Abstract
Background
The challenge of understanding factors influencing compliance with injectable treatments is critical as injectable biologics/medications become more common.
Objective
Understanding compliance issues for long term self-injectable treatments, using a chronic condition (osteoporosis) as a model.
Research design
A qualitative study to generate hypotheses regarding compliance issues for self-injectable treatments. Semi-structured interview guides were developed and data collected from patients and clinical experts. Findings were analyzed for common themes and a conceptual model of the compliance impact of self-injectable treatments generated.
Subjects
Six physicians (Rheumatology, Internal Medicine, and Endocrinology) and 22 patients (14% never began treatment, 23% had filled at least one prescription but discontinued treatment, and 63% were currently on treatment) were interviewed.
Results
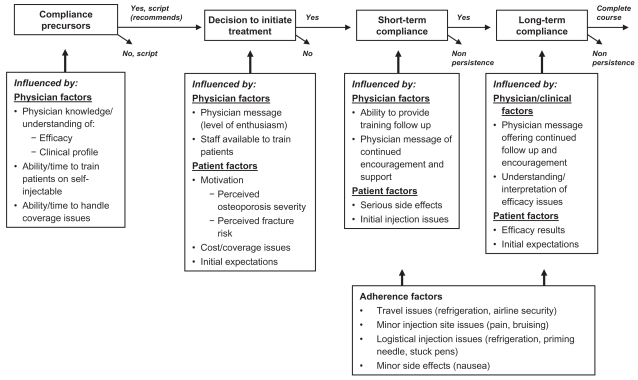
Physician and patient factors influenced the compliance process at four distinct time-points: pre-treatment, time treatment recommended, short-term, and long-term. Physician factors that influenced patients’ persistence were knowledge about treatment, patient-training resources, and clinical profile/efficacy evaluations. For patients, motivation level, physician message, and clinical profile were key. Logistical issues, minor side effects and injection site issues influenced adherence but not persistence.
Conclusions
Compliance is a multifactorial, dynamic process. Both physician and patient factors influence compliance at different points in the process.
Keywords: osteoporosis, self-injectable treatments, compliance, persistence, adherence
Introduction
The study of patient behavior regarding the taking of medications is not new (Dunbar-Jacobs et al 2001) and has been called compliance and more recently adherence and/or persistence. For the purpose of this study, we have defined “compliance” as having two components: treatment persistence (continuing on treatment for the recommended duration) and adherence (taking treatment as prescribed, ie, the correct time of day or number of times per day). However labeled, there is little doubt that taking medication as prescribed and for the recommended time period is problematic for many patients and has significant effects on health care outcomes and cost of care (Dunbar-Jacobs et al 2001; Piette et al 2004; Robiner 2005). A meta-analysis of 569 studies of adherence to treatment found the average nonadherence rate to be 24.8% (DiMatteo 2004) and the overall difference between high and low adherence has been shown to be 26% (DiMatteo et al 2002). For persons with chronic disorders, as many as 60% may be poorly adherent to their prescribed medication (Dunbar-Jacobs et al 2001). Both low persistence and adherence rates limit the benefits of medical treatments (Haynes et al 1996), impact the efficacy profile of a drug (Leo et al 2005), and present a challenge to prescribing physicians and their patients.
The literature on compliance is extensive and addresses key issues of theory, factors that influence compliance and interventions to improve compliance (For reviews of the literature: Ryan 1999; Dunbar-Jacobs et al 2001; DiMatteo et al 2002; McDonald et al 2002; Peterson et al 2003; DiMatteo 2004). The factors that influence compliance are generally considered to be multivariate in nature and include patient characteristics, knowledge and beliefs about their illnesses as well as patient’s disease and treatment modality (DiMatteo 2004; Schwartzman et al 2004; Leo et al 2005). Factors such as patients’ self-efficacy (Fraser et al 2001), ethnicity, and number of daily prescribed pills (Graveley et al 1991), perceived severity of illness (Roberson 1992), complexity of regimen (DiMatteo et al 1982), and cost (Piette et al 2004) have all been found to play a role in compliance. For example, compliance with oral osteoporosis medications has been associated with patients’ recognition of the serious consequences of nonadherence, weighting of risks and benefits and doubts about physicians’ competence to prescribe appropriate drugs (Unson et al 2003). Compliance has been found to be largely unaffected by age or demographic factors alone, although the data are sometimes contradictory (Ryan 1999; DiMatteo 2004). Little attention has been paid to the role of the physician in influencing compliance.
