Abstract
Radiation-induced apoptosis (RiA) is used therapeutically for tumor cell ablation as well as a tool to characterize hemopoietic cell lineages. We report that the peritoneal B-1 B cell subset is selectively resistant to RiA. Inherent radioresistance is not shared by splenic B-2 or B-1 cells. However, it is conferred upon B-2 cells by BCR crosslinking in the presence of IL-6 or IL-10. In vivo experiments with gene-targeted mice confirm that IL-6 and, to a lesser extent, IL-10 are the relevant stimuli that combine with BCR ligands to promote B-1 cell radioresistance. STAT3 promotes cell survival in response to selected growth factors, and is activated by combined BCR crosslinking and IL-6 (IL-10). Importantly, STAT3−/− B-1 cells become susceptible to irradiation, indicating that STAT3 activation by the BCR in the presence of IL costimuli account for the inherent radioresistance of peritoneal B-1 B cells.
In contrast to mature recirculating B cells (also referred to as conventional or “B-2” cells), the B-1 B cell subset predominates in the peritoneal cavity (PeC)3 and produces an abundance of protective natural Ab (1). Recent studies have identified CD19+CD45Rlow/negative progenitor cells in the fetal liver and adult bone marrow as preferentially giving rise to the CD5+ B-1a and CD5− B-1b subsets, respectively (2). This study supports earlier work suggesting that commitment to the B-1 lineage occurs before expression of the BCR (3). However, expression of particular VH and VL combinations encodes specificity for internal Ags such as Thy-1 or phosphatidylcholine, leading to Ag-driven expansion and maintenance of particular B-1 cell clonotypes (4–6).
Analysis of natural and induced mouse mutants provides an opportunity to identify signaling components that differentially regulate B-1 vs B-2 cell commitment, expansion, and survival. From such studies, it has become apparent that impairments in tonic BCR signaling cause a preferential reduction in the B-1 cell compartment (1). This conclusion seems at odds with the general observation that B-1 cells are hyporesponsive to BCR signaling. However, in vitro measurements address acute effects of Ag stimulation, which contrasts with chronic Ag stimulation thought to drive B-1 expansion and maintenance in vivo. Interestingly, peritoneal B-1 cells constitutively express an active form of the STAT3, which is essential for IL-6/IL-10 signaling and serine phosphorylated upon BCR engagement (7, 8). In this study, we report that B-1 cells are selectively resistant to ionizing radiation-induced apoptosis (RiA), and determine the integrated roles of Ag, IL-6/IL-10, and STAT3 in this response.
Materials and Methods
Animals
Mice were obtained from the following sources: wild type (WT), IL-6−/− (B6;129S2-Il6tm1Kopf/J), and IL-10−/− (B6.129P2-Il10tm1Cgn/J) from The Jackson Laboratory; STAT1−/− (129S6/SvEvTac-Stat1tm1Rds/Tac) from Taconic Farms; STAT5a/b−/− (129-Stat5atm1JniStat5btm2Jni) from Dr. J. Ihle (St. Jude’s Children’s Hospital, Memphis, TN), and VH12 (Tg(Igh-V12CH27/Igh-6)6–1Shc) from S. Clarke (University of North Carolina at Chapel Hill, Chapel Hill, NC). Mice lacking STAT3 (129-Stat3tm1Vpo) in B cells have been described (9, 10). Animals were housed and handled in accordance with protocols approved by the Institutional Animal Care and Use Committee of the University of California, San Diego. For irradiation experiments, mice were exposed to 5–10 Gy gamma irradiation from a cesium source and apoptosis measured in cell populations 24–72 h later.
Cell culture
B cells from 6- to 8-wk-old mice were obtained from the PeC by lavage or single cell suspensions made from spleen. Splenic B-2 cells were purified by negative selection using anti-CD43 beads (Miltenyi Biotec). Cells were cultured at 1 × 106 cells/ml in complete RPMI 1640 and stimulated with indicated concentrations of anti-IgM F(ab′)2 (Jackson ImmunoResearch), IL-6 (PeproTech), and IL-10 (PeproTech).
