Abstract
The World Health Organization claimed recently that improving patient adherence to long term therapies would be more beneficial than any biomedical progress. First, however, we must understand its mechanisms. In this paper I propose a novel approach using concepts elaborated in a field rarely explored in medicine, the philosophy of mind. While conventional psychological models (eg, the Health Belief Model) provide explanations and predictions which have only a statistical value, the philosophical assumption that mental states (eg, beliefs) are causally efficient (mental causation) can provide the basis for a causal theory of health behaviors. This paper shows that nonadherence to long term therapies can be described as the medical expression of a philosophical concept, that is, weakness of will. I use philosophical explanations of this concept to suggest a mechanistic explanation of nonadherence. I propose that it results from the failure of two principles of rationality. First, a principle of continence, described by the philosopher Donald Davidson in his explanation of weakness of will. This principle exhorts us to act after having considered all available arguments and according to which option we consider best. However, patients conforming to this principle of continence should rationally be nonadherent. Indeed, when patients face a choice between adherence and nonadherence, they must decide, in general, between a large, but delayed reward (eg, health) and a small, but immediate reward (eg, smoking a cigarette). According to concepts elaborated by George Ainslie and Jon Elster, the force of our desires is strongly influenced by the proximity of reward. This inter-temporal choice theory on one hand, and the mere principle of continence on the other, should therefore lead to nonadherence. Nevertheless, adherence to long term therapies is possible, as a result of the intervention of an additional principle, the principle of foresight, which tells us to give priority to mental states oriented towards the future.
Keywords: patient adherence, chronic diseases, weakness of will, inter-temporal choice, principle of foresight, causal theory of health behaviors, philosophy of mind
The lack of concordance between patients’ behavior and prescribed therapy is described in the medical literature as patient noncompliance (Sackett 1979) or nonadherence (Lutfey 1999). This phenomenon concerns all the pathologies. Typically, the disease prone to the phenomenon of nonadherence is chronic disease, remaining silent until a complication occurs. The patient does not understand its severity, its treatment necessitates a number of medications and interventions to change life style (diet, exercise, smoking habits) and is more preventive than curative (Meichenbaum and Turck 1987a). Nonadherence is considered to be a major issue in contemporary medicine. Indeed the World Health Organization (WHO), in a recent report entitled “Adherence to long term therapies, time for action”, claimed that solving this problem would be more beneficial than any biomedical discovery (WHO 2003).
This paper aims to investigate the mechanism of nonadherence: I will argue that patient nonadherence represents, together with manifestations like drug addiction, gambling, spending sprees, procrastination and the like, a manifestation of what philosophers have called weakness of will, where people seem to act against their best judgment. In other words, patient nonadherence shares with these behaviors a common mechanism, which can be used to define a general concept encompassing them all. In medical terms, weakness of will is a syndrome and patient nonadherence to long term therapies represents its medical manifestation.
The puzzling aspect of medical nonadherence evokes the concept of weakness of will
Nonadherence concerns all aspects of therapy: not only taking medicines, but also following recommendations on life-style changes such as diet and physical exercise, avoiding high-risk behaviors, such as the use of tobacco or alcohol, or simply returning for the next medical appointment. For instance, in diabetes care, a review of the literature revealed that about two thirds of patients followed advice on diet, but only 25% of patients followed advice on exercise, and only 7% of patients were found to follow all recommendations (McNabb 1997). Considering specifically medication, the rate of adherence varied according to the studies from 60% to 85%. Furthermore, only 16% to 80% of patients were found to persist with their treatment over a period of 6 to 24 months (Cramer 2004). One year after a heart transplant, the rate of nonadherence to immunosuppressive drug prescription ranged from 20% to 25% (Dew 1996).
This last observation is puzzling, because such patient behavior is extremely harmful to personal health, and this is not just a matter of physician opinion. This paradoxical aspect of nonadherence evokes the phenomenon of weakness of will, or incontinent actions, or akrasia (literally without strength): between two actions a and b, the akratic individual performs b, while her reason would exhort her to perform a. This paradox has puzzled philosophers since Aristotle (Aristotle, Nic Eth). They had to explain how weakness of will is possible (Davidson 1980a), which is typically a philosophical question, since “philosophers are interested in the conceptual line that separates the possible from the impossible. They ask how certain phenomena, including mental phenomena, can exist” (Pears 1998). Such questions justify the philosophical approach proposed herein to explain how nonadherence is possible. Furthermore, I will provide the evidence that adherence itself also appears to be paradoxical. Thus, explaining how adherence is possible is the main aim of this paper.
Nonadherence to treatment, a bunched phenomenon
As shown above, nonadherence presents a continuum, from rare patients entirely adherent to medical prescriptions, to patients who are completely nonadherent. Philosophers have pointed out that weakness of will is “regional” as well. Thus, as noted by Alfred Mele (1987), someone who exhibits a great deal of self-control in professional life may be quite weak-willed about eating or smoking. Nevertheless, different aspects of therapeutic nonadherence have often been observed simultaneously in a given patient. For example, diabetic patients who smoke are less adherent to recommendations concerning blood glucose monitoring and exercise, and skip more medical appointments than nonsmokers (Solberg 2004). In contrast, nonsmokers may readily accept a complex treatment (Perros 1998) and patients who monitor their blood glucose frequently also devote more time to caring for their feet, to their diet, or to exercise (Safford 2005). Similarly, a recent study showed that in a cohort of more than 20,000 users of statin, adherent patients were more likely to undergo prostate-specific antigen tests, fecal occult blood tests, screening mammograms, and to receive influenza or pneumococcal vaccinations during a 1-year ascertainment observation period (Brookhart 2007). Furthermore, a recent meta-analysis of 21 clinical trials showed that patients who were adherent to placebo had lower rates of mortality than other patients in the placebo arm, who were less adherent (Simpson 2006). This finding can be understood if one assumes that nonadherent patients not only did not take their medication, but had other harmful lifestyle habits.
Taken together, these data may suggest a typology concerning the fact of being adherent or nonadherent to therapy, which may be explained in part by extrinsic factors: nonadherence to medical recommendations is frequently observed, as shown above, in smokers, but also in those who live alone (Toljamo 2001), who are depressed (Ciechanowski 2000) or socially deprived (Self 2005). I will propose another hypothesis, however: these manifestations are bunched under the denomination of nonadherence because they share a common mechanism, involving weakness of will.