The challenge of understanding factors that influence compliance with injectable treatments in a primary care setting has become more critical as newer injectable biologics and medications for chronic illness prescribed in the primary care setting become more common (Mohr et al 2002). For injectable treatments, self injection is associated with better compliance than injection by a family member or by health professionals (Mohr et al 2002). Unfortunately, factors that influence compliance with self-injectable treatments are less well studied; although we do know that of women using a self-injectable treatment for contraception, only 42% are compliant at the end of one year and that side effects are cited as the main reason for treatment discontinuation (Beksinska et al 2001). In patients with multiple sclerosis, patients’ self-efficacy, attitudes toward the disease and the treatment, sense of hope, perception of the physician as supportive as well as the interaction between the patient and the healthcare team strongly influence compliance with daily self-injectable treatments (Fraser et al 2001; Schwartzman et al 2004). For diabetics, daily injectable insulin regimes may be viewed as burdensome, although this burden appears to be attenuated by experience (Vijan et al 2005).
The purpose of this qualitative study was to further our understanding of adherence and persistence issues for self-injectable treatments in a primary care setting, primarily from the patient perspective. To do this, we conducted individual or focus group interviews with patients for whom self-injectable treatments were prescribed. However, given that patients do not begin or continue on treatment without interactions with physicians, a limited number of individual interviews with physicians who prescribed self-injectable treatments (for patients other than those in the study sample) were also conducted. Based on the data gathered, a conceptual model of compliance for daily self-injectable treatments was developed. Teriparatide (Forteo®; Eli Lilly and Company, Indianapolis, IN, USA), a daily self-injectable treatment for osteoporosis, a condition diagnosed primarily in post-menopausal females, was used as the prototype therapy condition for the study.
Methods
Data collection
First, the relevant peer-reviewed journal literature on osteoporosis, self-injectable treatment and compliance was reviewed to identify potential issues that may influence compliance from both the patient and the physician’s perspective. Based on this review, two semi-structured interview guides regarding compliance issues for a daily self-injectable treatment were developed: one tailored for physicians who prescribed teriparatide, and one tailored for patients who were prescribed teriparatide. The patient interview guide asked about their expectations regarding a self-injectable treatment prior to initiating the treatment, the education/training they received, factors they believed affected their daily use of medication as prescribed, continued use over time, reasons for discontinuation, and any mediating factors which might have influenced their treatment behaviors. The physician interview guide asked similar questions and asked the physician to respond according to both how they felt about these issues as well as how they perceived that their patients felt. All interviews were conducted by the same trained professional. Ethics committee approval was obtained for the study and patients gave informed consent.
Sample
To identify the patient sample, physicians who had experience with teriparatide were identified from an Information Management System (IMS) database of physicians who had prescribed teriparatide or were known to the authors as treating osteoporosis as a major component of their practice. The physicians identified were contacted by the first author, starting with those physicians who had the greatest experience with prescribing teriparatide in each of 3 specialties (Rheumatology, Endocrinology, and Internal Medicine), were from varied geographic areas and were both academic and community-based physicians. Physicians were asked to participate in the study by identifying and recruiting, from their patient populations, a sample of three groups of patients: 1) those that had been recommended teriparatide but had chosen not to initiate treatment, 2) those that initiated treatment but did not complete the recommended course of treatment, or 3) individuals who initiated treatment and were currently on teriparatide. These patients were interviewed following the discussion guide in either an individual telephone interview (lasting approximately one hour) or in a focus group setting (lasting approximately three hours). The focus groups were audio-taped and transcribed. Each physician was then individually interviewed by telephone for approximately one hour following the semi-structured interview guide.
Data analysis
The qualitative data (transcripts, written notes) from both the physicians and the patients were analyzed by the first author for commonality of concepts regarding compliance issues. These commonalities were grouped into themes which were then categorized as important for either adherence or persistence and for when in the treatment process they exerted their influence (ie, start of treatment, during treatment). Based on the common themes, a conceptual model of the impact of treatment on compliance was developed.