Flow cytometry
Single-cell suspensions were prepared and RBC lysed with ACK buffer (0.15 M NH4Cl, 1 mM KHCO2, and 0.1 mM Na2EDTA, pH 7.4). Abs against the following surface markers were obtained from BD Pharmingen: IgD-FITC, IgM-allophycocyanin, CD23-PE, IL6Rα-PE, IL10RI-PE, and Annexin V-PE. Apoptotic cells were identified by flow cytometric analysis of sub-G0-G1 peaks after staining in 1 mM Tris (pH 8), 0.1% Triton X-100, 0.1% sodium citrate, 0.1 mM EDTA, and 50 µg/ml propidium iodide (PI).
Results and Discussion
B-1 cells are resistant to gamma radiation-induced apoptosis
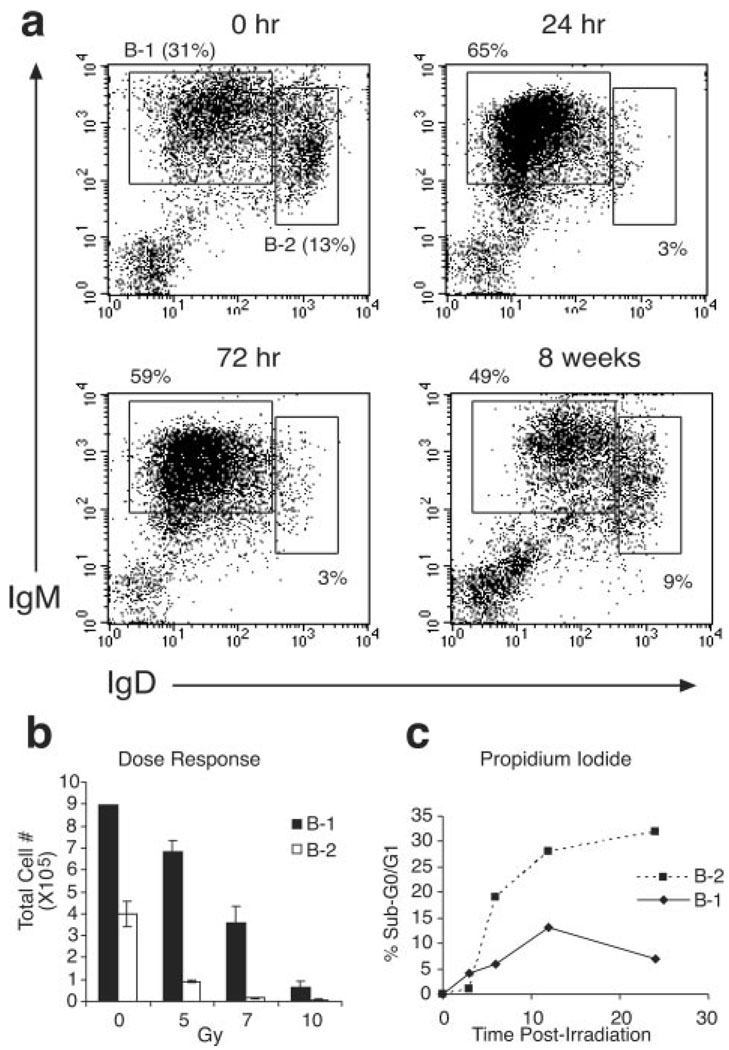
The use of bone marrow reconstitution for adoptive or autoreconstitution studies is based on the premise that progenitor and mature hemopoietic cells are relatively susceptible to ionizing radiation, whereas non-cycling stem cells are resistant. Similar to hemopoietic stem cells (HSCs), B-1 cells are also known to be long-lived self-renewing cells (1). To determine whether B-1 cells share the property of radioresistance with HSCs, mice were irradiated, and the composition of the B cell compartment was examined by flow cytometry. Importantly, B-1 cells persisted in the PeC for weeks following sublethal (5 Gy) irradiation (Fig. 1, a and b). Bromodeoxyuridine labeling studies confirmed that these cells were not newly generated from the proliferative expansion of a small subset of pre-existing or immigrating B cells (data not shown). By comparison, B-2 cells are eliminated from the PeC as well as the spleen at early time points, but re-emerge after 8 wk as a result of autoreconstitution by bone marrow stem cells (Fig. 1a and data not shown). Lethal (10 Gy) doses of irradiation eliminated all B-2 cells and the vast majority of B-1 cells (Fig. 1b).