Patient nonadherence and weakness of will
Interestingly, this explanation of their behavior is often spontaneously given by patients, maybe because the concept of will is strongly anchored in folk psychology. The word willpower is often used by lay people. On the difficulty of long term dieting and its consequence, obesity, a Spanish study (Lopez-Azpiazu 1999) showed that the three reasons most often given for an unhealthy diet were lack of willpower (30%), irregular work schedules (30%), and the unattractive appearance of the recommended food (21%). Some obese patients ask for a gastric band as a mechanical support for their weak will: “It will force me to follow my diet.” Similarly, the two reasons most often given by Canadian women (Olmsted 2004) to explain why they do not exercise when they know it would be good for their health, are also lack of time (40% of answers) and lack of willpower (also 40% of answers). An English study on more than 10,000 subjects showed that those who suggested internal type barriers (I am too busy, I lack willpower, I am lazy) rather than external barriers (transport is too long, I have no money) are significantly less physically active (Ziebland 1998).
Equating patient nonadherence to therapies with weakness of will (Reach 2000) represents a paradigm shift in the analysis of this problem: that is, a switch from a conception of nonadherence from the physician’s point of view (nonadherence is classically defined as the absence of concordance between patient behavior and medical recommendations) to a conception in which only the patient’s rationale is considered. In the next section, I will describe the current philosophical explanations for weakness of will, and try to determine whether they are relevant to the specific issue of nonadherence to long term therapy.
Patient nonadherence as a case of weakness of will: which mechanism?
Inter-temporal choice
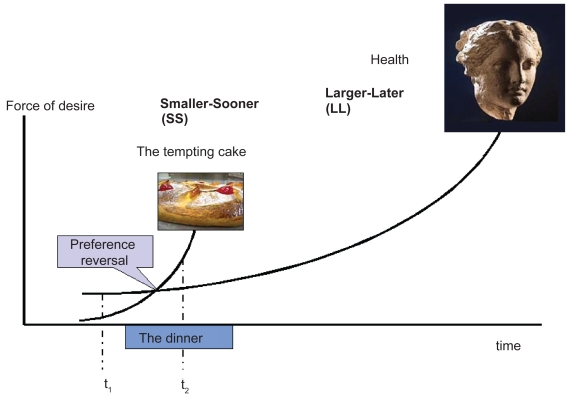
This first explanation, proposed by George Ainslie (1985) and Jon Elster (1999), can be demonstrated by the following scenario (Figure 1). I am entering a restaurant with a strong resolution to follow my diet. The value of the reward linked to this resolution (my health) is by that time more important than the value I give to the dessert I see on the menu. However, by the end of the dinner, the value given to the dessert suddenly increases, and becomes higher than the value I give to my desire to remain lean. This change is a result of the hyperbolic nature of the function describing the effect of time discounting (Ainslie 1985). At that time of the dinner, I am not irrational if I finally decide to order the dessert.
Figure 1.
Preference reversal.
Because of the hyperbolic nature of the curves describing time discounting of a small and a large reward, the curves cross over (preference reversal). At time t1, the large reward seems more important than the small, immediate reward. At t2, taking the small, immediate, reward is rational. According to George Ainslie:
“a hyperbolic discounter who faces a choice between smaller-sooner (SS) and larger-later (LL) rewards will evaluate them roughly in proportion to their objective size – their values at zero delay – when both are distant, but value the SS reward disproportionately when it is close. Thus she will have an innate tendency to form temporary preferences for SS rewards, purely as a function of elapsing time”. (Ainslie 2005).
Time discounting, ie, the bowing of the curves shown in Figure 1 and, therefore, the risk of preference reversal, are more or less marked depending on the individuals: people are more or less impatient, having a more or less important time discounting rate. Impatience may represent a heritage from our ancestors, when it was advantageous to be impatient (Elster 1986). The degree of impatience may have a neurophysiological, or even genetic basis (Manuck 2003). Furthermore it may be modified by exogenous factors, the rate of depreciation of the future increasing for example under the influence of social deprivation or of depression (Feldman 2002), or simply under the influence of alcohol, a phenomenon known as alcohol myopia (Steele and Josephs 1990).
In this way the nonadherent patient may well be the patient who is by nature impatient, preferring the immediate reward of nonadherence (smoking, the extra-piece of cake, rest) to the delayed reward of adherence, avoiding the long term complications of the disease. This common mechanism may explain why in a given individual, different manifestations of the weakness of will, including nonadherence to therapy, are bunched. The inter-temporal choice explanation of patient nonadherence is therefore appealing. It must be stressed, however, that while strong relationships between health behavior and measures of time preference can be found in addiction (Bickel 2003), a number of studies reviewed by Gretchen Chapman which examined other kinds of health behavior, found a weak or nonexistent relationship to time preference. For instance, one study examined two measures of adherence to hypertension treatment: pharmacy records of prescription refills and medical appointments kept. Neither measure was related to a hypothetical-choice measure of discount rate. As discussed by Chapman, this failure to relate health behavior to time preference may be due to the fact that both hypothetical choices and health behaviors reflect time preferences, but that time preferences vary sufficiently from situation to situation, so that the two are not related. Alternatively, some classes of behavior, like smoking, may reflect time preference, but not others, like health behaviors (Chapman 2003). It remains therefore to explain why smoking and other harmful health behaviors are bunched in a number of patients.
The principle of continence and the partition of mind hypothesis
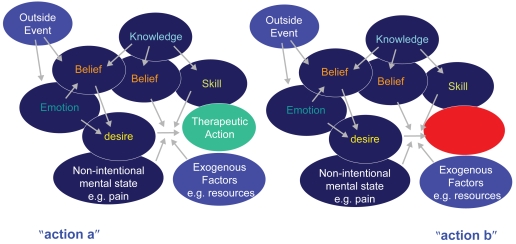
A second kind of explanation was given by the philosopher Donald Davidson, who offered two successive accounts of the weakness of will (Davidson 1980a, 1982). First he evoked the existence of a principle of rationality, which describes the coherence of our actions. This principle of continence exhorts us, when we have the choice between two possible actions, to consider all the available arguments, and to act, all things considered, according to our estimate of what is best for us: “the phrase ‘all things considered’ must, of course, refer only to things known, believed, or held by the agent, the sum of his relevant principles, opinions, attitudes, and desires” (Davidson 1980a). Thus, “incontinent” (weak-willed) action is due to a failure of this principle. The application of this conception of weakness of will to nonadherence is illustrated in Figure 2.
