Abstract
Background
Prior studies have shown an association between fast food restaurants and adolescent body size. Less is known about the influence of neighborhood food stores on a child's body size. We hypothesized that in the inner-city, minority community of East Harlem, New York, the presence of convenience stores and fast food restaurants near a child's home is associated with increased risk for childhood obesity as measured by body mass index (BMI).
Design/Methods
Baseline data of 6-8 year old East Harlem boys and girls (n=323) were utilized. Anthropometry (height and weight) were conducted with a standardized protocol. Food store data were collected via a walking survey. Stores located within the same Census block as the child's home address were identified using ArcGIS 8.3. We computed age- and sex-specific BMI-percentiles using CDC national norms. Using odds ratios, we estimated risk of a child's BMI-percentile being in the top tertile based on number and types of food stores on their Census blocks.
Results
Convenience stores were present in 55% of the surveyed blocks in which a study participant lived, and fast food restaurants were present in 41%. Children (n=177) living on a block with one or more convenience stores (range 1-6) were more likely to have a BMI-percentile in the top tertile (odds ratio 1.90, 95% CI 1.15-3.15), compared with children having no convenience stores (n=146).
Conclusions
The presence of convenience stores near a child's residence was associated with a higher BMI-percentile. This has potential implications for both child and neighborhood level childhood obesity interventions.
Keywords: Childhood Obesity, Food Store Availability, Inner City Neighborhood
Introduction
The childhood obesity epidemic is an increasing cause for national concern. Although a number of studies have demonstrated associations between availability of food stores and risk for obesity in adults,1,2 fewer studies have assessed impacts on children. Enhanced understanding of disparities in neighborhood food store availability may help in part explain racial/ethnic and socio-economic disparities in childhood obesity.
Low income, minority communities are particularly at risk for obesity, the very same communities that have limited access to grocery stores and supermarkets and increased access to fast food stores. Studies across the United States including Chicago,3 Detroit,4 and Los Angeles5 all demonstrate that lower socioeconomic and minority neighborhoods have fewer supermarkets. Meanwhile studies from New Orleans, Louisiana to Canada and Australia have demonstrated more fast food stores in low income neighborhoods compared to higher income neighborhoods.6-8
Low SES populations have less access to healthy foods to meet dietary guidelines. In a study comparing East Harlem, New York to the higher socioeconomic and predominantly white Upper East Side, only 18% of East Harlem stores carried foods recommended for diabetics, compared with 58% of the Upper East Side stores.9 In a separate study comparing two neighborhoods of Brooklyn, New York, predominantly black area stores carried canned and frozen fruits and vegetables whereas white neighborhood stores more typically offered fresh and organic produce.10 These studies highlight the community level barriers residents may face when trying to meet basic nutritional recommendations.
Why does this all matter? Food store availability, and supermarket availability in particular, has been shown to affect both dietary quality and body size as measured by body mass index (BMI). Residents without supermarkets close to their homes were 25-46% less likely to have a healthy diet than study participants who lived in areas of high supermarket density.11 Moreover, decreased neighborhood access to large, chain supermarkets was associated with higher BMI in adults.12
Less is known about the influence of the inner city food environment on a child's body size. Kipke et al. demonstrated that children living in low-income neighborhoods of East Los Angeles had proportionately more fast-food restaurants than grocery stores within walking distance of schools, which suggests that children have easy access to fast food and limited access to healthy food options.13 The greater the number of fast-food restaurants and convenience stores in proximity to the home, the lower the child's intake of fruits and vegetables14 and the higher the BMI.15 As seen in adults, decreased availability of supermarkets has demonstrated correlations with higher BMI in children aged 3 to 18 years.16
The present study investigated the relationship between the urban food environment of East Harlem, NY and body size of minority children living there. Specifically, we wanted to explore the relationships between convenience stores and fast food restaurants, both potential sources of high fat, calorie dense foods, and the risk for childhood obesity. This study contributes to our understanding of how the local food environment factors into the childhood obesity epidemic.