FIGURE 1.
Murine B-1 cells are radioresistant. a, Flow cytometry profiles of peritoneal B-1 (IgMhighIgDlow) and B-2 (IgMlowIgDhigh) cells at indicated time points postirradiation (5 Gy) (n = 6 mice). b, B cell recovery from PeC 48 h after indicated exposure (n = 3 per group). c, Kinetics of in vitro cell death determined by PI staining after 2 Gy exposure; representative of more than three experiments.
B-1 cells are not thought to efficiently repopulate from the bone marrow (1). Therefore, we reasoned that most B-1 cells present in the PeC at 8 wk postirradiation were also present before irradiation (Fig. 1a). To directly determine radioresistance of the B cell subsets, purified splenic B-2 cells and peritoneal B-1 cells were exposed to 2 Gy of irradiation and apoptosis tracked over time in vitro. B-2 cells were found to rapidly undergo apoptosis following irradiation, whereas B-1 cells maintained viability as measured by PI, Annexin V, and DiOC6 staining (Fig. 1c and data not shown). Thus, differentiation into the B-1 subset is associated with acquired radioresistance.
Microenvironment of the peritoneal cavity is critical for B-1 cell radioresistance
B-1 cells can be found in the spleen as well as the PeC and have been shown to differ in their responses to extracellular stimuli based upon anatomic location (6, 11, 12). Characterizing B-1 cells in the spleen is difficult due to their low frequency relative to B-2 cells and phenotypic similarity to marginal zone B cells. Therefore, to investigate whether splenic B-1 cells are similar to peritoneal counterparts in terms of radioresistance, we used mice expressing a rearranged Ig H chain transgene (VH12). This VH rearrangement is expressed in a high frequency of normal peritoneal B-1 cells and, when expressed as a transgene, drives uncommitted B cells into the B-1 cell compartment (5). VH12 mice were exposed to 5Gy irradiation and the number of B-1 cells in the spleen and PeC were compared relative to non-irradiated mice. Fig. 2a shows that while VH12 peritoneal B cells are radioresistant (like their endogenous counterparts in WT mice), splenic VH12 B-1 cells displayed similar radiation sensitivity to splenic B-2 cells. This finding suggests that the PeC represents a distinct environment that supports the survival of B-1 cells.
FIGURE 2.
Cytokines and cell activation contribute to B cell radioresistance. a, Recovery of splenic B-1 cells from VH12 transgenic mice 48 h postirradiation (5 Gy, n = 3 mice). b, Rescue of B-2 cells from RiA. Purified CFSE-labeled splenic B-2 cells were left untreated or stimulated with anti-IgM (10 µg/ml) and immediately injected i.p. or i.v. Recipient mice were irradiated (5 Gy) and transferred B cells from PeC or spleen were enumerated 24 h postirradiation. Graph represents percent cell recovery from irradiated mice compared with non-irradiated mice (n = 3 mice per group). c, In vitro rescue of B cells from RiA. Purified splenic B cells were irradiated (2 Gy) following an 18-h incubation with anti-IgM and/or IL-6. Apoptosis was measured by PI (sub-G0-G1) staining 24 h postirradiation; representative of four experiments. d, Expression levels of IL-6 and IL-10 receptor on ex vivo and stimulated (24 h) B cells; LPS (1 µg/ml), anti-CD40 (10 µg/ml), and anti-IgM (1 µg/ml). e, B cell recovery from the PeC of IL-6−/− and IL-10−/− mice. Relative numbers of B-1 (CD23negIgMhigh) and B-2 (CD23posIgMlow) cells were analyzed before and after (48 h) irradiation (5 Gy). Graph represents percent cell recovery from the PeC of irradiated mice compared with non-irradiated mice (average ± SEM of at least three mice per group).