Figure 2.
Weakness of will as a failure of Davidson’s principle of continence, and its application to patient nonadherence
The philosophy of action has, since Aristotle and Hume, proposed that our actions are driven by an attitude based on a desire and the belief that this particular action belongs to the actions which will contribute to granting this wish. Beliefs and desires can be driven by emotions that are triggered by outside events. Knowledge and skills have an instrumental role: they contribute to the formation of beliefs, or are involved in the accomplishment of the action. Nonintentional states, like pain, also belong to what Davidson calls “all things considered”. When an agent must decide between two actions, she uses a “principle of continence”, which exhorts her to consider all the available arguments, and to carry out the action that, all things considered, she has estimated to be the best for her. Thus, “incontinent” (weak-willed) action is due to a failure of this principle. Nonadherence to long term therapies can be considered as a choice between (a) performing a therapeutic action (eg, measuring blood glucose to adjust insulin dose) and (b) not performing this action, which can itself be considered as an “action” having its own reasons.
This explanation is insufficient, however, because it does not explain how a principle of rationality can be “exiled” from practical reasoning. Let’s suppose that the choice between action “a” and action “b” in Figure 2 is between nonsmoking and smoking a cigarette. The patient considers all the arguments and her best judgment tells her that she should refrain from smoking. If she exercised her principle of continence, she would refuse the cigarette. However, she takes it. One may suppose that her desire to smoke caused the “exile” of her principle of continence. Here, Davidson stumbled on a difficulty: this argument assumes that a mental state (a desire) causes a mental event (the exile of a principle of rationality) without being a reason for this event. This phenomenon contradicts his own causal theory of action, published in a seminal paper “Actions, reasons and causes” (1963), which demonstrated that the reason for an action is its cause (Davidson 1980b). In order to solve the paradox of the incontinent action, it became necessary to explain how a desire can cause a mental event without being its reason: “There is a mental cause which is not a reason for what it causes” (Davidson 1982).
Indeed, this can happen when cause and effect occur in different minds. In his essay “Paradoxes of irrationality”, Davidson gave the following example:
“Wishing to have you enter my garden, I grow a beautiful flower there. You crave a look at my flower and enter my garden. My desire caused your craving and action, but my desire was not a reason for your craving, nor a reason on which you acted. (Perhaps you did not even know about my wish). Mental phenomena may cause other mental phenomena without being reasons for them, then, and still keep their character as mental, provided cause and effect are adequately segregated” (Davidson 1982).
This led Davidson to appeal to a Freudian idea, that of a partitioned mind:
“I went on to explain the vague and confusing notion of an attitude or principle being ignored or suppressed by appealing to a Freudian idea, that of a partially partitioned mind. The idea, as I employed it, meant that attitudes in the same mind could be kept from actively interacting, so that the agent remained to some extent protected from the clash that would result from facing unwelcome thoughts or their consequences” (Davidson 1999).
Although he presented this partition of the mind as a “Freudian idea”, Davidson pointed out that this partition is not necessarily between the conscious and unconscious domains:
“The standard case of akrasia, or incontinent action is one in which the agent knows what he is doing, and why, and knows that it is not for the best and knows why. He acknowledges his own irrationality” (Davidson 1982).
Any clinician will recognize a number of clinical observations. When we tell a patient about an obvious occasion when we think she should have adjusted her insulin dose (for instance, her glycemia was very high every morning during the last two weeks), and when we ask her why she did not do it, either she cannot answer the question, or her explanation applies only to one element of the debate. For example, she might say she is afraid of hypoglycemia, or afraid of gaining weight, or she has had a lot of problems lately and was too preoccupied to take care of her diabetes (Reach 2005a). The other element, the plea to adjust the insulin doses, seems to have disappeared from the practical reasoning, although the patient is conscious of it: what is irrational is this disappearance. Some pipe smokers remove the packet labels that warn of tobacco’s dangerous effects. Although such action is irrational, in this way they can avoid ‘considering’ such issues.
However, applying this conception to health behavior is problematic, too. As Olav Gjelsvik pointed out, Davidson’s concept allows for causal/irrational deviations from what is considered best, all things considered. In theory, there is no reason to expect any particular pattern in these causal/irrational deviations, which might favor a long-term perspective or a short-term one (Gjelsvik 1999). If we consider the two opposing actions of accepting or refusing a cigarette, we can see that the desires which would cause the action of smoking are largely present-oriented, while those causing the refusal of the cigarette are concerned with the future. The theory of time discounting described above indicates that the force of a desire depends on the temporal proximity of its reward. Therefore, the incontinent desire should be stronger, and the principle of continence should exhort us, rationally, to be nonadherent. An additional principle is therefore necessary to give the advantage to those arguments linked to the future.
Why are people adherent to therapies in chronic disease? The need for an additional principle
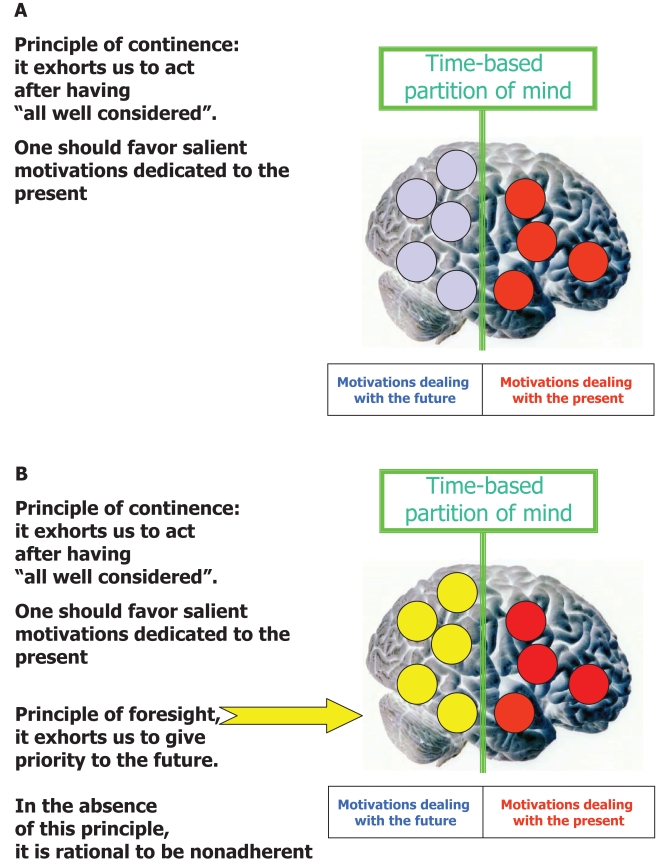
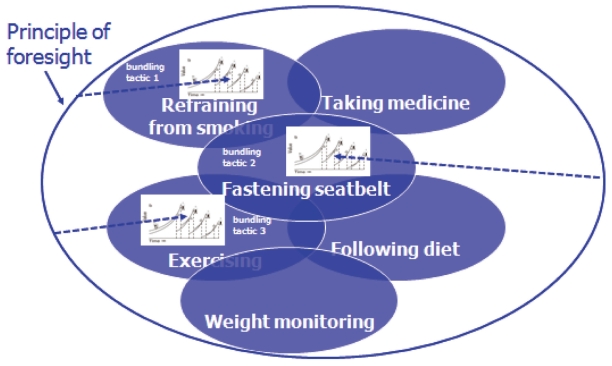
This analysis leads me to propose a hypothesis in which adherence would require using an additional principle, referred to as a principle of foresight, which would give priority to motivations that are directed toward the future, rather than immediate rewards (Figure 3). In the absence of such a principle, the patient would be nonadherent because the principle of continence would place priority on the present (Figure 3A). What we (the patient’s doctor or relatives) would consider irrational, according to our own principles of continence and foresight, and what we would qualify as nonadherence, would be, from the patient’s point of view, completely rational (Reach 2007).