Design/Methods
Baseline data from a 3 year longitudinal study of 6-8 year old East Harlem boys and girls (n=323) were utilized. Children were recruited as per an IRB approved protocol from the Mount Sinai Pediatrics Practice, East Harlem community health centers, community based organizations, and East Harlem schools. Boys and girls were eligible to participate if they were English or Spanish speaking and were residents of East Harlem, NY. Children with medical conditions involving endocrine disorders or other medical conditions that may be related to obesity were ineligible as these conditions can affect growth.
Dependent Variable
Anthropometry (height, weight) were conducted with a standardized protocol by trained interviewers.17,18 We computed age- and sex-specific body mass index (BMI)-percentiles based on the 2000 CDC Growth Charts for the United States which are used to define children as overweight (≥85th%ile and < 95th%ile for age and gender) and obese (≥95th%ile for age and gender). BMI percentiles were categorized into tertiles, ensuring sufficient sample size in each group to maintain sufficient power.19,20
Independent Variable
The unit for analysis for this study was the Census block, the smallest defined geographic area available. New York City Census blocks in general correspond to individual city blocks bounded by streets. Food store data on convenience stores, specialty stores, grocery stores, supermarkets, fast food restaurants and restaurants were collected via comprehensive walking survey of East Harlem Zip codes 10029 and 10035 in 2004. Food stores were classified as per the North American Industry Classification System (NAICS 2002) as previously reported.21 Stores located within the same Census block as the child's home address were identified using ArcGIS software version 8.3, which allowed for geocoding of both home and store address. Food stores and restaurants were measured as individual counts (0,1,2,…, x). Models were run separately for each type of food store/restaurant.
Statistical Analyses
Using odds ratios, we estimated risk of a child's BMI-percentile being in the top tertile for BMI based on the presence of certain types of food stores on their Census blocks. Odds ratios adjusted for gender, race/ethnicity, and family income, were calculated using the statistical software package SAS 9.1.
Results