Because B-1 cells in the spleen and B-2 cells in the PeC are both susceptible to gamma irradiation, we reasoned that BCR signaling and PeC-associated cytokine/growth factor responsiveness combine to establish the anti-apoptotic program in peritoneal B-1 cells. To test this hypothesis, purified splenic B-2 cells were stimulated with anti-IgM F(ab′)2 and immediately injected i.v. or into the PeC of syngeneic animals. Recipient mice were exposed to 5 Gy of irradiation within 1 h after the transfer and the efficiency of B-2 cell recovery (CFSE-labeled cells) measured at 24 h posttransfer. Fig. 2b shows that BCR-stimulation conferred survival to B-2 cells transferred into the PeC but not the spleen of irradiated recipients. No evidence of emigration from the PeC to the blood or secondary lymphoid tissues was detected following irradiation (data not shown). In addition, proliferative expansion cannot account for this effect since significant partitioning of the CFSE membrane dye was not observed (data not shown).
Whereas BCR engagement provided a significant survival advantage to B cells transferred into the PeC (Fig. 2b), we found that BCR stimulation in vitro offered minimal protection from RiA (Fig. 2c). This result suggests that the PeC provides an additional survival factor(s) acting in concert with the BCR. A defining feature of peritoneal B-1 cells, but not splenic B-1 or B-2 cells, is the expression of a transcriptionally active form of STAT3 (13). Given that IL-6 induces the up-regulation of STAT3-dependent prosurvival genes by binding to the IL-6Rα/gp130 complex (7), we sought to address the role of IL-6 in acquired B cell radioresistance. Indeed, splenic B-2 cells stimulated with varied concentrations of IL-6 and anti-IgM exhibited a synergistic protective effect from gamma irradiation (Fig. 2c). Despite its well-established role as a B cell growth and survival factor, IL-6 alone did not protect from RiA (Fig. 2c). To address the nature of this nonresponsiveness, we examined levels of the ligand-binding IL-6Rα-chain on the surface of resting and activated B-2 cells (Fig. 2d). IL-6Rα expression was not detected on freshly isolated resting B-2 cells, stimulation with LPS, anti-CD40, or anti-IgM up-regulated IL-6 receptor expression (Fig. 2d). Importantly, peritoneal and splenic (from VH12 mice) B-1 cells constitutively expressed high and low levels of IL-6Rα, respectively (Fig. 2d and data not shown). These findings provide an explanation for acquired radioresistance by IL-6/anti-IgM costimulation of B-2 cells, and are consistent with the in vivo requirements for B-1 cell radioresistance provided by the peritoneal environment.
In addition to IL-6, IL-10 also activates STAT3 by engaging the IL-10RI/RII complex. We found that splenic B-1 and B-2 cells expressed modest levels of IL-10RI that were up-regulated upon activation, whereas B-1 cells constitutively expressed high levels of IL-10RI, similar to IL-6Rα (Fig. 2d). If the cytokine environment of the PeC is indeed essential for resistance to RiA of B-1 cells, the absence of these cytokines should render B-1 cells more sensitive to the effects of irradiation. To test this hypothesis, we exposed IL-6−/− and IL-10−/− mice to sublethal doses of irradiation and evaluated the number of B-1 cells remaining 48 h postirradiation. Both IL-6−/− and IL-10−/− mice possessed normal numbers of peritoneal B-1 and B-2 cells (Fig. 2e). Following irradiation, B-2 cells were preferentially lost, resulting in a relative increase in the percentage of B-1 cells in all mice (Fig. 2e). However, the absolute number of B-1 cells from IL-6−/− mice was substantially reduced compared with non-irradiated mice, indicating that peritoneal B-1 cells become susceptible to RiA in the absence of IL-6. A similar but less dramatic effect was observed in IL-10−/− mice (Fig. 2e). These results underscore the importance of the cytokine environment, and IL-6 and IL-10 in particular, in promoting B-1 cell protection from RiA.
