Abstract
Objective
To assess the association of anxiety and depression with psychosocial and asthma related functional impairment in a large population-based sample of adolescents with asthma.
Method
The sample consisted of 767 youths ages 11 to 17 with a documented diagnosis of, and active treatment for, asthma. Phone interviews were completed with each youth and one parent to assess asthma related symptoms and self-report of psychosocial and asthma related functional status. Structured diagnostic interviews (C-DISC) were administered to determine psychiatric diagnoses. Weighted multiple linear regression models were employed to identify variables that were independently and significantly associated with levels of functioning.
Results
125 youths (16.2%) met DSM-IV criteria for ≥1 anxiety and depressive disorders in the last 12 months. After controlling for demographic variables, greater severity of self-reported depressive and anxiety symptoms and presence of ≥1 DSM-IV anxiety or depressive diagnosis were associated, with psychosocial and asthma related functional status. The mental health factors were more strongly associated with measures of asthma and psychological functional outcomes than the modified HEDIS asthma risk measure.
Conclusions
Increased awareness of the need to assess and effectively treat psychiatric symptoms in youth with asthma may reduce the functional burden associated with asthma.
Keywords: asthma, anxiety, depression, adolescents, functional impairment, asthma severity
INTRODUCTION
Morbidity and mortality due to asthma have increased in recent years, particularly among children and teenagers [1] suggesting the need for improving both control and prevention measures [2]. Numerous patient characteristics have been found to influence functional impairment and health utilization (emergency room and inpatient admissions) associated with asthma, including age, poverty, gender, psychosocial factors, psychiatric disorders and ethnicity [3–6]. Co-existing medical conditions such as allergic rhinitis and sinusitis have been shown to play a role in determining functional impairment in youth and adults with asthma but the contribution of comorbid psychiatric conditions has received less attention.
Asthma in childhood and adolescence is associated with increased risk for depression and anxiety disorders [7–10]. In fact, some investigators propose that asthma, anxiety and depression “ are all the “consequence of dysregulation of physiologically critical biochemical pathways” in that the same neurotransmitters that regulate affect may be involved in processes such as bronchoconstriction and inflammation [11]. It has also been posited that childhood adversity and other family factors may play a significant role in increasing risk for both asthma and mental health problems [12].
Comorbid anxiety or depressive disorders in patients with asthma may have a significant impact on the youth’s ability to cope effectively with their asthma. Less active asthma management as reflected in nonadherence to medication, monitoring peak expiratory flow and recommendations to quit smoking, may worsen asthma symptom burden, increase medical utilization and costs and lead to increased functional impairment. Anxiety and depressive disorders may also directly impact a youth’s perception and interpretation of symptoms, which could in turn increase anxiety and decrease ability to actively manage asthma symptoms [13]. In turn, asthma symptoms may interfere with functioning and precipitate anxiety and depressive disorders [14]. A recent study showed that inner-city children with asthma who scored higher on a measure of psychological distress had more hospitalizations, more days of wheezing and lower functional status than those scoring lower on distress [15]. A more sophisticated understanding of the interplay between emotional distress and asthma is clearly needed.
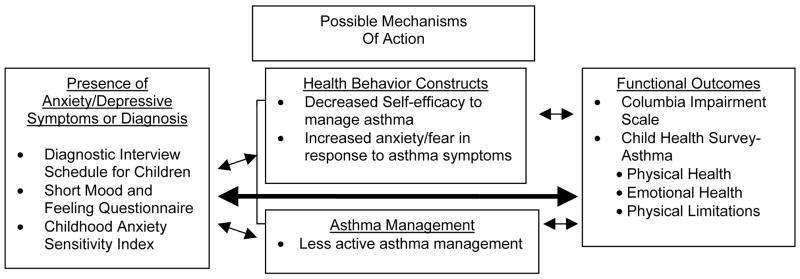
This paper begins to explicate the interaction of anxiety and depressive disorders and asthma by examining behavioral and asthma related functional outcomes in a large sample of adolescents with asthma enrolled in a health maintenance organization, while controlling for asthma severity using a standard measure. Both dichotomous (DSM-IV anxiety and depressive disorders ) and continuous measures of anxiety and depression are included. As depicted in Figure 1 we hypothesize that youth with comorbid asthma and ≥1 anxiety or depressive disorders will report more impairment in psychosocial and asthma related functional status than youth with asthma alone, even after controlling for asthma disease severity. Findings from this work will have significant implications for treatment. If these comorbidities are associated with poorer psychosocial and asthma related functional status then improved quality of treatment for anxiety and depressive disorders in patients with asthma may be one overlooked strategy which could lead to improved self-care, symptomatic, functional and medical outcomes..
Figure 1.
Model: Adverse Impact of ≥ 1 Anxiety/Depressive Disorder and Asthma Comorbidity
METHODS
Setting
The Stress and Asthma Research (STAR) study was developed by a multidisciplinary team of researchers working with a large nonprofit health maintenance organization (HMO) with 25 clinics with an additonal 75 contracted clinics. This HMO has mental health services that patients can either be referred to by their primary care physician or can self-refer to and computerized cost and accounting systems that have organized utilization and cost summaries of every enrollee since 1989. The study protocol was reviewed and approved by the cooperative’s institutional review board.