Figure 3.
The principle of continence (A) and the principle of foresight (B).
One may speculate that the differentiation of such a principle of foresight arises slowly in adulthood, leading to an age of foresight, where for example, we contract health and life insurance. In fact, the principle of continence may also appear slowly. Davidson quoted “St. Augustine’s extraordinary prayer: ‘give me chastity and continence, only not yet’ (Confessions, VIII, vii)”.
If one wants to take a reductionist view, it is tempting to speculate that this hypothesis may have a neurophysiological basis. Some mental states could in some way be tagged as “present-relevant” or “future-relevant”. Such labels would be neurophysiologically removed by alcohol, which explains the phenomenon of “alcoholic myopia”, or by some neuromediators released under the effect of emotion, which explains the role of emotions in triggering weakness of will (Tappolet 2003), in our case, nonadherence to therapies.
Clinical implications of the hypothesis
First, from a heuristic point of view, the hypothesis presented here is consistent with some obvious clinical observations. For example, the remarkable therapeutic adherence which arises at the time of pregnancy, well known by diabetologists (Ruggiero 1990) and physicians taking care of VIH-infected patients (Vaz 2007), but also the therapeutic nonadherence observed so often in those who are socially deprived (Feldman 2002). In the minds of these latter patients, who do not know what tomorrow will look like, the future-related domain is empty. It may be the same for adolescents, among whom adherence to therapy is often poor: they live in the present or even consider themselves immortal, which is the same. Significantly, a recent paper showed that adherence to therapies by adolescents and young adults, while undergoing heart transplants, is linked to the patient’s maturity (Stilley 2006).
Secondly, and more practically, helping the patient to develop a principle of foresight may represent a major goal in the trust-based patient-physician relationship. In this way the patient may become adherent, by sharing her views with her doctor about the benefits of the treatment, and also by accepting the long term gains of adopting a principle of foresight. Discussing with the patient her approach to the concept of time may therefore represent an important part of the educational diagnosis. Incidentally, it has been suggested that in general physicians may have a lower discounting rate, and are more concerned about the future than patients (Feldman 2002). When dealing with patients who apparently are not (or not yet) interested in the future, the search for intermediary rewards may represent a well known alternative, rather than proposing unrealistic long-term objectives: “The goals must be realistic or potentially achievable. The inclusion of subgoals that have a high likelihood of success increases adherence by both patients and HCPs” (Meichenbaum and Turk 1987b). Thus the conceptual framework proposed herein may pave the way toward the design of specific and testable interventions aimed at improving patient adherence.
Different avatars of the principle of foresight
In this paper, I have proposed a mechanism to explain the “nonadherence syndrome”, which involves two principles: Davidson’s principle of continence, which exhorts us to act only after having “all well considered”, and the additional principle of foresight, which tells us to give priority to the future. Behaving according to these principles would help to protect our health. The principle of foresight may have different avatars: a low discounting rate, as in the inter-temporal choice theory, self-control, as in Gary Watson’s and Alfred Mele’s explanations of the weakness of will (Watson 1977, Mele 1987), will-power, as in Roy Baumeister’s account, or Richard Holton’s strength of will (Baumeister 2003, Holton 2003).
A final avatar of the principle of foresight may be self-love, which is for the philosopher Harry Frankfurt the purest form of love and, indeed, the most authoritative form of caring. In his essay, “The importance of what we care about” (Frankfurt 1988), Frankfurt suggested that “the outlook of a person who cares about something is inherently prospective; that is, he necessarily considers himself as having a future”. In his recent book The Reasons of Love, he gives an interpretation of self-love, which appears directly relevant to our discussion:
“It may happen that a person loves something, finds it important, and, at the same time, does not want to love it. If the ambivalence cannot be resolved by a decisive identification with one side of the conflict, the person’s mind is fragmented. Ambivalence is a disease, and the health of mind demands a unified will. To have an undivided will is to be wholehearted. And, in turn, to be wholehearted is to love one-self” (Frankfurt 2004).
I propose that this construct can help us to understand one of the meanings of patient adherence. Thus, nonadherent patients are unable to decide between the long term reward of health and some immediate pleasure; their mind is “fragmented”; in contrast, adherent patients who take care of their health refuse the fatality of long-term complications; using their principle of foresight, their will is now undivided; their future is important to them and they are whole-heartedly willing to preserve it. According to a frankfurtian account of the phenomenon, I suggest that they do it because, in fact, they love themselves. The relationship between this philosophical concept of self-love and the more classical, psychological, construct of self-esteem deserves further consideration.
The play by the French dramatist Eugène Ionesco, Exit the King (1962) describes the behavior of King Bérenger when he learns that he will die at the end of the play. He refuses to do so. At the very end, he cries: I love myself! Let us propose that, as the everyman, he would like to keep taking care of himself, and that if a treatment was proposed to him, he would be a perfectly adherent patient.