Results
Sample
Twenty-two patients (21 women, 1 man), age range 42–88 years old (mean age 72), were interviewed. Eight of these patients were interviewed individually by telephone and 14 participated in one of two focus groups (Florida or Cleveland). The mean length of time with osteoporosis was nine years and most (55%) felt their condition was severe, they had suffered a previous fracture (68%) or considered themselves at risk for a future fracture (77%). Three (14%) of the subjects (2 women, 1 man) never began treatment with teriparatide even though their physicians recommended or prescribed it. Five (23%) of the woman filled at least one prescription but discontinued sometime during the course of treatment, and 14 (63%) of the woman were currently on treatment. Half of the sample was either married (41%) or had a partner (9%) and half were widowed (36%), divorced (9%) or single (5%). The majority were Caucasian (90%) with an average household income (59%) of US$20,000 to $60,000.
Six physicians, located in San Francisco, Cleveland, New York, and Florida, were interviewed. The physicians were practicing in the specialties of Rheumatology (2), Internal Medicine (2), and Endocrinology (2). Two physicians practiced in an academic setting and the remaining four practiced in a community setting. These experts had practiced an average of 19 years (range 5–30) and wrote an average of 20 teriparatide prescriptions a year (range 4–45).
Conceptual model
Based on the findings from the physician and patient interviews, a conceptual model of compliance with a self-injectable medication was developed (Figure 1).
Figure 1.
Compliance process.
Precursor factors influencing compliance
Physician knowledge about teriparatide was the key factor that determined whether or not the physician prescribed teriparatide and, if so, how the treatment was presented to the patient. This knowledge was shaped by their beliefs about the efficacy of the treatment, comfort with the available clinical data and their assessment of severity and incidence of side effects. The self-reported level of knowledge regarding teriparatide varied among physicians and several desired additional information on the efficacy and/or long-term safety data. There was also some confusion over the appropriate treatment after patients completed the recommended 18–24 month treatment course. These types of issues contributed to their hesitancy in prescribing the treatment. Physicians commented that “I don’t prescribe [this drug] because … it may be a short-term fix for this population … not convinced by data as N is too small.”
A second factor that influenced physicians’ decision to recommend teriparatide was their ability and/or resources to train the patients on a self-injectable medication. As one physician stated, “This drug requires more explanation and time for an office … a busy doctor may not have the patience or time that is needed to prescribe. Specialists can spend more time.” Additionally, issues regarding reimbursement and coverage were not clearly understood by physicians. Cost was considered an obstacle to prescribing as some offices did not have the resources to advocate coverage assistance for patients. In spite of these barriers to prescribing, physicians who did recommend teriparatide felt enthusiastic about the treatment as they gained more experience with the product.
Decision to initiate treatment
Both physicians and patients agreed that the patient’s motivation (based on perception of severity of their osteoporosis, previous fracture history, fear of future fractures, and/or availability of alternative treatments) was a key factor influencing a patient’s decision to begin treatment and remain treatment-persistent. As one physician commented, “Those who stay on it [teriparatide] have either experienced pain of fracture or are fearful of bone health in the future and so are very motivated … (they) are looking over the cliff and know that they don’t have enough bone to continue.” This sentiment was also often expressed by patients who felt that, “If you think your osteoporosis is bad enough, you’ve had some fractures … you try anything.” Patients weighed the potential risk of treatment (ie, teriparatide has a black box warning that in rat studies there is a duration and exposure relationship of therapy and bone sarcoma) against the benefits of treatment (ie, reduction in the risk of facture). Patients indicated they were more willing to accept the potential risks if they were highly motivated and had initial expectations of successful treatment.
The physician’s message to the patient and their level of enthusiasm for the treatment was another key factor influencing whether or not the patient accepted the treatment suggestion. One endocrinologist, who considered herself very familiar with the drug and wrote between 40–50 prescriptions a year felt that the “average doc does not know the data and can’t be passionate about it … (and this greatly influenced prescribing patterns).” Finally, cost could also be a major deterrent to patients starting treatment if they could not arrange payment coverage from their health care insurer or did not believe they could access the company-funded patient assistance program.