Sample Recruitment
Potential participants were identified from administrative data using the following criteria: 1) individuals between 11 and 17 years of age enrolled in an insurance plan for at least 6 months; 2) at least one of the following types of utilization in the prior year: a) hospitalized with an asthma diagnosis and ≥1 asthma prescriptions; b) ≥1 emergency room or urgent care visit with an asthma diagnosis and ≥ 1 asthma prescriptions; c) ≥2 office visits with an asthma diagnosis and ≥1 asthma prescriptions; d) only 1 asthma visit but ≥2 asthma prescriptions filled on different days; e) ≥4 prescriptions for asthma medication; f) ≥1 visit in the past year with an asthma diagnosis and another in the past 18 months and ≥1 asthma prescriptions. These criteria were developed to screen out patients with mild asthma (i.e. exercise induced only). Individuals diagnosed with bipolar disorder or schizophrenia were excluded.
Of the 1458 children/adolescents and parents in the initial sample, 1288 proved eligible. Following receipt of a letter inviting participation in the study, both the parent and the child/adolescent provided informed consent. They then completed a telephone interview that included a 10- to 15-minute parent interview and 45- to 75-minute child/adolescent interview. The parent interview included confirmation that their child had been diagnosed with asthma, use of asthma medication, questions about other mental health or behavioral problems, prior mental health diagnoses and treatment, and demographic questions. A total of 833 eligible parents gave consent and permission for us to contact their child/adolescent with asthma. Of these, we completed 781 child/adolescent interviews for a final recruitment rate of 60.6% adolescents. Twelve parents were unable to be interviewed so 59.7% parents (N = 769) completed the interview. Two youths did not complete the C-DISC 4.0, and 12 parents refused access to youth medical records. Our final propensity weighted (see below) sample sizes are 767 youth and 757 parents.
Characteristics of the final sample are depicted in Table 1; the mean age was 13.97 with a standard deviation of 1.93. 46.4% of the sample were female. The sample was 75% to 80% Caucasian and median household income based on zip codes and US census data was $50, 460 (SD = 17,015).
Table 1.
Demographics of youth with asthma (N = 767, unless otherwise specified)
| Total Sample N = 767 | Anxiety or Depressive Disorder (N=125) | No anxiety or depressive disorder (N = 642) | Test Statistics X2(1) or t(765) | |
|---|---|---|---|---|
| Gender (n(%)) | ||||
| Male | 411 (53.6) | 45 (36.0) | 366 (57) | X2 =17.73 (p < .001) |
| Female | 356 (46.4) | 86 (64.0) | 276 (43) | |
| Age (mean (SD)) | 13.97 (1.93) | 14.2 ± 2.0 | 14.0 ± 1.9 | 1.17 |
| Parental Education (n = 757) | ||||
| High School or Less | 61 (8.0) | 18 (14.8) | 43 (6.8) | X2 =7.76 (p = .005) |
| At least some college | 696 (92.0) | 104 (85.2) | 592 (93.2)) | |
| Race of Parent (n=754) (n (%)) | ||||
| White | 605 (80.3) | 91 (74.5) | 514 (81.4) | X2 =9.11 df = 4 (p = .06) |
| African-American | 48 (6.3) | 15 (12.3) | 33 (5.2) | |
| Asian & Pacific Islanders | 26 (3.5) | 3 (2.5) | 23 (3.6) | |
| Native American | 51 (6.8) | 9 (7.4) | 42 (6.6) | |
| Other | 24 (3.2) | 4 (3.3) | 20 (3.2) | |
| Any Parent Employed | 709 (93.7) | 110 (90.2) | 598 (94.30 | 2.14 |
| % of Families from Western Washington | 507 (66.1) | 83 (66.4) | 424 (66.0) | .01 |
| Median Income (GEO*) | 50,460 (17015)) | 47,211.8 (17842.0) | 51,091.0 (16806.4) | t (738) = 2.19 (p = .03) |
| Asthma Severity Measure | ||||
| Modified HEDIS** | ||||
| 0 | 535 (69.7) | 82 (65.6) | 453 (70.6) | 1.26 |
| 1 | 170 (22.2) | 32 (25.6) | 138 (21.5) | |
| 2+ | 62 (8.1) | 11 (8.8) | 51 (7.9) | |
| Self Report Measures | ||||
| Moods & Feeling Q | 3.7 (4.6) | 8.7 (5.9) | 2.6 (3.6) | t =10.73 (p < .001) |
| Anxiety Sensitivity Index | 11.7 (9.0) | 21.5 (11.5) | 9.8 (7.0) | t =11.02 (p < .001) |
| Columbia Impairment Scale | 11.2 (8.8) | 19.0 (9.4) | 9.7 (7.8) | t =10.42 (p < .001) |
| Child Health Survey for Asthma – | ||||
| Activities Subscale | 83.7 (17.1) | 74.2 (18.1) | 85.6 (16.2) | t =6.52 (p < .001) |
| Emotional Health Subscale | 83.8 (14.6) | 71.9 (17.4) | 86.2 (12.7) | t =8.71 (p < .001) |
| Physical Health Subscale | 73.7 (15.6) | 62.4 (16.4) | 75.9 (14.4) | t =8.56 (p < .001) |
GEO = the median household income based on census block group.