STAT3 activation is necessary for B-1 cell radioresistance
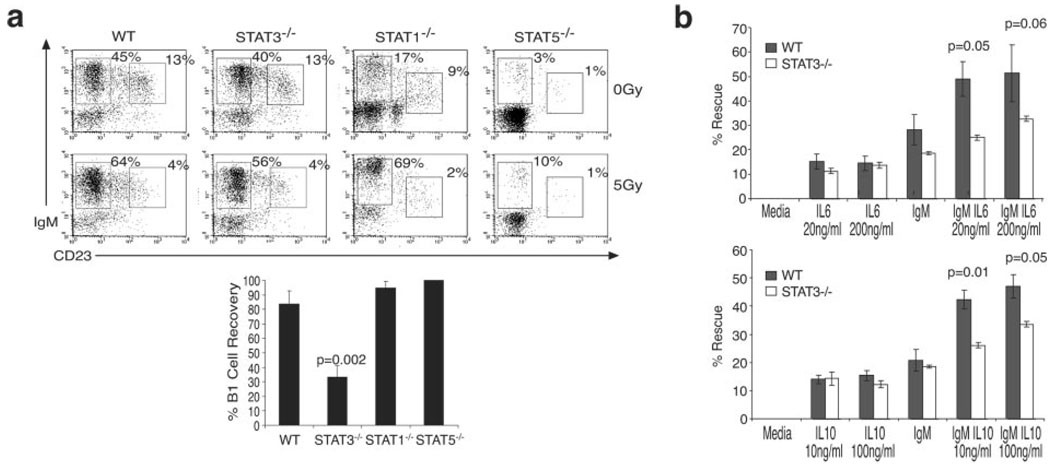
IL-10 signals through STAT1, STAT5, and STAT3, whereas IL-6 primarily activates STAT3. B-1 cells in the PeC express constitutively phosphorylated STAT3 and STAT1 (13), presumably due to stimulation by cytokines present in the PeC. It has been reported that anti-Ig and IL-6/IL-10 synergize in the activation of STAT3 (14), consistent with our hypothesis that BCR engagement in the presence of IL-6/IL-10 protects B cells from RiA via activation of STAT3. To directly determine whether this is the case, we ablated STAT3 in the B lineage by crossing mice bearing a loxP-flanked Stat3 gene with mice expressing the Cre recombinase gene under the control of the B cell-specific Cd19 promotor (9, 10). Importantly, B-1 cells were maintained in the PeC of conditional STAT3−/− mice, albeit at a somewhat lower frequency, but were significantly more susceptible to RiA than strain/age-matched WT counterparts (Fig. 3a).
FIGURE 3.
B-1 cell radioresistance requires STAT3. a, B cell recovery from the PeC of STAT3−/−, STAT1−/−, and STAT5a/b−/− mice. Relative numbers of B-1 and B-2 cells were determined before and after (48 h) irradiation (5 Gy). Graph represents percent cell recovery from the PeC of irradiated mice compared with non-irradiated mice (average ± SEM of at ≥3 mice per group). b, Impaired in vitro rescue of STAT3−/− B cells from RiA. Purified splenic B cells from WT and STAT-3−/− mice were cultured (18 h) in the presence of anti-IgM and/or IL-6 (top) or anti-IgM/IL-10 (bottom), irradiated (2 Gy), and apoptosis measured by PI (sub-G0-G1) staining 24 h postirradiation; representative of three experiments (mean ± SEM).
In addition to homodimers, STAT3 can form heterodimers with STAT1, and to a lesser extent with STAT5. Therefore, to assess the specificity of the STAT3 defect in RiA, the B-1 cell compartment was also examined in STAT1−/− and STAT5a/b−/− mice. Unlike conditional STAT3−/− mice, both STAT1−/− and STAT5a/b−/− mice showed significantly reduced numbers of peritoneal B cells (Fig. 3a). The B cell defect in STAT5a/b−/− mice is likely attributed to impaired IL-7R signaling in early B cell development (15, 16), whereas a B-1 cell defect has not been previously noted in STAT1−/− mice. Nonetheless, it appears that neither STAT1 nor STAT5a/b has a clear role in B-1 cell RiA (Fig. 3a), illustrating that this is a unique property of STAT3.