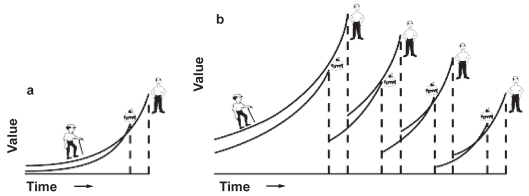
A top-down model of adherence
In his Breakdown of Will, George Ainslie suggests that an impatient individual may serve her long term interests by obeying a personal rule (Ainslie 2001). Here, her current choice (for instance refusing the dessert at the end of the dinner) will to some extent include the bundle of future rewards that this choice predicts. That is, the current choice, today, of a larger, later reward (eg, her health) over a smaller, more immediate reward (eg, this piece of cake), if perceived as a test case, could possibly predict a whole bundle of larger, later rewards in the future, and thus be valued more than it would be by itself. Ainslie elegantly demonstrated that this mental mechanism transforms hyperbolic curves into exponential-like curves which cannot cross each-other (Figure 4, from Ainslie 2005). Hyperbolic curves lead to the danger of preference reversal (at the end of the dinner, I order the dessert), but this is not possible with exponential curves. It is important to point out that such a personal rule applies only to a specific behavior (ie, refraining from smoking). Of course, the patient may form different personal rules for different behaviors. I suggest that she may do this by using the principle of foresight.
Figure 4.
George Ainslie’s personal rules.
“If the person makes a whole series of choices at once – for instance a class of choices united by a principle – the curve describing her valuation of the LL rewards will be much higher: Principled choice boosts LL reward values only when discount curves are hyperbolic or otherwise deeply bowed. Such curves from a series of paired SS and LL rewards may come never to cross (b), with the same amounts that cause curves from a single pair to cross (a, = last pair in b).” (Ainslie 2005).
A specific aim of this paper was to provide a mechanistic explanation of a clinical observation: different manifestations of nonadherence are often “bunched” in a given patient, who is influenced by the principle of foresight. However, there is a difference between this effect of the principle of foresight, which results in the bunching in the same patient of different aspects of adherence, and the solution of bundling larger rewards according to a personal rule, which Ainslie found increases their value. In the first case, several distinct tasks of therapy are connected (Figure 5). Interestingly, in Holton’s account, will-power is described as a general faculty, which enables one “to abide by all of one’s resolutions: resolutions not to drink, not to smoke, to eat well, to exercise, to work hard, not to watch daytime television, or whatever” (Holton 2003). We arrive therefore at a “top-down” conception of adherence, in which principles of rationality represent the mechanistic basis of adherence. This idea is consistent with the clinical observation that different nonadherent manifestations are often present in the same patient.
Figure 5.
A top-down model of adherence to therapies in chronic diseases.
In this model, the patient may be adherent to a given recommendation (eg, refraining from smoking, fastening seatbelt, exercising) by applying to each specific task the tactic of a personal rule. George Ainslie suggests that this tactic consists in considering the current choice of the larger, later reward over a smaller, sooner reward (see Figure 1), as a test case which predicts a whole bundle of larger, later rewards in the future (bundling tactic) described in Figure 4. In this example, the patient has three personal rules concerning smoking, exercising, and fastening seatbelt. By using a principle of foresight, the patient adopts a general, top-down, strategy giving priority to the future and thus bunching different therapeutic tasks, also including taking medicine, following diet etc. Note that the principle of foresight may also represent the driving force, which leads the patient to adopt individual bundling tactics (dotted lines). (Modified with permission from Reach 2007).
A pathophysiological approach: principles of rationality as devices
The hypothesis presented here relies on two principles of rationality to explain how one can, in the long term, be adherent to medical therapies, namely Davidson’s principle of continence, and the principle of foresight. One may argue that principles are actually nothing but ad hoc explanations, which do not explain anything. This argument can be defeated if one follows Robert Nozick’s reasoning that principles are devices, whose function is to help us avoid random decisions (Nozick 1993). Similarly, in the natural world, the function of enzymes is to make it possible that a given biochemical reaction is oriented in a specific direction. Indeed, although reasons are causes of actions (Davidson 1980b), there are no psychological laws, as in the natural world, where a reason A leads always to an effect B. In a “physiology of mind”, A may lead to B or C, where C can be the opposite of B: alcoholism in the parents may cause alcoholism or sobriety in the children (Elster 2003). Thus, principles may be understood as necessary “teleological” devices of human logic.
Therefore those who are not adherent to medical therapies are those who do not have the principles that allow them to be adherent. This conclusion may seem to be circular. However, it is not more circular than the statement that insulin is the hormone which prevents the development of a diabetic state. Indeed, it is compatible with the fact that in medicine, as shown by the French philosopher Georges Canguilhem, pathology always precedes physiology: the understanding of the adrenal function had to wait for the observation that some people have an adrenal insufficiency and the description of its symptoms by Thomas Addison (Canguilhem 1991). Accordingly, observing patients’ refusal to take their medication, to exercise, to follow a particular diet and the like, is the first step which helps us to understand how adherence to medical therapies is possible. Once the mechanism of adherence is understood, one is in a better position to strengthen it, if necessary.
Psychological and philosophical accounts of nonadherence
In this paper, I have proposed a philosophical account of nonadherence to long term therapies. In the psychological literature, several models have been proposed to aid our understanding of how a health behavior can be changed. These models are a product of psychology, sometimes called the science of behavior, and more specifically of one of its relatively new fields, the psychology of health. Rigorous empirical research must demonstrate statistically significant correlations between the supposed determinants, and the health behavior. The first model, the Health Belief Model, showed the importance of beliefs in the adoption of a health behavior (Becker 1975). The notion of motivation, in the form of the concept of intention, was introduced by the Theory of Reasoned Action (Fishbein and Ajzen 1975) and the Theory of Planned Behavior (Ajzen 1985). The Theory of Interpersonal Behavior (Triandis 1979) introduced the role played by habit. The Self-Regulatory Model showed that a subject’s self-evaluation of behavior creates a situation of feedback, which manifests itself not only at the cognitive, but also at the emotional level (Leventhal 1997). The Health Locus of Control (Wallston 1978) and the Sociocognitive Theories (Bandura 1991) highlighted the psychological notion of self-efficacy. The Transtheoretical Model of Change (Prochaska 1983) has to be set apart, however. It attempts to explain the adoption of a health behavior as a dynamic process, concerned not so much with what leads the subject to a change in behavior, but rather with how to describe the stages of the change.