Both patients and physicians felt that patient fear of injection or having a previous negative experience with self injection were not major deterrents to accepting treatment, especially after patients saw the injection pen. One of the physicians commented, “I use the demo pen for the first time and show them exactly how to do it … this really helps. If (patient) decides to go on then we schedule a real training … makes a difference.” However, the absence of adequate staff or resources to train patients was problematic for many offices.
Factors influencing short-term compliance (the first month of treatment)
Patients agreed that the first month of treatment was a critical time frame for resolving factors that determined whether or not they remained on treatment and that simply receiving the prescription without continued encouragement and support was problematic. Physicians agreed that this support was important. As one endocrinologist emphasized, “Doctors must work with patients to get them to follow through (with a self-injectable treatment). This is not just writing a script.”
Problems with self-injecting that occurred within the first few weeks of starting treatment could be ameliorated by the physician or their staff. Most patients who were given this support were able to work through their difficulties. However, the ability to provide adequate training or follow-up support to patients varied among offices. Offices that had one-on-one training where patients practiced self injecting in the office and/or had a protocol where a patient was followed up soon after starting treatment reported fewer compliance issues than in offices with poorer self-injection training and little or no follow up. The optimal training scenario seemed to be one described by one of the physicians, “(we) have a clinical protocol to teach technique … then (we) call the patient a few days later to see how they are doing … a high percentage of patients have contact with the office within the first week. Then everyone is brought back at three months … (we) don’t spend a lot of time but if they have technical problems with (the) shot … they go to the nurse to address … seems to make a difference.” Additionally, written and visual instructions helped women gain proper experience and confidence when injecting at home for the first few times. One patient commented, “It took me a while to get the steps going. Every time I did it I’d have to take out the instructions and read them … And I think it was like three or four weeks before I didn’t need that paper anymore. And I just used it to make sure I got it right. And then one day I’d forgotten the paper and just did it. So I said, ‘well, I can do it now.’ But it did take a while, because I think it’s kind of stressful.” Most patients agreed that after about a month of self-injection they became much more confident and comfortable with the injection process.
The most common reasons for stopping treatment in the first few weeks were side effects such as severe rash or dizziness. Both patients and physicians agreed that this was a sufficient reason to end treatment without further interventions. Nonserious side effects did not impact compliance. For example, as one patient commented, “So after you’ve spent six weeks in a hospital because of [a] fracture … you’re willing to do most anything to avoid that again. [Being] a little nauseous in the middle of the night is nothing like being in the hospital for close to two months.”
Factors influencing long-term persistence (from one month to end of recommended treatment)
Long-term persistence was most strongly influenced by perceived treatment efficacy over time. For some patients, efficacy was judged by their experience. As one patient said, “If I fall now, I don’t break anything … before that I had broken wrists.” Others evaluated efficacy by a repeat test for bone mineral density (BMD). As one patient noted, “What I’m unhappy about is the fact that after taking it for seven months … it showed absolutely no change … So my plan is to stop it … For that much money I wanted to see at least some kind of change, and there wasn’t really anything.”
Patients’ decision to stay on treatment after poor BMD results or a new fracture experience was tempered by their initial expectations of the drug. Those who expected a “miracle cure” were more likely to be disappointed and discontinue treatment. A common sentiment was, “once you take [the drug] it’s supposed to fix everything … you know, everything will go back into place.” An initial enthusiastic physician message sometimes backfired when extreme efficacy expectations were not met. As one patient put it, “[My] physician said, ‘I’m so thrilled because we’re now going to accomplish something and hopefully you’re not going to break any more ribs.’ He was really excited about it and anxious to start on it. He really thought it was going to be great and I wouldn’t have so many breaks and [that] we had finally found an answer to this. And it didn’t turn out that way.” In contrast to this, another patient, who had not seen any improvement on a previous treatment, was simply happy to have another option. In spite of “injections sometimes hurtful … [and] occasional reactions …. [felt that] I’m still handling it” and intended to stay on treatment.