Three hundred and twenty three children ages 6-8 years old enrolled in the study (see Table 1), with an even distribution amongst 6 year old (37%), 7 year old (31%) and 8 year old (32%) children. Seventy-one percent were female. Sixty-seven percent of the study participants were Hispanic, 18% were Black, and 15% were Black-Hispanic. The majority of household incomes (91%) were less than $49,999 and of those 60% had incomes less than $24,999, well below the 2008 US Census Bureau poverty line of $35,600 for a family of eight. Of the participants included in the study 40% of the girls and 50% of the boys had BMI's above the 85th percentile for age and gender as per CDC norms.
Table 1. Baseline Characteristics (n=323).
| Age in years | |
| 6 | 37% |
| 7 | 31% |
| 8 | 32% |
| Race | |
| Black | 18% |
| Hispanic | 67% |
| Black-Hispanic | 15% |
| Gender | |
| Female | 71% |
| Income | |
| <12,000 | 20% |
| 12-24,999 | 40% |
| 25-49,999 | 31% |
| 50-74,999 | 5% |
| 75-99,999 | 3% |
| 100,000+ | 1% |
| Overweight (BMI≥85th%ile) | |
| Girls | 40% |
| Boys | 50% |
| Mean BMI %ile by tertiles | |
| 1 | 33rd percentile |
| 2 | 76th percentile |
| 3 | 97th percentile |
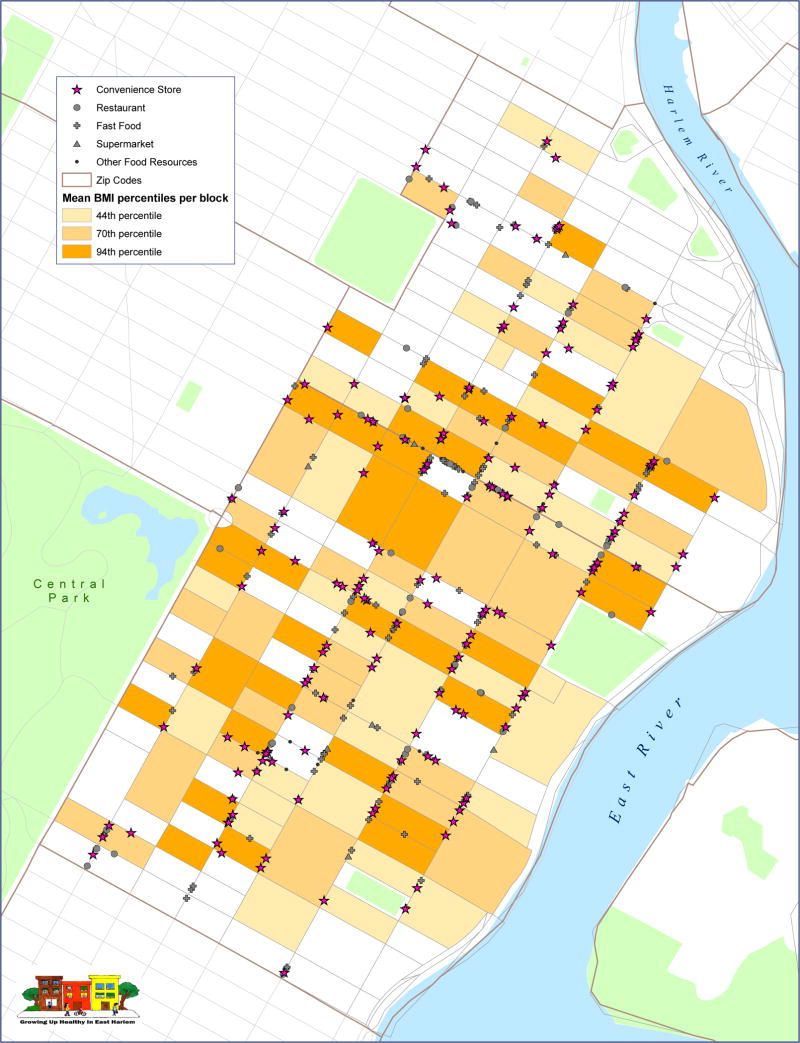
Convenience stores were present in 55% of the Census blocks on which a study participant lived (See Figure 1). Fast food restaurants were present in 41% of Census blocks. Sixty-six percent of the 323 children lived in Census blocks with no specialty stores, grocery stores, or restaurants. Mean BMI-percentiles for each tertile were 33rd percentile, 76th percentile, and 97th percentile, respectively. Statistically significant associations between BMI-percentile and number of specialty stores, grocery stores, supermarkets, fast food restaurants or restaurants on a child's Census block were not observed likely due to the small sample size (see Table 2). However, children (n=177) living on a block with one or more convenience stores (range 1-6) were more likely to have a BMI-percentile in the top tertile (odds ratio 1.90, 95% CI 1.15-3.15, p=0.01), than children living on a block with no convenience stores on their block of residence (n=146).
Figure 1.
Map of East Harlem Food Stores and Blocks by BMI In 2004, there were 168 convenience stores, 34 specialty stores, 8 grocery stores, 9 supermarkets, 139 fast food restaurants and 57 restaurants in East Harlem.
55% of children lived on a Census block with a convenience store and 41% had fast food restaurants present on their block. 66% of the 323 children lived in Census blocks with no specialty stores, grocery stores, supermarkets or restaurants.
Table 2. Adjusted Odds Ratios * of Child's BMI in Top Tertile by Food Store Availability.