HEDIS = Health Plan Employer Data and Information Set criteria/definition of children/adolescents who are at high risk of adverse asthmatic events
Procedures
All survey contacts were conducted via telephone. At the time of interview, informed consent was obtained both from a parent and the youth study participant. The telephone interview included a 10 to 15 minute parent interview of the consenting parent and 45 to 75 minute child/adolescent interview. The parent interview included confirmation that their child had been diagnosed with asthma, use of asthma medication, questions about prior mental health diagnosis and treatment, and demographic questions. The child interview included a more in-depth assessment of asthma related symptoms and issues and psychological functional status.
Measures
Demographics
The parent interview included questions about the child’s race/ethnicity, education and employment status for both the responding parent and his/her partner, marital status of the responding parent, and number of children in the household. Child age and sex was obtained from administrative data and confirmed with the parent. The families’ address and zip code were used to develop a GEO code, which is the median household income based on census block group.
Psychiatric Diagnoses
The child/adolescent interview included the following measures. The Childhood Anxiety Sensitivity Index (ASI) [16, 7] is an 18-item self report measure which assesses fear of anxiety symptoms and catastrophic cognitions regarding bodily sensations. The ASI includes items such as “It scares me when my heart beats rapidly”.....when I become short of breath”; When I cannot keep my mind on a task, I worry that I might be going crazy”). High scores on the ASI in patients with asthma have been shown to correlate with anxiety comorbidity [16,17]. The Mood and Feelings Questionnaire [18] short form (SMFQ) is a 13-item questionnaire that codes symptoms on a 3-point scale (“true”, “sometimes true”, “not true”). Example items include “ I felt miserable or unhappy”; “I did not enjoy anything at all”; “ I felt that I was a bad person.”) This scale has been found to have high reliability and validity and the short form is made up of items that best discriminated depressed and non-depressed children in field trials using structured psychiatric interviews [18]. Other mental health and behavioral concerns including attention problems, rule-breaking behaviors, aggressive behavior and somatic complaints were assessed using the Child Behavior Checklist [19]
The child/adolescent interview also included a computer assisted telephone version of the depression and anxiety modules from the Diagnostic Interview Schedule for Children NIMH DISC-4.0 [20], a reliable and valid structured interview designed for lay interviewers to diagnose DSM-IV disorders in children and adolescents. Telephone versions of structured psychiatric interviews have been found to have a high correlation with in-person interviews [21, 22].
All interviewers received 12 hours of classroom and hands-on training, including project-specific training on the Computerized Diagnostic Interview Schedule for Children (C-DISC-4.0). The C-DISC-4.0 training leader (EM) completed C-DISC training at Columbia University and was authorized to train others. Interviewers were also required to perform a series of interviews proving their ability to handle a wide array of responses that typically occur in the course of telephone interviewing. Interview quality was continuously assessed through silent monitors installed on all telephones. Written feedback on errors, and corrective instruction were provided.
Assessment of Functional Impairment
The 13-item Columbia Impairment Scale (CIS) [23] is a psychosocial functional impairment scale with high reliability and validity that is widely used in youth anxiety and depression studies. Items follow the uniform lead in of “In the past 3 months, in general, how much trouble have you had with:” and include “getting into trouble”; getting along with your mother/mother figure”; getting along with other kids your age”; your school work or doing your job”. It has been shown to be highly correlated with other indicators of psychological dysfunction and with the clinician-rated Children’s Global Assessment Scale (CGAS) [23, 24].
The Child Health Survey-Asthma (CHS-A) is an asthma functional status measure with high reliability and validity in capturing a broad range of asthma-related experiences [25]. The instrument contains 3 scales (physical health, emotional health, activity limitations) which are rated on a 5 point scale from 1 (all of the time) to 5 (none of the time). Examples of the physical health items include “During the last 2 weeks, because of your asthma, how much of the time have you …”had shortness of breath”,”wheezing without a cold”. Examples of the emotional health items include “ how much did the following statements describe you in that last two weeks”, ”I was upset about having asthma”, I felt left out by other people because of my asthma”, I was angry about having to take asthma treatments”. Examples of the activity limitation items include “how much of the time were you limited from participating in the following activities—“school gym classes”, strenuous activities such as running fast or playing hard”, moderate activities such as bike riding or walking upstairs”, “mild activities such as walking” (activity limitations).
Asthma severity was assessed using a modified version of the Health Plan Employer Data and Information Set (HEDIS) [26] definition of children/adolescents who are at high risk of adverse asthmatic events. Reviews of the HEDIS as an asthma measure indicate that while it is the most widely used tool it may overclassify patients with intermittent asthma as having persistent asthma [27]; . In an effort to improve sensitivity and specificity of the HEDIS measure as a risk factor for subsequent medical costs and adverse events in the current study we used a more conservative medication criteria (criteria 1 below) than is used in the standard HEDIS criteria. In this modified definition, meeting criteria for any of the following four health care utilization variables over a 12-month period identify the individuals at high medical risk: 1) ≥1 oral steroid prescriptions for asthma over a 12-month period; oral steroids are used only with youth with more severe disease; 2) >1 emergency visit or hospitalization for asthma; 3) ≥4 ambulatory visits for asthma. These criteria were used to divide the overall sample into three groups reflecting mild (No high medical risk markers), moderate (1 marker of high medical risk) or severe (2 or more markers of high medical risk).