No one of these models incorporates the concept of weakness of will – which is surprising, given that failure to diet or to refrain from smoking are routinely used by philosophers as examples of paradigmatic cases of weakness of will, and that patients themselves point to their lack of willpower to explain why they do not follow recommendations, at least concerning diet and exercise. A possible explanation is historical. Most of these psychological models were published during the years 1970 to 1980, before, or during, the period when the concept of weakness of will was revisited by philosophers. For example, Donald Davidson’s classic paper, “How is weakness of will possible?” (Davidson 1980a) was first published in 1970, papers on weakness of will and akrasia by Gary Watson and by Amelie Rorty were published in the late 1970s (Watson 1977, Rorty 1980), and Alfred Mele published his book on akrasia in 1987. Similarly, the concepts of inter-temporal choice and of multiple self, which are used to explain the weakness of will, derive from George Ainslie’s first experimental works in the early 1970s (Ainslie 1974) and were mainly popularized in “The Multiple Self”, edited by Jon Elster in 1986 (Elster 1986), and in his “Picoeconomics” published in 1992 (Ainslie 1992), the year when the first textbook on inter-temporal choice, “Choice Over Time”, was edited by Jon Elster and George Loewenstein (1992).
Actually, it would be fair to recognize that these various psychological models, proposed to explain how one adopts a health behavior, do not explicitly refer to the concept of will, or its weakness, but some make clear the importance of constructs, which may be related, such as intention or self-efficacy. Thus, in the Theories of Reasoned Action and Planned Behavior, the likelihood of adopting a health behavior is closely associated with the intention expressed by the patient. In these models, the patient’s intention to perform a health behavior is a construct combining her attitude toward performing the behavior and subjective norms, represented by beliefs, concerning the way the behavior is perceived by persons who may be import to her.
Similarly, in the Transtheoretical Model described by James Prochaska, neither will nor intention is explicitly mentioned. However, I have shown elsewhere that we can interpret this model philosophically (Reach 2005b), and recognize the step from pre-contemplation to contemplation, to the formation by the individual of an intention, and the step from contemplation to preparation, to the patient’s decision to adopt a health behavior. In the same way, the maintenance phase of the Prochaska model may require from the patient what Richard Holton calls a resolution, that is, a special form of intention, used to defeat contrary inclinations that may emerge. But, according to Holton, the agents must have a strong will – that is, strength of will, which is the contrary to the weakness of will – to be able “to stick by their resolutions even in the face of strong contrary desires; agents whose willpower is weak readily abandon their resolutions” (Holton 2003).
Therefore, if patient nonadherence has not been formally related to the concept of weakness of will in these health psychological models, this may simply be connected with its pure philosophical nature. Although psychologists who elaborated these models used other words to describe the motor of behaviors, implicitly, they also used either a simple humean desire-belief account (Hume 1740), or an augmented humean account, including intention, as proposed by the philosopher Michael Bratman (Bratman 1999).
Conclusion: from statistical models to a causal theory of adherence, a change of paradigm
Nevertheless, this argument does not mean that these two accounts, psychological or philosophical, of adherence, are only different ways of saying the same thing. Most psychological models quoted above can be illustrated by showing boxes containing mental states (for instance, a belief), connected by arrows to boxes containing the behavior (for instance, quit smoking). The arrows represent associations between the mental state and the behaviors that were shown to exist during trials conducted with a certain number of subjects. However, it is well known that the existence of an association, statistically proven for a population of subjects, does not imply that in a particular subject there is a real causal link between the mental state and the subject’s behavior. At the most, we can predict, according to the Health Belief Model, that if an individual, let’s say Jane, believes that smoking is bad for her health, then Jane has a better chance of quitting smoking than if she does not hold this belief. But such a prediction remains simply statistical. Thus, if one day Jane really quits smoking, it does not mean that she did it because of this belief. She may have done it for a completely different reason, for example to please her daughter or because the price of cigarettes went up. On the other hand, Jane could also continue to smoke, even though she believes smoking is bad for her health. These models have a major limitation: they cannot explain why a given individual is or is not adherent to medical advice. Such behavior remains a mystery. And when one tries to improve the adherence of this individual, these models may prove to be useless, because they do not provide a mechanistic explanation of nonadherence of this particular individual.
Therefore, the search for a true explanation of the concept of adherence meant switching from descriptions of phenomena, which are certainly objective but have only statistical value, and returning to the individual, which would be unavoidably subjective, but would allow us to draw conclusions applicable to this particular individual. This is obviously crucial in clinical practice, since we do not take care of populations, but of patients. In other words, the investigation should no longer have as its object the behavior observed in a population of patients. It must focus on what a given patient is actually doing and for what reasons. Thus, the aim of this paper was to show that this investigation can no longer belong only to the field of psychology, but must move to philosophy.
Philosophical analysis is the only way to get close to the mechanisms of adherence. Using a philosophical, rather than a psychological, framework makes this possible, because philosophers, or at least some of them, admit that mental states are causally efficient. According to Jaegwon Kim,
“The possibility of human agency, and hence our moral practice, evidently requires that our mental states have causal effects in the physical world […] A science that invokes mental phenomena in its explanation is presumptively committed to their causal efficacy; if a phenomenon is to have an explanatory role, its presence or absence must make a difference, a causal difference” (Kim 2005).
Therefore, the philosophy of mind can provide a way to explain how some mental states, for instance a belief, cause the observed behavior of a given individual, in the same sense that insulin causes hypoglycemia in a given patient, and not only as a statistical phenomenon observed in a population of subjects. This paper attempts to apply the concept of mental causation, described in the philosophy of mind, to the medical issue of adherence, and may provide the change of paradigm necessary to reach a real understanding of the mechanism of nonadherence to long term therapies, and to resolve this crucial problem in contemporary medicine.
Acknowledgments
This paper, was presented in part under the title “Why people do not take their medication” at a Conference on moral and psychological weakness, organized by Akeel Bilgrami and Jon Elster at the Heyman Center for the Humanities, Columbia University, April 21 and 22, 2006. The author has no conflicts of interest to report.
