Bratton S, Myers T, Krane E, Gentry SR, Kashtan CE. Influenza B virus infection in pediatric solid organ transplantant recipients. Paediatrics. 1994;94:225–229. [PubMed] [Google Scholar]
- e11.Whimbey E, Elting LS, Couch RB, et al. Influenza A infections among hospitalized adult bone marrow transplantant recipients. Bone Marrow Transplant. 1994;13:437–440. [PubMed] [Google Scholar]
- e12.Aschan J, Ringdén O, Ljungman P, Andersson J, Lewensohn-Fuchs I, Forsgren M. Influenza B in transplantant patients. Scand J Infect Dis. 1989;21:349–350. doi: 10.3109/00365548909035710. [DOI] [PubMed] [Google Scholar]
- e13.Rusk J. Mandatory flu shots boost health care worker immunization rate at Virginia Mason. Infectious Disease News March. 2006 Available at: http://www.infectiousdiseasenews.com/200603/mandatory.asp. Last accessed on 24 March 2009. [Google Scholar]
- e14.Carman WF, Elder AG, Wallace LA. Effects of influenza vaccination of health-care workers on mortality of elderly people in long-term care: a randomised controlled trial. Lancet. 2000;355:93–97. doi: 10.1016/S0140-6736(99)05190-9. [DOI] [PubMed] [Google Scholar]
- e15.Potter J, Stott DJ, Roberts MA, et al. Influenza vaccination of health care workers in long-term-care hospitals reduces the mortality of elderly patients. J Infect Dis. 1997;175:1–6. doi: 10.1093/infdis/175.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e16.Witte W. Tollkirschen und Quarantäne. Wagenbachverlag Berlin. 2008 [Google Scholar]
- e17.European Influenza Surveillance Scheme: EISS-Weekly Electronic Bulletin Week 2: 05/01/2009-11/01/2009. Available at: www.eiss.org, last accessed on 24 March 2009. [Google Scholar]
- e18.Glezen WP. Herd protection against influenza. J Clin Virol. 2006;37:237–234. doi: 10.1016/j.jcv.2006.08.020. [DOI] [PubMed] [Google Scholar]
- e19.Anikeeva O, Braunack-Mayer A, Rogers W. Requiring Influenza vaccination for health care workers. Am J Public Health. 2009;99:24–29. doi: 10.2105/AJPH.2008.136440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e20.Greene LR, Cain TA, Dolan SA, et al. APIC Position Paper: Influenza immunization of healthcare personnel. Available at: http://www.apic.org/AM/Template.cfm?Section=Home1&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTFILEID=11049. Last accessed on 24 March 2009. [Google Scholar]
- e21.McLennan S, Gillett G, Celi LA. Healer, heal thyself: Health care workers and the influenza vaccination. Am J Infect Control. 2008;36:1–4. doi: 10.1016/j.ajic.2007.07.010. [DOI] [PubMed] [Google Scholar]
- e22.Tilburt JC, Mueller PS, Ottenberg AL, Poland GA, Koenig BA. Facing the challenges of influenza in healthcare settings: The ethical rationale for mandatory seasonal influenza vaccination and its implications for future pandemics. Vaccine. 2008;26S:D27–D30. doi: 10.1016/j.vaccine.2008.07.068. [DOI] [PubMed] [Google Scholar]
- e23.Helms CM, Polgreen PM. Should influenza immunisation be mandatory for healthcare workers? Yes. BMJ. 2008 doi: 10.1136/bmj.a2142. [DOI] [PubMed] [Google Scholar]
- e24.Steckel CM. Mandatory influenza immunization for health care workers - an ethical discussion. AAOHN J. 2007;55:34–39. doi: 10.1177/216507990705500105. [DOI] [PubMed] [Google Scholar]
- e25.Tucker SJ, Poland GA, Jacobson RM. Requiring influenza vaccination for health care workers. AJN. 2008;108:32–34. doi: 10.1097/01.NAJ.0000310328.47809.d4. [DOI] [PubMed] [Google Scholar]
- e26.Marckmann G. Impfprogramme im Spannungsfeld zwischen individueller Autonomie und allgemeinem Wohl. Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2008;51:175–183. doi: 10.1007/s00103-008-0448-2. [DOI] [PubMed] [Google Scholar]