Statistical Analyses
We examined differences in unidentified data between survey respondents and non-respondents using GHC automated data. Due to the response rate of about 60% we estimated the propensity to, or the probability of responding to the survey (yes/no) as a function of the following variables: age, gender, being on Medicaid or state-funded insurance because of low income, Eastern versus Western Washington, Pediatric Chronic Disease Score [28], number of primary care visits, number of asthma-related emergency room visits and hospitalizations, oral steroid prescriptions, any prescription for antidepressant or anti-anxiety medication, number of specialty mental health visits, and an ICD-9 diagnosis of anxiety or depression. All health utilization variables refer to the prior 12 months.
Using these predictors, we estimated a response probability (using PROC logistic of SAS) for each survey respondent (response propensity score). All analyses in this study are weighted analyses (weights inversely proportional to estimated probability of response) rescaled to sum to the observed sample size (i.e. the number of survey respondents). In weighted analyses, individuals with a low probability of response were given a higher weight to represent the larger number of non-respondents with similar characteristics. Weighting was used to adjust for the fact that only a subsample of the eligible group care cooperative population were included in the sample.
The two study groups (those with no psychiatric diagnoses, and those with at least one anxiety or depression diagnosis) were compared on demographic and clinical variables using chi square analyses with corrections for continuity for the categorical variables and t tests for the continuous variables.
In order to identify variables that were independently and significantly associated with levels of functioning on the four measures of functional impairment, weighted multiple linear regression models were employed. Our dependent variables were the CIS and the three CHS-A scales (emotional, physical and activities). In the first step of the analyses, we tested the significance of the covariates (i.e., demographic indicators) in each model and retained only significant variables. In the second step, we added the asthma severity variable and retained it in the model regardless of statistical significance. In the third step we added the three psychological independent variables of interest: a diagnosis of anxiety and/or depression, the mood feelings questionnaire and the anxiety sensitivity index. In the last step we tested for two-way statistical interactions of the 3 independent variables and the asthma severity indicator using backwards and forwards stepwise techniques. None of the interactions were statistically significant for any model. Therefore, the final models presented contain significant covariates, asthma severity, and the statistically significant independent variables. No significant demographic variable from the first step lost its significance in the presence of the significant asthma or independent variables.
Finally as a sensitivity analysis, we ran the four multiple regression analyses without the use of the weights. The results were nearly identical to those found using the weighted approach and therefore the weighted results are presented.
Results
A total of 125 children/adolescents met DSM-IV criteria for one or more anxiety and depressive disorders in the last 12 months (16.2%) with 68 (8.9%) having an anxiety disorder alone, 20 (2.5%) a depressive disorder alone, and 37 (4.8%) both an anxiety and depressive disorder. The presence of an anxiety or depressive disorder was distributed evenly across all age groups within the sample. Only 35% of youth with ≥1 anxiety and depressive disorders and 43% of those with major depression had been recognized by the medical system over the 12-month period prior to these interviews [29]. Furthermore, only 10% of youth with >1 DSM IV anxiety or depressive disorders and 20% of those with major depression received 4 or more sessions of psychotherapy and only 14 (11.4%) of youth with >1 anxiety or depressive disorders and 9 (16.1%) of youth with major depression received 90 days or more of an antidepressant prescription [29].
Table 1 summarizes the demographic characteristics and questionnaire responses of youth without an anxiety or depressive disorder compared to those with ≥1 anxiety or depressive disorders. As reported by Katon [30], youth in this sample with a disorder were more likely to be female, to have a parent with less than high school education, and to have a lower median household income than youth with no diagnosis. There was no significant difference between the groups on the modified HEDIS asthma severity measure. The group with at least one anxiety or depressive disorder had mean scores indicating significantly worse psychological symptoms (SMFQ, ASI) and functioning (CIS, CHS-A scales).
Given the overlapping nature of the constructs measured, Table 2 presents the correlations between each of the measures. Table 3 presents the results of the regression models for the association between youth asthma and mental health characteristics and the four functional status outcomes. Standardized betas that represent the relative importance of the association of the variable with the outcome controlling for the other model variables and adjusted R2’s are presented. Standardized betas allow you to compare the association of variables that are measured in very different units. They are numerically very similar to the correlation of the variable and the outcome controlling for all the other model variables (partial correlation). At each step the incremental R2 and its significance is presented. The betas presented are those from the full model.
Table 2.
Pearson Correlations between Measures
| MEASURE | ASTHMA SEVERITY | Mood & Feelings Q | Anxiety Sensitivity Index | CIS Scale | CHS-A - Activities | CHS-A - Emotional Health | CHS-A - Physical Health |
|---|---|---|---|---|---|---|---|
| ASTHMA SEVERITY (N=769) | .008 | .074(*) | .026 | −.069 | −.099(**) | −.129(**) | |
| Mood & Feeings Q (N=765) | 1 | .547(**) | .667(**) | −.247(**) | −.423(**) | −.390(**) | |
| Anxiety Sensitivity Index (N=767) | 1 | .472(**) | −.277(**) | −.455(**) | −.332(**) | ||
| CIS Scale (N=767) | 1 | −.304(**) | −.431(**) | −.396(**) | |||
| CHS-A – Activities (N=769) | 1 | .512(**) | .485(**) | ||||
| CHS-A - Emotional Health (N=769) | -. | 1 | .572(**) |
Correlation is significant at the 0.05 level (2-tailed).