We have shown that costimulation of splenic B-2 cells with anti-IgM and IL-6/IL-10 confers radioresistance (Fig. 2). To determine whether this acquired property is STAT3-dependent, B-2 cells from WT and STAT3−/− mice were cultured overnight in the presence of IL-6/IL-10 and/or anti-IgM, irradiated (2 Gy) and viability assessed 24 h postirradiation (Fig. 3b). Both IL-6 and IL-10 were found to synergize with anti-IgM treatment in protecting B-2 cells from RiA. This effect was largely dependent on STAT3, which was not detectable in splenic B-2 cells from STAT3−/− mice (data not shown). Therefore, STAT3 appears to actively repress RiA downstream of IL-6 and IL-10 in Ag-experienced peritoneal B-1 cells, a condition that can be reproduced in B-2 cells through costimulation of the BCR and the IL-6R or IL-10R complexes.
Our data demonstrate that B-1 cell radioresistance is a property of B-1 cells conferred by Ag recognition in the context of the cytokine microenvironment of the PeC. BCR crosslinking induces up-regulation of IL-6Rα, allowing for synergistic activation of STAT3 by the BCR and IL-6R. IL-6 and IL-10 activate STAT3 via the Jak kinases, which phosphorylate STAT3 at Tyr705, resulting in dimerization and nuclear translocation (7). We previously found that BCR engagement selectively induces STAT3 Ser727 phosphorylation in the absence of Tyr705 phosphorylation (8). This modification augments transcriptional activation of STAT3 in the context of Tyr705 phosphorylation (17). In its homodimeric form, STAT3 has oncogenic potential (18, 19), likely through the up-regulation of target pro-survival genes such as bcl-2, bcl-xL, and mcl-1, or down-regulation of fas. Thus, B cell malignancies should be considered for emerging clinical applications for STAT3 inhibitors.
Acknowledgments
We thank Dr. J. Ihle and Dr. S. Clarke for provision of the STAT5a/b−/− and VH12 mice, respectively; Dr. G. Kansas for facilitating the transfer of the STAT3loxP mice, and Dr. I. Pedersen and members of the Rickert laboratory for discussions and critical reading of the manuscript.
Footnotes
This work was supported by an American Cancer Society Research Scholar Award (to R.C.R.), a Concern Foundation Junior Faculty Award (to R.C.R.), an Italian Cancer Research Association (AIRC) grant (to V.P.), and National Institutes of Health Grant NCICA80105 (to M.D.). D.C.O. is supported by National Institutes of Health Training Grant T32 CA09523.
Abbreviations used in this paper: PeC, peritoneal cavity; RiA, radiation-induced apoptosis; HSC, hematopoietic stem cell; PI, propidium iodide; WT, wild type.
Disclosures
The authors have no financial conflict of interest.
References
- 1.Berland R, Wortis HH. Origins and functions of B-1 cells with notes on the role of CD5. Annu. Rev. Immunol. 2002;20:253–300. doi: 10.1146/annurev.immunol.20.100301.064833. [DOI] [PubMed] [Google Scholar]
- 2.Montecino-Rodriguez E, Leathers H, Dorshkind K. Identification of a B-1 B cell-specified progenitor. Nat. Immunol. 2006;7:293–301. doi: 10.1038/ni1301. [DOI] [PubMed] [Google Scholar]
- 3.Hardy RR, Hayakawa K. A Developmental Switch in B Lymphopoiesis. PNAS. 1991;88:11550–11554. doi: 10.1073/pnas.88.24.11550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayakawa K, Asano M, Shinton SA, Gui M, Allman D, Stewart CL, Silver J, Hardy RR. Positive selection of natural autoreactive B cells. Science. 1999;285:113–116. doi: 10.1126/science.285.5424.113. [DOI] [PubMed] [Google Scholar]