Factors influencing adherence
Of those women who continued on treatment, most felt that they were very adherent (more than 95% of time as prescribed). Many patients experienced occasional bruising or pain from injections, minor side effects or difficulties using the injection pen over the course of their treatment. Concerns about proper injection procedure (priming the pen properly, refrigeration issues and travel issues) continued over time. These difficulties were viewed as inconveniences rather than factors determining persistence. However, this did not impact adherence. For example, one patient noted, “I bruise easily … probably get a bruise every 10 times that I give it [to myself]. No, I would not consider stopping it … it is not a big deal.” Concerns and difficulties with traveling with teriparatide (refrigeration issues, carrying the pen through security) were common and also impacted adherence. Many patients commented that, “When I travel … I was out of my routine … so I forgot it … [or] because I don’t want to have to deal with it.” These problems generally did not get addressed with a health care professional due to limited physician follow up after initiating treatment or patient reluctance to bring up these perceived “minor” problems or worries to their physician.
Discussion
This study found that both physician and patient factors influence the compliance process and that there are four distinct decision points that influence compliance behavior: pre-initiation of treatment, at the time treatment is recommended to the patient, the short-term period (the first month of treatment) after a prescription is given and in the long term. Of note is that the first decision point actually occurs even before the patient is seen by the physician and is influenced by the physician’s beliefs and knowledge about the treatment. These pre-initiation of treatment factors influence how treatment is presented to the patient and helps “set the stage” for future patient compliance behaviors and attitudes. Thus, these precursor factors should be considered in understanding the broader factors which influence patient compliance over time. When the treatment is discussed with the patient, it is this degree of physician comfort with the treatment that will determine the “enthusiasm” by which the treatment option is presented to the patient. This initial message to the patient will, in turn, strongly influence the patient’s decision as to whether she or he actually accepts and fills the prescription and remains treatment persistent.
The key patient factors that were found to influence the decision to initiate treatment were patient motivation and initial expectations about treatment. Once treatment was initiated, the key patient factor influencing compliance in the short term was the training given to the patient for self injecting and/or the occurrence of serious side effects. Serious side effects were generally not an influence in the long term. After approximately the first month of treatment, the next critical decision point affecting persistence occurred once treatment effectiveness could be evaluated. Patients who did not see a significant improvement felt very discouraged and were more likely to discontinue treatment despite encouragement from their physicians. In general, short-term persistence was heavily influenced by physician factors whereas long-term persistence was heavily influenced by patient factors.
Factors that influenced adherence were different than those that influenced persistence. “Convenience factors,” such as ease of travel with the medication and minor injection site issues, continued to affect compliance behavior over the course of treatment.
Influential factors were not constant over the course of treatment. Thus, compliance should be considered a dynamic (constantly changing), ongoing process with different factors influencing adherence and persistence and at different points in the process. Just as other studies have found variable compliance rates depending upon the definition used and/or the method of assessing compliance (Dunbar-Jacob et al 2001; DiMatteo et al 2002; DiMatteo 2004), so will differences in factors influencing compliance vary by where in the time course of treatment they are examined and whether it is persistence or adherence that is of issue. Interventions to improve compliance should address all of the social factors, regimen characteristics and system issues (Robiner 2005) that were identified in this study. By understanding the dynamic and interacting nature of these factors, more targeted interventions can be developed to help improve compliance with the increasing number of self-injectable treatments.
The perception that the physician is supportive and knowledgeable of the treatment has been found to be one of the significant predictors of compliance in a chronic disease such as osteoporosis (Fraser et al 2001; Unson et al 2003), as well as for psychiatric treatments (Bourgeois 2005; Leo et al 2005). This study confirmed the important role that physicians/health care providers play in influencing both adherence and persistence. The physician/health care provider message, including level of enthusiasm for the treatment, played a key role in determining if the patient would initially accept the treatment or remain persistent in the first few weeks. This physician message was in turn highly influenced by the physician’s comfort with the treatment and knowledge about its efficacy. For a new treatment just becoming available, particular attention should be given to educating and informing physicians as to the potential of the treatment, including its limitations. Uninformed or ill-informed health care providers may unintentionally provide a “less than enthusiastic” or an “overly inflated expectation” message to their patients regardless of the efficacy of a new treatment. Physician enthusiasm which sets unrealistic high patient expectations may have contributed to some patients being discouraged with the degree of their long-term improvement and resulted in premature treatment discontinuation.