Correlation is significant at the 0.01 level (2-tailed).
Table 3.
Multiple Linear Regression Results for the Functional Status Outcomes
| FUNCTIONAL STATUS OUTCOMES | ||||
|---|---|---|---|---|
| CHS-A ACTIVITIES SCALEc |
CHS-A EMOTIONAL SCALEc |
CHS-A PHYSICAL SCALEc |
COLUMBIA IMPAIRMEN T SCALEd |
|
| Total Model Test | F(6,760) = 19.80*** | F(5,761) = 56.89*** | F(4,762) = 47.02*** | F(6,760) = 111.57*** |
| Total Adjusted R2 | R2 = .13 | R2 = .27 | R2 = .20 | R2 = .47 |
| Standardized Betaa | Standardized Betaa | Standardized Betaa | Standardized Betaa | |
|
Covariates | ||||
| Genderb | −0.14*** | −0.06* | ||
| GEO Income | 0.11*** | No Significant Covariates | ||
| White Parente | 0.07* | |||
| Employment | −0.05* | |||
| Adjusted R2 for all covariates | R2 = .06*** | R2 = .01** | R2 = .01* | |
| Asthma Severity Standardized Betaa | −0.04 | −0.07* | −0.11*** | 0.01 |
| Adjusted R2 Change | R2 = .00 | R2 = .01** | R2 = .02*** | R2 = .00 |
|
Psychological Variables | ||||
| Mood Feelings Q | −0.09* | −0.21*** | −0.26*** | 0.57*** |
| Anxiety Sensitivity Index | −0.14*** | −0.27*** | −0.11** | 0.14*** |
| DSM-IV Anxiety/Depression Diagnosis | −0.10** | −0.13*** | −0.14*** | 0.06* |
| Adjusted R2 Change | R2 = .07*** | R2 = .25*** | R2 = .18*** | R2 = .46*** |
= standardized betas reflect the relative importance of the association of the variable with the outcome controlling for the other model variables and are the standardization of the raw regression coefficients. The values presented betas when all the variables are in the model;
p < .05;
p < .01;
p < .001;
= Gender 0 = Male, 1 = Female;
= higher indicates better functioning;
= higher scores indicated poorer functioning. E = white = 0, non-white = 1.
All four models explained statistically significant amounts of variance in the functional status outcomes. The adjusted R2s ranged from .47 for the CIS to .13 for the CHS-A activities scale. Gender, GEO code income, having a Caucasian parent and parental employment were significant covariates in the models: Female youths had worse functioning than males on the CHS-A activities scale [Adjusted mean ± SD for females = 80.9 ± 17.6; males = 86.0 ± 16.0]. In contrast, on the CIS, female youths reported less impairment in functioning [Adjusted mean ± SD for females = 10.8 ± 9.0; males = 11.8 ± 8.6] however, the difference of 1 point is not clinically meaningful. Increasing median household income was associated with better functioning on the CHS-A activities scale (r = .15). Having a Caucasian parent was associated with better functional status on the CHS-A emotional scale functioning [Adjusted mean ± SD for youth with white parents = 84.2 ± 14.1; non-Caucasian parents = 81.8 ± 16.6], having least one parent employed was associated with less impairment on the CIS scale [Adjusted mean ± SD for not employed = 13.2 ± 10.4; employed = 11.2 ± 8.8] but these differences are not clinically meaningful and are only statistically significant due to the large sample size.
Asthma severity (modified HEDIS score) was significantly associated with more severe impairment on the CHS-A Emotional and Physical Functional status scales, but not with the CHS-A Activities score or the CIS. Although increases in asthma severity were associated with poorer functioning, the actual R2s of 1% – 2% are not clinically meaningful.
The psychological variables were significantly associated with all 4 outcomes with incremental adjusted R2s ranging from .07 for CHS-A Activities scale to .46 for the CIS. In spite of the potential colinearity of the psychological variables they all explained independent and significant variation in the outcomes. Based on the size of the beta coefficients, the associations appear to be clinically meaningful.
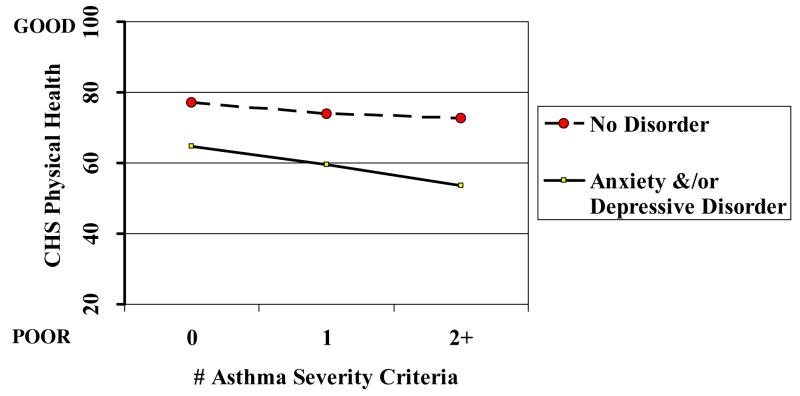
No statistically significant interactions of asthma severity and the psychological variables were found. This indicates that asthma severity and the psychological variables are additive in their explanatory power for functional impairment and there is no negative synergism. As depicted in Figure 2 for each level of increasing asthma severity, there are similar decreases in functioning among youths with an anxiety and/or depressive diagnosis. At each level of asthma severity, meeting criteria for ≥1 anxiety and/or depressive disorder was associated with increased functional impairment.