| N | Percentage of blocks with store present | Odds Ratio (95% CI and p value) | |
|---|---|---|---|
| Convenience Stores | |||
| 0 | 146 | 45% | 1 |
| 1+ | 177 | 55% | 1. 90 (1.15, 3.15) p=0.01 |
| Specialty Stores | |||
| 0 | 282 | 87% | 1 |
| 1+ | 41 | 13% | 0.75 (0.39, 1.46) p=0.40 |
| Grocery Stores | |||
| 0 | 311 | 96% | 1 |
| 1 | 12 | 4% | 0.88 (0.30, 2.56) p=0.81 |
| Supermarkets | |||
| 0 | 301 | 93% | 1 |
| 1 | 22 | 7% | 1.09(0.47, 2.52) p=0.84 |
| Fast Food Restaurants | |||
| 0 | 192 | 59% | 1 |
| 1+ | 131 | 41% | 1.11 (0.71, 1.73) p=0.65 |
| Restaurants | |||
| 0 | 242 | 75% | 1 |
| 1+ | 81 | 25% | 1.26 (0.74, 2.14) p=0.40 |
Odds ratios adjusted for gender, race/ethnicity, and family income
Discussion
This study examined the relationship between neighborhood food stores and a child's body size. We found that in the inner-city, minority community of East Harlem, New York, presence of convenience stores on the block in which a child resides is associated with increased risk for childhood obesity as measured by BMI. These findings are supported by Powell et al. who found that greater availability of convenience stores in school Zip codes was significantly associated with higher BMI among 8th- and 10th-grade students15 and Morland et al who demonstrated similar findings in adults.22
Convenience stores provide ample opportunities for children to purchase and consume energy-dense foods. Several studies have reported that convenience stores lower healthy food consumption among children. Timperio et al. found that among 5-6 and 10-12 year-old Australian children, the more convenience stores located close to a child's home, the lower the likelihood of consuming fruit 2 or more times per day.14 Similar findings have been reported for boys ages 10-14 years old.23
There are several limitations to our study in addition to a small sample size, which we noted earlier. First, we were interested in the food environment of the Census block in which a child resides. When studying the impact of the food environment on BMI, it remains unclear what geographic boundaries are most precise for examining a child's food habits. Geographic areas thus far used in research include the Census Block, Census Tract, Zip code or defined “buffer” zones that are within walking distance from the primary residence. Each of these geographic boundaries has intrinsic limitations. By restricting analyses to the Census block, we did not consider adjacency, i.e. food stores that were available on a neighboring block to where a child resides. Still, it remains significant that 55% of the children in our study had a convenience store and 41% had a fast food restaurant on the block in which they reside.
Analysis restricted to the Census block level provides a limited assessment of the entire scope of food environment exposures in a child's day to day life. We did not account for (1) exposures to food stores at different points in the course of a child's day, i.e. en route to and from school and after-school activities, (2) individual behaviors including frequency with which children are purchasing from stores on their block of residence, or (3) quantity and/or quality of purchases children are making at various food stores.
To deepen our understanding of how food store availability shapes a child's dietary behavior, further studies are needed across all racial/ethnic groups, socio-economic demographics, and geographic areas including urban, suburban, and rural settings to explain children's daily travel, purchasing, and consumption patterns in relation to the local food environment. Factors to explore in future research include what types of foods are available in stores and how they are displayed, advertised, and priced. These data would further enhance support for our findings that suggest that children who live near convenience stores may be at increased risk for obesity due to increased exposure to unhealthy foods.
Interestingly, we observed no statistically significant associations between a child's BMI and the number of fast food restaurants on a child's Census block. Existing studies that examined fast food restaurant availability report similar results.24,25 One issue is the classification of food stores and it remains unclear which elements are essential to defining food store types.
In summary, we found that convenience stores located on the Census block in which a child resides may influence a child's risk for obesity. This suggests that in addition to interventions targeting individuals, there is a role for community level changes to address the obesity epidemic. Every public health success over the course of the past several decades has employed a multifaceted approach. Novel approaches to tackling obesity have targeted access to unhealthy snacks. Some examples include: eliminating vending machines from schools nationwide, requiring fast food restaurants to post calorie counts, partnering with convenience stores to encourage stocking low-fat milk, reducing prices on healthy food items, and offering coupons to encourage shopping at green markets. Longitudinal studies examining the influence of neighborhood food stores can inform multifaceted obesity interventions that combine counseling families on children's neighborhood food purchasing behaviors with innovative food policy initiatives and urban planning that promote healthy communities.
Conclusions
The presence of convenience stores within the same Census block as a child's residence was associated with a higher BMI-percentile. Children living on a block with 1 or more convenience stores (range 1-6) were more likely to have a BMI-percentile in the top tertile (OR 1.90, 95% CI 1.15-3.15, p value 0.01) compared with children having no convenience stores on their block. This has potential implications for both child and neighborhood level interventions with respect to childhood obesity.