- 5.Arnold LW, Pennell CA, McCray SK, Clarke SH. Development of B-1 cells: segregation of phosphatidyl choline-specific B cells to the B-1 population occurs after immunoglobulin gene expression. J. Exp. Med. 1994;179:1585–1595. doi: 10.1084/jem.179.5.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chumley MJ, Dal Porto JM, Kawaguchi S, Cambier JC, Nemazee D, Hardy RR. A VH11V kappa 9 B cell antigen receptor drives generation of CD5+ B cells both in vivo and in vitro. J. Immunol. 2000;164:4586–4593. doi: 10.4049/jimmunol.164.9.4586. [DOI] [PubMed] [Google Scholar]
- 7.Levy DE, Lee CK. What does Stat3 do? J. Clin. Invest. 2002;109:1143–1148. doi: 10.1172/JCI15650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Su L, Rickert RC, David M. Rapid STAT phosphorylation via the B cell receptor. Modulatory role of CD19. J. Biol. Chem. 1999;274:31770–31774. doi: 10.1074/jbc.274.45.31770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fornek JL, Tygrett LT, Waldschmidt TJ, Poli V, Rickert RC, Kansas GS. Critical role for Stat3 in T-dependent terminal differentiation of IgG B cells. Blood. 2006;107:1085–1091. doi: 10.1182/blood-2005-07-2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alonzi T, Maritano D, Gorgoni B, Rizzuto G, Libert C, Poli V. Essential role of STAT3 in the control of the acute-phase response as revealed by inducible gene inactivation [correction of activation] in the liver. Mol. Cell Biol. 2001;21:1621–1632. doi: 10.1128/MCB.21.5.1621-1632.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chumley MJ, Dal Porto JM, Cambier JC. The Unique Antigen Receptor Signaling Phenotype of B-1 Cells Is Influenced by Locale but Induced by Antigen. J. Immunol. 2002;169:1735–1743. doi: 10.4049/jimmunol.169.4.1735. [DOI] [PubMed] [Google Scholar]
- 12.Tumang JR, Hastings WD, Bai C, Rothstein TL. Peritoneal and splenic B-1 cells are separable by phenotypic, functional, and transcriptomic characteristics. Eur. J. Immunol. 2004;34:2158–2167. doi: 10.1002/eji.200424819. [DOI] [PubMed] [Google Scholar]
- 13.Karras JG, Wang Z, Huo L, Howard RG, Frank DA, Rothstein TL. Signal transducer and activator of transcription-3 (STAT3) is constitutively activated in normal, self-renewing B-1 cells but only inducibly expressed in conventional B lymphocytes. J. Exp. Med. 1997;185:1035–1042. doi: 10.1084/jem.185.6.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan H, Rothstein TL. Lymphokine dependence of STAT3 activation produced by surface immunoglobulin cross-linking and by phorbol ester plus calcium ionophore treatment in B cells. Eur. J. Immunol. 2001;31:665–671. doi: 10.1002/1521-4141(200102)31:2<665::aid-immu665>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Sexl V, Piekorz R, Moriggl R, Rohrer J, Brown MP, Bunting KD, Rothammer K, Roussel MF, Ihle JN. Stat5a/b contribute to interleukin 7-induced B-cell precursor expansion, but abl- and bcr/abl-induced transformation are independent of stat5. Blood. 2000;96:2277–2283. [PubMed] [Google Scholar]
- 16.Yao Z, Cui Y, Watford WT, Bream JH, Yamaoka K, Hissong BD, Li D, Durum SK, Jiang Q, Bhandoola A, Hennighausen L, O’Shea JJ. Stat5a/b are essential for normal lymphoid development and differentiation. Proc. Natl. Acad. Sci. USA. 2006;103:1000–1005. doi: 10.1073/pnas.0507350103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wen Z, Zhong Z, Darnell JE., Jr Maximal activation of transcription by Stat1 and Stat3 requires both tyrosine and serine phosphorylation. Cell. 1995;82:241–250. doi: 10.1016/0092-8674(95)90311-9. [DOI] [PubMed] [Google Scholar]
- 18.Bromberg JF, Wrzeszczynska MH, Devgan G, Zhao Y, Pestell RG, Albanese C, Darnell JE., Jr Stat3 as an oncogene. Cell. 1999;98:295–303. doi: 10.1016/s0092-8674(00)81959-5. [DOI] [PubMed] [Google Scholar]
- 19.Turkson J, Bowman T, Garcia R, Caldenhoven E, De Groot RP, Jove R. Stat3 activation by Src induces specific gene regulation and is required for cell transformation. Mol. Cell Biol. 1998;18:2545–2552. doi: 10.1128/mcb.18.5.2545. [DOI] [PMC free article] [PubMed] [Google Scholar]