Figure 2.
Relationship of CHS Physical Health Scale to Anxiety/Depressive Disorders and Asthma Severity
DISCUSSION
This goal of this paper was to explore the extent to which psychiatric factors as reflected in DSM-IV anxiety and depressive diagnosis and severity of self-reported anxiety and depressive symptoms play a significant role in how young people with asthma function in terms of both asthma related and psychosocial adjustment.. These data from this large epidemiological study of adolescents with asthma in an HMO revealed that self-report of depressive and anxiety symptoms and presence of ≥ DSM-IV anxiety or depressive diagnosis each independently are associated with more impaired psychosocial and asthma related functional status. Each of these depression and anxiety measures were more significantly associated with all four functional outcomes than the modified HEDIS asthma risk measure. After controlling for a host of demographic variables (age, gender, parental employment, parental education, family median income, race and whether the family lived in a more urban (west) or rural (east) part of the state) youth who endorsed more symptoms of depression or anxiety also reported greater psychosocial and asthma related functional impairment. The fact that a similar degree of additive impairment based on having ≥1 anxiety or depressive disorder was seen at each level of asthma severity suggests that this effect is not due to greater severity of asthma in youth with psychiatric disorders. It is possible that some overlap in content on the symptom and behavioral function measures would explain the stronger association observed between depression and anxiety and psychosocial versus asthma related function. Furthermore, anxiety and depression were not significantly related to asthma severity as reflected in the modified HEDIS scoring system. These findings suggest that identification and treatment of psychiatric comorbidities may be one promising strategy to improve asthma outcomes.
These findings complement the significant body of work that has been conducted with adults. Large epidemiologic studies of patients with illnesses such as diabetes mellitus [31] and coronary artery disease [32] have also shown that depression is associated with increased functional impairment after controlling for severity of disease. Studies of adults have consistently found that comorbid depressive and anxiety disorders are associated with increased symptom burden in patients with chronic medical illness, potentially worsening the disability associated with these illnesses [33]. Wells and colleagues [34] demonstrated that when major depression is comorbid with medical illness, there is additive functional impairment. Studies have also demonstrated that major depression and anxiety disorders have an adverse impact on adherence to self-care regimens (i.e., diet, exercise, quitting smoking) in adult patients with chronic medical illness [31–37]. A recent meta-analysis of the effect of depression and anxiety on adherence by Dimatteo and colleagues [38] showed that, compared to nondepressed/nonanxious patients, the odds were three times greater that depressed and anxious patients would be nonadherent with medical treatment recommendations. Nonadherence may cause increased complications, health utilization and medical costs as well as worsen the course of symptoms and physical impairment due to medical illness [39].
Less research has been reported on the impact of mental health problems on the functional status of asthmatic youth. However, in a recent study of adolescents, Kean and colleagues [40] found that, even after accounting for asthma severity, asthma functional morbidity was significantly associated with anxiety, depressive and asthma related Post Traumatic Stress symptoms. Anxiety and depression may be more common in youth with asthma because the same neurotransmitters that regulate affect may be involved in processes such as bronchoconstriction and inflammation [11] Others propose that experience with asthma may generate fearful or catastrophic beliefs about respiratory symptoms which provoke and sustain anxiety and over time, depressive symptoms [41. 42]. Furthermore, because children with asthma have a higher level of intrinsic airway resistance, negative stressors and mood states may be much more likely to result in significant airway changes in resistance undermining self-confidence in learning to master these situations [43]. Decreased confidence and sense of control to manage illness symptoms may, in turn, undermine active behavioral self-management strategies such as taking medication regularly, monitoring peak expiratory flow and quitting smoking. Decreased self-management may then worsen asthma symptom burden, increase medical utilization and costs and lead to increased functional impairment.
Limitations
The cross sectional design of this study precludes causal interpretations of the findings. Inclusion of only adolescents with health insurance limits the ability to generalize to the large population of youth who do not have ready access to health care.. As pointed out by Goodwin and colleagues (1 2) the association between asthma, anxiety, and depression, and in turn the impact of anxiety and depression on functional status, may also reflect the effects of common familial (poverty, childhood abuse) or environmental factors (exposure to secondhand smoke or pollution). Another limitation is the reliance on self-reports for anxiety and depression as well as asthma related functional status. While self-report of depression has been shown to have good reliability [44], depression and anxiety can affect response style such that youth who report more symptoms of depression or anxiety may see themselves and their ability to function in a more negative light.
In addition, the use of the HEDIS as an independent measure of asthma severity is limited by its lack of a biological measure. We are able to corroborate some of our findings via medical record data but a multimethod, multisource, longitudinal approach is needed to more fully explore the relations among these key variables over time. The strengths of this study included sampling from a large community-based sample using a physician-based definition of asthma, youth representing a wide range of asthma severity, and an interview based DSM-IV diagnostic assessments as well as self-reported mood and anxiety symptoms.