References
- Ainslie G. Impulse control in pigeons. J Exp Anal Behav. 1974;21:485–9. doi: 10.1901/jeab.1974.21-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ainslie G. Beyond microeconomics, conflict among interests in multiple self as a determinant of value. In: Elster J, editor. The Multiple Self. Oxford: Cambridge University Press; 1985. pp. 133–75. [Google Scholar]
- Ainslie G. Picoeconomics: The strategic interaction of successive motivational states within the person. Oxford: Cambridge University Press; 1992. [Google Scholar]
- Ainslie G. Implications of Self-Control Disorders of Volition. Cambridge: MIT; 2005. A selectionist model of the ego: Implications for self-control. [Google Scholar]
- Ainslie G. Breakdown of Will. Oxford: Cambridge University Press; 2001. [Google Scholar]
- Ajzen I. From intention to actions: A theory of planned behaviour. In: Kuhl J, Beckmann J, editors. Action-control: From cognition to behaviour. Heidelberg: Springer; 1985. pp. 11–39. [Google Scholar]
- Aristotle. Nicomachean Ethics Book VII [online] [Accessed on 9 Jan, 2008]. URL: http://www.ilt.columbia.edu/publications/projects/digitexts/aris-totle/nicomachean_ethics/books07.html.
- Bandura A. Kurtines WM, Gerwitz JL, Hillsdale NJ, editors. Social cognitive theory of moral thought and action. Handbook of Moral Behavior and Development. 1991;1:45–103. [Google Scholar]
- Baumeister RF, Vohs KD. Willpower, choice and self-control. In: Loewenstein G, Read D, Baumeister RF, editors. Time and Decision: Economic and psychological perspectives on intertemporal choice. New York: Russell Sage Foundation; 2003. pp. 201–16. [Google Scholar]
- Becker MH, Maiman LA. Sociobehavioural determinants of compliance with health care and medical care recommendations. Med Care. 1975;13:10–24. doi: 10.1097/00005650-197501000-00002. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW. Delay discounting: a fundamental behavioural process of drug dependence. In: Loewenstein G, Read D, Baumeister RF, editors. Time and Decision: Economic and psychological perspectives on intertemporal choice. New York: Russell Sage Foundation; 2003. pp. 419–40. [Google Scholar]
- Bratman ME. Faces of Intention: Selected essays on intention and agency. Cambridge: Cambridge Studies in Philosophy; 1999. [Google Scholar]
- Brookhart MA, Patrick AR, Dormuth C, et al. Adherence to lipid-lowering therapy and the use of preventive health services: An investigation of the healthy user effect. Am J Epidemiol. 2007;166:348–35. doi: 10.1093/aje/kwm070. [DOI] [PubMed] [Google Scholar]
- Canguilhem G. Presse Universitaire de France, Collection Quadrige. 3ème édition. 1991. Le normal et le pathologique; p. 139. [Google Scholar]
- Chapman GB. Time discounting of health outcomes. In: Loewenstein G, Read D, Baumeister RF, editors. Time and Decision: Economic and psychological perspectives on intertemporal choice. New York: Russell Sage Foundation; 2003. pp. 395–417. [Google Scholar]
- Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- Cramer JA. A systematic review of adherence with medication for diabetes. Diabetes Care. 2004;27:1218–24. doi: 10.2337/diacare.27.5.1218. [DOI] [PubMed] [Google Scholar]
- Davidson D. How is weakness of will possible? In: Feinberg J, editor. Moral Concepts. Oxford: Oxford Readings in Philosophy; 1970. Reprinted as the second essay in Essays on Actions and Events. Oxford: Oxford University Press; 1980b.
- Davidson D. Actions, reasons, and causes. J Phil 1963Reprinted as the first essay in Essays on Actions and Events. Oxford: Oxford University Press; 1980b.
- Davidson D. Paradoxes of irrationality. In: Wollheim R, Hopkins J, editors. Philosophical Essays on Freud. Cambridge: Cambridge University Press; 1982. [Google Scholar]
- Davidson D. Reply to Ariela Lazar. In: Hahn LE, editor. The Philosophy of Donald Davidson: The library of living philosophers. XXVII. Open Court; 1999. [Google Scholar]
- Dew MA, Roth LH, Thompson ME, et al. Medical compliance and its predictors in the first year after heart-transplantation. J Heart Lung Transplant. 1996;15:631–45. [PubMed] [Google Scholar]
- Elster J. In: Le Laboureur et ses enfants. Gerschenfeld A, editor. 1986. p. 162. [Google Scholar]
- Elster J, Loewenstein G. Choice Over Time. New York: Russell Sage Foundation; 1992. [Google Scholar]
- Elster J. Ulysses Unbound. Cambridge: Cambridge University Press; 1999. [Google Scholar]
- Elster J. Proverbes, maximes, emotions. P.U.F. 2003. Un plaidoyer pour les mécanismes; pp. 25–82. [Google Scholar]
- Feldman SR, Chen GJ, Hu JY, et al. Effects of systematic asymmetric discounting on physician-patient interactions: a theoretical framework to explain poor compliance with lifestyle counseling. BioMed Central (BMC) Medical Informatics and Decision Making. 2002;2:8. doi: 10.1186/1472-6947-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, Attitude, Intention and Behavior. Don Mills, NY: Addison-Wesley; 1975. [Google Scholar]
- Frankfurt HG. The Importance of What We Care About. Cambridge: Cambridge University Press; 1988. p. 83. [Google Scholar]
- Frankfurt HG. The Reasons of Love. Princeton: Princeton University Press; 2004. [Google Scholar]
- Gjelsvik O. Getting Hooked: Rationality and addiction. In: Elster J, Skog J-O, editors. Addiction, weakness of will and relapse. Cambridge: Cambridge University Press; 1999. [Google Scholar]
- Holton R. How is strength of will possible? In: Stroud S, Tappolet C, editors. Weakness of Will and Practical Irrationality. Oxford: Clarendon Press; 2003. pp. 39–67. [Google Scholar]
- Hume D. A Treatise of Human Nature: Being an attempt to introduce the experimental method of reasoning into moral subjects. [online] 1740. [Accessed on 9 Jan, 2008]. URL: http://www.gutenberg.org/etext/4705.