Acknowledgments
Special thanks to our community partners and collaborators including: Drs. Cherita Raines and Jessica Kobil, Susan Resnick at the NYCDOHMH, the Growing Up Healthy Community Advisory Board, North General Hospital, the Children's Aid Society at Dunlevy Milbank, Little Sisters of the Assumption Family Health Services, Union Settlement, School Based Health, Mount Sinai Pediatrics Associates, the Pediatric/Child Health Sub-Committee of the East Harlem Community Health Committee and the NYCDOHMH East Harlem District Public Health Office.
We are especially grateful to our colleagues at the Mount Sinai Center for Children's Environmental Health and Disease Prevention Research: Drs. Mary Wolff, Susan Teitelbaum, Kimberly Morland, Joel Forman, Luz Claudio and Philip Landrigan as well as the Growing Up Healthy families and staff: Rochelle Osborne, Maureen Miller, Ana Mejia, Jessica Gutierrez, Arkeyris Richiez, and Carla Torocolon.
“Growing up Healthy in East Harlem” is supported by the National Institute of Environmental Health Sciences (NIEHS Grant # 2 P01 ES009584), the Environmental Protection Agency (EPA Grant # P50 RD8317101), NIEHS/National Cancer Institute Grant (NCI Grant U01 ES012771), National Center for Research Resources (GCRC) NCRR Grant #MO1-RR-00071 and Agency for Toxic Substances and Disease Registry ATSDR Grant #ATU 300014.
Research Support:
National Institute of Environmental Health Sciences: Mary S. Wolff, PhD
- NIEHS Grant # 2 P01 ES009584
Environmental Protection Agency: Mary S. Wolff, PhD
- EPA Grant # P50 RD8317101
National Cancer Institute: Mary S. Wolff, PhD, Susan Teitelbaum, PhD
- NCI Grant U01 ES012771
National Center for Research Resources (GCRC): Hugh Sampson, MD
- NCRR grant #MO1-RR-00071
Agency for Toxic Substances and Disease Registry, Phil Landrigan, MD, Msc
- ATSDR Grant #ATU 300014
Footnotes
Potential Conflicts of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Inagami S, Cohen DA, Finch BK, Asch SM. You are where you shop: grocery store locations, weight, and neighborhoods. Am J Prev Med. 2006;31(1):10–17. doi: 10.1016/j.amepre.2006.03.019. [DOI] [PubMed] [Google Scholar]
- 2.Wang MC, Kim S, Gonzalez AA, MacLeod KE, Winkleby MA. Socioeconomic and food-related physical characteristics of the neighbourhood environment are associated with body mass index. J Epidemiol Community Health. 2007;61(6):491–498. doi: 10.1136/jech.2006.051680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alwitt L, Donley TD. Retail stores in poor urban neighborhoods. Journal of Consumer Affairs. 1997;31(1):139–164. [Google Scholar]
- 4.Zenk SN, Schulz AJ, Israel BA, James SA, Bao S, Wilson ML. Fruit and vegetable access differs by community racial composition and socioeconomic position in Detroit, Michigan. Ethn Dis. 2006;16(1):275–280. [PubMed] [Google Scholar]
- 5.Shaffer A. The Persistence of LA's Grocery Gap: The Need for a New Food Policy and Approach to Market Development. Los Angeles, CA: Center for Food and Justice, Urban and Environmental Policy Institute, Occidental College; 2002. [Google Scholar]
- 6.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: a geographic analysis. Am J Prev Med. 2004;27(3):211–217. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 7.Smoyer-Tomic KE, Spence JC, Raine KD, et al. The association between neighborhood socioeconomic status and exposure to supermarkets and fast food outlets. Health Place. 2008;14(4):740–754. doi: 10.1016/j.healthplace.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Reidpath DD, Burns C, Garrard J, Mahoney M, Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place. 2002;8(2):141–145. doi: 10.1016/s1353-8292(01)00028-4. [DOI] [PubMed] [Google Scholar]