A major predictor of adherence may be the patient’s perception of the burden of treatment (Vijan et al 2005). Contrary to some common wisdom, patients’ fear of self injection was not found to be a major burden in either persistence or adherence. This finding is supported by similar findings with self-injectable treatments for diabetes, where the greatest number of barriers to adherence was in the dietary and exercise realms rather than with insulin injection (Glasgow et al 1986). Also of interest was the finding that many of these patients did not know how to properly evaluate the efficacy of the treatment and were disillusioned with the treatment when their expectations of benefit were not met. This is particularly problematic for a condition like osteoporosis where markers of long-term benefit are sometimes confusing as lumbar spine BMD has been found to be a poor predictor of vertebral fracture risk after treatment (Cummings et al 2002; Sarkar et al 2004). This may also present a problem for other chronic conditions where self injection is common. For example, multiple sclerosis patients may confuse the relapsing-remitting nature of a disease with lack of treatment efficacy. Similarly for diabetics, the absence of current complications which may take many years to manifest may be confused with treatment success. In such circumstances, patient education regarding expected benefits and improved understanding of how to judge treatment efficacy should help improve both adherence and persistence with treatment.
It was not the purpose of this study to examine differences and similarities between patient and physician perceptions regarding compliance. However, some interesting differences were noted. Although both physicians and patients agreed that patient motivation was key to successful treatment, physicians might be underestimating their influence in motivating patients and shaping their expectations regarding treatment outcomes. Additionally, patients may have a greater need for ongoing support and access to information to ongoing questions and issues than is anticipated or available from many health care offices. It is hoped that future research can more directly address the issues of similarities and differences between physician and patient perspectives and their impact on compliance.
Caution should be used in generalizing the findings of this study to models of compliance for other self-injectable treatments. The study used a convenience sample and all but one of our participants were female. The persistence rate of our sample (65%) was also higher than generally reported in the literature (Dunbar-Jacob et al 2001; DiMatteo et al 2002; DiMatteo 2004). Our sample was also older, predominately Caucasian, and retired. Thus our model may be disease, treatment, gender and/or sample dependent. However, the wide age range and geographic distribution of the sample should help improve the generalizability of our findings. Continued research is necessary to confirm or adapt our model for other conditions with their respective treatments and it is hoped that this study will further the generation of new hypotheses on which these future studies can collect quantitative data more suitable for statistical testing. Finally, although the purpose of this study was not to enter the debate on the correct labeling of medication behavior as compliance, adherence or persistence, we do believe that a common language and definition of terms is necessary if we are to be able to accurately report and further our understanding of the role of medication behavior. Differences in defining compliance terms may account for some of the variability in estimates found in the literature. Given that one can be persistent and yet not adherent, we suggest that the two concepts be addressed separately under a broader umbrella of compliance. Further, uniformity in methods of assessing each aspect of compliance would greatly facilitate the interpretation of much of the literature. However labeled or measured, it remains clear that compliance is a key factor in determining the overall effectiveness of treatments.
Conclusions
Based on the findings from this study, the following basic principles of compliance were formulated:
Compliance is a process over time that is influenced by both physician and patient factors.
This process begins BEFORE the patient is prescribed the treatment.
Physician factors (such as physician level of comfort with a treatment’s safety and efficacy) play a key role in the physician’s decision to prescribe a treatment.
The physician’s message (level of enthusiasm) conveyed to the patient AND the type of training received by the patient are major factors in determining if the patient will actually start treatment.
Physician support and continued enthusiasm for the treatment during the first weeks of treatment plays a key role in compliance at the start of treatment.
Perceived efficacy on the part of the patient is a key factor for long-term persistence.
Factors that influence adherence differ from factors that influence persistence.
Acknowledgments
We would like to thank all the patients and physicians who generously gave of their time and allowed us to interview them.
Footnotes
Disclosure
The authors were supported by Eli Lilly and Company.