- Kim J. Physicalism, or Something Near About. Princeton: Princeton University Press; 2005. pp. 9–10. [Google Scholar]
- Leventhal H, Falconer Lambert J, Diefenbach M, et al. From compliance to social-self-regulation: models of the compliance process. In: Blackwell B, editor. Treatment Compliance and the Therapeutic Alliance. Harwood Academic Publishers; 1997. pp. 21–26. [Google Scholar]
- Lopez-Azpiazu I, Martinez-Gonzalez MA, Kearney J, et al. Perceived barriers of, and benefits to, healthy eating reported by a Spanish national sample. Public Health Nutr. 1999;2:209–15. doi: 10.1017/s1368980099000269. [DOI] [PubMed] [Google Scholar]
- Lutfey KE, Wishner WJ. Beyond “compliance” is “adherence”, improving the prospect of diabetes care. Diabetes Care. 1999;22:635–39. doi: 10.2337/diacare.22.4.635. [DOI] [PubMed] [Google Scholar]
- McNabb WL. Adherence in diabetes: can we define it and can we measure it? Diabetes Care. 1997;20:216–18. doi: 10.2337/diacare.20.2.215. [DOI] [PubMed] [Google Scholar]
- Meichenbaum D, Turk DC. Facilitating Treatment Adherence. New York: Plenum Press; 1987a. Factors affecting adherence; pp. 41–68. [Google Scholar]
- Meichenbaum D, Turk DC. Facilitating Treatment Adherence. New York: Plenum Press; 1987b. Behavior modification approaches; pp. 149–184. [Google Scholar]
- Mele AR. An Essay on Akrasia, Self-deception and Self-control. Oxford: Oxford Univesity Press; 1987. p. 4. [Google Scholar]
- Nozick R. The Nature of Rationality. Princeton: Princeton University Press; 1993. p. 40. [Google Scholar]
- Olmsted MP, McFarlane T. Body weight and body image. BMC Womens Health. 2004;4(Suppl 1):S5. doi: 10.1186/1472-6874-4-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pears D. Motivated irrationality. South Bend, IN: St. Augustine’s Press; 1998. p. 1. [Google Scholar]
- Perros P, Deary IJ, Frier BM. Factors influencing preference of insulin regimen in people with type 1 (insulin-dependent) diabetes. Diabetes Res Clin Pract. 1998;39:23–9. doi: 10.1016/s0168-8227(97)00109-5. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking : Toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–5. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Reach G. Application de la théorie causale de l’action à l’analyse de la non-observance thérapeutique. Presse Médicale. 2000;29:1939–46. [PubMed] [Google Scholar]
- Reach G, Zerrouki A, Leclercq D, et al. Adjusting insulin doses: from knowledge to decision. Patient Educ Couns. 2005a;56:98–103. doi: 10.1016/j.pec.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Reach G. Role of habit in adherence to medical treatment. Diabet Med. 2005b;22:415–20. doi: 10.1111/j.1464-5491.2004.01449.x. [DOI] [PubMed] [Google Scholar]
- Reach G. Préface de Pascal Engel, Le Bord de l’Eau. 2007. Pourquoi se soigne-t-on, Enquête sur la rationalité morale de l’observance. 2ème édition revue et augmentée. [Google Scholar]
- Rorty A. Self-deception, akrasia, and irrationality. Soc Sci Info. 1980;19:193–212. [Google Scholar]
- Ruggiero L, Spirito A, Bond A, et al. Impact of social support and stress on compliance in women with gestational diabetes. Diabetes Care. 1990;13:441–3. doi: 10.2337/diacare.13.4.441. [DOI] [PubMed] [Google Scholar]
- Sackett DL. Introduction. In: Sackett DL, Haynes RB, editors. Compliance with Therapeutic Regimens. Baltimore: The John Hopkins University Press; 1979. [Google Scholar]
- Safford MM, Russell L, Suh DC, et al. How much time do patients with diabetes spend on self-care? J Am Board Fam Pract. 2005;18:262–70. doi: 10.3122/jabfm.18.4.262. [DOI] [PubMed] [Google Scholar]
- Self R, Oates P, Pinnock-Hamilton T, et al. The relationship between social deprivation and unilateral termination (attrition) from psychotherapy at various stages of the health care pathway. Psychol Psychother. 2005;78:95–111. doi: 10.1348/147608305X39491. [DOI] [PubMed] [Google Scholar]
- Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ. 2006;333:15–20. doi: 10.1136/bmj.38875.675486.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg LI, Desai JR, O’Connor PJ, et al. Diabetic patients who smoke: are they different? Ann Fam Med. 2004;2:26–32. doi: 10.1370/afm.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele CM, Josephs RA. Alcohol myopia. Its prized and dangerous effects. Am Psychologist. 1990;45:921–33. doi: 10.1037//0003-066x.45.8.921. [DOI] [PubMed] [Google Scholar]
- Stilley CS, Lawrence K, Bender A, et al. Maturity and adherence in adolescent and young adult heart recipients. Pediatr Transplant. 2006;10:323–30. doi: 10.1111/j.1399-3046.2005.00473.x. [DOI] [PubMed] [Google Scholar]
- Tappolet C. Emotions and the intelligibility of akratic action. In: Stroud S, Tappolet C, editors. Weakness of Will and Practical Irrationality. Oxford: Oxford University Press; 2003. [Google Scholar]
- Toljamo M, Hentinen M. Adherence to self-care and social support. J Clin Nurs. 2001;10:618–27. doi: 10.1046/j.1365-2702.2001.00520.x. [DOI] [PubMed] [Google Scholar]
- Triandis HC. Page MM, editor. Values, attitudes and interpersonal behavior. Nebraska Symposium on Motivation. 1979;27:195–260. [PubMed] [Google Scholar]
- Vaz MJ, Barros SM, Palacios R, et al. VIH HIV-infected pregnant women have greater adherence with antiretroviral drugs than non-pregnant women. Int J STD AIDS. 2007;18:28–32. doi: 10.1258/095646207779949808. [DOI] [PubMed] [Google Scholar]
- Wallston BS, Wallston KA. Locus of control and health: a review of the literature. Health Educ Monographs. 1978:107–17. doi: 10.1177/109019817800600102. [DOI] [PubMed] [Google Scholar]
- Watson G. Skepticism about weakness of will. Phil Rev. 1977;86:316–39. [Google Scholar]
- [WHO] World Health Organization. Adherence to long term therapies, time for action. Geneva: World Health Organization; 2003. [Google Scholar]
- Ziebland S, Thorogood M, Yudkin P, et al. Lack of willpower or lack of wherewithal? “Internal” and “external” barriers to changing diet and exercise in a three year follow-up of participants in a health check. Soc Sci Med. 1998;46:461–5. doi: 10.1016/s0277-9536(97)00190-1. [DOI] [PubMed] [Google Scholar]