- 9.Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health. 2004;94(9):1549–1554. doi: 10.2105/ajph.94.9.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morland K, Filomena S. Disparities in the availability of fruits and vegetables between racially segregated urban neighbourhoods. Public Health Nutr. 2007;10(12):1481–1489. doi: 10.1017/S1368980007000079. [DOI] [PubMed] [Google Scholar]
- 11.Moore LV, Diez Roux AV, Nettleton JA, Jacobs DR., Jr Associations of the local food environment with diet quality--a comparison of assessments based on surveys and geographic information systems: the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2008;167(8):917–924. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown AF, Vargas RB, Ang A, Pebley AR. The neighborhood food resource environment and the health of residents with chronic conditions: the food resource environment and the health of residents. J Gen Intern Med. 2008;23(8):1137–1144. doi: 10.1007/s11606-008-0601-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kipke MD, Iverson E, Moore D, et al. Food and park environments: neighborhood-level risks for childhood obesity in east Los Angeles. J Adolesc Health. 2007;40(4):325–333. doi: 10.1016/j.jadohealth.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 14.Timperio A, Ball K, Roberts R, Campbell K, Andrianopoulos N, Crawford D. Children's fruit and vegetable intake: associations with the neighbourhood food environment. Prev Med. 2008;46(4):331–335. doi: 10.1016/j.ypmed.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 15.Powell LM, Auld MC, Chaloupka FJ, O'Malley PM, Johnston LD. Associations between access to food stores and adolescent body mass index. Am J Prev Med. 2007;33(4 Suppl):S301–7. doi: 10.1016/j.amepre.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Liu GC, Wilson JS, Qi R, Ying J. Green neighborhoods, food retail and childhood overweight: differences by population density. Am J Health Promot. 2007;21(4 Suppl):317–325. doi: 10.4278/0890-1171-21.4s.317. [DOI] [PubMed] [Google Scholar]
- 17.Lohman TG, Roche AF, Martorell R, editors. Anthropometric Standardization Reference Manual. Champaign: Human Kinetics Books; 1991. [Google Scholar]
- 18.Wang J, Thornton JC, Kolesnik S, Pierson RN., Jr Anthropometry in body composition. An overview. Ann N Y Acad Sci. 2000;904:317–326. doi: 10.1111/j.1749-6632.2000.tb06474.x. [DOI] [PubMed] [Google Scholar]
- 19.Taylor GW, Becker MP. Increased efficiency of analyses: cumulative logistic regression vs ordinary logistic regression. Community Dent Oral Epidemiol. 1998;26(1):1–6. doi: 10.1111/j.1600-0528.1998.tb01916.x. [DOI] [PubMed] [Google Scholar]
- 20.Fuentes RM, Notkola IL, Shemeikka S, Tuomilehto J, Nissinen A. Tracking of body mass index during childhood: a 15-year prospective population-based family study in eastern Finland. Int J Obes Relat Metab Disord. 2003;27(6):716–721. doi: 10.1038/sj.ijo.0802271. [DOI] [PubMed] [Google Scholar]
- 21.Galvez MP, Morland K, Raines C, et al. Race and food store availability in an inner-city neighbourhood. Public Health Nutr. 2008;11(6):624–631. doi: 10.1017/S1368980007001097. [DOI] [PubMed] [Google Scholar]
- 22.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Jago R, Baranowski T, Baranowski JC, Cullen KW, Thompson D. Distance to food stores & adolescent male fruit and vegetable consumption: mediation effects. Int J Behav Nutr Phys Act. 2007;4:35. doi: 10.1186/1479-5868-4-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sturm R, Datar A. Body mass index in elementary school children, metropolitan area food prices and food outlet density. Public Health. 2005;119(12):1059–1068. doi: 10.1016/j.puhe.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 25.Burdette HL, Whitaker RC. Neighborhood playgrounds, fast food restaurants, and crime: relationships to overweight in low-income preschool children. Prev Med. 2004;38(1):57–63. doi: 10.1016/j.ypmed.2003.09.029. [DOI] [PubMed] [Google Scholar]