References
- Beksinska ME, Rees HV, Smit J. Temporary discontinuation: a compliance issue in injectable users. Contraception. 2001;64:309–13. doi: 10.1016/s0010-7824(01)00268-2. [DOI] [PubMed] [Google Scholar]
- Bourgeois JA. Compliance with psychiatric treatment in primary care: review and strategies. Prim Psychiatry. 2005;12:40–7. [Google Scholar]
- Cummings SR, Karpf DB, Harris F, et al. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med. 2002;112:281–9. doi: 10.1016/s0002-9343(01)01124-x. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, DiNicola DD. Achieving Patient Compliance: Psychology of the Medical Practitioner’s Role. Tarrytown, NY: Pergamon Press Inc; 1982. [Google Scholar]
- DiMatteo MR, Giordani PJ, Lepper HS, et al. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- Dunbar-Jacob J, Mortimer-Stephens MK. Treatment adherence in chronic disease. J Clin Epidemiol. 2001;54(Suppl 1):S57–60. doi: 10.1016/s0895-4356(01)00457-7. [DOI] [PubMed] [Google Scholar]
- Fraser C, Hadjimichael O, Vollmer T. Predictors of adherence to Copaxone therapy in individuals with relapsing-remitting multiple sclerosis. J Neurosci Nurs. 2001;33:231–9. doi: 10.1097/01376517-200110000-00003. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, McCaul KD, Schafer LC. Barriers to regimen adherence among persons with insulin-dependent diabetes. J Behav Med. 1986;9:65–77. doi: 10.1007/BF00844645. [DOI] [PubMed] [Google Scholar]
- Graveley EA, Oseasohn CS. Multiple drug regimens: medication compliance among veterans 65 years and older. Res Nurs Health. 1991;14:51–8. doi: 10.1002/nur.4770140108. [DOI] [PubMed] [Google Scholar]
- Haynes RB, McKibbon KA, Kanani R. Systematic review of randomized trials of interventions to assist patients to follow prescriptions for medications. Lancet. 1996;348:383–6. doi: 10.1016/s0140-6736(96)01073-2. Erratum in: Lancet, 1997. 349:1180. [DOI] [PubMed] [Google Scholar]
- Leo RJ, Jassal K, Badhai YD. Nonadherence with psychopharmacologic treatment among psychiatric patients. Prim Psychiatry. 2005;12:33–9. [Google Scholar]
- McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868–79. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Cox D, Epstein L, et al. Teaching patients to self-inject: pilot study of a treatment for injection anxiety and phobia in multiple sclerosis patients prescribed injectable medications. J Behav Ther Exp Psychiatry. 2002;33:39–47. doi: 10.1016/s0005-7916(02)00011-3. [DOI] [PubMed] [Google Scholar]
- Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657–65. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- Piette JD, Wagner TH, Potter MB, et al. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42:102–9. doi: 10.1097/01.mlr.0000108742.26446.17. [DOI] [PubMed] [Google Scholar]
- Roberson MHB. The meaning of compliance: patient perspectives. Qual Health Res. 1992;2:7–26. [Google Scholar]
- Robiner WN. Enhancing adherence in clinical research. Contemp Clin Trials. 2005;26:59–77. doi: 10.1016/j.cct.2004.11.015. [DOI] [PubMed] [Google Scholar]
- Ryan AA. Medication compliance and older people: a review of the literature. Int J Nurs Stud. 1999;36:153–62. doi: 10.1016/s0020-7489(99)00003-6. [DOI] [PubMed] [Google Scholar]
- Sarkar S, Reginster JY, Crans GG, et al. Relationship between changes in biochemical markers of bone turnover and BMD to predict vertebral fracture risk. J Bone Miner Res. 2004;19:394–401. doi: 10.1359/JBMR.0301243. [DOI] [PubMed] [Google Scholar]
- Schwartzman S, Morgan GJ., Jr Does route of administration affect the outcome of TNF antagonist therapy? Arthritis Res Ther. 2004;6(Suppl 2):S19–23. doi: 10.1186/ar996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unson CG, Siccion E, Gaztambide J, et al. Nonadherence and osteoporosis treatment preferences of older women: a qualitative study. J Womens Health (Larchmt) 2003;12:1037–45. doi: 10.1089/154099903322643965. [DOI] [PubMed] [Google Scholar]
- Vijan S, Hayward RA, Ronis DL, et al. The Burden of Diabetes Therapy: Implications for the Design of Effective Patient-centered Treatment Regimens. J Gen Int Med. 2005;20:479–82. doi: 10.1111/j.1525-1497.2005.0117.x. [DOI] [PMC free article] [PubMed] [Google Scholar]