CONCLUSIONS
This paper adds significantly to the literature by underscoring the need for identification and treatment of anxiety and depressive symptoms as one strategy to improve asthma management and outcomes. Increased awareness of, and attention to, the assessment and management of psychiatric symptoms in youth with asthma may reduce the burden of asthma, contribute to an improved sense of efficacy in ability to manage asthma symptoms and improve treatment compliance and outcomes.
Acknowledgments
Supported by a grant #MH 01643 from the National Institute of Mental Health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weiss KB, Gergen PJ, Wagener DK. Breathing better or wheezing worse? The changing epidemiology of asthma morbidity and mortality. Annu Rev Public Health. 1993;14:491–513. doi: 10.1146/annurev.pu.14.050193.002423. [DOI] [PubMed] [Google Scholar]
- 2.Nystad W, Magnus P, Gulsvik A, Skarpaas IJ, Carlsen KH. Changing prevalence of asthma in school children: evidence for diagnostic changes in asthma in two surveys 13 yrs apart. Eur Respir J. 1997;10:1046–51. doi: 10.1183/09031936.97.10051046. [DOI] [PubMed] [Google Scholar]
- 3.Lozano P, Connell FA, Koepsell TD. Use of health services by African-American children with asthma on Medicaid. Jama. 1995;274:469–73. [PubMed] [Google Scholar]
- 4.Vollmer WM, Buist AS, Osborne ML. Twenty year trends in hospital discharges for asthma among members of a health maintenance organization. J Clin Epidemiol. 1992;45:999–1006. doi: 10.1016/0895-4356(92)90115-4. [DOI] [PubMed] [Google Scholar]
- 5.Greineder DK, Loane KC, Parks P. Reduction in resource utilization by an asthma outreach program. Arch Pediatr Adolesc Med. 1995;149:415–20. doi: 10.1001/archpedi.1995.02170160069010. [DOI] [PubMed] [Google Scholar]
- 6.Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104:1274–80. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- 7.Ortega AN, Huertas SE, Canino G, Ramirez R, Rubio-Stipec M. Childhood asthma, chronic illness, and psychiatric disorders. J Nerv Ment Dis. 2002;190:275–81. doi: 10.1097/00005053-200205000-00001. [DOI] [PubMed] [Google Scholar]
- 8.McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: a meta-analysis. J Dev Behav Pediatr. 2001;22:430–9. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Wamboldt MZ, Fritz G, Mansell A, McQuaid EL, Klein RB. Relationship of asthma severity and psychological problems in children. J Am Acad Child Adolesc Psychiatry. 1998;37:943–50. doi: 10.1097/00004583-199809000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Vila G, Nollet-Clemencon C, de Blic J, Mouren-Simeoni MC, Scheinmann P. Prevalence of DSM IV anxiety and affective disorders in a pediatric population of asthmatic children and adolescents. J Affect Disord. 2000;58:223–31. doi: 10.1016/s0165-0327(99)00110-x. [DOI] [PubMed] [Google Scholar]
- 11.Mrazek DA. Psychiatric symptoms in patients with asthma causality, comorbidity, or shared genetic etiology. Child Adolesc Psychiatr Clin N Am. 2003;12:459–71. doi: 10.1016/s1056-4993(03)00028-2. [DOI] [PubMed] [Google Scholar]
- 12.Goodwin RD, Fergusson DM, Horwood LJ. Asthma and depressive and anxiety disorders among young persons in the community. Psychol Med. 2004;34:1465–74. doi: 10.1017/s0033291704002739. [DOI] [PubMed] [Google Scholar]
- 13.Richardson LP, Lozano P, Russo J, McCauley E, Bush T, Katon W. Asthma Symptom Burden: Relationship to Asthma Severity and Anxiety and Depression Symptoms. Pediatrics. doi: 10.1542/peds.2006-0249. in press. [DOI] [PubMed] [Google Scholar]
- 14.Annett RD, Bender BG, Lapidus J, Duhamel TR, Lincoln A. Predicting children’s quality of life in an asthma clinical trial: what do children’s reports tell us? J Pediatr. 2001;139:854–61. doi: 10.1067/mpd.2001.119444. [DOI] [PubMed] [Google Scholar]
- 15.Weil CM, Wade SL, Bauman LJ, Lynn H, Mitchell H, Lavigne J. The relationship between psychosocial factors and asthma morbidity in inner-city children with asthma. Pediatrics. 1999;104:1274–80. doi: 10.1542/peds.104.6.1274. [DOI] [PubMed] [Google Scholar]
- 16.Silverman WK, Ginsburg GS, Goedhart AW. Factor structure of the childhood anxiety sensitivity index. Behav Res Ther. 1999;37:903–17. doi: 10.1016/s0005-7967(98)00189-2. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: replication and extension. J Abnorm Psychol. 1999;108:532–7. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- 18.Angold A, Costello EJ, Messer SC, et al. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–49. [Google Scholar]
- 19.Achenbach TM. Child Behavioral Checklist (CBCL) Burlington: University of Vermont; 2001. [Google Scholar]
- 20.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Wells KB, Burnam MA, Leake B, Robins LN. Agreement between face-to-face and telephone-administered versions of the depression section of the NIMH Diagnostic Interview Schedule. J Psychiatr Res. 1988;22:207–20. doi: 10.1016/0022-3956(88)90006-4. [DOI] [PubMed] [Google Scholar]
- 22.Simon GE, Revicki D, VonKorff M. Telephone assessment of depression severity. J Psychiatr Res. 1993;27:247–52. doi: 10.1016/0022-3956(93)90035-z. [DOI] [PubMed] [Google Scholar]
- 23.Bird HR, Andrews H, Schwab-Stone ME, et al. Columbia Impairment Scale (CIS). Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research. 1996;6:295–307. [Google Scholar]
- 24.Bird HR, Canino G, Rubio-Stipec M, Ribera JC. Further measures of the psychometric properties of the Children’s Global Assessment Scale. Arch Gen Psychiatry. 1987;44:821–4. doi: 10.1001/archpsyc.1987.01800210069011. [DOI] [PubMed] [Google Scholar]
- 25.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and validity of the Children’s Health Survey for Asthma. Pediatrics. 1999;104:e71. doi: 10.1542/peds.104.6.e71. [DOI] [PubMed] [Google Scholar]
- 26.National Committee for Quality Assurance. HEDIS 3.0. 1997.
- 27.Gelfand EW, Colice GL, Fromer I, Bunn WB, David TJ. Use of the Health Plan Employer Data and Information Set for measuring and improving the quality of asthma care. Annals of Allergy, Asthma & Immunology. 2006;97:298–305. doi: 10.1016/S1081-1206(10)60793-4. [DOI] [PubMed] [Google Scholar]
- 28.Fishman PA, Shay DK. Development and estimation of a pediatric chronic disease score using automated pharmacy data. Med Care. 1999;37:874–83. doi: 10.1097/00005650-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Katon WJ, Richardson L, Russo J, Lozano P, McCauley E. Quality of mental health care for youth with asthma and comorbid anxiety and depression. Med Care. 2006;44:1064–1072. doi: 10.1097/01.mlr.0000237421.17555.8f. [DOI] [PubMed] [Google Scholar]
- 30.Katon W, Lozano P, Russo J, McCauley E, Richardson L, Bush T. The Prevalence and Demographic and Clinical Factors Associated with DSM-IV Anxiety and Depressive Disorders in Children and Adolescents with Asthma. under review. [Google Scholar]
- 31.Ciechanowski P, Katon W, Russo J. Depression and diabetes: impact of depressive symptoms on adherence, function and costs. Arch Intern Med. 2000;160:3278–85. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 32.Sullivan MD, LaCroix AZ, Baum C, Grothaus LC, Katon WJ. Functional status in coronary artery disease: a one-year prospective study of the role of anxiety and depression. Am J Med. 1997;103:348–56. doi: 10.1016/s0002-9343(97)00167-8. [DOI] [PubMed] [Google Scholar]
- 33.Katon W, Sullivan MD. Depression and chronic medical illness. J Clin Psychiatry. 1990;51(Suppl):3–11. discussion 2–4. [PubMed] [Google Scholar]
- 34.Wells KB, Golding JM, Burnam MA. Psychiatric disorder in a sample of the general population with and without chronic medical conditions. Am J Psychiatry. 1988;145:976–81. doi: 10.1176/ajp.145.8.976. [DOI] [PubMed] [Google Scholar]
- 35.Glasgow RE. Compliance to diabetic regimens: conceptualization, complexity, and determinants. In: Cramer JA, Spilker B, editors. Patient compliance in medical practice and clinical trials. New York: Raven Press; 1991. pp. 209–24. [Google Scholar]
- 36.Blumenthal JA, Williams RS, Wallace AG, Williams RB, Jr, Needles TL. Physiological and psychological variables predict compliance to prescribed exercise therapy in patients recovering from myocardial infarction. Psychosom Med. 1982;44:519–27. doi: 10.1097/00006842-198212000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL. Depression and the dynamics of smoking. A national perspective. Jama. 1990;264:1541–5. [PubMed] [Google Scholar]
- 38.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 39.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–26. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 40.Kean EM, Kelsay K, Wamboldt F, Wamboldt MZ. Posttraumatic stress in adolescents with asthma and their parents. J Am Acad Child Adolesc Psychiatry. 2006;45:78–86. doi: 10.1097/01.chi.0000186400.67346.02. [DOI] [PubMed] [Google Scholar]
- 41.Zaubler TS, Katon W. Panic disorder and medical comorbidity: a review of the medical and psychiatric literature. Bull Menninger Clin. 1996;60:A12–38. [PubMed] [Google Scholar]
- 42.Roy-Byrne P, Stein M. Inspiring panic. Arch Gen Psychiatry. 2001;58:223–4. doi: 10.1001/archpsyc.58.2.123. [DOI] [PubMed] [Google Scholar]
- 43.Pine D. Respiration in children at risk for panic disorder. (Response to Perna et al.’s Letter to the Editor) Arch Gen Psychiatry. 2002;59:186. doi: 10.1001/archpsyc.59.2.185. [DOI] [PubMed] [Google Scholar]
- 44.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2006;74(3):401–415. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]